Abstract
The objective of the study is to find predictors of remission, radiographic progression (RP), and erosive disease in a cohort of patients with early onset rheumatoid arthritis (EORA) that followed a therapeutic protocol aiming at remission, in a real world tight-control setting. EORA patients were enrolled in a 3-year follow-up study. Clinical, biological, immunogenetic, and radiographical data were analyzed. Radiographs were scored according to Sharp–van der Heijde (SvdH) method. RP was defined by an increase of 3 units in 36 months. Remission was defined as DAS28 <2.6. A stepwise multiple logistic regression model was used to identify independent predictors of the three target outcomes. One hundred twenty-nine patients were included. Baseline disease activity was high. Significant overall improvement was observed, but only 33.3 % achieved remission. At 36 month, 50.4 % (65) of patients showed erosions. RP was observed in 62.7 % (81) of cases. Statistical analysis showed that baseline SvdH score was the only predictive factor associated with the three outcomes evaluated. Lower HAQ-DI and absence of autoantibodies were predictive of remission. Higher levels of ESR and presence of erosions at entry were predictive of RP. Independent baseline predictors of incident erosive disease were anti-CCP and RF positivity, symptom duration at baseline >3 months, and presence of HLA-DRB1 shared epitope. Radiographic damage at baseline was the main predictor of outcomes. Autoantibodies, HAQ and ESR at baseline, symptom duration before diagnosis, and HLA-DRB1 status had influence on clinical course and development of structural joint damage in Colombian RA patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Rheumatoid arthritis (RA) is a complex, multifactorial, inflammatory disease of unknown etiology with considerable social and economic costs. The clinical course ranges from mild joint swelling to severe polyarthritis with progressive destruction of cartilage and bone. Both genetic and environmental factors can contribute to disease initiation and severity course. It is considered that after 12 years of disease progression, 80 % of patients are partially limited and 16 % has a total limitation [1, 2]. It has been shown that the first 2–3 years of evolution of RA are crucial to predict the long-term prognosis of the disease, and early treatment with disease-modifying antirheumatic drugs (DMARDs) and/or biologic therapy improves clinical and radiological outcome in these patients [3–8].
The underlying inflammatory process of the RA can produce joint erosions even 8 weeks subsequent to the onset of symptoms [9]. Although no drug therapy completely prevents the development of erosions at present, each day becomes more important to predict which patients will develop erosive disease which determines a worse clinical and functional prognosis. This may allow treatment to be tailored for the individual patient with RA.
Various studies have attempted to identify prognostic factors of radiographic progression in patients with early onset RA (EORA). Most studies that have been published to determine prognostic factors in EORA have been conducted in Caucasian and American population. Due to important contribution of genetic factors in RA as shown by twin concordance studies [10] and genetic differences between those people and Latin American population, results obtained are not completely reproducible in our population.
In this study, we examined the baseline clinical, immunological, and genetic prognostic factors of radiographic progression and disease activity in a serie of Colombian patients with EORA followed during a period of 3 years.
Patients and methods
Patients
The study included patients with EORA (disease duration <12 months) fulfilling the 1987 and 2010 American College of Rheumatology (ACR) criteria for RA who were attending the Rheumatology Unit of the “Universidad Nacional de Colombia,” and the “Clínica de Artritis y Rehabilitación (CAYRE)” in Bogota, Colombia, and that reached a follow-up of 36 months. Exclusion criteria were the presence of other inflammatory arthropathies (e.g., psoriatic arthritis), current or previous use of DMARDS or oral glucocorticoids, serious medical disorders (e.g., hepatic or cardiac failure), and women in child bearing age without adequate contraceptive protection. This study was conducted in accordance with the Declaration of Helsinki for the protection of human subjects in research. All patients gave their informed consent to enter into the study, which was approved by our Ethics Institutional Committee.
Study design
We conducted a prospective open-label study where all patients were treated according to a therapeutic protocol, with early introduction of DMARDs using a step-up approach. In all cases, Methotrexate (MTX) at a dose of 7.5 mg/week was prescribed as the first-choice DMARD. An increasing dose of 7.5 to 20 mg was used if no clinical improvement was observed at month 6. At baseline, it was also allowed the concurrent use of antimalarials, Hydroxychloroquine (HCQ) 200 mg/day—chloroquine (CQN) 150 mg/day, or sulphasalazine (SSZ) 1 g/day according to the physician’s criteria.
Depending on clinical judgment, glucocorticoid therapy was used, without exceeding 15 mg of prednisolone or equivalent. After the first year of therapy, patients were treated without an established protocol algorithm and according to the criteria of the treating physician, but with an aggressive approach using other DMARDs in monotherapy or in combination in cases with a poor response to previous DMARDs. Biological therapy was initiated in a few cases in patients with a poor response to DMARDs. The use of NSAIDs and analgesics was allowed in all strategies. The study design was proposed under these conditions in order to simulate a “real-life”-like situation.
All patients were assessed by a rheumatologist at the start of the study and every 6 months thereafter during 3 years. Using standard methods, detailed assessments by the physicians included complete tender (TJC) and swollen joint counts (SJC), fatigue, morning stiffness duration, and physician global assessment. Patient-reported outcomes included global assessments of pain and general health on 10-cm visual analog scales and HAQ disability index (HAQ-DI). In addition, blood was drawn for routine chemistry and hematology as well as for erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP). This set of outcome measures served additionally to calculate the disease activity score (DAS28), DAS28 PCR, the Simplified Disease Activity Index (SDAI), and the Clinical Disease Activity Index (CDAI). Disease activity according to DAS28 was interpreted as remission (DAS28 <2.6), low (2.6 ≤DAS28 ≤3.2), moderate (3.2 <DAS28 ≤5.1), and high (DAS28 >5.1) activity.
At study entry, demographic characteristics, disease duration, serum rheumatoid factor (RF), anticyclic citrullinated peptide antibodies (aCCP), antinuclear antibodies (ANAs), and anti-SSA/Ro. A DNA sample for determination of HLA-DRB1 genotype and TNF single nucleotide polymorphism (SNP) at −308 position was also obtained. Radiographs of the hands/wrists and feet were performed at baseline and third year.
TNF and HLA-DRB1 genotyping
Genomic DNA was extracted from 10 ml of an EDTA-anticoagulated blood sample using the standard salting out technique. Genotyping for the TNF SNP at −308 position was performed by polymerase chain reaction (PCR). This SNP has been shown to influence the risk of acquire RA in Latin-Americans [11]. HLA-DRB1 typing was done by reverse dot-blot hybridization of the PCR products (Inno-LiPA assay, Innogenetics, Ghent, Belgium). Genetic susceptibility to RA is associated with certain HLA-DRB1 alleles encoding a similar sequence motif called the “shared epitope” (SE). This SE is coded mainly by the HLA-DRB1 *0101, *0102, *0401, *0404, *0405, *0408, *0409, *0410, *1402, and *1001 alleles. Also, HLA-DRB1 *0103, *0402, *1102, *1103, *1301, *1302, and *1304 alleles encode the DERAA sequence at the same positions. Hence, HLA-DRB1 status was categorized according to the presence or absence of the SE and DERAA motifs.
Radiographic assessments
Radiographs in a standard posteroanterior view of the hands/wrists and anteroposterior view of the feet were performed at baseline and third year. Films were digitalized (VIDAR® SIERRA plus Film Digitizer) and scored by two independent and experienced readers according to the Sharp–van der Heijde (SvdH) method. For each radiograph set (By using three Kodak directView 5 MP monochrome display model # DV5MM), the scores of the two readers were averaged. The readers were blind to patient’s identity and treatment and to chronological sequence of the films. Sixteen joint areas were assessed for erosions (scale, 0–5) and fifteen areas for joint space narrowing (JSN) (scale, 0–4) in each hand. A total of 6 joints of each forefoot were scored for erosions (scale, 0–10) and JSN (scale, 0–4). The maximum total scores for hands and feet combined were 280 for erosions and 168 for JSN (total score, 448). The reliability of the scores was assessed through intraclass correlation coefficients, which for hands radiographic score was 0.95 (95 % CI 0.89–0.97) and for feet was 0.80 (95 % CI 0.62–0.90). Overall progression of radiographic damage was defined by an increase in the total score of 3 units in 36 months [12, 13].
Laboratory measurements
ESR was determined by Westergren method, CRP and RF were determined by nephelometry. aCCP were measured by (third generation) enzyme-linked immunosorbent assay (ELISA, (QUANTA-Lite, INOVA, San Diego, CA) and considered positive at a cut-off value >40 units as suggested by the manufacturer
Statistical analysis
Categorical and quantitative variables were described as frequencies, percentages, means and standard deviations (mean ± SD). The non-parametric Mann–Whitney U test was used to compare the continuous variables. Categorical variables were analyzed using χ 2 test or Fisher’s exact test. A stepwise multiple logistic regression model was used to examine which factors were associated with DAS28 remission, erosive disease and radiologic progression at the end of follow-up. The variables included in the multivariate model were selected using univariate analysis (p < 0.10). The significance level was set at 0.05. Data were analyzed using SPSS 20.0 software
Results
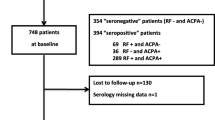
This study enrolled 159 patients with EORA (78.2 % women), whose mean (SD) age was 46.6 (±14, 6) years at the start of the study. Follow-up duration was 36 months. Of the 159 patients, 30 dropped out during follow-up and were not included in the final statistical analysis. Causes of drop out were death (2), moved out of the area (18), and otherwise, or reason unknown (10). No patient left the study because of side-effects. At 36 months, data was available for 129 patients. Baseline characteristics are shown in Table 1.
There was a short interval between symptom onset and RA diagnosis in most cases with a mean of 4.29 (±3.0) months. Disease activity at baseline was high as reflected by a mean SJC of 20.69 (±7.9), a mean of TJC of 21.84 (±7.0), a mean of DAS28 6.73 (±0.9), SDAI 59.26 (±17) and CDAI 57.31 (±16.7). Sixty-four (49.6 %) of the patients were SE carriers and 22 (17 %) were DERAA carriers. Ninety-one (70.5 %) of the patients were RF positive, and 90 (69.7 %) were aCCP positive.
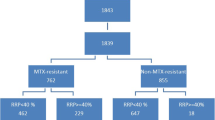
Over the 36-month period, 20 patients (15.5 %) received MTX monotherapy, 80 (62.0 %) were on a combination of MTX plus antimalarials, and 29 (22.4 %) on MTX plus SSZ. The starting dose of MTX 7.5 mg/week was increased gradually to a maximum of 20 mg/week (mean (SD) dose 15 (3.4) mg/week) at 36 months. Glucocorticoids (5–15 mg/day) were prescribed in 105 (81.3 %) of patients. Biological therapy was initiated in 8 (6.2 %) patients with a poor response to DMARDs.
Disease remission
In all, 43 patients (33.3 %) achieved remission defined as DAS28 <2.6 at the end of follow-up. Mean DAS28 was 3.47 (±1.72), a significant improvement from baseline (p < 0.0001); 14.7 % (19) of patients achieved low disease activity, 30.2 % (39) had moderate disease activity, and 21.7 % (28) patients had high disease activity. At study entry, moderate functional disability was observed with a mean HAQ-DI of 1.21 (±0.62), which decreased significantly to 0.35 (±0.46) from baseline (p < 0.0001) at 36 months of follow-up. Considering disease activity, 100 % of patients in remission reached a HAQ less than 0.5 (no disability) compared with 67.4 % (28) of patients not reaching remission (p 0.0001). Other parameters of disease’s activity, as ESR, serum CRP levels, TJC, SJC, SDAI, CDAI were reduced (all p values < 0.001), as expected (Table 1).
Mean values of the following baseline characteristics were significantly worse for patients with DAS28 >2.6 than for those in remission at end of follow-up: fatigue (6.54 ± 2.5 vs 5.37 ± 3.0 p = 0.02) and HAQ (1.31 ± 0, 6 vs 1.01 ± 0.5 p = 0.009) . The percentage of patients with positive aCCP, RF, and ANAs at baseline was significantly higher in patients with active disease than in those without (76.7 % v 55.8 % p = 0.02), (76.7 % v 58.1 % p = 0.04) and (38.3 % vs 16.2 % p = 0.01), respectively. Age, genre, smoking history, education level, first involved joints, symptom duration at diagnosis, SJC, TJC, ESR, CRP, baselines DAS28, DAS28CRP, SDAI, and CDAI did not differ significantly between the two groups. There were no differences in patients carrying HLA-DRB1 SE, DERAA-alleles, or TNF-α (SNP)–308 polymorphism (Table 2).
The percentage of patients in remission at end of follow-up was not significantly different between the treatment strategy groups with p > 0.05 for all comparisons.
Radiographic assessment
At the baseline visit, the mean (SD) erosion score was 1.58 (3.73) with 29.4 % (38) of the patients showing erosions; the mean (SD) JSN scores was 6.18 (5.30) with 93.0 % (120) displaying JSN; at this visit, the mean SvdH (SD) total score was 7.8 (7.69). At 36 months, the mean (SD) erosion score was 3.73 (7.31) with 50.4 % (65) of the patients showing erosions, whereas the mean (SD) JNS score was 9.96 (7.56) with 96.8 % (125) of the patients displaying JSN; the mean SvdH (SD) total score was 13.69 (12.84) with 3.2 % of the patients showing either erosions or JSN.
Overall, radiographic progression was observed in 62.7 % (81) of the patients. Baseline variables did not differ between the progression group and the non-progression group, except for higher ESR levels (32.4 (±14.2) vs 25.35 (±13.9) p = 0.006), presence of erosions (39.5 % vs 28.5 % p = 0.04) and SvdH total score (SD) (9(±8.6) vs. 5.8(±5.3) p = 0.02) in the first set of radiographs. These data are depicted in Table 3.
At end of follow-up, patients who had progressed had higher DAS28 than those without progression (p = 0.04) but similar patient-reported outcomes. Also, patients in remission had lower SvdH total score (8.4(±6.7) vs. 16.3(±14.3) p = <0.0001) and lower presence of erosions (34.8 % vs. 58.1 % p = 0.0003) than patients with active disease.
Erosive disease was more frequent in patients with positive aCCP (80 % vs. 59.3 % p = 0.01), positive RF (80 % vs. 60.9 % p = 0.02) and positive ANAs (39.4 % vs. 21.8 % p = 0.04). At study entry, mean disease duration was shorter for patients with erosive disease (4.35 months (±3, 1) vs 5.48 months (±3,2) p = 0.04) than for those with non erosive disease. Likewise, it was found that patients with high SvdH total score in the first set of X-rays were more likely to have long-term erosions (10.7 (±9.2) vs 4.8 (±4.0) p = <0.0001). Among genetic factors evaluated, presence of HLA-DRB1 SE was significantly more frequent in patients who had erosions (61.5 % vs 37.5 % p = 0.01) (Table 3).
Of those patients without erosions at baseline, 56.3 % (49) had progressed; of those with erosions at baseline, 76.1 % (32) had progressed. The difference between these two groups was significant (p = 0.04). Regarding the therapeutic strategy, there was no statistically significant difference in treatment prescribed between the erosive vs non-erosive and progression vs. non-progression patients.
Stepwise multiple logistic regression
Table 4 shows the baseline parameters identified by the multiple logistic regression model that were independently predictive of the presence of remission, radiographic progression, and incident erosive disease at 3 years.
Baseline SvdH total score was the only predictive factor associated with the three outcomes evaluated. Absence of aCCP, RF and ANAs, and lower HAQ-DI were predictive of remission at 3 years. Higher levels of ESR and presence of erosions at entry were predictive of radiographic progression. Independent baseline predictors of incident erosive disease were anti-CCP and RF positivity, symptom duration at baseline >3 months, and presence of HLA-DRB1 SE.
Discussion
The goal of this study was to find predictors of remission, radiographic progression, and erosive disease in a cohort of Colombian patients with EORA that followed a therapeutic protocol aiming at remission, in a real world tight-control setting. We tested the most of the clinical, biological, immunological, and genetic factors previously reported as possible prognostic factors in rheumatoid arthritis.
In spite of an overall reduction in disease activity over the 36 months with traditional DMARDs therapy in this cohort, only a third of patients reached complete disease remission. Even though our findings are not dissimilar to those reported in a French cohort [14] and a Austrian cohort [15] in whom 25.1 and 29 % of patients, respectively, achieved a remission state at 36 months with traditional DMARDs treatment, the poor response rate in our patients is, at least in part, reflective of a particularly aggressive disease, as demonstrated by the high index of disease activity (DAS28 mean 6.73, SJC mean 20.69 and TJC mean 21.84) and radiographic damage at baseline. The majority of patients exhibited structural damage in their X-rays at study entry (29 % erosions and 93 % JSN). To our knowledge, this is the cohort of RA patients with the higher scores of disease activity at baseline that has been published.
In this study, disease remission defined as DAS28 <2.6 at end of follow-up was more likely to occur in patients with less radiographic damage, in those who were RF, aCCP, and ANAs negative, and in those with a lower HAQ-DI at baseline. We found no association of other clinical markers of disease activity with remission. Previous prospective studies in patients treated with conventional therapy have reported diverse baseline predictive factors for remission. These include negativity of autoantibodies (aCCP and RF), low baseline HAQ-DI, and absence of radiographic damage, similar to the findings in this study [14, 16, 17]. Some other studies have found male sex, swollen and/or tender joints at baseline to have influence on clinical course, and disease remission [18, 19]. Fatigue severity at study entry was associated to lower probability of remission. We did not find other studies reporting this prevalent and disabling symptom as a predictive factor for remission. This could be related to lack of regular evaluation in RA cohorts.
Studies of radiographic progression in patients with RA have shown diverging results. Several important factors should be considered when interpreting those results, such as patient selection, disease duration at inclusion, the number of radiographic examinations performed in each patient during the study, the order in which the radiographs were evaluated, and the scoring method used. In our study, a high rate of radiographic progression (62.7 %) was observed. Similar findings have been reported previously [15, 20–25], showing that early introduction of a therapeutic strategy with DMARDs in EORA improves clinical and biological parameters of disease activity, but does not prevent radiographic progression in a significant proportion of patients.
The current study identified several factors associated with radiographic progression. High levels of ESR, presence of erosions, and SvdH total score elevated at baseline were found to be predictive. Clinical markers of disease activity were not found to be predictors of radiographic damage. The findings on the association between the ESR level and radiographic progression are in agreement with those observed in the prospective study by Lindqvist et al. [26], which found that ESR at the study start was the best predictor for radiographic progressive disease in early RA. Similarly, in a 19-year study, Wolfe and Sharp [27] found that 55 % of the variance in radiographic progression scores was explained by the ESR, concluding that acute-phase reactants are the strongest determinants of progression.
In our population, 50.4 % had erosive arthritis after 3 years. This appears similar when compared with the observation of other series that assessed patients for the same period [14, 15]. Serological factors at baseline (aCCP and RF) were predictors of incident erosive disease. The results are consistent with previous studies which have shown positive associations between autoantibodies and radiologic damage [15, 20–25, 28, 29]. Importantly, clinical features as joint counts, HAQ-DI, VAS ratings as well as acute phase reactants did not differ at baseline, nor was the appearance of erosions predictable by these clinical and laboratory criteria.
The influence of RA-associated HLA-DRB1 alleles is controversial. Molenaar et al. [30], like us, found no association between remission and HLA-DRB1 alleles in 167 patients. Similarly, Gossec et al. [14] found that the presence of SE had no impact on remission rates in 191 early RA patients. Other workers found the opposite [31, 32]. Regarding the effect of the SE on the radiological damage, there is greater consensus. Most studies including patients of european ancestry show an association between SE and erosive disease [25, 31–36]. In Colombian RA patients, Rojas-Villarraga et al. [37] found that HLA-DRB1 SE and aCCP influence time at appearance of substantial joint damage. We confirm the effect of HLA-DRB1 SE on incident erosive disease in our population.
An additional and important prognostic factor for incident erosive disease in the current study was symptom duration before study inclusion. 27.6 % of erosive patients had <3-month symptoms at presentation, compared with 46.8 % in non-erosive patients. This confirms the importance of early referral and treatment for achieving the best possible outcome in RA, as reported in studies focused on patients with very early rheumatoid arthritis [38, 39].
Interestingly, we did not find an influence of TNF (SNP)-308 in our cohort. Although this conclusion should be taken with caution because of the relatively small number of patients analyzed to find differences between three genotypes (A/A, G/A, G/G), it is in line with other recent observations [34, 40, 41].
The potential role of DMARDs treatment was not the focus in our cohort. However, clinical and radiological status was shown to be similar after 36 months of treatment with both MTX monotherapy or in combination with antimalarials or SSZ, making it unlikely that different drug regimens could have induced different remission rates in our study.
The most important finding of this study was that joint damage occurred early in the course of RA becoming the harbinger of further damage in these patients. Baseline SvdH score was the only predictive factor associated with the three outcomes evaluated (disease remission, radiographic progression, and incident erosive disease) at 36-month follow-up. Multiple studies have highlighted the importance of baseline radiological compromise as a predictor for future joint damage [14, 42, 43]. Notably, although previous data have suggested that joint erosions are more prevalent than joint space narrowing in EORA, as well as in advanced RA [44, 45], in this Colombian RA cohort, we found the opposite, i.e., higher rate of JSN than joint erosions, even from the onset of disease.
Besides disease remission, autoantibodies (aCCP and RF) at baseline were predictive of erosive disease but not of radiographic progression. This could be explained by the fact that radiographic progression take into account changes in SvdH total score, which includes both erosions and JSN, two processes that have been considered as partly independent of each other [44].
Study limitations included a relatively small sample size, so weak associations between outcomes and baseline factors may not have been detected. Thirty patients dropped out during follow-up and were not included in the final statistical analysis; however, at baseline, the data for those patients were not substantially different of those included. We examined a relatively short period of time considering that RA may last for decades. Disease remission was assessed in a transversal way and not as a period of sustained clinical remission, which could better reflect the disease activity.
In conclusion, this prospective study reports, for the first time in Colombia, a large amount of information concerning the profile and the course of EORA. Our data provide a useful benchmark to compare disease patterns among different populations and emphasize the importance of assessing X-rays and autoantibodies at baseline, since these factors may be used to predict a more aggressive disease and guide therapeutic interventions.
References
Pincus T, Callahan LF, Sale WG et al (1984) Severe functional declines, work disability, and increased mortality in seventy-five rheumatoid arthritis patients studied over nine years. Arthritis Rheum 27:864
Yelin E, Wanke LA (1999) An assessment of the annual and long-term direct costs of rheumatoid arthritis: the impact of poor function and functional decline. Arthritis Rheum 42:1209–1218
Boers M, Verhoeven AC, Markusse HM et al (1997) Randomised comparison of combined step-down prednisolone, methotrexate and sulphasalazine with sulphasalazine alone in early rheumatoid arthritis. Lancet 350:309–18
Mottonen T, Hannonen P, Korpela M et al (2002) Delay to institution of therapy and induction of remission using single-drug or combination-disease-modifying antirheumatic drug therapy in early rheumatoid arthritis. Arthritis Rheum 46:894–898
St. Clair EW, van der Heijde DMFM, Smolen JS et al (2004) Combination of infliximab and methotrexate therapy for early rheumatoid arthritis: a randomized, controlled trial. Arthritis Rheum 50:3432–43
Goekoop-Ruiterman YPM, de Vries-Bouwstra JK, Allaart CF et al (2005) Clinical and radiographic outcomes of four different treatment strategies in patients with early rheumatoid arthritis (the BeSt study): a randomized, controlled trial. Arthritis Rheum 52:3381–90
Breedveld FC, Weisman MH, Kavanaugh AF et al (2006) The PREMIER study: a multicenter, randomized, double-blind clinical trial of combination therapy with adalimumab plus methotrexate versus methotrexate alone or adalimumab alone in patients with early, aggressive rheumatoid arthritis who had not had previous methotrexate treatment. Arthritis Rheum 54:26–37
Goekoop-Ruiterman YPM, de Vries-Bouwstra JK, Allaart CF et al (2007) Comparison of treatment strategies in early rheumatoid arthritis: a randomized trial. Ann Intern Med 146:406–15
Machold KP, Stamm TA, Eberl GJ et al (2002) Very recent onset arthritis - clinical, laboratory, and radiological findings during the first year of disease. J Rheumatol 29:2278
MacGregor AJ, Snieder H, Rigby AS, Koskenvuo M, Kaprio J, Aho K et al (2000) Characterizing the quantitative genetic contribution to rheumatoid arthritis using data from twins. Arthritis Rheum 43:30–7
Lee YH, Ji JD, Song GG (2007) Tumor necrosis factor-alpha promoter −308 A/G polymorphism and rheumatoid arthritis susceptibility: a metaanalysis. J Rheumatol 1:43–9
Syversen SW, Goll GL, van der Heijde D, Landewe R, Gaarder PI, Odegard S et al (2009) Cartilage and bone biomarkers in rheumatoid arthritis: prediction of 10-year radiographic progression. J Rheumatol 36:266–272
Bruynesteyn K, van der Heijde D, Boers M, Saudan A, Peloso P, Paulus H et al (2002) Determination of the minimal clinically important difference in rheumatoid arthritis joint damage of the Sharp/van der Heijde and Larsen/Scott scoring methods by clinical experts and comparison with the smallest detectable difference. Arthritis Rheum 46:913–920
Gossec L, Dougados M, Goupille P, Cantagrel A, Sibilia J, Meyer O et al (2004) Prognostic factors for remission in early rheumatoid arthritis: a multiparameter prospective study. Ann Rheum Dis 63:675–80
Machold KP, Stamm TA, Nell VP, Pflugbeil S, Aletaha D et al (2007) Very recent onset rheumatoid arthritis: clinical and serological patient characteristics associated with radiographic progression over the first years of disease. Rheumatology (Oxford) 46:342–9
Eberhardt K, Fex E (1998) Clinical course and remission rate in patients with early rheumatoid arthritis: relationship to outcome after 5 years. Br J Rheumatol 37:1324–9
van der Woude D, Young A, Jayakumar K, Mertens BJ, Toes RE, van der Heijde D et al (2009) Prevalence of and predictive factors for sustained disease-modifying antirheumatic drug-free remission in rheumatoid arthritis: results from two large early arthritis cohorts. Arthritis Rheum 60:2262–71
Forslind K, Hafstrom I, Ahlmen M, Svensson B (2007) For the BARFOT study group. Sex: a major predictor of remission in early rheumatoid arthritis? Ann Rheum Dis 66:46–52
Jayakumar K, Norton S, Dixey J, James D, Gough A, Williams P et al (2012) Early Rheumatoid Arthritis Study (ERAS). Sustained clinical remission in rheumatoid arthritis: prevalence and prognostic factors in an inception cohort of patients treated with conventional DMARDS. Rheumatology (Oxford) 51:169–75
Kroot E-J, de Jong BA, van Leeuwen MA, Swinkels H, van den Hoogen FH, van’t Hof M et al (2000) The prognostic value of anti-cyclic citrullinated peptide antibody in patients with recent onset rheumatoid arthritis. Arthritis Rheum 43:1831–1835
Kastbom A, Strandberg G, Lindroos A, Skogh T (2004) Anti-CCP antibody test predicts the disease course during 3 years in early rheumatoid arthritis (the Swedish TIRA project). Ann Rheum Dis 63:1085–1089
Brennan P, Harrison B, Barrett E, Chakravarty K, Scott D, Silman A et al (1996) A simple algorithm to predict the development of radiological erosions in patients with early rheumatoid arthritis: prospective cohort study. BMJ 24:471–476
Jansen MA, van der Horst-Bruinsma IE, van Schaardenburg D, Bezemer PD, Dijkmans BA (2001) Predictors of radiographic joint damage in patients with early rheumatoid arthritis. Ann Rheum Dis 60:924–927
Combe B, Dougados M, Goupille P, Cantagrel A, Eliaou JF, Sibilia J et al (2001) Prognostic factors for radiographic damage in early rheumatoid arthritis. A multiparameter prospective study. Arthritis Rheum 44:1736–1743
Sanmartí R, Gómez-Centeno A, Ercilla G, Larrosa M, Viñas O, Vazquez I et al (2007) Prognostic factors of radiographic progression in early rheumatoid arthritis: a two year prospective study after a structured therapeutic strategy using DMARDs and very low doses of glucocorticoids. Clin Rheumatol 26:1111–8
Lindqvist E, Jonsson K, Saxne T, Eberhardt K (2003) Course of radiographic damage over 10 years in a cohort with early rheumatoid arthritis. Ann Rheum Dis 62:611–6
Wolfe F, Sharp JT (1998) Radiographic outcome of recent-onset rheumatoid arthritis: a 19-year study of radiographic progression. Arthritis Rheum 41:1571–82
Contreras-Yáñez I, Rull-Gabayet M, Vázquez-Lamadrid J, Pascual-Ramos V (2011) Radiographic outcome in Hispanic early rheumatoid arthritis patients treated with conventional disease modifying anti-rheumatic drugs. Eur J Radiol 79:e52–7
Rönnelid J, Wick MC, Lampa J, Lindblad S, Nordmark B, Klareskog L et al (2005) Longitudinal analysis of citrullinated protein/peptide antibodies (anti-CP) during 5 year follow up in early rheumatoid arthritis: anti-CP status predicts worse disease activity and greater radiological progression. Ann Rheum Dis 64:1744–9
Molenaar ET, Voskuyl AE, van der Horst-Bruinsma IE, Schreuder GM, Zanelli E, Dijkmans BA (2002) Influence of HLA polymorphism on persistent remission in rheumatoid arthritis. Ann Rheum Dis 61:351–3
Gough A, Faint J, Salmon M, Hassell A, Wordsworth P, Pilling D et al (1994) Genetic typing of patients with inflammatory arthritis at presentation can be used to predict outcome. Arthritis Rheum 37:1166–70
van Zeben D, Hazes JMW, Zwinderman AH, Cats A, Schreuder GM, D’Amoro J et al (1991) Association of HLA-DR4 with a more progressive disease course in patients with rheumatoid arthritis. Arthritis Rheum 34:822–30
Gorman JD, Lum RF, Chen JJ, Suarez-Almazor ME, Thomson G, Criswell LA (2004) Impact of shared epitope genotype and ethnicity on erosive disease: a meta-analysis of 3,240 rheumatoid arthritis patients. Arthritis Rheum 50:400–12
Reneses S, González-Escribano MF, Fernández-Suárez A, Pestana L, Davila B, Wichmann I et al (2009) The value of HLA-DRB1 shared epitope, −308 tumor necrosis factor-alpha gene promoter polymorphism, rheumatoid factor, anti-citrullinated peptide antibodies, and early erosions for predicting radiological outcome in recent-onset rheumatoid arthritis. J Rheumatol 36:1143–9
Karlson EW, Chibnik LB, Cui J, Plenge RM, Glass RJ, Maher NE et al (2008) Associations between human leukocyte antigen, PTPN22, CTLA4 genotypes and rheumatoid arthritis phenotypes of autoantibody status, age at diagnosis and erosions in a large cohort study. Ann Rheum Dis 67:358–63
Janssens AC, Steyerberg EW, Jiang Y, Habbema JD, Van Duijn CM, Criswell LA (2006) Value of the HLA-DRB1 shared epitope for predicting radiographic damage in rheumatoid arthritis depends on the individual patient risk profile. J Rheumatol 33:2383–9
Rojas-Villarraga A, Diaz FJ, Calvo-Páramo E, Salazar JC, Iglesias-Gamarra A, Mantilla RD et al (2009) Familial disease, the HLA-DRB1 shared epitope and anti-CCP antibodies influence time at appearance of substantial joint damage in rheumatoid arthritis. J Autoimmun 32:64–9
Bosello S, Fedele AL, Peluso G, Gremese E, Tolusso B, Ferraccioli G (2011) Very early rheumatoid arthritis is the major predictor of major outcomes: clinical ACR remission and radiographic non-progression. Ann Rheum Dis 70:1292–5
Gremese E, Salaffi F, Bosello SL, Ciapetti A, Bobbio-Pallavicini F, Caporali R et al (2013) Very early rheumatoid arthritis as a predictor of remission: a multicentre real life prospective study. Ann Rheum Dis 72:858–62
Pavy S, Toonen EJ, Miceli-Richard C, Barrera P, van Riel PL, Criswell LA et al (2010) Tumour necrosis factor alpha -308G- > A polymorphism is not associated with response to TNFalpha blockers in Caucasian patients with rheumatoid arthritis: systematic review and meta-analysis. Ann Rheum Dis 69:1022–8
Aranda F, Perés Wingeyer SD, Schneeberger E, Valerio M, Saint Martin E, Dal Pra F, et al. (2014) The −308 G/A polymorphism in the tumor necrosis factor-α gene is not associated with development and progression of rheumatoid arthritis in Argentinean patients. Int J Rheum Dis. doi: 10.1111/1756-185X.12343.
Bridges SL Jr, Causey ZL, Burgos PI, Huynh BQ, Hughes LB, Danila MI et al (2010) Radiographic severity of rheumatoid arthritis in African Americans: results from a multicenter observational study. Arthritis Care Res (Hoboken) 62:624–31
van Nies JA, van Steenbergen HW, Krabben A, Stomp W, Huizinga TW, Reijnierse M et al (2015) Evaluating processes underlying the predictive value of baseline erosions for future radiological damage in early rheumatoid arthritis. Ann Rheum Dis 74(5):883–9
Smolen JS, van der Heijde DM, Aletaha D, Xu S, Han J, Baker D et al (2009) Progression of radiographic joint damage in rheumatoid arthritis: independence of erosions and joint space narrowing. Ann Rheum Dis 68:1535–40
Landewé R, Smolen JS, Florentinus S, Chen S, Guérette B, van der Heijde D (2015) Existing joint erosions increase the risk of joint space narrowing independently of clinical synovitis in patients with early rheumatoid arthritis. Arthritis Res Ther 17:133
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
This study was conducted in accordance with the Declaration of Helsinki for the protection of human subjects in research. All patients gave their informed consent to enter into the study, which was approved by our Ethics Institutional Committee.
Disclosures
None.
Rights and permissions
About this article
Cite this article
Quintana-Duque, M., Rondon-Herrera, F., Mantilla, R. et al. Predictors of remission, erosive disease and radiographic progression in a Colombian cohort of early onset rheumatoid arthritis: a 3-year follow-up study. Clin Rheumatol 35, 1463–1473 (2016). https://doi.org/10.1007/s10067-016-3246-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-016-3246-5