Abstract
Currently, we use the Nipro paracorporeal VAD (p-VAD) for initial short-term ventricular support, as a bridge to decision (BTD) or a bridge to candidacy (BTC) treatment, in Interagency Registry for Mechanically Assisted Circulatory Support (INTERMACS) levels 1 and 2 patients. However, it is possible that compared to patients with primary implantable-VADs (P-iVAD), the bridge-to-bridge (BTB) patients are more likely to develop complications. This retrospective study used data from 24 consecutive BTB patients who were initially implanted with Nipro p-VAD as BTD or BTC treatments between April 2011 and March 2016, and subsequently underwent conversion to an i-VAD. The data from 72 patients who underwent a primary i-VAD (P-iVAD) procedure were used for comparison. Between the two groups, there was no significant difference in the incidence of infectious events (p = 0.72) or stroke (p = 0.44). Orthotropic heart transplantation was performed in 6 of the 24 patients in the BTB group and in 21 of the 72 patients in the P-iVAD group. The 1- and 2-year survival rates were 95.8% and 95.8% in the BTB group and 91% and 85.8% in the P-iVAD group; these values were not significantly different between groups (p = 0.91). Based on these results we conclude that BTB using Nipro p-VAD is a reasonable strategy for treating patients with severe decompensated end-stage heart failure.
Similar content being viewed by others

Avoid common mistakes on your manuscript.
Background
The formulation of effective management strategies for patients categorized as INTERMACS levels 1 and 2 remains the most challenging issue in the field of refractory end-stage heart failure [1]. The Nipro paracorporeal ventricular assist device (p-VAD; Nipro, Osaka, Japan) is one of the two paracorporeal devices approved by the Japanese health insurance, but has many problems with long-term use. A previous report has shown that the survival rate has recently improved recently, but the actual survival rate among patients on Nipro p-VAD support is 66.3% at 6 months and 45.9% at 1 year [2, 3]. Given these outcomes, it is expected that conversion from Nipro p-VAD to implantable VAD (i-VAD) can result in better survival if the procedure is performed safely. Additionally, as patients with i-VAD can be discharged, it is also advantageous in terms of quality of life (QOL) and health economics [3].
At our institute, the Nipro p-VAD has been used for short-to-midterm ventricular support, either as a bridge to decision (BTD) or a bridge to candidacy (BTC) device, in patients with severe decompensated end-stage heart failure. We believe that conversion from Nipro p-VAD to i-VAD, known as the bridge to bridge (BTB) strategy, can provide a safer bridge to transplantation (BTT) for refractory end-stage heart failure. The basic clinical indications for BTB followed at our institute are that the patients display acceptable organ recovery, except for cardiac function, with p-VAD support and have no severe exit site infections. Exit site infection is defined as apparent active findings of infection including fever, redness, swelling, pain, or presence of purulent drainage at the exit site.
However, since there are few studies to support or deny the efficacy of this strategy, the purpose of this study was to analyze whether our indications for BTB in p-VAD patients are acceptable by comparing mortality and morbidity, including infection or stroke, between BTB and P-iVAD patients.
Patients and methods
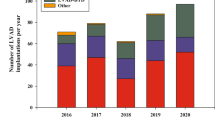
All the subjects enrolled in this study gave informed consent. Between December 2010 and March 2016, 58 patients were implanted with paracorporeal LVADs as BTD or BTC that were configured for aortic perfusion or left ventricle drainage at the University of Tokyo Hospital. Of these patients, we reviewed and retrospectively analyzed the medical records and accompanying data of 24 consecutive BTB patients (2 patients with biventricular p-VAD support) since these patients had undergone BTB procedures for conversion from paracorporeal LVAD to i-VAD. Central ECMO and percutaneous cardiopulmonary support (PCPS) had not been used as BTD or BTC procedures in the subjects selected for this study. We excluded those who were dependent to continuous biventricular VAD support. BTR was performed in 13 patients (22.4%) and a heart transplant in 5 (8.6%). Furthermore, 13 patients (22.4%) died; 3 patients (5.1%) continued with p-VAD and 14 patients (24.1%) needed biventricular VAD (BiVAD) support (Fig. 1). The data on the preoperative parameters, including laboratory, echocardiographic, and hemodynamic data, were obtained before p-VAD implantation and before the BTB procedure.
Additionally, we analyzed data from 72 patients who had undergone a P-iVAD procedure for comparison as controls, and adverse outcomes such as infection, stroke, and death was analyzed between the BTB and P-iVAD groups, based on the data available in the Japanese registry for Mechanically Assisted Circulatory Support (J-MACS). In addition, the freedom from adverse event rate was calculated. The definition of adverse events is described below.
In each patient, wound dressings on the driveline (DL) exit site were changed daily under sterile conditions, and to prevent mechanical trauma at the exit site, an anchor or binder was used to immobilize DL.
Definition of adverse event
Definition of adverse events was based on J-MACS guidelines. A cerebrovascular accident was defined as an ischemic or hemorrhagic intracranial event that persisted for more than 24 h or lasted less than 24 h but with infarction observed on imaging. Device-related infection was categorized as either (1) DL infection, which was localized to the tissue surrounding the DL accompanied by pain, fever, drainage, or leukocytosis, and treated with non-prophylactic antimicrobial agents, or (2) pump pocket infection, which involved tissue surrounding the pump and within the body or mediastinal tissue along the inflow or outflow tracts, coupled with the need for antimicrobial therapy. Sepsis was defined as systemic infection, with or without a device-related infection, as evidenced by positive blood culture and treated with antimicrobial agents. Device malfunction was defined as failure of one or more of the components of mechanical cardiac support device system that directly caused or could potentially induce a state of inadequate circulatory support or death. The data from the J-MACS database (as of June 30th 2016) were used to analyze all the adverse events.
Data analysis
The JMP software, ver. 11, (SAS Institute Inc., Cary, NC, USA) was used to perform the statistical analyzes. Continuous variables were compared using the unpaired t tests or the Wilcoxon rank-sum test, and categorical variables were compared using the Chi-square test. Variables are expressed as mean ± standard deviation or median with interquartile range. The Kaplan–Meier method was used to generate freedom-from-event curves. Statistical significance was defined as p < 0.05.
Results
Status of BTB patients before and after p-VAD implantation
Concomitant support measures such as PCPS (n = 6), intra-aortic balloon pumping (n = 22), ventilator support (n = 11), and continuous hemodiafiltration (n = 2) were used at the time of p-VAD implantation. Table 1 and Fig. 2 provide data on BTB patient demographics before and after p-VAD implantation. Importantly, in BTB patients, p-VAD implantation significantly improved laboratory and hemodynamic parameters, including albumin (Alb), aspartate aminotransferase (AST), alanine aminotransferase (ALT), total bilirubin (T-Bil), C-reactive protein (CRP), B-type natriuretic peptide (BNP), pulmonary artery pressure (PAP), and pulmonary wedge capillary pressure (PCWP), as Table 1 shows. However, p-VAD did not improve echocardiographic data or the cardiac index (CI).
Laboratory, echocardiographic, and hemodynamic parameters of BTB patients obtained at pre and post p-VAD implantation (TP: total protein, Alb albumin, AST aspartate transferase, ALT alanine transferase, γ-GTP gamma glutamyl transpeptidase, T-Bil total bilirubin, BUN blood urea nitrogen, Cre creatinine, CRP C-reactive peptide, BNP B-type natriuretic peptide, LVDd: left ventricle diastolic diameter, LVDs: left ventricle systolic diameter, LVEF: left ventricle ejection fraction, RA right atrial pressure, PAP pulmonary artery pressure, PCWP pulmonary capillary wedge pressure, CI cardiac index)
Patient demographics
Table 2 shows the patient demographics. There were 24 patients in BTB group with a mean age of 38.3 ± 9.3 years and 72 patients in the P-iVAD group with a mean age of 39.1 ± 13.5 years. The HeartMate II (HM II) pump was implanted in 45.8% (11/24) of BTB patients and in 33.3% (24/72) of P-iVAD patients. In addition, Table 2 lists the primary diagnoses; dilated cardiomyopathy was seen in 66.7% (16/24) of BTB patients and 65.2% (47/72) of P-iVAD patients, and the median duration of p-VAD support in BTB patients was 137 days (range 28–606 days). No significant difference was seen in i-VAD support duration between the two groups (691.1 ± 306.6 days in BTB vs. 571.0 ± 356.9 days in P-iVAD). At the time of p-VAD implantation, 14 patients were categorized as INTERMACS profile 1 and 10 as INTERMACS profile 2 in the BTB group. All cases improved to be categorized as INTERMACS profile 3 at the time of conversion. Similarly, in the P-iVAD group, 34 patients with marginal renal function were classified as INTERMACS profile 2 and 36 as INTERMACS profile 3 (p = 0.0014).
Infection
Infections were seen in 54.2% (13/24) of the patients in the BTB group and in 51.4% (37/72) of the patients in the P-iVAD group; incidence was not significantly different between the two groups (p = 0.72; Log rank test; Fig. 3). The freedom-from-infectious-event rate at 1 and 2 years was 51.3 and 41.1% in the BTB group and 52.4 and 36.1% in P-iVAD group, respectively.
In the BTB group, 16.7% (4/24) of the patients required a redo pump exchange. (3 patients of pump-related infection and 1 patient of gastric perforation induced by direct contact of VAD to gastric wall) Whereas there was 8.3% (6/72) of the patients who required a redo pump exchange in the P-iVAD group (3 patients of pump-related infection and 3 patients of DL injury). Regarding pump exchange due to pump-related infection, there was no significant difference between BTB (3/24) and P-iVAD (3/72). (p = 0.14; Chi-square test).
Stroke
Stroke was seen in 16.7% (4/24) of the patients in the BTB group and in 22.2% (16/72) of the patients in the P-iVAD group; this incidence of stroke was not significantly different between the two groups (p = 0.44, Log rank test). The freedom-from-stroke rate at 1 and 2 years was 87.5 and 87.5% in the BTB group and 77.9 and 75.2% in the P-iVAD group, respectively (Fig. 4).
Mortality and transplantation
An orthotropic heart transplant was performed in 25% (6/24) of the patients in the BTB group and in 29.2% (21/72) of the patients in the P-iVAD group. The number of deaths in the BTB group was 3 (12.5%) while that in the P-iVAD group was 7 (9.7%), resulting in 1- and 2-year survival rates of 95.8 and 95.8% in the BTB group and 91 and 85.8% in the P-iVAD group, respectively; these values were not significantly different (p = 0.91 Log rank test; Fig. 5).
Discussion
This study retrospectively analyzed data from a substantial series of BTB patients, initially implanted with Nipro p-VADs as either BTD or BTC options. Before the approval of iVADs, and for a long time in Japan, such patients were forced to wait for donor hearts and were dependent on p-VADs; however, recovery of cardiac function was achieved in some patients. However, currently, these patients have three treatment options, namely, BTB, BTT, and bridge to recovery (BTR).
Despite their initial critical condition, overall survival in Nipro p-VAD patients was not inferior to that of P-iVAD patients, as described in previous reports [2]. The long-term use of Nipro p-VADs is associated with serious complications, including high rates of stroke, driveline infection, and low QOL due to mandatory hospitalization [4, 5]. The results of this study support those reported previously that BTB outcomes are almost equivalent to that of P-iVAD, especially with respect to infection, stroke, and mortality rates. There was no statistically significant difference between two groups regarding pump-related infection requiring a redo pump exchange. These are important issues as they strongly affect the patients’ survival.
Since the backgrounds of the P-iVAD and BTB patients were quite different, it might be hard to compare the two cohorts. However, BTB is considered to be a better option than BTT with p-VAD. Furthermore, there was no statistically significant difference between the groups in terms of the 2-year survival rate. Survival in patients with refractory cardiogenic shock is reported to be lower than in more stable patients, when implanted with an i-VAD [2, 6].
The Impella 2.5 and Impella 5.0 heart pumps (Abiomed, Inc, Danvers, Mass) were covered by Japanese health insurance in 2017 [7]. Catheter-based micro-axial flow pump appears to offer a valid therapeutic option in cardiogenic shock, and thus, may lead more easily to higher level of mechanical circulatory support (MCS) such as i-VAD in the near future. Progressive end organ dysfunction is a hallmark of persistent profound cardiogenic shock [8]. However, recovery from end organ dysfunction cannot be predicted at the time of initial treatment of advanced cardiogenic shock. We believe that paracorporeal VAD such as Nipro p-VAD and centrifugal pump system may be justified as a durable mid-term LVAD for the patients with insufficient organ recovery even with this percutaneous MCS.
The use of i-VADs as destination therapy is expected to be approved, and some of the patients in our cohort would be appropriate candidates for the P-iVAD as BTC strategy. Nonetheless, some of the patients in our cohort presented in critical condition and could not wait until approval of the i-VAD procedure; thus, it is important to use an appropriate device based on general condition and end organ dysfunction, as therapeutic options are increasing.
The most important contraindication for BTB is exit site infection and exit site infection extending to the level of the rectus abdominal muscle is considered as a BTB contraindication in our institute. Another contentious issue is the optimal timing for conversion from p-VAD to i-VAD, and since there are no exact guidelines for this issue, it is advisable to postpone the BTB procedure when patients have an active infection. In our experience, cerebrovascular accidents occurred in 2 patients while waiting for the BTB procedure. Furthermore, in our series, the median duration of p-VAD support was 137 days (28–606 days). Our policy is to observe carefully for 3–4 months after p-VAD implantation along with aggressive medication and cardiac rehabilitation to find out if cardiac function recovers well enough to explant the device [9, 10]. BTB can be performed when acceptable organ recovery is achieved without any exit site infection. The results of this study demonstrate that the general condition of BTB patients improved before BTB surgery, partially because the Nipro p-VAD enabled patients to undergo further rehabilitation compared to patients who were treated with ECMO or PCPS. However, BTR was not a viable treatment option in these patients as their cardiac function did not improve (Table 1; Fig. 2).
It is needless to say that careful dissection and hemostasis are important during the BTB procedure, and it is mandatory to sufficiently debride and close the abdominal muscle and anterior abdominal fascial layers at both exit sites to prevent SSI and pump pocket infection [11]. BTB was indicated exceptionally in 2 cases that aggressive debridement and omentopexy could control infection. One patient had a device infection presenting both exit site infection and bacteremia. We had no choice to explant the device. The other patient was postoperative status of BTR and after treatment of mediastintis. We consider that omentopexy is the last resort, so routine omentopexy is not performed.
Regarding the indication of BTB in Bi-VAD patients in our institute, basic management of Bi-VAD is to wean off the RVAD. After end organ dysfunction has recovered, it is judged whether weaning off is acceptable while periodically lowering the flow rate of RVAD. About the details of our 2 cases, BTB was performed after the RVAD was weaned off in one case. And BTB and explantation of the RVAD were performed concomitantly because the right ventricular function was fully recovered when the heart transplant was indicated in the other case.
Our criteria for BTB with short-term use of Nipro p-VAD might be acceptable as the 1- and 2-year survival rates were excellent at greater than 95%. Despite this, the main limitations of our study are the relatively small cohort of patients involved and its retrospective nature. Due to the small sample number of this study, it was hard to compare BTB patients with those undergoing BTT with p-VAD in a matched setting.
Conclusion
In Japan, the shortage of donor organs is of significant concern and even i-VAD patients have to wait for 3–4 years for a heart transplant. Thus, a BTB procedure is a reasonable strategy that enables the p-VAD patient to be discharged while awaiting a heart transplant. We conclude that BTB using Nipro p-VAD as a BTD or a BTC is a reasonable strategy for treating patients with severe decompensated end-stage heart failure since there were no statistically significant differences in complication rates between BTB and primary iVAD patients.
References
Rousse N, Juthier F, Pincon C, Hysi I, Banfi C, Robin E, et al. ECMO as a bridge to decision: recovery, VAD, or heart transplantation? Int J Cardiol. 2015;187:620–7.
Suwa H, Seguchi O, Fujita T, Murata Y, Hieda M, Watanabe T, et al. Paracorporeal ventricular assist device as a bridge to transplant candidacy in the era of implantable continuous-flow ventricular assist device. J Artif Organs. 2014;17:16–22.
Yoshioka D, Sakaguchi T, Saito S, Miyagawa S, Nishi H, Yoshikawa Y, et al. Initial experience of conversion of Toyobo paracorporeal left ventricular assist device to DuraHeart left ventricular assist device. Circ J. 2012;76:372–6.
Morita S. An old ventricular assist device still working for patients with end-stage heart failure in Japan. Circ J. 2010;75:53–4.
Saito S, Matsumiya G, Sakaguchi T, Fujita T, Kuratani T, Ichikawa H, et al. Fifteen-year experience with Toyobo paracorporeal left ventricular assist system. J Artif Organs. 2009;12:27–34.
Takayama H, Soni L, Kalesan B, Truby LK, Ota T, Cedola S, et al. Bridge-to-decision therapy with a continuous-flow external ventricular assist device in refractory cardioogenic shock of various causes. Circ Heart Fail. 2014;7:799–806.
ABIOMED press release Sep 27,2016. http://investors.abiomed.com/news-releases/news-release-details/abiomed-impella-25tmand-impella-50tm-heart-pumps-receive.
Brown JL, Estep JD. Temporary percutaneous mechanical circulatory support in advanced heart failure. Heart Fail Clin. 2016;12:385–98.
Imamura T, Kinugawa K, Hatano M, Fujino T, Muraoka H, Inaba T, Maki H, Kagami Y, Endo M, Kinoshita O, Nawata K, Kyo S, Ono M. Preoperative beta-blocker treatment is a key for deciding left ventricular assist device implantation strategy as a bridge to recovery. J Artif Organs. 2014;17:23–32.
Kashiwa K, Nishimura T, Saito A, Kubo H, Fukaya A, Tamai H, Yambe T, Kyo S, Ono M. Left heart bypass support with the Rotaflow Centrifugal Pump as a bridge to decision and recovery in an adult. J Artif Organ. 2012;15:207–10.
Yoshitake S, Itoda Y, Nawata K, Iwase T, Hoshino Y, Kimura M,et al. Successful management of apical abscess after Nipro left ventricular assisted device explantation by removal of apical cuff and omentopexy. J Artif Organs. 2016;19:396–8.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
No disclosure on this study.
Rights and permissions
About this article
Cite this article
Yoshitake, S., Kinoshita, O., Nawata, K. et al. Single-center experience of the bridge-to-bridge strategy using the Nipro paracorporeal ventricular assist device. J Artif Organs 21, 405–411 (2018). https://doi.org/10.1007/s10047-018-1053-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10047-018-1053-2