Abstract
We aim to study the educational impact of a clinical anatomy workshop in 1st-year orthopedic and rheumatology fellows. First-year rheumatology fellows (N = 17) and a convenience sample of 1st-year orthopedic fellows (N = 14) from Mexico City in the 9th month of training participated in the study. The pre- and the post- workshop tests included the same 20 questions that had to be answered by identification or demonstration of relevant anatomical items. The questions, arranged by anatomical regions, were asked in five dynamic stations. Overall, the 31 participants showed an increase of correct answers, from a median of 6 (range 1 to 12) in the pre-workshop test, to a median of 14 (range 7 to 19) in the post-workshop test. In the pre-workshop test, the correct median answers were 7 (range 2 to 12) in the orthopedic fellows and 5 (range 1 to 10) in the rheumatology fellows (p = 0.297). Corresponding scores in the post-workshop were 15 (range 10 to 19) and 12 (range 7 to 18) (p = 0.026) showing a significant difference favoring the orthopedic group. Our clinical anatomy workshop was efficacious, in the short term, as a teaching instrument for 1st-year orthopedic and rheumatology fellows. The post-workshop scores, although significantly improved in both groups, particularly in the orthopedic fellows, were still suboptimal. Further refinements of our workshop might yield better results.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Clinical anatomy is the anatomy that is useful in the care of patients [1, 2]. Within the field of clinical anatomy, superficial structures of the limbs including joints, muscles, tendons, and nerves lend themselves naturally to the use of the clinician’s classic senses of sight and touch. Clinicians have the ability to palpate many of the body’s well-known superficial arteries such as the radial or carotid artery. Similarly, the identification of superficial anatomical items such as a muscle origin, belly, and insertion need no further validation when performed by one who has mastered this discipline. Examples include muscles such as brachioradialis in the forearm and tensor fascia lata at the lateral hip region. Palpable bone eminences such as the radial styloid and the lateral tubercle (Gerdy) of the tibia and fat bodies such as Hoffa fat pad in the knee and Kager fat in the ankle are hard to miss. Ligaments such as the lateral and tibial collateral ligaments of the knee, and the spring ligament at the ankle, may be identified by a skilled physician. Finally, superficial nerves such as the ulnar at the elbow, the radial in the upper arm, and the common peroneal should be explored by the clinician in the appropriate circumstances. It is our belief that clinical anatomy is a cornerstone in the diagnosis of most rheumatic diseases and critical to the proper and cost effective diagnosis of the regional pain syndromes. These conditions fall within the realm of multiple specialists who see musculoskeletal conditions whether an orthopedist, a rheumatologist, a physiatrist, as well as a generalist. Unfortunately, the undergraduate teaching of anatomy has decayed over time, and a need for improvement has been voiced [3].
The literature has consistently demonstrated inadequate knowledge of clinical anatomy at the graduate and post-graduate levels [4–6]. Indeed, we have previously found that rheumatology trainees and practicing rheumatologists in seven American countries performed sub-optimally in a pre-workshop test of baseline anatomic identification or demonstration [7].
The current study represents an extension of our initial study to include a parallel investigation in orthopedic trainees as representative of another discipline involved in the care of patients with musculoskeletal conditions. Our decision to include orthopedic trainees was based on the paradigm that anatomic knowledge is central to competence in patient assessment in office orthopedics as well as in orthopedic procedures.
Our primary goal was to study the impact of our clinical anatomy workshop on the learning of clinical anatomy among both rheumatology and orthopedic trainees. Also, this study allowed us to analyze and compare the pre- and post-workshop practical knowledge of clinical anatomy between both groups.
Material and methods
Participants and recruitment method
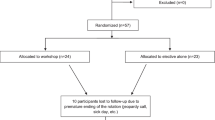
Rheumatology fellows were recruited through personal invitation after approval of the directors of all ten rheumatology training programs in Mexico City (footnote). Of the twenty rheumatology fellows invited, 17 agreed to participate in the study. From the 12 orthopedic training programs in Mexico City, a geographical convenience cohort of residents from four hospitals was chosen. Residents were invited to participate after approval by their respective program directors. Of the 15 orthopedic residents invited, 14 agreed to participate in the study. None of the participating fellows had undergone musculoskeletal ultrasonography training.
Evaluation tool
The anatomical knowledge evaluation tool consisted of a series of questions in which fellows were asked to identify or demonstrate the action of key anatomical items in the examiners’ or their bodies. The questions included most of the items used in our previous publications [7, 8]. However, they were selected from a new item list that was compiled to develop an evaluation tool for a workshop held at the 2014 PANLAR meeting in Punta del Este, Uruguay. The procedure was as follows: three members of our group (JJC, RAK, PVO) compiled a list of 112 anatomical items felt relevant to the regional pain syndromes. These included 24 hand/wrist items, 12 elbow items, 14 shoulder items, 10 neck items, 10 spine items, 8 hip/thigh items, 14 knee items, and 20 ankle/foot items. These items were independently ranked according to their clinical relevance and degree of difficulty. The 50 highest ranked questions were chosen for the pre- and post-seminar Punta del Este examinations (unpublished data). For the present study, from this pool of 50 questions, 5 were excluded because they referred to the spine. Of the 45 remaining questions, 2 were removed because all participants in the workshop answered them correctly, and 3 were removed because all answered them incorrectly, leaving a pool of 40 questions of intermediate difficulty. Of these, 20 questions were randomly chosen to be used in the current pre- and post-workshop examinations. Table 1 shows the anatomical items surveyed, the wording of the questions, and the relevance of each of the chosen anatomical items to the fields of orthopedics and rheumatology. Participants rotated through five different dynamic stations, and in each station four questions were asked. The same examiners (AV, KCG, PVO/JENZ, JJC, CHD) asked the pre- and post-workshop questions.
Instructors
The instructors are members of the Mexican Group of Clinical Anatomy (GMAC) since 2009. They are all board-certified in rheumatology, and three had one or more years of MSK ultrasonography training. GMAC’s experience included at the time of this study 32 similar workshops held in 8 American countries and Spain.
Clinical anatomy workshop
The methodology of this workshop has been published [9–14]. The workshop uses clinical vignettes that highlight the involvement of key anatomical items. Following each vignette, the highlighted item is shown diagramatically, and its relation to the discussed condition is reviewed. After several vignettes that relate to the same anatomical region, the practical part of the workshop takes place. This includes the identification and demonstration of the highlighted items in the instructors and participants’ bodies. Since each participant identifies each item in the bodies of 5 or 6 peers plus the instructor, the important issue of anatomical variation is understood. By experience, this teaching system requires an instructor to participant ratio of one to 6–10 per group. Thus, since we had 31 participants in the current study, there were 6 participants per instructor in the practical portions of the workshop. The current workshop consisted of five modules that were presented in sequence, hand/wrist, elbow/shoulder, hip, knee, and ankle/foot. The total duration of this seminar was 7 h including 30 min for lunch and was preceded and followed by a 75-min practical examination.
Institutional review board
The protocol was approved by the institutional review boards of the American British Cowdray Medical Center and the Hospital de Especialidades Dr. Antonio Fraga Mouret, Centro Medico Nacional La Raza, Instituto Mexicano del Seguro Social. All participants signed an informed consent that described the protocol. The examiners were not blinded as to the identity of the workshop participants; however, anonymity was achieved in the interpretation of the results through de-identification of the score sheets.
Statistical analysis
The sample size was calculated to detect a 30 % difference between the pre- and post-workshop tests with a power of 80 % and a two-tail α of 0.05 %. A minimum of 12 participants per subspecialty was required. Age of participants is shown as mean and standard deviation and answers to the individual questions as means and percentages. Overall results are expressed as median and range. Overall and intragroup correct answers in the pre and post-workshop evaluations were compared with the Wilcoxon test. Pre- and post-workshop scores of one subspecialty versus the other were compared with the Mann-Whitney U test. Intergroup percentages of correct answers per anatomical item, comparing the pre- and post-workshop evaluations was done with the chi-square test. Differences with a p < 0.05 was considered statistically significant. All data were processed using the SPSS statistical package (Chicago, Il.) version 20.0.
Results
There were 31 participants in the study, 17 rheumatology fellows and 14 orthopedic fellows, all of them in the 9th month of their 1st year of training. Age and sex of the participants are shown in Table 2. Gender of participants differed in the two groups, reflecting a female predominance in rheumatology trainees and a male predominance in orthopedic trainees. This table also shows the pre- and post-workshop test scores, according to the subspecialty. Orthopedic fellows had significantly greater pre- and post-workshop scores than rheumatology fellows.
Pre- and post-workshop scores
As shown in Table 3, all post-workshop scores showed an improvement that reached statistical significance. In the entire group (N = 31), a median of 6 of 20 questions (range 1 to 12) were responded to correctly prior to the workshop and 14 (range 7 to 19) in the post-workshop assessment. Orthopedic fellows responded correctly to 7 of 20 questions (range to 2–12) prior to the workshop and 15 (range 10 to 19) in the post-workshop assessment. Rheumatology fellows responded correctly to 5 of 20 questions (range 1 to 10) prior to the workshop and 12 (range 7 to 18) in the post-workshop assessment. Finally, overall results, broken down to upper and lower extremity items, also showed a significant gain (Table 3).
Intergroup comparisons per anatomical item
The correct answers per individual anatomical item comparing the subspecialties in the pre-test and the post-test are shown in Table 4. In the pre-workshop test, orthopedic fellows scored significantly higher than rheumatology fellows in questions 11 (piriformis muscle), 19 (opening of sinus tarsi), and 20 (base of the 5th metatarsal). In the post-workshop test, question 18 (tibial nerve at the ankle) was scored significantly higher by the orthopedic fellows, question 20 remained unchanged, and questions 11 and 19 changed to a non-significant difference. For the remaining 16 questions, the lack of statistical significance between specialties in the pre-test was paralleled in the post-test. On the other hand, comparing the pre- and post-test scores for the entire group (N = 31), there was a significant difference in the percentage of correct answers in 13 of the 20 questions (65 %) (Table 5). Only 5 of the 20 questions were answered correctly by more than 50 % of the 31 fellows in the pre-test, as compared with 16 in post-test. As expected, the items that scored lowest in pre-test where those that increased most in the post-test.
Discussion
Our results indicate that both orthopedic and rheumatology fellows increased their ability to correctly identify key anatomic structures and functions. Out of a total of 20 questions, the median of correct answers increased from 7 to 15 among the orthopedic fellows and from 5 to 12 among the rheumatology fellows. When the two groups were compared, pre-workshop scores tended to be higher in the orthopedic group and post-workshop scores were significantly higher in the orthopedic group. However, it was disappointing that in the pre-workshop test, the orthopedic fellows answered correctly only 35 % of the questions, and the rheumatology fellows, 25 %. The beneficial effect of the workshop was shown by a significant knowledge gain in both fellows groups. In the post-workshop test, the orthopedic group answered correctly 75 vs. 60 % in the rheumatology group. We consider the pre-workshop results dismal and the post-workshop results suboptimal. In reviewing the participating rheumatology programs, only one has a formal clinical anatomy course. The three 1st-year fellows in this program had a median pre-workshop score of 8 (range 5 to 9) compared with 5 (range 1 to 10) for the entire group. Their median post-workshop score was 18 (range 16 to 18) compared with 12 (range 7 to 18) for the entire group. Although these findings are encouraging, the small sample size did not allow us to draw valid comparisons.
We have previously shown similar pre-workshop clinical anatomy knowledge in rheumatology fellows and rheumatologists from seven American countries. In this study, there were 170 participants, 84 of them rheumatology fellows, from Argentina, Chile, Ecuador, El Salvador, Mexico, Uruguay, and the USA. Fellows achieved higher scores than practicing rheumatologists [7]. In this study, time limitations precluded us from assessing the short-term efficacy of the workshop in the majority of sites. In one country, however, conducive conditions allowed us to include a post-workshop test, which showed a score increase from 37.6 ± 15.6 to 78.2 ± 15.5 % in the post-workshop test. These figures are higher than in the present study. However, in this country, the seminar extended to 3.5 days, as compared to 6.5 h in the present study. As suggested by Evangelisto et al. [15], subsequent analysis of our data showed that the highest pre-workshop scores, 60.7 ± 14.2 and 67 ± 16.1 %, were attained by fellows from programs that included musculoskeletal ultrasonography (MSU) as a teaching tool. The usefulness of adding ultrasonography to courses of musculoskeletal clinical anatomy has recently been discussed [16].
The surveyed items in our previous and present studies are basic to an understanding of the regional musculoskeletal pain syndromes. These conditions are not only frequent in the population at large [17] but also comprise approximately 20 % of the patients seen by rheumatologists in their offices [18]. Generalists, rheumatologists, orthopedic surgeons, and physiatrists share the care of these patients and proficiency in patient assessment become critical to achieving a common standard of care. Therefore, we feel it is of utmost importance that trainees in both primary care as well within the specialties in which musculoskeletal assessment is a primary mandate achieve a higher level of competency in clinical anatomy than what we and others are finding.
In the current study, we attempted to evaluate the efficacy of our workshop in two different groups of participants, all from Mexico City. One group included 1st-year rheumatology fellows and the other, orthopedic fellows, all in the 9th month of their 1st-year training. The design of the study allowed us to compare, as a secondary goal, the scores of both groups of fellows prior to, and immediately after the seminar. To the best of our knowledge, there are no published data comparing the proficiency in clinical anatomy between orthopedic and rheumatology fellows. Thus, the current study represents not only an initial attempt to evaluate these fellows, but more importantly, to determine opportunities for improvement in orthopedic, and rheumatology training.
There are several weaknesses in our study. One is the limited number of orthopedic residents evaluated. The reason was the logistical difficulty in assembling a larger sample. However, of the 15 invited orthopedic fellows, only one did not participate. A second limitation was the immediacy of the post-workshop test. Although the protocol design includes an assessment at 1 year, this is a tenuous possibility in Mexico City because of expected difficulties in re-assembling the group, particularly the orthopedic fellows given their multiple rotations and research time. Nevertheless, we have indirect evidence from a competence survey obtained in our previous study, which indicates a positive impact of our seminar 1 to 3 months after it took place [8]. Additional efforts to determine the persistence of the acquired knowledge, and whether an increased knowledge of clinical anatomy translates into an improved delivery of rheumatology and orthopedic care, are warranted. A further limitation is the relatively short duration of the workshop for the large number of items included. Counteracting this weakness, is the practical and fun nature of our workshop, based on the cross-examination of participants and instructors, which we hope helps the retention process. Our positive results contrast with a recent study in medical students in which a lecture-enhanced musculoskeletal medicine course appeared to have a negative impact on the learning process [19]. A fourth limitation in our study is its pre-test/post-test nature. This is a weaker evidence than could be obtained, for instance, in a controlled trial. However, we still feel there is validity in demonstrating acquisition and retention of the ability to identify a taught anatomic identification, even if only in the short-term, with practical considerations of recruitment and scheduling of busy fellows precluding a true controlled study in our setting.
There are several strengths in our study. One was the painstaking process to select the questions. The selection process included a field test that led to the exclusion of those questions that were uniformly answered correctly and incorrectly by all participants. A second strength is that there were five dynamic stations, with four questions each. This method allowed a uniform wording of the questions and a uniform assessment of the answers with a single examiner able to assess each participant.
The task of better educating our trainees in the area of clinical anatomy is a challenge but one that could be achievable with a well-designed curriculum that could be disseminated through the literature or professional organizations. We could envision for example a course in which trainees are provided a review of anatomic structures in advance and then participate in an all day practical workshop such as ours followed by a post-test for reinforcement and a structured OSCE on real or standardized patients months later. Variations and enhancements would be possible to the workshop that could be program specific including a musculoskeletal ultrasound or fresh cadaver component [20]. Alternatively, the workshop could be structured in smaller segments that could be implemented on a weekly basis over a longer period of time if that would better fit a particular program. Though it would take skilled and persistent coordination, as a next step, long-term outcomes could be assessed by randomizing clinical anatomy training among training programs, and then performing utilization studies based on procedures performed, quality measures including outcomes and patient satisfaction, and cost analysis. Medicare and insurance companies’ data could potentially be used in the comparison.
In conclusion, we have observed a short-term positive impact of our clinical anatomy workshop in both orthopedic and rheumatology fellows. There was a trend towards greater knowledge in orthopedic fellows that reached statistical significance in the post-workshop test. However, when the absolute number of correct answers is considered, ample room for improvement in both groups of fellows is apparent. We believe that a more substantial course of clinical anatomy, of several days duration or spread through the 1st year of training, practical in nature, and reinforced throughout all subsequent years of training should be useful in orthopedic and rheumatology training programs. The long-term impact of the workshop remains to be established. Whether or not an increased knowledge of clinical anatomy results in a better or less expensive patient care is unknown. Finally, whether expertise in clinical anatomy is useful not just in regional rheumatology, but also in systemic rheumatic disorders, beyond the regional pain syndromes, is another important question that remains to be answered [21].
References
Moore KL, Dalley AF, Agur AMR (2010) Clinically oriented anatomy, 6th edn. Wolters Kluger, Lippincott, Williams & Wilkins, Philadelphia, p vii
Kalish RA, Canoso JJ (2007) Clinical anatomy: an unmet agenda in rheumatology training. J Rheumatol 34:1208–1211
Swamy M, Venkatachalam S, McLachlan J (2014) A Delphi consensus study to identify current clinically most valuable orthopaedic anatomy components for teaching medical students. BMC Med Educ 14:230
Freedman KB, Bernstein J (1998) The adequacy of medical school education in musculoskeletal medicine. J Bone Joint Surg Am 80:1421–1427
Matzkin E, Smith EL, Freccero D, Richardson AB (2005) Adequacy of education in musculoskeletal medicine. J Bone Joint Surg Am 87:310–314
Bandinelli F, Bijlsma JW, Ramiro MS, Pia E, Goekoop-Ruiterman YP, Sivera F et al (2011) Rheumatology education in Europe: results of a survey of young rheumatologists. Clin Exp Rheumatol 29:843–845
Navarro-Zarza JE, Hernandez-Díaz C, Saavedra MA, Alvarez-Nemegyei J, Kalish RA, Canoso JJ, Villaseñor-Ovies P (2012) Pre-workshop knowledge of musculoskeletal anatomy of rheumatology fellows and rheumatologists of seven North, Central and South American countries. Arthritis Care Res 66:270–276
Saavedra MA, Navarro-Zarza JE, Alvarez-Nemegyei J, Canoso JJ, Kalish RA, Villaseñor-Ovies P, Hernández-Díaz C (2015) Self-perceived efficacy of a workshop on musculoskeletal clinical anatomy. Reumatol Clin 11:224–226
Kalish RA, Canoso JJ (2012) A clinical musculoskeletal anatomy seminar: development of the method. Reumatol Clin 8(Suppl 2):10–12
Vargas A, Chiapas-Gasca K, Hernández-Díaz C, Canoso JJ, Saavedra MA, Navarro-Zarza JE, Villaseñor-Ovies P, Kalish RA (2012) Clinical anatomy of the hand. Reumatol Clin 8(Suppl 2):25–32
Villaseñor-Ovies P, Vargas A, Chiapas-Gasca K, Canoso JJ, Hernández-Díaz C, Saavedra MA, Navarro-Zarza JE, Kalish RA (2012) Clinical anatomy of the elbow and shoulder. Reumatol Clin 8(Suppl 2):13–24
Navarro-Zarza JE, Villaseñor-Ovies P, Vargas A, Canoso JJ, Chiapas-Gasca K, Hernández-Díaz C, Saavedra MA, Kalish RA (2012) Clinical anatomy of the hip. Reumatol Clin 8(Suppl 2):33–83
Saavedra MA, Navarro-Zarza JE, Villaseñor-Ovies P, Canoso JJ, Vargas A, Chiapas-Gasca K, Hernández-Díaz C, Kalish RA (2012) Clinical anatomy of the knee. Reumatol Clin 8(Suppl 2):39–45
Hernández-Díaz C, Saavedra MA, Navarro-Zarza JE, Canoso JJ, Villaseñor-Ovies P, Vargas A, Kalish RA (2012) Clinical anatomy of the ankle and foot. Reumatol Clin 8(Suppl 2):46–52
Evangelisto AM, Nishio MJ, Higgs JB, Kissin EY, Kaeley GS (2014) Musculoskeletal ultrasound and anatomy: comment on the article by Navarro-Zarza et al. Arthritis Care Res 66:1432–1433
Torralba KD, Villaseñor-Ovies P, Evelyn CM, Koolaee RM, Kalish RA (2015) Teaching of clinical anatomy in rheumatology: a review of methodologies. Clin Rheumatol 34:1157–1163
Alvarez-Nemegyei J, Peláez-Ballestas I, Sanin LH, Cardiel MH, Ramirez-Angulo A, Goycochea-Robles MV (2011) Prevalence of musculoskeletal pain and rheumatic diseases in the southeastern region of Mexico. A COPCORD-based community survey. J Rheumatol Suppl 86:21–25
Alarcón-Segovia D, Ramos-Niembro F, González-Amaro RF (1983) One thousand private rheumatology patients in Mexico City. Arthritis Rheum 26:688–689
Weiss K, Curry E, Matzkin E (2015) Assessment of medical school musculoskeletal education. Am J Orthop (Belle Mead NJ) 44:E64–67
Bernstein S (2015) 2014 ACR/ARHP Annual Meeting: Medical Education Trends. The Rheumatologist February 1. http://www.the-rheumatologist.org/article/2014-acrarhp-annual-meeting-medical-education-trends/. Accesed 6 Sept 2015
Savvas S, Panush RS (2015) Should all rheumatologists study musculoskeletal anatomy? Clin Rheumatol 34:1153–1156
Acknowledgements
We thank the Department of Orthopedics of the ABC Medical Center, Mexico City, Mexico, for the logistical support that allowed us to conduct this research.
We also wish to thank the following program directors of Orthopedics and Rheumatology, Mexico City, Mexico, for encouraging their trainees to participate in our study:
Orthopedics: Dr. Sergio Abush-Torton, Centro Médico ABC; Dr. Diego de La Torre, Hospital Juárez de México; Dra. Dra. Josefina Molina-Méndez, Hospital General de México; Dr. Cesáreo Trueba, Hospital Español
Rheumatology: Dra. Leonor Barile-Fabris, Centro Médico Nacional Siglo XXI del IMSS; Dr. Rolando Espinosa-Morales, Instituto Nacional de Rehabilitación; Dra. Fedra Irazoque-Palazuelos, Centro Médico Nacional 20 de Noviembre del ISSSTE; Dr. Gustavo Lugo, Hospital Juárez de México; Dr. Manuel Martínez-Lavín, Instituto Nacional de Cardiología Ignacio Chávez; and Dra. Marina Rull, Instituto Nacional de Ciencias Médicas y Nutrición Salvador Zubirán.
Disclosures
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Saavedra, M.A., Villaseñor-Ovies, P., Harfush, L.A. et al. Educational impact of a clinical anatomy workshop on 1st-year orthopedic and rheumatology fellows in Mexico City. Clin Rheumatol 35, 1299–1306 (2016). https://doi.org/10.1007/s10067-015-3076-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-015-3076-x