Abstract
The aims of the present investigation, performed in 118 consecutive patients with refractory ARDS treated with veno-venous extracorporeal membrane oxygenation (VV-ECMO), were as follows: (a) to assess ICU mortality in overweight, obese and morbid obese patients in respect to normal weight; (b) to evaluate echocardiographic findings according to BMI subgroups. Echocardiography was performed before VV-ECMO implantation. Forty-five patients (38.1%) showed normal BMI, 37 patients (31.4%) were overweight and the remaining were obese (21.2%), or morbid obese (9.3%). Morbid obese showed the lowest ICU mortality rate (p = 0.003). No differences were detectable among BMI subgroups in echocardiographic findings apart from the fact that obese patients showed the lowest incidence of LV dysfunction (p = 0.015). At stepwise regression analysis the following variables were independent predictor of ICU mortality (when adjusted for age): RV dilatation (OR 4.361, 95 % CI 1.809–10.512, p < 0.001), BMI (OR 0.884, 95% CI 0.821–0.951, p < 0.001). In other terms, the presence of RV dilatation is an independent predictor of ICU mortality. In refractory ARDS treated with VV-ECMO, BMI > 30 kg/m2 is common (accounting for one-third of the entire population) but it is not associated with a worse outcome, so that it cannot be considered per se a contraindication to ECMO implantation. The incidence of RV dilatation and failure, which are known to negatively affect prognosis in ARDS patients, were comparable among BMI subgroups.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Obesity shows an increasing incidence featuring as a global-health problem and obese patients are at higher risk of developing ARDS [1, 2]. In a cohort of critically ill patients, BMI was associated with increased risk of ARDS in a weight dependent manner and with increased length of stay [1]. Moreover, obesity is known to increase cardiac workload, with the development of left ventricle dilatation and/or hypertrophy [3] and increasing BMI has been shown to be associated with increasing severity of right ventricle dysfunction in overweight and obese subjects, without over heart disease [4].
Veno-venous extracorporeal membrane oxygenation (VV-ECMO) is widely applied as supportive treatment in ARDS refractory to conventional therapy [5–7] but few papers investigated the prognostic impact of increased BMI in patients supported by VV-ECMO [8, 9]. Mongero et al. [10] described 2 patients with a BMI greater than 50 kg/m2 who were successfully supported with VV-ECMO, while Swol et al. [11], in their single-center experience, reported that 12 patients with a BMI greater than 35 kg/m2 (7 of whom had a BMI > 40 kg/m2) showed a similar survival to discharge than a cohort of patients with a BMI less than 35 kg/m2 (50 and 51%, respectively). Kon et al. [12], in single-center cohort of 55 patients with ARDS supported with ECMO, found that class III obesity (BMI > 40 kg/m2, 12 patients) was not associated with worse outcome.
Echocardiography has recently proved to be an useful clinical tool in risk stratifying ARDS submitted to VV-ECMO [8, 13, 14]. In 21 patients with refractory ARDS and pulmonary hypertension, survival was associated with LVEF and lower systolic pulmonary arterial pressure [15].
The aims of the present investigation, performed in 118 consecutive patients with refractory ARDS treated with VV-ECMO, were therefore as follows: (a) to assess ICU mortality in overweight, obese and morbid obese patients in respect to normal weight; (b) to evaluate echocardiographic findings according to BMI subgroups.
Materials and methods
In our retrospective observational study we enrolled all patients with refractory ARDS [16] requiring VV-ECMO consecutively admitted to our intensive care unit, which is an ECMO referral center from October 10, 2009 to February 28, 2015. According to our clinical standard operating procedure [15, 17, 18] an echocardiographic exam is performed just before ECMO implantation (Echo ECMO Florence Registry). Data were prospectively recorded and retrospectively analyzed.
Baseline characteristics were collected for all patients and the simplified acute physiology score (SAPS II) score was calculated [19].
Echocardiographic assessment
Echocardiography is performed routinely before ECMO implantation at our ICU by the cardiologist (CL and PB) who is part of our ECMO team which also includes an intensivist, a cardiac surgeon and a perfusionist, all trained on ECMO technique and management. The cardiologist’s main task is to evaluate cardiac function in the pre-ECMO phase and guides the correct positioning of ECMO cannulas by transesophageal/transthoracic ultrasonography [5, 13–15].
According to our protocol [13–15, 17, 18] the echocardiographic examination is transthoracic (TTE), transesophageal (TEE) or both, according to the best acoustic window (Esaote MyLab™30Gold Cardiovascular, Esaote S.p.A, Genoa, Italy) [15]. The LV ejection fraction (LVEF) was estimated by eyeball examination on short-axis views [15, 20, 21]. LV systolic dysfunction was defined as LV ejection fraction less than 45% [15, 22]. The right ventricle size was assessed by the RV end-diastolic area (EDA) (four-chamber view) and the ratio between EDAs of the right and left ventricles was calculated (RVEDA/LVEDA). RV dilatation was defined as RVEDA/LVEDA > 0.6 [15, 23].
Systolic pulmonary artery pressure (sPAP] was obtained using the simplified Bernouilli’s equation: 4 · (Vmax tricuspid regurgitation)2 + central venous pressure (CVP). To reduce the lack of precision of CVP estimation based on the size of the inferior vena cava, CVP was invasively measured through central venous catheters [15, 20].
Tricuspid annular plane excursion (TAPSE) was also measured, as the difference of displacement during diastole and systole. A TAPSE < 16 mm is known to indicate RV dysfunction [15, 24, 25].
The requirement of ECMO implantation was decided on the basis of the Italian Ministry of Health criteria, as previously described [17, 18]. Conditions of severe hypoxia or hypercapnia, where the limits of a protective ventilation strategy could not be maintained (tidal volume less than 6 ml/kg of predictive body weight and plateau pressure of 30 cm H2O), were the indication for starting extracorporeal circulation [17, 18].
Body mass index
Body mass index (BMI) was calculated from height and weight recorded on admission to the ICU (BMI = weight (kg)/ht(m)2). According BMI, in our study population, the following subgroups were considered [26]:
-
(a)
Normal (BMI < 25 kg/m2);
-
(b)
Overweight (BMI > 25 kg/m2 < 30 kg/m2);
-
(c)
Obese (BMI > 30 kg/m2 <40 kg/m2.
-
(d)
Morbid obese (BMI > 40 kg/m2).
The subgroup of patients with normal BMI included also 4 patients who were underweight (that is with a BMI < 18.5 kg/m2).
Outcome
Mortality during ICU stay was the outcome.
All Participants (or their kins) signed a written informed consent for storing their clinical data. The study is a retrospective analysis of data and the study design was approved by our Institutional Board.
Statistical analysis
Statistical analysis has been conducted with SPSS 13.0 for Windows software (SPSS Inc, Chicago, IL, USA) A two-tailed p value <0.05 was considered statistically significant. Categorical variables are reported as frequencies and percentages; continuous variables are reported as mean ± standard deviation (SD). For continuous variables, between-groups comparisons have been performed with Student’s t test or ANOVA (followed by Bonferroni post-tests if overall p was significant) or by means of Kruskal–Wallis H test. Categorical variables have been compared with Chi-square.
Univariate analysis (Chi-squared or Fisher’s exact test for categorical data; Student’s t test or Mann–Whitney U test for continuous data) was used to identify candidate variables (age, gender, BMI, SAP II, pO2, pCo2, pH, LVEF, RV dilatation (RVEDA/LVEDA ration >0.6), TAPSE, sPAP) for multivariate analysis which included those variables that resulted significant at univariate analysis (BMI and RV dilatation). Backward stepwise logistic regression was performed to identify predictors of ICU mortality. Hosmer–Lemeshow goodness-of-fit test and Nagelkerke pseudo-R 2 are reported.
Results
Our population comprises 118 consecutive patients, among whom 69 patients (58.4%) were transferred by peripheral hospitals. All the ECMO transportation were carried out by ambulance and no adverse event was observed. The average distance from the local hospital to our ECMO-center was 77 km (median, range 5–456 km).
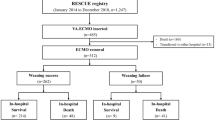
As depicted in Table 1, 45 patients (38.1%) showed normal BMI, 37 patients (31.4%) were overweight and the remaining were obese (21.2%), or morbid obese (9.3%) (Fig. 1). Overweight patients were significantly older than normal weight and morbid obese patients (p < 0.001, and p < 0.001, respectively). Normal weight patients showed higher values of SAPS II in respect to morbid obese (p < 0.01) and to overweight patients (p < 0.05). Morbid obese patients showed the lower ICU mortality rate (p = 0.003). No other difference was detectable among BMI subgroups in baseline characteristics nor in ICU length of stay.
As shown in Table 2, no difference was observed in sPAP and in the incidence of RV dysfunction (as expressed by TAPSE) and RV dilatation among BMI subgroups. Obese patients showed a lower incidence of LV dysfunction than normal weight patients (p = 0.005, Chi square).
At stepwise regression analysis (Table 3) the following variables were independent predictor for ICU mortality (when adjusted for age): RV dilatation (OR 4.361, 95 % CI 1.809–10.512, p < 0.001), BMI (OR 0.884, 95% CI 0.821–0.951, p < 0.001). Hosmer–Lemeshow χ 2 8.49, p = 0.387; Nagelkerke pseudo-R 2 0.297. 8.
Discussion
The main findings of the present investigation, performed in 118 consecutive patients with refractory ARDS treated with VV-ECMO, were as follows: (a) increased BMI (>30 kg/m2) account for one-third (30.5%) of the entire population; (b) no difference in echocardiographic findings were detectable among BMI subgroups except for a lower incidence of LV dysfunction in obese patients; (c) BMI was related with ICU mortality, since increased BMI was associated with a better outcome.
In our series, overweight and obese patients represent the majority of the study population (61.9%), in agreement with previous reports which found a high prevalence of overweight and obesity in ARDS requiring VV-ECMO [27, 28].
Few reports specifically addressed the relationship between BMI and outcome for patients supported with VV-ECMO [9, 10], mainly performed in small series of patients and all documenting that increased BMI was not associated with a worse outcome. Al-Soufi and et al. [29] analyzed all patients supported by VV-ECMO from 2005 to 2011 (International Extracorporeal Life Support Organization Registry) and observed that patients in the highest quartile for body weight showed a trend towards decreased risk-adjusted mortality compared with patients in the lowest quartile. However, in the study by Al-Soufi et al. [29], only body weight (and not BMI) was considered, since the ELSO Registry does not collect patient height. We confirm and extend these findings observing in a large cohort of patients that BMI is associated with ICU mortality and that obese and morbid obese patients showed a significant lower mortality than normal weight patients.
Several hypothesis have been previously proposed to explain this paradoxical protective effect of increased BMI in ARDS, comprising more adequate nutritional stores [30] and immune modulation by the adipose tissue [31]. Kon et al. [12] speculated that morbidly obese offered ECMO showed a less severe parenchymal disease since they had developed early respiratory failure 9 due to chest wall restrictive mechanics. According to our data, echocardiography pre-ECMO implantation may provide other factors which may contribute to this phenomenon. Indeed, in our series, a lower incidence of LV dysfunction was observed in obese patients in respect to normal weight patients. In a recent paper [15] in 21 patients with refractory ARDS and pulmonary vascular dysfunction supported with VV-ECMO higher left ventricular ejection fraction was associated with survival.
Moreover, in our study population, no difference was observed in the incidence of RV dilatation and dysfunction (as indicated by TAPSE) among BMI subgroups. The prognostic role of RV failure in ARDS has been previously documented by others [22–24] and us [15]. In fact in a small subset of patients with refractory ARDS and pulmonary vascular dysfunction, survivors showed higher values of TAPSE, an index of RV function [15].
Limitation of the study
A limitation of the present study may be that this a single-center investigation, thus including a small number of patients, so that the subgroup of underweight patients could not have been analyzed separately since it included only 4 patients. However, this is the largest series of ARDS patients supported by VV-ECMO in whom the prognostic role of BMI was specifically addressed, focusing on echocardiographic findings. LV ejection fraction was calculated by eyeball, a method which can be performed more rapidly and has been shown a good correlation with the Simpson method in critically ill patients [32]. We were not able to adjust for some factors that may be associated with mortality that were not reported in all patients such as tidal volume and plateau pressures of ventilation before ECMO support. However, the aim of the present investigation was to specifically evaluate differences (if any) in echocardiographic findings among BMI subgroups.
Conclusions
According to our findings, in refractory ARDS treated with VV-ECMO, increased BMI (>30 kg/m2) is common and it is not associated with worse outcome, so that it cannot be considered per se a contraindication to ECMO treatment. Echocardiography, performed prior to VV-ECMO implantation, may help in understanding this phenomenon since the incidence of RV dilatation and failure, which are known to negatively affect prognosis in ARDS patients, was comparable among BMI subgroups. Further studies are needed to confirm our findings in a larger cohort of patients.
Abbreviations
- ARDS:
-
Acute respiratory distress syndrome
- BMI:
-
Body mass index
- LV:
-
Left ventricle
- RV:
-
Right ventricle
- sPAP:
-
Systolic pulmonary arterial hypertension
- TAPSE:
-
Tricuspid annular plane excursion
- TTE:
-
Transthoracic echocardiography
- TEE:
-
Transesophageal echocardiography
- VV-ECMO:
-
Veno-venous extracorporeal membrane oxygenation
References
Gong MN, Bajwa EK, Thompson BT, Christiani DC. Body mass index is associated with the development of acute respiratory distress syndrome. Thorax. 2010;65:44–50.
Anzueto A, Frutos-Vivar F, Esteban A, Bensalami N, Marks D, et al, Ventila group. Influence of body mass index on outcome of the mechanically ventilated patients. Thorax. 2011; 66:66–73.
Wong CY, O’Moore-Sullivan T, Leano R, Byrne N, Beller E, Arwick TH. Alterations of left ventricular myocardial characteristics associated with obesity. Circulation. 2004;110:3081–7.
Wong CY, O’Moore-Sullivan T, Leano R, Hukins C, Jenkins C, Marwick TH. Association of subclinical right ventricular dysfunction with obesity. J Am Coll Cardiol. 2006;47:611–6.
Combes A, Brodie D, Bartlett R, Brochard L, Brower R, et al. The international ECMO network (ECMONet). Position paper for the organization of extracorporeal membrane oxygenation programs for acute respiratory failure in adult patients. Am J Respir Crit Care Med. 2014;190:488–96.
Combes A, Ranieri M. Rescue therapy for refractory ARDS should be offered early: yes. Intensive Care Med. 2015;. doi:10.1007/s00134-015-3721-5.
Schmidt M, Hodgson C, Combes A. Extracorporeal gas exchange for acute respiratory failure in adult patients: a systematic review. Crit Care. 2015;19:99. doi:10.1186/s13054-015-0806z.
Schmidt M, Zogheib E, Rozé H, Repesse X, Lebreton G, Luyt CE, et al. The PRESERVE mortality risk score and analysis of long-term outcomes after extracorporeal membrane oxygenation for severe acute respiratory distress syndrome. Intensive Care Med. 2013;39:1704–13.
Schmidt M, Bailey M, Sheldrake J, Hodgson C, Aubron C, Rycus PT, et al. Predicting survival after extracorporeal membrane oxygenation for severe acute respiratory failure. The respiratory extracorporeal membrane oxygenation survival prediction (RESP) score. Am J Respir Crit Care Med. 2014;189:1374–82.
Mongero LB, Beck JR, Charette KA, Stewart A. Respiratory failure of two sp gastric bypass patients and subsequent rescue with extracorporeal membrane oxygenation. Perfusion. 2006;21:73–6.
Swol J, Buchwald D, Dudda M, Strauch J, Schildhauer TA. Veno-venous extracorporeal membrane oxygenation in obese surgical patients with hypercapnic lung failure. Acta Anaesthesiol Scand. 2014;58:534–8.
Kon ZN, Dahi S, Evans CF, Byrnes KA, Bittle GJ, et al. Class III obesity is not a contraindication to venovenous extracorporeal membrane oxygenation support. Ann Thorac Surg. 2015;100:1855–60.
Peris A, Lazzeri C, Cianchi G, Bonizzoli M, Batacchi S, et al. Clinical Significance of echocardiography in patients supported by venous-venous extracorporeal membrane oxygenation. J Artif Organs. 2015;18:99–105.
Lazzeri C, Gensini GF, Peris A. The assessment of cardiac function in veno-venous extracorporeal membrane oxygenation: the emerging role of bedside echocardiography. Heart Lung Vessel. 2015;7:99–100.
Lazzeri C, Cianchi G, Bonizzoli M, Batacchi S, Terenzi P, et al. Pulmonary vascular dysfunction in refractory acute respiratory distress syndrome before veno-venous extracorporeal membrane oxygenation. Acta Anaesthesiol Scand. 2015;. doi:10.1111/aas.12643.
Definition Task Force ARDS, Ranieri VM, Rubenfeld GD, Thompson BT, Ferguson ND, Caldwell E, et al. Acute respiratory distress syndrome: the Berlin Definition. JAMA. 2012;307:2526–33.
Cianchi G, Bonizzoli M, Pasquini A, Bonacchi M, Zagli G, et al. Ventilatory and ECMO treatment of H1N1-induced severe respiratory failure: results of an Italian referral ECMO center. BMC Pulm Med. 2011;11:2. doi:10.1186/1471-2466-11-2.
Ciapetti M, Cianchi G, Zagli G, Greco C, Pasquini A, et al. Feasibility of inter-hospital transportation using extra-corporeal membrane oxygenation (ECMO) support of patients affected by severe swine-flu(H1N1)-related ARDS. Scand J Trauma Resusc Emerg Med. 2011;19:32.
Le Gall JR, Lemeshow S, Saulnier F. A new simplified acute physiology score (SAPS II) based on a European/North American multicenter study. JAMA. 1993;270:2957–63.
Lang R, Badano LP, Mor-Avi V, Afilalo J, Armstrong A, et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American society of echocardiography and the European association of cardiovascular imaging. J Am Soc Echocardiogr. 2015;28:1–39.
Fagnoul D, Pasquier P, Bodson L, Ortiz JA, Vincent JL, et al. Myocardial dysfunction during H1N1 influenza infection. J Crit Care. 2013;28:321–7. doi:10.1016/j.jcrc.2013.01.010.
Boissier F, Katsahian S, Razazi K, Thille AW, Roche-Campo F, et al. Prevalence and prognosis of cor pulmonale during protective ventilation for acute respiratory distress syndrome. Intensive Care Med. 2013;39:1725–33. doi:10.1007/s00134-013-2941-9.
Jardin F, Dubourg O, Bourdarias JP. Echocardiographic pattern of acute cor pulmonale. Chest. 1997;111:209–17.
Khrishnan S, Schmidt GA. Acute right ventricular dysfunction. A real-time management with echocardiography. Chest. 2015;147:835–46.
Lhéritier G, Legras A, Caille A, Lherm T, Mathonnet A, et al. Prevalence and prognostic value of acute cor pulmonale and patent foramen ovale in ventilated patients with early acute respiratory distress syndrome: a multicenter study. Intensive Care Med. 2013;39:1734–42.
Clinical Guidelines on the Identification. Evaluation, and treatment of overweight and obesity in adults. The evidence report. National Inst Health Obes Res. 1998;6:51S–209S.
Brogan TV, Thiagarajan RR, Rycus PT, Bartlett RH, Bratton SL. Extracorporeal membrane oxygenation in adults with severe respiratory failure: a multi-center database. Intensive Care Med. 2009;35:2105–14.
Roch A, Lepaul-Ercole R, Grisoli D, Bessereau J, Brissy O, Astanier M, et al. Extracorporeal membrane oxygenation for severe influenza A (H1N1) acute respiratory distress syndrome: a prospective observational comparative study. Intensive Care Med. 2010;36:1899–905.
Al-Soufi S, Buscher H, Nguyen ND, Rycus P, Nair P. Lack of association between body weight and mortality in patients on veno-venous extracorporeal membrane oxygenation. Intensive Care Med. 2013;39:1995–2002.
Oliveros H, Villamor E. Obesity and mortality in critically ill adults: a systematic review and meta-analysis. Obesity. 2008;16:515–21.
Stapleton RD, Dixon AE, Parsons PE, Ware LB, Suratt BT. The association between BMI and plasma cytokine levels in patients with acute lung injury. Chest. 2010;138:568–77.
Bergenzaun L, Gudmundsson P, Öhlin H, Düring J, Ersson A, et al. Assessing left ventricular systolic function in shock: evaluation of echocardiographic parameters in intensive care. Crit Care. 2011;15:R200. doi:10.1186/cc10368.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lazzeri, C., Bonizzoli, M., Cianchi, G. et al. Body mass index and echocardiography in refractory ARDS treated with veno-venous extracorporeal membrane oxygenation. J Artif Organs 20, 50–56 (2017). https://doi.org/10.1007/s10047-016-0931-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10047-016-0931-8