Abstract
Hemofilters applied in continuous renal replacement therapies (CRRTs) for the treatment of acute kidney injury must meet high standards in biocompatibility and permeability for middle and large molecules over extended treatment times. In general, cellulose-based membranes exhibit good biocompatibility and low fouling, and thus appear to be beneficial for CRRT. In this in vitro study, we compared a novel asymmetric cellulose triacetate (ATA) membrane with three synthetic membranes [polysulfone (PS), polyethersulfone (PES), and polyethylenimine-treated acrylonitrile/sodium methallyl sulfonate copolymer (AN69 ST)] regarding thrombogenicity and cytokine removal. For thrombogenicity assessment, we analyzed the thrombin–antithrombin complex (TAT) generation in human whole blood during 5 h recirculation and filtration. Sieving coefficients of interleukin-6 (IL-6), IL-8, IL-10, and tumor necrosis factor-alpha (TNF-α) were determined using human plasma as test fluid. ATA and AN69 ST membrane permeability were determined also during long-term experiments (48.5 h). ATA exhibited the lowest TAT generation (6.3 µg/L at 5 h), while AN69 ST induced a pronounced concentration increase (152.1 µg/L) and filter clogging during 4 out of 5 experiments. ATA (IL-8: 1.053; IL-6: 1.079; IL-10: 0.898; TNF-α: 0.493) and PES (0.973; 0.846; 0.468; 0.303) had the highest sieving coefficients, while PS (0.697; 0.100; 0.014; 0.012) and AN69 ST (N/A; 0.717; 0; 0.063) exhibited lower permeability. Long-term experiments revealed stronger fouling of the AN69 ST compared to the ATA membrane. We observed the highest permeability for the tested cytokines, the lowest thrombogenicity, and the lowest fouling with the ATA membrane. In CRRT, these factors may lead to increased therapy efficacy and lower incidence of coagulation-associated events.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Continuous renal replacement therapies (CRRT) are a cornerstone for the treatment of patients with acute kidney injury (AKI) and they are also discussed as an appropriate supporting therapy for sepsis [1]. AKI is characterized by an inflammatory reaction in the kidneys and in the circulation. The injury induces the generation of a wide range of inflammatory mediators like cytokines and chemokines by tubular and endothelial cells. These factors trigger inflammation in a feedback loop promoting further kidney injury [2]. In sepsis, pro-inflammatory cytokines also promote the progression of the disease during the hyperinflammation phase. It has been hypothesized that the excessive inflammatory response could be downregulated by extracorporeal removal of cytokines and other mediators [3, 4]. Hemofiltration aims specifically for the convective removal of middle and large target molecules by using highly permeable filters. At the same time, albumin loss during the treatment must be considered. Modern membranes are, therefore, specifically designed to exhibit a steep sieving coefficient curve with a cutoff below the molecular weight of albumin. Besides the biocompatibility, which is generally good for modern membranes, an important performance benchmark for long-term applications of hemofilter or dialyzer membranes in CRRT is their susceptibility to protein fouling. Protein fouling can cause deterioration of the membrane permeability and potentially result in a less efficacious therapy. There is ongoing research in optimizing filtration properties for long-term applications and biocompatibility. Cellulose triacetate (CTA) membranes exhibit comparatively low fouling rates [5,6,7,8] and good biocompatibility [9,10,11,12,13], which, thus, might be beneficial in CRRT.
In the present study, we characterized a novel asymmetric cellulose triacetate (ATA) membrane regarding its thrombogenicity and removal capability for cytokines relevant in AKI and sepsis in recirculation models. ATA exhibits even less protein fouling compared to conventional CTA membranes [14]. Thrombogenicity and permeability of the ATA membrane were compared to three state-of-the-art synthetic membrane hemofilters [polysulfone (PS), polyethersulfone (PES), and acrylonitrile/sodium methallyl sulfonate copolymer with polyethylene imine surface treatment (AN69 ST)]. Furthermore, the filtration performance of the AN69 ST and ATA hemofilters was determined in long-term experiments to assess the membranes’ susceptibility to fouling.
Materials and methods
In vitro recirculation model
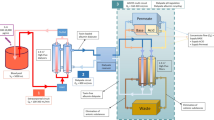
500 mL medical infusion bags (Impromediform, Germany) served as reservoir for the test solutions (see below). The reservoir bag was gently agitated using a rocking shaker (Rocker 2D digital; IKA, Germany) to ensure continuous mixing of the fluids throughout the experiments. Tubing and connectors for fluid transport were single-use, medical-grade dialysis equipment (Meise Medizintechnik, Germany). Test solutions were tempered to 37 °C with an infrared flow blood warmer (Fluido; the Surgical Company, Germany). Laboratory roller pumps (MCP; Ismatec, Germany) were used for recirculation of the test fluid and for filtration (see Fig. 1).
Hemofilters with four different membrane materials were tested, namely polysulfone (1.8 m2 membrane area; Ultraflux® AV 1000S, Fresenius Medical Care, Germany), polyethersulfone (1.5 m2; ELISIO™-HF, Nipro Corporation, Japan), acrylonitrile/sodium methallyl sulfonate copolymer with a polyethyleneimine surface treatment (1.5 m2; Prismaflex ST150, Gambro Lundia AB, Sweden), and asymmetric cellulose triacetate (1.5 m2; SOLACEA™-HF, Nipro Corporation, Japan).
Thrombogenicity
500 mL of citrate-anticoagulated human whole blood (German Red Cross blood donation center Rostock, Germany) donated at the longest 24 h prior to the experiments and stored at 4 °C served as test solution for the assessment of thrombogenicity of the filter membranes. The blood contained 70 mL of citrate-phosphate-dextrose (1.84 g sodium citrate dihydrate) as anticoagulant and was recalcified with approximately 5 mL of a 0.5-M CaCl2 solution to a Ca2+ target concentration of 0.4 mmol/L.
Rinsing of the test devices was conducted with pre-warmed phosphate-buffered saline (Gibco® PBS (1 ×), w/o Ca and Mg; Thermo Fischer Scientific, USA) prior to circulation of the test solution. By means of simultaneous filtration (filtrate flow ≈ 0.2 times the blood flow), the filtrate compartment of the hemofilter was filled with PBS.
During the experiments, the recalcified blood was pumped into the arterial inlet of the test devices. To ensure comparability between the filters with 1.5 m2 (PES, AN69 ST, ATA) and 1.8 m2 (PS) effective membrane area, a normalized blood flow rate with respect to the membrane area was set to 133 mL/(min m2), resulting in blood flows of 200 mL/min and 240 mL/min, respectively. Filtration was conducted with 25 mL/(min m2). The ratio of filtrate and blood flow was hence constant (0.1875) and a comparable hemoconcentration within the blood compartment of the hemofilters was ensured. After discarding the rinsing solution, the blood was circulated and the filtrate was continuously returned into the reservoir bag. The pressure at the hemofilter inlets was monitored to prevent the tubing from bursting in the case of filter clogging. A filter inlet pressure of 300 mmHg (maximum pressure for the flow heater) was chosen as the highest acceptable pressure.
Samples were taken from the arterial sampling port at the beginning and after 5, 10, 30, 60, 120, and 300 min. In the case of a premature test termination, the final samples were taken shortly before stopping the pumps. Samples for TAT quantification were taken in 2.9-mL citrate S-Monovettes® (Sarstedt, Germany). The samples were centrifuged immediately at 1500 rcf for 10 min. The plasma was carefully collected and stored at − 25 °C. TAT concentration in plasma was measured in duplicate with a commercially available ELISA kit (Enzygnost® TAT micro, Siemens Healthcare, Germany) and a microplate reader (CLARIOstar, BMG LABTECH, Germany).
Cytokine removal
The removal capabilities for the cytokines interleukin-6 (IL-6; molecular weight 20.9 kDa), IL-8 (8.4 kDa), IL-10 (18.6 kDa), and tumor necrosis factor-alpha (TNF-α; 17.4 kDa) were determined. These test molecules were selected on one hand because of their clinical relevance and on the other hand because of their molecular weights. It was intended to use cytokines with molecular weights distributed over the relevant transfer range of a hemofilter membrane. It is important to consider that two of the cytokines used as test molecules do not appear as monomeric molecules, but form dimers as in the case of IL-10 (37.2 kDa) or trimers as in the case of TNF-α (52.2 kDa). Therefore, the expected permeability is highest for IL-8 and lowest for TNF-α.
Prior to the experiments, the tubing set was rinsed with 500 mL pre-warmed and degassed physiological 0.9% saline solution and primed with pooled human plasma (Octaplas; Octapharma, Germany) for 30 min to decrease non-specific adsorption of cytokines to the polymeric tubing surfaces.
All cytokines were added in parallel in concentrations of 1.5 µg/L to the test solution (400 mL Octaplas). This starting concentration was chosen to obtain sample concentrations above the detection limits of the analytical methods, both in the venous outlet and also in the filtrate. The prepared test solution was pumped into the arterial inlet of the test device. To consider the different membrane areas of the hemofilters, the filtrate flow was set to 6 mL/(min m2) at a blood flow of 100 mL/min. After air and the rinsing solution were displaced, the test solution circulated and the filtrate was continuously returned. This was performed for 30 min to prime the plasma contacting surfaces of the hollow fibers with a uniform protein layer as well as to reach a steady state of concentrations and temperature. Five replicate experiments were conducted for each hemofilter type tested. Samples were taken at the filter inlet (cin) and outlet (cout), and at the filtrate outlet (cf) after 30 min and the duplicate 3 min later.
In addition, long-term cytokine removal experiments were conducted with the ATA and the AN69 ST hemofilters. A test medium pool was made from 1000 mL of standardized human plasma (Octaplas). The test pool was spiked with the recombinant human cytokines IL-6, IL-10, and TNF-α (Biolegend, USA) in a concentration of 1.5 µg/L each. After rinsing of the test circuit, the test solution recirculated for 48 h at 200 mL/min. Meanwhile, filtration was performed at 20 mL/min and the filtrate was returned into the pool.
Since cytokines may be adsorbed significantly, a repeated bolus of the cytokine stock solution was added to the test pool after 24 h and after 48 h. Samples were taken 30 min after each bolus from the test fluid pool, at the hemofilter’s arterial inlet, the venous outlet, and the filtrate outlet for determination of cytokine and albumin concentrations. The transmembrane pressure (TMP) was monitored continuously to obtain additional data about the fouling process.
Cytokine concentrations in plasma and filtrate were analyzed at the Central Laboratory of the University Medicine Rostock and with commercially available ELISA kits (Human ELISA MAX Deluxe; Biolegend, USA) using a microplate reader (Infinite M200; Tecan, Switzerland). The albumin concentrations were determined photometrically with a biochemistry analyzer (Cobas Mira; Roche, Switzerland) using an albumin diagnostic kit (LT-SYS, Germany).
Sieving coefficients (SC) were calculated from each measured sample triplet (cin, cout, cf) as follows:
The data were assessed regarding total cytokine removal to obtain information about the contribution of adsorption to cytokine removal. Since the samples were taken from the test fluid before the start of the circulation and after 30 min, it was possible to assess the decrease of cytokine concentrations caused by adsorption onto the polymeric surfaces of the test system, which mainly consisted of the hemofilter’s membrane area. The adsorbed cytokine mass was calculated as follows:
where mads is the sum of adsorbed cytokine masses on the surfaces of the tubing set, the hemofilter housing, and the outer and inner membrane surfaces; V0, Vf, and VB the volume of the test pool, the filtrate compartment (calculated from the filter dimensions), and the blood circuit (V0–Vf), respectively; c0, cin, and cf the concentration of the respective cytokine in the test pool at start of the experiments, and the concentrations at the filter inlet and filtrate outlet after 30 min, respectively. The inner and outer membrane surfaces are considerably larger than the tubing and housing surfaces and, therefore, account to the bulk of the adsorption. Furthermore, the tubing was identical for all experiments and its contribution to adsorption was, therefore, regarded as identical in all the experiments.
Ethical approval
Prior to blood donation, all donors have consented that their blood can be used for research purposes. The experimental use of donor blood was approved by the Ethics Committee of the University of Rostock (no. A 2018-0087).
Statistical analysis
Statistical analysis was conducted using GraphPad Prism version 6.05 (GraphPad Software Inc., USA). The data were expressed as the mean ± standard deviation (SD). Comparisons among the membrane-induced TAT levels were conducted using a two-way analysis of variance (ANOVA) after log transformation of the data and graphical evaluation of the transformation result. With a p value < 0.05, differences between the filters were considered significant.
Results
Thrombogenicity
TAT concentrations induced by the different membrane materials during the recirculation experiments are shown in Fig. 2. In the experiments with the PES and the PS membrane, a moderate increase of TAT concentrations of 10.74 ± 7.61 and 24.37 ± 11.74 µg/L, respectively, was observed after 300 min, with the latter differing significantly from ATA and AN69 ST membrane. It is of note that the PS filter with its membrane area of 1.8 m2 likely induced a higher TAT generation than it would have been observed with 1.5 m2. The ATA membrane induced only minor increases in TAT levels throughout the entire test period, resulting in a nearly physiological concentration of 6.32 ± 2.13 µg/L at the end of the experiments. With 5.28 ± 1.92 and 5.19 ± 1.16 µg/L, the AN69 ST and ATA membrane, respectively, exhibited similar thrombogenicity characteristics until 120 min. However, within the remaining 180 min, abrupt global coagulation occurred in the recirculation model with the AT69 ST membrane in 4 out of 5 experiments, after 274, 184, 263, and 194 min, respectively. Samples immediately taken prior to stopping the pumps exhibited a pronounced increase of 152.11 ± 116.69 µg/L in TAT concentrations, differing significantly from the other membrane materials.
TAT concentrations in human whole blood over the course of 300 min recirculation in the in vitro model system (mean ± SD, N = 5, *p < 0.05). The TAT mean of the AN69 ST membrane at 300 min was calculated from concentrations measured at the different experiment end times: filter #1: tend = 274 min; #2: 184 min; #3: 300 min; #4: 263 min; #5: 194 min. One replicate of the experiments with the PS membrane was omitted from evaluation because of non-physiological initial TAT concentrations in the donor blood (65.2 µg/L)
TAT concentrations were measured in duplicate with intra- and inter-assay coefficients of variability of 3.7 and 6.1%, respectively. Therefore, the high standard deviations of TAT concentrations partly observed were attributed to the naturally occurring high biological variance of the donor blood.
Cytokine removal
Figure 3 shows the differences of SC between the four membrane types that were determined in the short-term (30- and 33-min sampling time) experiments. ATA exhibited a high permeability for IL-6, IL-8, IL-10, and even a SC of almost 0.5 for the large trimer of TNF-α. The PES membrane was also highly permeable for IL-8 and IL-6, while IL-10 and TNF-α pass the membrane with SCs of 0.47 and 0.3. The SCs of the PS membrane were clearly lower. Only IL-8 could pass the membrane with a comparatively high SC of 0.7. The AN69 ST membrane was more difficult to assess: For IL-8 and IL-10, no SC could be calculated. In case of IL-8, all molecules were removed from plasma and filtrate prior to the first sampling at 30 min, so it is assumed that this cytokine has been completely adsorbed onto the membrane. In case of IL-10, blood inlet and outlet concentrations at 30 and 33 min lay within a similar range, and were considerably decreased compared to the initial IL-10 pool concentration. This indicates that the adsorption of IL-10 reached an equilibrium state prior to the first sampling, i.e., afterwards, no further molecules were removed by adsorption. Furthermore, the filtrate concentrations were below the detection limit, indicating that IL-10 did not pass the membrane. This behavior corresponds to a SC of zero.
Sieving coefficients of the four membrane materials and relative amount of adsorbed cytokine masses (mean ± SD, N = 5). The adsorbed masses for the PS membrane filter are related to a membrane area of 1.5 m2. Asterisk indicates no SC stated; see in the “Results” section. Double asterisk indicates N = 4
The relative mass of the respective cytokine adsorbed onto the membrane surfaces after 30 min of recirculation and filtration is also shown in Fig. 3. The data show distinct differences between the four membrane types. While the ATA and PES membrane adsorbed minor and moderate amounts of cytokines below 20 and 30% of the applied masses, respectively, cytokines are adsorbed to the PS and, particularly, the AN69 ST membrane at considerable levels: Except for IL-8 that adsorbed only slightly onto the PS membrane, more than 50% of the respective applied cytokine masses adsorbed onto both membranes, whereby IL-8 was even completely removed by the AN69 ST membrane due to adsorption.
During the long-term experiments, the TMP of the ATA and AN69 ST membrane increased to 159 and 271% of the initial value, respectively (Fig. 4a). The relative increase in TMP of the ATA membrane after 48.5 h was lower than the increase of the AN69 ST membrane after 24 h. It can be seen that the increase in TMP of the ATA membrane filter was predominantly due to an increase in blood inlet pressure, whereas blood and filtrate outlet pressure remained almost constant. The increase in TMP observed with the AN69 ST filter was a superposition of two pressure changes: on one hand, a comparable absolute increase in blood inlet pressure as measured with the ATA membrane and, on the other hand, a considerable decrease in filtrate outlet pressure. Again, the blood outlet pressure remained almost constant, because it mainly corresponded to the constant hydrostatic pressure originating from the test reservoir.
Inlet, outlet, filtrate, and transmembrane pressure (a), cytokine and albumin sieving coefficients (b), and HSA concentrations in the filtrate and at the arterial inlet (c) of the ATA and the AN69 ST membrane filters during the 48.5 h long-term experiments (mean ± SD, N = 2). Asterisk indicates N = 1
The ATA membrane’s initial IL-6, IL-10, TNF-α, and albumin SCs decreased from 1.057, 0.921, 0.795, and 0.035 to 0.610, 0.494, 0.207, and 0.010, respectively, whereas the SCs of the AN69 ST membrane remained constant at a comparatively low level of approximately 0.4, 0.01, 0.05, and 0.01 for IL-6, IL-10, TNF-α, and albumin, respectively (Fig. 4b).
The albumin loss of the ATA membrane as a result of filtration, which was expressed by the albumin concentration in the filtrate, initially was comparatively high and decreased over time to the same level as that of the AN69 ST membrane, while the albumin SC of the latter remained constantly low throughout the experiments. Considering the constant filtrate flow rate of 20 mL/min and assuming average HSA concentrations in the filtrate of 0.35 g/L (AN69 ST) and 0.79 g/L (ATA; Fig. 4c), the theoretical filtration-induced albumin loss during the 48.5 h of the experiments amounted to 20 and 46 g with the AN69 ST and the ATA membrane, respectively. The decrease in albumin concentration at the inlet of the AN69 ST filter as a result of adsorption was more pronounced than with the ATA membrane (Fig. 4c). The total albumin mass removed from the 1 L test pool by adsorption amounted to approximately 4 g in the AN69 ST filter and 0.7 g in the ATA filter after 48.5 h.
Discussion
CRRTs for treatment of AKI and sepsis in the intensive-care unit require long lifespans of the filters used, good biocompatibility, as well as preferably constant filtration performance for middle and large molecules. In the present study, four filter types with different membrane materials were characterized regarding their thrombogenicity and filtration properties for different cytokines in short- and long-term experiments. The contribution of adsorption to cytokine removal was also assessed.
All experiments assessing thrombogenicity were performed without any incident, like, e.g., clogging or overly strong hemolysis (data not shown), except for four out of five experiments with the AN69 ST hemofilters in which strongly pronounced increases in TAT concentrations were observed and which were terminated prematurely due to a critical rise in pressure. At the first sight, this result seems unusual because even for the apparently more poorly performing hemofilters in the present in vitro study filter lifespans of (mean ± SD) 55.4 ± 22.4 h (PS; FMC Ultraflux AV 1000S) [15] and 38.4 ± 25.9 h (AN69 ST; Gambro Prismaflex ST150) [16] are reported from clinical studies. However, the recirculation model applied in this study was designed to induce detectable differences in TAT concentrations within the comparatively short 5-h duration of the in vitro experiments with human whole blood. On the one hand, this was achieved by adjusting the ionic calcium concentration to a value of 0.4 mmol/L, which corresponds to the upper boundary stated for the post-filter ionic calcium level applied in regional citrate anticoagulation [17, 18] and which was expected to allow a pronounced TAT generation. On the other hand, the low cycle time of 2.5 min, in which the 500 mL blood reservoir was recirculated completely through the model, must almost inevitably have induced the activation of platelets and other cells relevant for coagulation resulting in elevated TAT levels. Therefore, the partly highly elevated TAT concentrations and observed filter clogging can only be translated to a limited extent to the clinical application. Nevertheless, our results are in accordance with the filter lifespans mentioned above and could, therefore, be indicative for actual longer filter life times of the PES and ATA membrane hemofilters in the clinic. The lower procoagulatory activity observed in our in vitro model with the PES and ATA membrane filters could also be clinically relevant in the case of patients with increased bleeding risk, when low-dose anticoagulation strategies are essential.
The experiments assessing cytokine removal capabilities revealed a high permeability of the ATA and PES membrane for all analyzed cytokines and minor to moderate adsorption, whereas the PS and AN69 ST membranes were less permeable, especially for the large IL-10 and TNF-α molecules, and exhibited pronounced adsorption of cytokines. Although the adsorptive removal rates of up to 60% and more than 75% of the applied cytokine masses observed with the PES and the AN69 ST membrane, respectively, suggest a considerable contribution of adsorption to the total cytokine removal, it must be considered that a comparatively small pool volume was treated in the present study. The 3 L of plasma of an average AKI or sepsis patient presumably contain larger amounts of cytokines and, in addition, a continuous cytokine release can occur during the clinical treatment. Furthermore, we observed that the adsorptive removal of one cytokine, namely IL-10, stagnated already within the priming and equilibration time prior to the first sampling, suggesting that adsorption can contribute to cytokine removal only to a limited extent. The AN69 ST membrane exhibited a markedly higher increase in TMP than the ATA membrane during the long-term experiments, which is indicative for stronger fouling. However, its cytokine SCs remained constant at a low level, whereas the initially high SCs of the ATA membrane decreased considerably over time despite a comparatively small increase in TMP. The increase in TMP of the ATA membrane was predominantly due to an increase in blood inlet pressure, whereas blood outlet and filtrate pressure remained almost constant. An increasing blood inlet pressure suggests narrowing of the inner lumen of the capillary fibers, probably as a result of protein adsorption (cake-layer formation) onto the inner hollow fiber surface. We estimated a protein layer thickness of approximately 3–4 µm inserting the radius of the pristine ATA hollow fiber (100 µm [19]) and the pressure drop over the hollow fiber (pin–pout) at the beginning and after 24 h into the Hagen–Poiseuille equation. This thickness is in the same order of magnitude as estimated by Boyd and Zydney [20] from the observations of a comparable study.
The protein layer resulted in a reduced permeability for large molecules but only in a slight increase in TMP, presumably because of the high hydraulic permeability of the ATA membrane (ultrafiltration coefficient: 66 mL/h/mmHg [19]). A possible explanation for the more pronounced increase in TMP (and decrease in filtrate pressure) of the AN69 ST membrane might be the lower hydraulic permeability (37.5 mL/h/mmHg [21]) making it more prone to fouling. Nevertheless, the higher TMP might have led to increased convective transmembrane transport of fluid and entrained molecules [22], possibly compensating the expected SC decrease.
Conclusion
From a clinical perspective, hemocompatibility and membrane fouling are of great concern especially in long-term treatments as used in intensive-care therapy of AKI or sepsis. For this reason, such treatments might benefit from the use of ATA or PES hemofilters with comparatively low thrombogenicity. Especially, patients with increased bleeding risk might benefit from the application of membranes with reduced need for anticoagulation. The consistently higher permeability observed with the ATA membrane during long-term experiments compared to the AN69 ST membrane should enable a more efficient convective removal of large molecular weight cytokines during prolonged treatment times, which might be beneficial for the treatment of AKI and sepsis in clinical practice.
References
Ronco C, Ricci Z, Backer D de, Kellum JA, Taccone FS, Joannidis M, et al. Renal replacement therapy in acute kidney injury: controversy and consensus. Crit Care. 2015;19:146.
Akcay A, Nguyen Q, Edelstein CL. Mediators of inflammation in acute kidney injury. Mediat Inflamm. 2009;2009:137072. https://doi.org/10.1155/2009/137072.
Ronco C, Tetta C, Mariano F, Wratten ML, Bonello M, Bordoni V, et al. Interpreting the mechanisms of continuous renal replacement therapy in sepsis: the peak concentration hypothesis. Artif Organs. 2003;27:792–801.
Vriese AS de, Colardyn FA, Philippe JJ, Vanholder RC, Sutter JH de, Lameire NH. Cytokine removal during continuous hemofiltration in septic patients. J Am Soc Nephrol. 1999;10:846–53.
Mueller J, Davis RH. Protein fouling of surface-modified polymeric microfiltration membranes. J Membr Sci. 1996;116:47–60.
Güell C, Davis RH. Membrane fouling during microfiltration of protein mixtures. J Membr Sci. 1996;119:269–84.
Fujimori A, Naito H, Miyazaki T. Adsorption of complement, cytokines, and proteins by different dialysis membrane materials: evaluation by confocal laser scanning fluorescence microscopy. Artif Organs. 1998;22:1014–7.
Clark WR, Hamburger RJ, Lysaght MJ. Effect of membrane composition and structure on solute removal and biocompatibility in hemodialysis. Kidney Int. 1999;56:2005–15.
Pieroni L, Levi Mortera S, Greco V, Sirolli V, Ronci M, Felaco P, et al. Biocompatibility assessment of haemodialysis membrane materials by proteomic investigations. Mol Biosyst. 2015;11:1633–43.
Kuragano T, Kuno T, Takahashi Y, Yamamoto C, Nagura Y, Takahashi S, Kanmatsuse K. Comparison of the effects of cellulose triacetate and polysulfone membrane on GPIIb/IIIa and platelet activation. Blood Purif. 2003;21:176–82.
Liu S, Shi W, Liang X, Su Y, Liang Y, Zhang B, et al. Cellulose triacetate dialyzer reduces platelet loss during continuous veno-venous hemofiltration. Blood Purif. 2010;29:375–82.
Grooteman MP, Nube MJ, van Limbeek J, van Houte AJ, Daha MR, van Geelen JA. Biocompatibility and performance of a modified cellulosic and a synthetic high flux dialyzer. A randomized crossover comparison between cellulose triacetate and polysulphon. ASAIO J. 1995;41:215–20.
Hoenich NA, Woffindin C, Matthews JN, Goldfinch ME, Turnbull J. Clinical comparison of high-flux cellulose acetate and synthetic membranes. Nephrol Dial Transplant. 1994;9:60–6.
Sunohara T, Masuda T. Fundamental characteristics of the newly developed ATA membrane dialyzer. Contrib Nephrol. 2017;189:215–21.
Brucke M. Untersuchung zur Sicherheit und Prozessqualität der kontinuierlichen veno-venösen Hämodialyse mit regionaler Citratantikoagulation. 2012. https://www.deutsche-digitale-bibliothek.de/binary/V42N3DPOELLENWHQINNERYJRJOFPLVXZ/full/1.pdf. Accessed 6 Dec 2016.
Burry LD, Tung DD, Hallett D, Bailie T, Carvalhana V, Lee D, et al. Regional citrate anticoagulation for PrismaFlex continuous renal replacement therapy. Ann Pharmacother. 2009;43:1419–25.
Kutsogiannis DJ, Mayers I, Chin WDN, Gibney RTN. Regional citrate anticoagulation in continuous venovenous hemodiafiltration. Am J Kidney Dis. 2000;35:802–11.
Opatrny K, Richtrova P, Polanska K, Wirth J, Sefrna F, Brandl M, Falkenhagen D. Citrate anticoagulation control by ionized calcium levels does not prevent hemostasis and complement activation during hemodialysis. Artif Organs. 2007;31:200–7.
Nipro Corporation. Fineflux FIX product brochure. 2014. http://www.hcmed.com.tw/system/product_files/files/000/000/042/original/finefluxFIX.pdf?1493022452. Accessed 5 Jun 2018.
Boyd RF, Zydney AL. Analysis of protein fouling during ultrafiltration using a two-layer membrane model. Biotechnol Bioeng. 1998;59:451–60.
Baxter Medical AB. Prismaflex ST150 datasheet. 2016. http://www.baxter.se/sv_SE/assets/downloads/products_expertise/multi-organ-support/Prismaflex-ST60_ST100_ST150.pdf. Accessed 5 Jun 2018.
Deppisch R, Storr M, Buck R, Göhl H. Blood material interactions at the surfaces of membranes in medical applications. Sep Purif Technol. 1998;14:241–54.
Acknowledgements
The authors gratefully acknowledge excellent experimental work by Fanny Doss. Part of this work was financially supported by a grant from the Ministry of Education, Science and Culture of the State of Mecklenburg-Vorpommern (Grant number AU 15 002).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The study was financially supported by Nipro Corporation. ATA membrane (SOLACEA™-HF) and PES membrane hemofilters (ELISIO™-HF) were provided by Nipro Corporation. Otherwise, the authors declare that they have no conflicts of interest. The results presented in this paper have not been published previously.
Rights and permissions
About this article
Cite this article
Körtge, A., Wild, T., Heskamp, B. et al. Thrombogenicity and long-term cytokine removal capability of a novel asymmetric triacetate membrane hemofilter. J Artif Organs 21, 435–442 (2018). https://doi.org/10.1007/s10047-018-1062-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10047-018-1062-1