Abstract
Despite the high diagnostic and prognostic performance in adult rheumatoid arthritis, the role of antibodies to cyclic citrullinated peptide (anti-CCP) in juvenile idiopathic arthritis (JIA) is controversial. Occurrence of anti-CCP was mainly seen in rheumatoid factor (RF)-positive polyarthritis patients. In the present study, our aim was to investigate the prevalence and significance of anti-CCP for subjects with JIA in our population. We evaluated anti-CCP reactivity in the sera of 70 patients with various subtypes of JIA in a prospective cohort study. Anti-CCP titres were correlated with the evolution of joint involvement and the presence of joint damage. Nine JIA patients were seropositive for anti-CCP with respect to the cut-off value of the test. In our cohort, 34 patients had a polyarticular joint disease, most of them being RF-negative (30/34, 88 %). All four RF-positive polyarthritis patients had high anti-CCP concentrations and an aggressive erosive disease. In the RF-negative JIA patients, anti-CCP reactivity was in lower titres but significantly associated with polyarticular joint involvement (p = 0.016) and also with the presence of joint damage (p < 0.001). Presence of anti-CCP, at both low and high concentration, was significantly associated with a more severe articular disease in our JIA patients. Investigating anti-CCP should clearly be taken into consideration even among patients with JIA subtypes other than RF-positive polyarthritis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Juvenile idiopathic arthritis (JIA), the most common chronic rheumatic disease in children, is an umbrella term comprising seven related disorders, according to the revised International League of Associations for Rheumatology (ILAR) classification system [1], all associated with persistent arthritis. Within these subgroups of JIA, the prognosis varies markedly. Despite appropriate treatment, some cases develop joint damage, a significant cause of short- and long-term disability. Therefore, it is essential to early identify these patients, preferably at the time of diagnosis. At this point, few early predictors for the disease long-term outcome are available for JIA patients [2].
One of the most important serological discoveries in rheumatology in recent years is the identification of rheumatoid arthritis (RA)-specific autoantibodies directed against different citrulline-containing peptides from the inflamed RA synovia [3]. Anti-cyclic citrullinated peptide antibodies (anti-CCP), present in human serum or plasma, were demonstrated to be 95–98 % specific, but moderately sensitive (48–70 %), for adult RA [4, 5]. They can be found early in the disease course of RA, even years before the onset of clinical symptoms, and they can predict erosive disease [6, 7].
Anti-CCP were also detected in children with JIA but with a lower prevalence than in RA (range between 2 [8, 9] to 24 % [10]) and mainly in rheumatoid factor (RF)-positive JIA patients. A great deal of evidence for the anti-CCP positivity in RF-positive JIA patients with erosive joint disease has been published so far [11–17]. These data may be explained by the fact that this specific form of JIA has pathogenic and prognostic common features with adult RA. But in the spectrum of JIA, this particular form of disease counts only for 2–7 % [18]. In the other JIA subsets, a much more heterogeneous population in terms of outcome and response to treatment, anti-CCP were rarely found by previous investigators [8, 10, 11, 15, 16]. However, to date, the role of anti-CCP reactivity in these patients remains unclear.
Importantly, few previous studies demonstrated significant correlations between anti-CCP and joint damage in JIA patients [8, 10, 11, 19, 20], which can be indicative of a possible role in predicting joint damage in this population. Additional studies are needed to assess this potential predictive role of anti-CCP, especially in RF-negative JIA patients. Therefore, the aim of our study was to investigate the prevalence and significance of anti-CCP for subjects with JIA in our population.
Patients and methods
This was a prospective cohort study, conducted in the 2nd Paediatric Clinic (Children’s Hospital at Cluj-Napoca, Romania) between January 2009 and July 2014. The study was performed in accordance with the Declaration of Helsinki and good clinical practice. A written informed consent has been obtained prior to their inclusion in the study as appropriate.
Patients
A total of 70 JIA Romanian patients were consecutively included in the study. Inclusion criteria were a confirmed diagnosis of JIA based on the revised ILAR criteria for JIA [1], a disease duration longer than 1 year in order to provide reliable outcome data and obtaining a parent informed consent for our study. The median duration of the disease at the sample collection was 2 years (range 1–15). Patients with other associated autoimmune diseases or intercurrent infectious diseases were excluded. All patients were submitted to complete clinical examination made by a paediatric rheumatologist, blood collection for laboratory investigations and joint damage assessment. Patient characteristics, the disease features and the use of medication were recorded for the study. The duration of follow-up ranged from 1 to 20 years with a median of 5 years [1 year in 3 (4.3 %) patients, 2 years in 5 (7.1 %) patients, 3 years in 6 (8.6 %) patients, 4 years in 12 (17.1 %) patients, 5 years in 12 (17.1 %) patients, 6 years in 9 (12.8 %) patients, 7 years in 6 (8.6 %) patients, 8 years in 1 (1.4 %) patient, 9 years in 3 (4.3 %) patients, 10 years in 1 (1.4 %) patient, 11 years in 4 (5.7 %) patients, 12 years in 2 (2.8 %) patients, 13 years in 1 (1.4 %) patient, 14 years in 1 (1.4 %) patient, 15 years in 2 (2.8 %) patients, 19 years in 1 (1.4 %) patient and 20 years in one (1.4 %) patient]. The evolution of joint involvement during follow-up in our patients was noted as oligoarticular (less than 4 affected joints) and polyarticular (more than 5 affected joints).
At the time of sample collection, the disease activity status was assessed by applying the Juvenile Arthritis Disease Activity Score-27 (JADAS-27) [21] and also by determination of C-reactive protein (CRP). The JADAS-27 includes the following four measures: physician global assessment of disease activity, measured on a 10-cm visual analog scale (VAS) where 0 = no activity and 10 = maximum activity; parent/patient global assessment of well-being, measured on a 10-cm VAS where 0 = very well and 10 = very poor; count of joints with active disease (in 27 joints: cervical spine, elbows, wrists, metacarpophalangeal joints—from the first to third, proximal interphalangeal joints, hips, knees, and ankles) and erythrocyte sedimentation rate (ESR)—normalized to a 0 to 10 scale according to the following formula: (ESR (mm/h) − 20)/10. The level of disease activity as measured with JADAS-27 (range 0–57) was found to be low (JADAS-27 < 10) in 14 patients, moderate (JADAS-27 range 10–25) in 22 patients and high (JADAS-27 > 25) in two patients. Thirty-two patients were in disease remission at the time of the study.
The outcome of disease severity was determined by assessment of the joint damage at the first visit for the study and again, at last follow-up, and also by evaluation of the prescription pattern of JIA medication [biological agents or nonbiologic disease-modifying anti-rheumatic drugs (DMARDs)]. The articular damage was established by reanalyzing the patient conventional radiographs for documenting the structural joint damage (joint space narrowing, bone deformity, erosions or ankylosis) and also by clinical articular assessment looking for motion restrictions, joint deformities and contractures not related to active arthritis and persistent for at least 6 months, disturbances of bone growth and also the need for orthopaedic surgery. The radiographs of the involved joints were taken according to treating physician at the JIA diagnosis and during the disease course when patient history or physical exam raised clinical concern about joint damage or decline in function. Radiographic assessment was performed by a paediatric radiologist and reviewed by a paediatrician with experience in paediatric rheumatology, using anteroposterior and lateral films of hands, wrists, knee, ankles, feet, pelvis or sacroiliac joints. An agreement between the two observers was reached in cases with subtle differences in radiographic interpretation.
Information on the therapeutic outcome was obtained from the treating physician. At the time of the sample collection, 14 patients were treated with nonsteroidal anti-inflammatory drugs, 24 with DMARDs (Methotrexate, Sulfasalazine), 18 with oral glucocorticosteroids and five patients were receiving Etanercept. Eleven of them were on disease remission without medication. Three patients have discontinued the Etanercept by the time of our study, one of them after sustained disease remission and two of them because of serious adverse events. By the end of the research, ten more patients were switched to anti-TNF-α inhibitors. In two more patients, the prescription of anti-TNF-α agents was done by the treating physician and refused by the parents.
Laboratory methods
Sera were collected for all patients as part of their periodic clinical and biological assessment of disease activity. Anti-CCP quantitative determination was performed in a commercial laboratory by microparticle enzyme immunoassay (MEIA), using second-generation CCP2 peptides without knowledge of the patient’s clinical details of the disease. The assay range of detection was 0–200 U/mL. The cut-off between positive and negative was 3 U/mL, as established by the fabricant among adult population. ESR determination used the Westergreen method, millimetre per half hour, and immunological investigations as CRP, RF-IgM and serum total immunoglobulin G (IgG) were analysed by immunoturbidimetry. The cut-off for RF in our laboratory was 19 IU/mL. Designation of RF seropositive status was done according to ILAR criteria, when presence of RF was documented on at least two occasions at least 3 months apart. Anti-CCP were analysed only once, at the time of the study. Repeated RF determinations were made for all patients throughout their regular medical care.
Statistical analysis
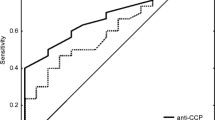
Statistical analyses were conducted using SPSS 13. Patient groups were compared using Fisher’s exact test. P values less than 0.05 were considered significant. The relative risk (RR) with 95 % confidence interval was also calculated.
Results
The study population consisted of 46 females and 24 males (65.7 versus 34.3 %). At the time of sample collection, the median age of the patients was 11.54 years (range 1.8–20). ILAR categorization was 4 patients with RF-positive polyarthritis (5.7 %), 15 with RF-negative polyarthritis (21.4 %), 6 with extended oligoarthritis (8.6 %), 26 with persistent oligoarthritis (37 %), 3 (4.3 %) with enthesitis-related arthritis (ERA), 15 with systemic disease (21.4 %) and 1 (1.4 %) with undifferentiated arthritis. In our cohort, 34/70 (48.6 %) patients were identified as having a polyarticular joint disease, and among them, 30 patients were RF-negative. Seventeen patients (24.3 %) were confirmed with joint damage (4 with RF-positive polyarthritis JIA, 7 with RF-negative polyarthritis JIA, 3 with extended oligoarthritis, 2 with HLA-B27 positive ERA and 1 with systemic JIA with polyarticular course).
Throughout the disease follow-up, no conversions from RF seronegative to RF seropositive polyarticular disease were noted, even in patients with joint damage.
Nine JIA patients were seropositive for anti-CCP with respect to the cut-off value of the test. All RF-positive polyarthritis patients had high anti-CCP levels (two of them exceeding the assay range of detection, and the other two having 105.2 and 9.8 U/mL, respectively). Positive serum anti-CCP levels also occurred in four patients with RF-negative polyarthritis (3.9, 3.6, 3.6 and 3.2 U/mL) and in one patient with extended oligoarthritis (4.8 U/mL), all with erosive joint disease (Table 1).
Another two patients with polyarticular disease (RF-negative polyarthritis and extended oligoarthritis) had marginally negative anti-CCP levels (2.8 and 2.7 U/ml, respectively), both with considerable joint damage at follow-up. All the rest demonstrated very low or undetectable anti-CCP levels.
When patients with JIA subtypes other than RF-positive polyarthritis were investigated separately, there was a significant association between anti-CCP reactivity and polyarticular joint involvement (p = 0.016, Fisher’s exact test), also with the presence of joint damage (p < 0.001, Fisher’s exact test). Patients with positive anti-CCP were significantly more likely to develop a polyarthritis (RR = 2.4; 95 % CI, 1.8–3.3) and to have an erosive joint disease (RR = 7.6; 95 % CI, 3.9–14.5) compared to patients with negative anti-CCP.
The distinct features of articular damage found in patients with positive and marginally negative anti-CCP are described in detail in Table 1. Six patients with radiological damage (35.3 %) had very low or undetectable anti-CCP levels. Among them, one female patient at 20 years follow-up had multiple erosions, osteopenia, subluxations and lateral deviation in both hands and feet and significant growth retardation. Another girl with long-term articular damage was remarked with multiple erosions and cystic changes in the carpal bones, advanced osteoporosis. Marginal irregularities and sclerosis in the sacroiliac joints and coxarthrosis were noted in a 17-year-old boy with HLA-B27-positive ERA. The joint damage in the other three patients was characterized by erosions in the right second metatarsophalangeal joint in one boy with HLA-B27-positive ERA, loss of joint space of the left PIP 4 and PIP 5 area with flexion deformity in another 3-year-old boy with RF-negative polyarticular disease and bone growth disturbance and osteonecrosis of femoral heads with severe degenerative changes of both hip joints in a girl with a polyarticular RF-negative disease at 5 years follow-up.
We detected no correlation between anti-CCP titres and total IgG levels (p = 0.73), JADAS-27 (p = 0.51, Mann-Whitney test), CRP levels (p = 0.42, Mann-Whitney test), ESR (p = 0.77, Mann-Whitney test), prescription of biologicals (p = 0.63, Fisher’s exact test) or DMARDs’ use (p = 0.32, Fisher’s exact test).
Discussion
Our findings offer additional information regarding the potential role of anti-CCP in predicting joint involvement during disease course, particularly among patients with JIA subtypes other than RF-positive polyarthritis. In our study, all patients with RF-positive polyarthritis had high anti-CCP levels and an aggressive erosive disease. For the rest of the patients, anti-CCP levels were less prevalent, and when positive, they were in much lower titres. But we could easily observed, that these patients could also benefit from anti-CCP results, as polyarticular joint involvement and also the presence of joint damage in these patients were significantly associated with the presence of anti-CCP. Likewise, patients with borderline anti-CCP levels (>2.5 U/mL) also exhibit articular damage.
The prevalence of anti-CCP in our RF-negative JIA population was 7.5 % comparable to 6.9 [12] and 6.25 % [13] from the recent published cohorts. Moreover, the discrepancy in the anti-CCP quantitative status between RF-positive and RF-negative patients has also been reported by other investigators [8, 12, 20]. It has been suggested that patients with a low titre of anti-CCP in the absence of RF may represent a distinct subset of JIA patients [12]. Additionally, we observed that this subset of JIA patients was significantly more likely to develop a polyarthritis and to have an erosive joint disease compared to anti-CCP seronegative patients. Several prior observations have also indicated a correlation between radiographic joint damage and anti-CCP positivity [8, 10, 14, 19, 22] and even with borderline anti-CCP levels [8], but their analysis looked at the whole group of JIA patients. Therefore, investigating anti-CCP should clearly be taken into consideration in the decision whether a patient should be treated aggressively at an early stage and probably in future revisions of ILAR criteria.
An important aspect of our cohort is that six anti-CCP negative JIA patients have also developed significant structural joint damage at follow-up. This is a strong indication that anti-CCP alone may not be sufficient in predicting joint destruction in JIA patients and that other associated factors could also be involved in the pathogenesis.
The performance of anti-CCP in predicting the therapeutic outcome was also examined in our study. No association was found between anti-CCP reactivity and prescription of biologicals or the use of DMARDs. Additionally, we observed no relationship between anti-CCP titres and severity of the disease activity quantified with a composite disease activity score (JADAS-27) or serum concentrations of CRP at the time of the study. This composite index provides a comprehensive view of disease activity for JIA patients and is the only one available for JIA at the moment. Studies in adults with RA have also addressed this issue [21] and concluded that changes in antibody levels do not reflect changes in disease activity. Moreover, nowadays, there is strong evidence that anti-CCP may be present years before the onset of the disease in RA. Therefore, we believe that anti-CCP appears to have a greater prognostic importance rather than a meaning of disease activity status.
One limitation of our study is that our patients were investigated for anti-CCP at one specific point in time, at different moments after disease onset. Adult studies have shown that very few patients change their anti-CCP antibody status over time over a 1 to 5-year period, but when qualitative changes occurred, they tend to be in marginally positive samples [23]. In 2002, Avcin et al. assessed serial anti-CCP determination in 20 JIA patients; of whom, the only two patients with low positive anti-CCP levels at first determination were transiently positive [24]. Having high specificity for inflammatory arthritis, we believe that evidence of anti-CCP positivity at some point during the disease course should be relevant for the clinical judgement in JIA patients and not necessarily the level of anti-CCP or its fluctuation in time.
In paediatric patients, there have been suggested a potential effect of age on the prevalence and titre of anti-CCP. Dewint et al. detected higher anti-CCP titres in polyarthritis patients older than 16 years of age compared to younger patients [25]. The investigators hypothesized that the positivity of anti-CCP may be influenced by lower IgG production in children [25]. We detected no correlation between anti-CCP titres and total IgG levels. Whether anti-CCP reactivity is dependent on RF positivity, upon age or other external factors causing the disease need to be determined by further studies.
The accurate assessment of joint destruction in paediatric patients is challenging. According to domain experts, the conventional radiography is currently still the reference for assessment of bone and cartilage destruction in JIA but without standardized protocols for monitoring the radiographic damage [26, 27]. Most studies published to date, investigating the potential role of anti-CCP in predicting erosive disease in JIA, have used conventional radiography to evaluate joint space narrowing and/or erosions [8, 10, 14, 19, 22]. Our study is limited by the fact that in patients without poor prognosis factors, previous evidence of joint damage and no recent alteration in their symptoms or clinical examination, no additional radiographs have been taken for the study. In these children, radiation exposure was considered a potential risk and of no clear benefit for the patient, and therefore, inappropriate.
Other limitations for our study are related to very few patients of RF-positive polyarticular JIA included and also to the low number of patients with RF-negative polyarticular course. However, distribution of JIA subtypes in our cohort is in accordance with that of other JIA populations [18], and the prevalence of anti-CCP in our patients was comparable to other published cohorts.
On conclusion, investigating anti-CCP should clearly be taken into consideration even among patients with JIA subtypes other than RF-positive polyarthritis. Although at low concentration, presence of anti-CCP in our RF-negative JIA patients gave indication of a more severe articular disease. Larger cohorts still need to be studied in order to validate these findings.
Abbreviations
- CCP:
-
Cyclic citrullinated peptide
- DMARDs:
-
Disease-modifying anti-rheumatic drugs
- ERA:
-
Enthesitis-related arthritis
- ILAR:
-
International League Against Rheumatism
- IgG:
-
Immunoglobulin G
- JIA:
-
Juvenile idiopathic arthritis
- JADI-A:
-
Juvenile arthritis damage index-articular damage
- JADAS-27:
-
Juvenile Arthritis Disease Activity Score-27
- RA:
-
Rheumatoid arthritis
- RF:
-
Rheumatoid factor
References
Petty RE, Southwood TR, Manners P et al (2004) International League of Associations for Rheumatology classification of juvenile idiopathic arthritis: second revision, Edmonton, 2001. J Rheumatol 31:390–392
van Dijkhuizen EH, Wulffraat NM (2014) Early predictors of prognosis in juvenile idiopathic arthritis: a systematic literature review. Ann Rheum Dis. doi:10.1136/annrheumdis-2014-205265
Schellekens GA, de Jong BA, van den Hoogen FH, van de Putte LB, van Venrooij WJ (1998) Citrulline is an essential constituent of antigenic determinants recognized by rheumatoid arthritis-specific autoantibodies. J Clin Invest 101:273–281
Schellekens GA, Visser H, de Jong BA, van den Hoogen FH, Hazes JM, Breedveld FC, van Venrooij WJ (2000) The diagnostic properties of rheumatoid arthritis antibodies recognizing a cyclic citrullinated peptide. Arthritis Rheum 43:155–163
Payet J, Goulvestre C, Bialé L et al (2014) Anticyclic citrullinated peptide antibodies in rheumatoid and nonrheumatoid rheumatic disorders: experience with 1162 patients. J Rheumatol 41:2395–2402
van Gaalen FA, Linn-Rasker SP, van Venrooij WJ et al (2003) Autoantibodies predict progression to rheumatoid arthritis in undifferentiated arthritis: a prospective cohort study. Arthritis Res Ther 5:28
Kokkonen H, Mullazehi M, Berglin E, Hallmans G, Wadell G, Rönnelid J, Rantapää-Dahlqvist S (2011) Antibodies of IgG, IgA and IgM isotypes against cyclic citrullinated peptide precede the development of rheumatoid arthritis. Arthritis Res Ther 13:R13
Kasapcopur O, Altun S, Aslan M et al (2004) Diagnostic accuracy of anti-cyclic citrullinated peptide antibodies in juvenile idiopathic arthritis. Ann Rheum Dis 63:1687–1689
Machado SH, von Mühlen CA, Brenol JC, Bisotto L, Xavier RM (2005) The prevalence of anti-cyclic citrullinated peptide antibodies in juvenile idiopathic arthritis. J Pediatr (Rio J) 81:491–494
Syed RH, Gilliam BE, Moore TL (2008) Prevalence and significance of isotypes of anti-cyclic citrullinated peptide antibodies in juvenile idiopathic arthritis. Ann Rheum Dis 67:1049–1051
van Rossum M, van Soesbergen R, de Kort S et al (2003) Anti-cyclic citrullinated peptide (anti-CCP) antibodies in children with juvenile idiopathic arthritis. J Rheumatol 30:825–828
Tebo A, Jaskwski T, Wayne Davis K et al (2012) Profiling anti-cyclic citrullinated peptide antibodies in patients with juvenile idiopathic arthritis. Pediatr Rheumatol 10:29
Gilliam BE, Reed MR, Chauhan AK, Dehlendorf AB, Moore TL (2011) Evidence of fibrinogen as a target of citrullination in IgM rheumatoid factor-positive polyarticular juvenile idiopathic arthritis. Pediatr Rheumatol Online J 9:8
Habib HM, Mosaad YM, Youssef HM (2008) Anti-cyclic citrullinated peptide antibodies in patients with juvenile idiopathic arthritis. Immunol Invest 37:849–857
Kwok JS, Hui KH, Lee TL et al (2005) Anti-cyclic citrullinated peptide: diagnostic and prognostic values in juvenile idiopathic arthritis and rheumatoid arthritis in a Chinese population. Scand J Rheumatol 34:359–366
Ferucci ED, Majka DS, Parrish LA et al (2005) Antibodies against cyclic citrullinated peptide are associated with HLA-DR4 in simplex and multiplex polyarticular-onset juvenile rheumatoid arthritis. Arthritis Rheum 52:239–246
Low JM, Chauhan AK, Kietz DA, Daud U, Pepmueller PH, Moore TL (2004) Determination of anti-cyclic citrullinated peptide antibodies in the sera of patients with juvenile idiopathic arthritis. J Rheumatol 31:1829–1833
Ravelli A, Martini A (2007) Juvenile idiopathic arthritis. Lancet 369:767–778
Omar A, Abo-Elyoun I, Hussein H, Nabih M, Atwa H, Gad S, Emad Y (2013) Anti-cyclic citrullinated peptide (anti-CCP) antibody in juvenile idiopathic arthritis (JIA): correlations with disease activity and severity of joint damage (a multicenter trial). Joint Bone Spine 80:38–43
Berntson L, Nordal E, Fasth A et al (2014) Anti-type II collagen antibodies, anti-CCP, IgA RF and IgM RF are associated with joint damage, assessed eight years after onset of juvenile idiopathic arthritis (JIA). Pediatr Rheumatol Online J 12:22
Consolaro A, Ruperto N, Bazso A et al (2009) Development and validation of a composite disease activity score for juvenile idiopathic arthritis. Arthritis Rheum 61:658–666
Gupta R, Thabah MM, Vaidya B, Gupta S, Lodha R, Kabra SK (2010) Anti-cyclic citrullinated peptide antibodies in juvenile idiopathic arthritis. Indian J Pediatr 77:41–44
Rönnelid J, Wick MC, Lampa J, Lindblad S, Nordmark B, Klareskog L, van Vollenhoven RF (2005) Longitudinal analysis of citrullinated protein/peptide antibodies (anti-CP) during 5 year follow up in early rheumatoid arthritis: anti-CP status predicts worse disease activity and greater radiological progression. Ann Rheum Dis 64:1744–1749
Avcin T, Cimaz R, Falcini F et al (2002) Prevalence and clinical significance of anti-cyclic citrullinated peptide antibodies in juvenile idiopathic arthritis. Ann Rheum Dis 61:608–611
Dewint P, Hoffman IE, Rogge S et al (2006) Effect of age on prevalence of anticitrullinated protein/peptide antibodies in polyarticular juvenile idiopathic arthritis. Rheumatology (Oxford) 45:204–208
Breton S, Jousse-Joulin S, Finel E, Marhadour T, Colin D, de Parscau L, Devauchelle-Pensec V (2012) Imaging approaches for evaluating peripheral joint abnormalities in juvenile idiopathic arthritis. Semin Arthritis Rheum 41:698–711
Magni-Manzoni S, Malattia C, Lanni S, Ravelli A (2012) Advances and challenges in imaging in juvenile idiopathic arthritis. Nat Rev Rheumatol 8:329–336
Acknowledgments
This paper was published under the frame of European Social Found, Human Resources Development Operational Programme 2007–2013; project no. POSDRU 159/1.5/S/138776.
Disclosures
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Spârchez, M., Miu, N., Bolba, C. et al. Evaluation of anti-cyclic citrullinated peptide antibodies may be beneficial in RF-negative juvenile idiopathic arthritis patients. Clin Rheumatol 35, 601–607 (2016). https://doi.org/10.1007/s10067-015-2971-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-015-2971-5