Abstract
The aims of this study are to analyse the characteristics of septic arthritis stratified by age and to identify the predictors of treatment failure and mortality in septic arthritis. A retrospective single-centre study was conducted in patients with native septic arthritis between 1994 and 2012. The primary outcome was treatment failure. Secondary outcomes included mortality, complications, endocarditis, bacteraemia, hospital readmission and the duration of the hospital stay. Logistic regression analyses with a propensity score were performed to identify the predictors of response and mortality. Additional analyses were performed according to age and the initial treatment (surgery or conservative). A total of 186 patients were studied. The median (interquartile range) age was 64 (46, 74) years, and the percentage of male patients was 68.9 %. A logistic regression analysis showed that Staphylococcus aureus infection [OR 2.39 (1.20–4.77), p = 0.013], endocarditis [OR 4.74 (1.16–19.24), p = 0.029] and the involvement of joints difficult to access with needle drainage [OR 2.33 (1.06–5.11), p = 0.034] predict treatment failure and that age [OR 1.27 (1.07 = 1.50), p = 0.005], the leucocyte count at baseline [OR 1.01 (1.00–1.02), p = 0.023], bacteraemia [OR 27.66 (1.39–551.20), p = 0.030], diabetes mellitus [OR 15.33 (1.36–172.67), p = 0.027] and chronic renal failure [OR 81.27 (3.32–1990.20), p = 0.007] predict mortality. No significant differences in treatment failure by age were found. In septic arthritis, the predictors of mortality and the predictors of treatment failure differ. The predictors of treatment failure concern local factors and systemic complications, whereas conditions related to the host’s immune competence, such as age and comorbidities that hamper the host’s response, predict mortality.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
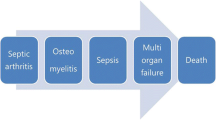
Septic arthritis is a serious and potentially life-threatening condition. Delays in its diagnosis and treatment can lead to irreversible joint damage with consequent functional loss and death [1]. The administration of intravenous antibiotics coupled with drainage of the joint through needle aspiration or surgery (arthroscopy or arthrotomy) are the standard treatments. A better understanding of the diagnosis and management of septic arthritis is still needed to improve the prognosis of this disorder.
Previous studies that analysed the predictors of outcome and mortality in septic arthritis included a small number of patients or patients with septic arthritis of a joint prosthesis [2, 3]. However, this type of septic arthritis presents substantial differences in its clinical and microbiological data and in its management compared with native septic arthritis. Both the age of the population and the comorbidities are increasing in current clinical practice. Age may be considered to be not only a risk factor for septic arthritis but also may be an important prognostic factor of response to treatment [4, 5]. However, reports of the characteristics of septic arthritis in the older population and information about the differences in response to treatment compared with younger patients are limited. Small case series [2, 5, 6] and one large descriptive study that included native and prosthetic septic arthritis analyse these differences [7].
The selection of the type of joint drainage is generally based on the individual physician’s experience. The data that describe the effectiveness of these interventions are based on small descriptive studies that yielded conflicting results. Some comparative studies show that surgical treatment is not superior to daily needle aspiration [8–11]. In contrast, one study shows the superiority of early surgical intervention over closed daily needle aspiration [12]. Thus, the role of needle aspiration, arthrotomy, or arthroscopy in the treatment of septic arthritis is not clear [13]. A careful selection of treatment for each patient may be essential to improve the prognosis of septic arthritis.
The aims of the present study are to analyse the characteristics and differences in responses stratified by age and to identify the predictors of treatment failure and mortality in native septic arthritis, with special attention to the type of drainage.
Materials and methods
This is a single-centre retrospective observational study of patients with a diagnosis of septic arthritis and a synovial fluid culture yielding bacterial growth identified via the coding system in a university hospital from 1994 to 2012. The data were obtained from the hospital’s database records. This study was performed using a checklist based on the preliminary core set of domains and reporting requirements for longitudinal observational studies in rheumatology [14]. The study protocol was approved by the Clinical Research Ethic Committee of Galicia. Informed consent from the patients was not required owing to the nature of the study.
The selection criteria were defined as follows: (1) men or women of at least 18 years of age, (2) diagnosis of septic or infectious arthritis and (3) synovial fluid culture yielding bacterial growth. Septic arthritis related to prosthetic materials was not included.
Patients were treated with early surgery, including either arthroscopy or arthrotomy (in the first 72 h after diagnosis) or daily closed needle aspiration, selected at the physician’s discretion.
The primary endpoint was treatment failure, which was operatively defined as death, admission to the intensive care unit, the need for surgery after 72 h of initial treatment or readmission to the hospital for the same reason. The investigated secondary endpoints were mortality during hospitalisation and mortality in the first year after the diagnosis, the number of hospitalised days, and complications, such as endocarditis or bacteraemia. The data collected included age, gender, joints involved, presence of comorbidities, admitting department, number of hospitalised days, joint and blood culture results, baseline leucocyte counts, baseline erythrocyte sedimentation rate (ESR), baseline C-reactive protein (CRP) levels, treatment and development of complications, such as endocarditis or bacteraemia. Special attention was paid to the data on early surgery, including arthroscopy or arthrotomy (in the first 72 h after diagnosis) or closed needle aspiration.
Statistical analysis
A descriptive analysis was stratified by the age (70 years or older vs. younger than 70 years). Significant differences in the baseline characteristics and differences in the response were analysed in both populations. A second analysis was performed to identify the differences in the baseline characteristics and the differences in response according to the type of early intervention, i.e. early surgical intervention (in the first 72 h after admission) or conservative medical treatment with repetitive joint taps as needed. Dichotomous variables were analysed using the chi-squared or Fisher’s exact test and continuous variables were analysed using the Wilcoxon-Mann-Whitney test. A p < 0.05 was considered to be statistically significant.
Logistic regression analyses were performed to identify the predictors of treatment failure and mortality. Dichotomous variables included in the univariate analyses were the gender, joint, Staphylococcus aureus, early surgical intervention, comorbidities (described in Table 1), endocarditis, bacteraemia and admission to the rheumatology unit. This variable was included to take into account that the rheumatology unit is more experienced than other departments in the treatment of septic arthritis in our hospital. Continuous variables included in the univariate analyses were the age, baseline leucocytes, ESR baseline and CRP baseline. Variables in the univariate analysis with a p < 0.10 were included in the multivariate analysis. Finally, a propensity score model was created to correct for the confounding factors. The quality of the propensity score model was assessed using a Hosmer-Lemeshow test (statistical test for goodness of fit for logistic regression models) [15]. A logistic regression analysis that included the propensity score was performed to identify the predictors of treatment failure and mortality. Stata version 11.1 (Stata/IC 11.1 for Windows, StataCorp LP, Texas, USA) was used in all of the statistical analyses.
Results
A total of 186 patients with native septic arthritis were included in the study. The median (interquartile range) age was 64 (46, 74) years, and the percentage of male patients was 68.9 %. The knee was the most commonly involved joint, and it was significantly more frequently involved in patients aged less than 70 years (younger population) than in the population aged 70 years or older (older population) (p = 0.043). The sternoclavicular joint was also affected more frequently in the younger population than in the older population (p = 0.012). In contrast, the shoulder was more frequently affected in the older population than in the younger population (p = 0.047). Osteoarthritis (p = 0.003), cardiovascular disease (p < 0.001), malignancies (p = 0.043), rheumatoid arthritis (p = 0.006) and chronic obstructive pulmonary disease (p = 0.003) were more frequent in the older population than in the younger population. Details of the baseline characteristics are described in Table 1.
Staphylococcus aureus was the most common microorganism in all populations (63.8 % of infections). The frequency of Staphylococcus aureus in the older group was 68.1 and 61.5 % in the younger group. Streptococcus pneumoniae was statistically more prevalent in the older population than in the younger population (p = 0.043). No other differences were found (see details in Table 2).
The frequency of treatment failure in all populations was 39.7 %. No significant differences were found between the older and younger populations (47.8 vs. 35.0 %, p = 0.085). The mortality was 8.6 % in the global population. The mortality was higher in the older population than in the younger population (20.2 vs. 1.7 %, p < 0.001). The mortality 12 months after the diagnosis was 16.6 %, with a significantly higher frequency in the older population than in the younger population (28.9 vs. 9.4 %, p = 0.001). The frequency of complications in the global population was 45.1 %. Complications were also more frequent in the older than the younger population (59.4 vs. 36.7 %, p = 0.003). The frequency of hospital readmission in the global population was 12.3 %, and readmission was more frequent in the younger group than in the older population (17.0 vs. 4.3 %, p = 0.011). No significant differences in endocarditis (p = 0.059), bacteraemia (p = 0.073) or the duration of the hospital stay (p = 0.458) were found in the two groups.
Thirty-two patients had early surgery, and 154 received conservative treatments (see Tables S1 and S2 in the online supplementary material). Groups did not differ statistically except for the frequency of infected hips, which was more commonly treated with surgery (p = 0.024). Furthermore, patients hospitalised in the rheumatology unit habitually underwent conservative treatment (p < 0.001), and patients hospitalised in the orthopaedic surgery unit underwent early surgery (p < 0.001). The groups treated surgically and conservatively did not differ statistically in the rates of treatment failure (53.1 % in the early surgery-treated group vs. 37.0 % in the conservatively treated group, p = 0.090). In addition, the other secondary outcomes were not significantly different.
A propensity score model identified the admitting department as a confounding factor (Hosmer-Lemeshow chi-square result of 90.21, p < 0.001). A logistic regression analysis that included the propensity score model showed that endocarditis [OR 4.74 (1.16–19.24), p = 0.029], Staphylococcus aureus infection [OR 2.39 (1.20–4.77), p = 0.013], and involved joints with more difficult access to drainage, including the hip and small joints of the hands and feet [OR 2.33 (1.06–5.11), p = 0.034], predict treatment failure (see Table 3). Additionally, a logistic regression analysis that included the propensity score model showed that age [OR 1.27 (1.07–1.50), p = 0.005], the leucocyte count at baseline [OR 1.01 (1.00–1.02), p = 0.023], bacteraemia [OR 27.66 (1.39–551.20), p = 0.030], diabetes mellitus [OR 15.33 (1.36–172.67), p = 0.027] and chronic renal failure [OR 81.27 (3.32–1990.20), p = 0.007] predict mortality (see Table 4).
Discussion
In the present study of septic arthritis, treatment failure is predicted by the type of joint involved and the bacteria, and mortality is predicted by age, chronic comorbidities, the presence of an important inflammatory response and disseminated infection and the experience of the admitting unit.
Overall, the population in our study does not differ from that in other studies. The percentage of males and the proportion of patients with rheumatoid arthritis are higher than expected in the general population. A higher percentage of males with septic arthritis have been previously reported, especially in the younger population [7]. The risk of septic arthritis in patients with RA is increased several-fold [16–18]. This higher risk is explained by the reduced bactericidal activity of the synovial fluid and the defective phagocytosis related to the disease and/or to the medications [19–21]. In addition, rheumatoid arthritis patients treated with TNF antagonists are particularly susceptible to septic arthritis [22, 23]. The predominance of the knee infections characteristic in our study has been recurrently reported. Sternoclavicular septic arthritis is uncommon, and in previous studies, it has been more frequently reported in younger patients with risk factors [24]. In our study, sternoclavicular septic arthritis was also more frequent in the younger population, and 60 % of these patients had comorbidities. Other joints with similar structural characteristics, such as the pubic symphysis or sacroiliac joint, were commonly infected in the younger population [9, 25]. In the elderly, these joints are sclerosed and difficult for microorganisms to access due to poor vascularisation. In contrast, septic shoulder arthritis is more common in older patients who have predisposing factors, such as structural damage or comorbidities [26].
The logistic regression analysis showed that Staphylococcus aureus infection, endocarditis and joints with more difficult access to drainage (the hip and the small joints of the hands and feet) predict treatment failure. In addition, age, leucocytosis at the baseline, bacteraemia and comorbidities are predictors of mortality. Staphylococcus aureus was the most commonly isolated pathogen in the joint independent of age, as reported by many investigators. Previous reports have shown that Staphylococcus aureus is associated with a poor prognosis in septic arthritis [13]. Staphylococcus aureus is also a leading cause of community- and hospital-acquired bacteraemia. Staphylococcus aureus bacteraemia can often occur and ubiquitously seed the bacteria, resulting in severe disease and significant morbidity and death [27]. The frequency of endocarditis in patients with Staphylococcus aureus bacteraemia is high (∼30 %). This is consistent with our data that identified Staphylococcus aureus as a predictor of a poor response and endocarditis and bacteraemia as predictors of both poor response and mortality, respectively. Streptococcus pneumoniae septic arthritis is considered uncommon and is more frequently reported in older patients with comorbidities [28, 29]. In our study, pneumococcal septic arthritis was more common in the older population with cardiovascular disease, rheumatoid arthritis, diabetes mellitus or cirrhosis but did not in itself predict a poor outcome. The most effective method of joint drainage has yet to be clearly delineated, given the paucity of quality studies. There is no definitive evidence to recommend one method over another, and most studies focus on a specific joint [30, 31]. Traditionally, infected hip joints are drained by open arthrotomy, but arthroscopy appears to be as effective as open drainage [32]. Herein, the type of joint drainage was influenced by the department that the patient entered, and this difference was related to the decision of the physician in the emergency department. Only infected hips were more frequently treated with early surgery. This difference was expected because the hip is not easily accessible by needle aspiration. Patients hospitalised in the orthopaedic department were more likely to be treated surgically than those who were hospitalised in other departments. Therefore, a propensity score model was used to correct for this confounding factor. No significant differences in response outcomes were identified for the patients who were surgically and conservatively treated. A published systematic review showed that a significantly higher percentage of the conservatively treated patients had successful outcomes compared with the surgically treated patients. The authors of this work recommend the initial use of medical therapy and surgical drainage for unsuccessful or difficult joint drainage via needle aspiration [8]. Interestingly, when only the conservatively treated patients were analysed, mortality was significantly lower in the group of patients hospitalised in the rheumatology unit, where the largest number of patients had been admitted. Therefore, these results suggest that the experience of the admitting department in treating septic arthritis is an important predictor of mortality. Age was also identified as a predictive factor of mortality. In prior studies, the mortality rates of septic arthritis in older patients ranged from 9 to 23 % [2, 5–7]. In one study of septic arthritis including prosthesis infectious arthritis, an age older than 65 years was a risk factor for mortality [2]. In addition, septic arthritis in older patients has a high percentage of complications and risk of mortality in the first 12 months after the diagnosis. In contrast, the readmission rate was higher in the younger populations. However, these results should be interpreted with caution because they could reflect indirectly the higher rate of mortality in older patients instead of hospital readmission. Leucocytosis is an independent predictor for death [33–35]. In one study, leucocytosis (>10 × 109/l) at the time of hospital admission for any reason predicts inpatient mortality (OR = 2.0; p < 0.0001) [36]. The basis of this effect remains unknown. In keeping with this report, leucocytosis at the baseline was a predictor of mortality in our study.
Our study presents limitations. Some data were missing, as commonly happens in retrospective studies. Additionally, bias in the treatment choice was clear and related to the admitting unit. Nevertheless, our analysis including a propensity score may have accounted for this variable. The strengths of our work were the inclusion of only the patients with a synovial fluid culture yielding bacteria growth and the exclusion of patients with prosthetic joint infections.
In conclusion, the predictors of mortality and the predictors of treatment failure are different in septic arthritis. Conditions related to the host immune competence as age and comorbidities hamper the host’s response to an aggressive pathogen predict mortality. The definition of treatment failure was more comprehensive and included poor local and systemic infection outcomes. Predictors of this composited outcome concerned local factors and systemic complications. Our present work may help to improve therapeutic decisions for high-risk patients.
References
Ward J, Cohen AS, Bauer W (1960) The diagnosis and therapy of acute suppurative arthritis. Arthritis Rheum 3:522–535
Weston VC, Jones AC, Bradbury N, Fawthrop F, Doherty M (1999) Clinical features and outcome of septic arthritis in a single UK Health District 1982–1991. Ann Rheum Dis 58(4):214–219
Yu LP, Bradley JD, Hugenberg ST, Brandt KD (1992) Predictors of mortality in non-post-operative patients with septic arthritis. Scand J Rheumatol 21(3):142–144
Cooper C, Cawley MI (1986) Bacterial arthritis in the elderly. Gerontology 32(4):222–227
Vincent GM, Amirault JD (1990) Septic arthritis in the elderly. Clin Orthop Relat Res 251:241–245
McGuire NM, Kauffman CA (1985) Septic arthritis in the elderly. J Am Geriatr Soc 33(3):170–174
Gavet F, Tournadre A, Soubrier M, Ristori JM, Dubost JJ (2005) Septic arthritis in patients aged 80 and older: a comparison with younger adults. J Am Geriatr Soc 53(7):1210–1213
Dubost JJ, Fis I, Denis P, Lopitaux R, Soubrier M, Ristori JM et al (1993) Polyarticular septic arthritis. Medicine (Baltimore) 72(5):296–310
Vyskocil JJ, McIlroy MA, Brennan TA, Wilson FM (1991) Pyogenic infection of the sacroiliac joint. Case reports and review of the literature. Medicine (Baltimore) 70(3):188–197
Bynum DK Jr, Nunley JA, Goldner JL, Martinez S (1982) Pyogenic arthritis: emphasis on the need for surgical drainage of the infected joint. South Med J 75(10):1232, –1235, 1238
Broy SB, Stulberg SD, Schmid FR (1986) The role of arthroscopy in the diagnosis and management of the septic joint. Clin Rheum Dis 12(2):489–500
Mathews CJ, Weston VC, Jones A, Field M, Coakley G (2010) Bacterial septic arthritis in adults. Lancet 375(9717):846–855
Dubost JJ, Soubrier M, De Champs C, Ristori JM, Bussiere JL, Sauvezie B (2002) No changes in the distribution of organisms responsible for septic arthritis over a 20 year period. Ann Rheum Dis 61(3):267–269
Wolfe F, Lassere M, van der Heijde D, Stucki G, Suarez-Almazor M, Pincus T et al (1999) Preliminary core set of domains and reporting requirements for longitudinal observational studies in rheumatology. J Rheumatol 26(2):484–489
Hosmer D, Lemeshow S (2000) Applied logistic regression. Wiley, New York
Kaandorp CJ, Van Schaardenburg D, Krijnen P, Habbema JD, van de Laar MA (1995) Risk factors for septic arthritis in patients with joint disease. A prospective study. Arthritis Rheum 38(12):1819–1825
Doran MF, Crowson CS, Pond GR, O’Fallon WM, Gabriel SE (2002) Frequency of infection in patients with rheumatoid arthritis compared with controls: a population-based study. Arthritis Rheum 46(9):2287–2293
Edwards CJ, Cooper C, Fisher D, Field M, van Staa TP, Arden NK (2007) The importance of the disease process and disease-modifying antirheumatic drug treatment in the development of septic arthritis in patients with rheumatoid arthritis. Arthritis Rheum 57(7):1151–1157
Dolganiuc A, Stavaru C, Anghel M, Baltaru D, Georgescu E, Olinescu A (2000) The migratory and phagocytic activity of polymorphonuclear leukocytes in rheumatoid arthritis and osteoarthritis patients. Roum Arch Microbiol Immunol 59(1–2):43–53
Turner RA, Schumacher R, Myers AR (1973) Phagocytic function of polymorphonuclear leukocytes in rheumatic diseases. J Clin Invest 52(7):1632–1635
Goldenberg DL (1989) Infectious arthritis complicating rheumatoid arthritis and other chronic rheumatic disorders. Arthritis Rheum 32(4):496–502
Strangfeld A, Listing J (2006) Infection and musculoskeletal conditions: bacterial and opportunistic infections during anti-TNF therapy. Best Prac Res Clin Rheumatol 20(6):1181–1195
Galloway JB, Hyrich KL, Mercer LK, Dixon WG, Ustianowski AP, Helbert M et al (2011) Risk of septic arthritis in patients with rheumatoid arthritis and the effect of anti-TNF therapy: results from the British Society for Rheumatology Biologics Register. Ann Rheum Dis 70(10):1810–1814
Ross JJ, Shamsuddin H (2004) Sternoclavicular septic arthritis: review of 180 cases. Medicine (Baltimore) 83(3):139–148
Ross JJ, Hu LT (2003) Septic arthritis of the pubic symphysis: review of 100 cases. Medicine (Baltimore) 82(5):340–345
Lossos IS, Yossepowitch O, Kandel L, Yardeni D, Arber N (1998) Septic arthritis of the glenohumeral joint. A report of 11 cases and review of the literature. Medicine (Baltimore) 77(3):177–187
Keynan Y, Rubinstein E (2013) Staphylococcus aureus bacteremia, risk factors, complications, and management. Crit Care Clin 29(3):547–562
Ispahani P, Weston VC, Turner DP, Donald FE (1999) Septic arthritis due to Streptococcus pneumoniae in Nottingham, United Kingdom, 1985–1998. Clin Infect Dis 29(6):1450–1454
Ross JJ, Saltzman CL, Carling P, Shapiro DS (2003) Pneumococcal septic arthritis: review of 190 cases. Clin Infect Dis 36(3):319–327
Goldenberg DL, Brandt KD, Cohen AS, Cathcart ES (1975) Treatment of septic arthritis: comparison of needle aspiration and surgery as initial modes of joint drainage. Arthritis Rheum 18(1):83–90
Sammer DM, Shin AY (2009) Comparison of arthroscopic and open treatment of septic arthritis of the wrist. J Bone Joint Surg Am 91(6):1387–1393
Nusem I, Jabur MK, Playford EG (2006) Arthroscopic treatment of septic arthritis of the hip. Arthroscopy 22(8):e901–903
de Labry LO, Campion EW, Glynn RJ, Vokonas PS (1990) White blood cell count as a predictor of mortality: results over 18 years from the Normative Aging Study. J Clin Epidemiol 43(2):153–157
Barron HV, Harr SD, Radford MJ, Wang Y, Krumholz HM (2001) The association between white blood cell count and acute myocardial infarction mortality in patients > or =65 years of age: findings from the cooperative cardiovascular project. J Am Coll Cardiol 38(6):1654–1661
Cannon CP, McCabe CH, Wilcox RG, Bentley JH, Braunwald E (2001) Association of white blood cell count with increased mortality in acute myocardial infarction and unstable angina pectoris. OPUS-TIMI 16 Investigators. Am J Cardiol 87(5):636, –639, A610
Asadollahi K, Hastings IM, Beeching NJ, Gill GV (2007) Laboratory risk factors for hospital mortality in acutely admitted patients. QJM : Mon J Assoc Physicians 100(8):501–507
Conflict of interest
All authors have declared no conflicts of interest.
Funding
None.
Contributors
J.R.M. took part in the study design, collection and interpretation of data and drafting the article. A.S. took part in the study design, collection and interpretation of data and drafting the article. E.C. took part in the collection of data. A.M. took part in the interpretation of data. L.C. took part in the interpretation of data. J.J.G.-R took part in the conception and study design, interpretation of data, drafting the article and critically revising it for important intellectual content. All authors gave the final approval for submission for publication.
Author information
Authors and Affiliations
Corresponding author
Additional information
The contribution of Jose R. Maneiro and Alejandro Souto to this article is equal.
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(DOCX 18 kb)
Rights and permissions
About this article
Cite this article
Maneiro, J.R., Souto, A., Cervantes, E.C. et al. Predictors of treatment failure and mortality in native septic arthritis. Clin Rheumatol 34, 1961–1967 (2015). https://doi.org/10.1007/s10067-014-2844-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-014-2844-3