Abstract
In addition to the well-known traditional risk factors, uremia-related so-called novel risk factors and medications appear to affect coronary artery calcification in hemodialysis patients. This study was performed to evaluate coronary artery calcification score (CACS) in maintenance hemodialysis (MHD) patients, and to identify significantly related factors. We assessed CACS using Agatston Score by MDCT, sex, age, dialysis vintage, presence of diabetes mellitus, smoking history, presence of ≥100 ml urine volume/day, normalized protein catabolic rate, geriatric nutritional risk index, administration of active vitamin D3, cinacalcet, phosphate binders or antihypertensive agents, and circulation parameters including creatinine, albumin, corrected calcium and phosphate in 207 MHD patients. Coronary artery calcifications were observed in 192 patients (92.8 %). In multivariate analysis, CACS showed direct associations with age (p < 0.001), dialysis vintage (p < 0.001) and presence of diabetes mellitus (p < 0.01), and an inverse association only with active vitamin D3 administration (p < 0.001) in MHD patients. Patients with active vitamin D3 showed significantly lower CACS than in those without it (1349.6 ± 1635.0 vs. 2475.6 ± 2646.6 H, p < 0.05). Older age, longer duration of dialysis and diabetes mellitus are risk factors and administration of active vitamin D3 is protective factor for coronary artery calcification in MHD patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Coronary artery calcification is common in chronic kidney disease (CKD) patients, especially in those on dialysis therapy, and is important for increased mortality from cardiovascular complications in such patients [1, 2]. Recent evidence suggests that the interaction of traditional [i.e., age, smoking, diabetes mellitus (DM), hypertension, dyslipidemia] and uremia-related so-called novel cardiovascular risk factors [e.g., hyperphosphatemia, high calcium × phosphorus (Ca × P) product, hyperparathyroidism, oxidative stress, systemic inflammation, protein-energy wasting, asymmetric dimethylarginine, P-cresol, fetuin A] contributes to excessive and accelerated vascular calcification in CKD patients [3]. Strategies to lower the vascular calcification burden in CKD patients should include minimizing risk factors. An animal study demonstrated that calcitriol and paricalcitol were protective against aortic calcification at dosages sufficient to correct secondary hyperparathyroidism, although higher dosages stimulated aortic calcification [4]. Cinacalcet with low-dose active vitamin D attenuated the progression of vascular and aortic valve calcification in 360 hemodialysis patients [5]. However, a large randomized controlled trial in 3883 hemodialysis patients with a 2-year follow-up reported that cinacalcet did not significantly reduce the risk of death or major cardiovascular events in patients with moderate-to-severe secondary hyperparathyroidism who were undergoing dialysis [6]. As far as we know, only 1 human study has provided the results that the chronic hemodialysis patients, those who received higher dose of 1 alfa-hydroxy vitamin D3 (without cinacalcet) experienced a slow progression of aortic arch calcification [7]. But the study had evaluated only 65 patients using plain chest radiography [7]. Non-calcium containing phosphate binders may have favorable impact on vascular calcification compared to calcium-containing phosphate binders [8]. While, it is also reported that phosphate binders in chronic kidney disease patients significantly lowered serum and urinary phosphorus and attenuated progression of secondary hyperparathyroidism, but resulted in progression of coronary artery and abdominal aortic calcification, and it was speculated that phosphate binders could result in an increased availability of free calcium in the intestine [9].
Thus the influence of (traditional and novel) risk factors and medication on coronary artery calcification in maintenance hemodialysis (MHD) patients remains to be elucidated. Use of multidetector computed tomography (MDCT) for evaluating coronary artery disease in patients undergoing dialysis is a useful and non-invasive approach [10]. The objective of the present study was to evaluate CACS using MDCT and to identify risk factors and protective factors in MHD patients.
Patients and methods
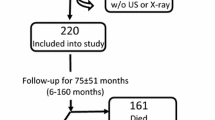
This study included an unselected population of 207 MHD patients, 58 females and 149 males, aged 23–91 years (mean ± SD: 64 ± 14 years). All of the patients underwent routine hemodialysis three times a week (4 h per session) using standard high-flux dialysis membranes. The dialysate contained the following ion concentrations: Na 140, K 2.0, Ca 3.0 and bicarbonate 25.0 mmol/l (NIKKISO, Ishikawa, Japan). Patients with a history of neoplastic disease and active infection were excluded from this study. The patients were informed about the purpose and nature of the study and gave written consent. The study protocol was accepted by Ichiyokai Harada Hospital’s Ethics Committee, Hiroshima, Japan. The presence of past or present smoking, urine volume ≥100 ml/day, DM, antihypertensive agents, active vitamin D3, phosphate binders and cinacalcet use were evaluated. All biochemical samples were drawn before the beginning of a week HD session. Twenty-four-hour urine samples were also collected 1 day before the blood sampling from patients who produced some urine. Bone mineral disorders in all patients were managed according to the treatment guidelines devised by the Japanese Society of Dialysis Therapy (JSDT) [11]. Nutritional status was assessed using normalized protein catabolic rate (nPCR), geriatric nutritional risk index (GNRI) [12], serum albumin and creatinine levels. Imaging techniques comprised the assessment of CACS using Agatston score [13] with MDCT Aquilion 64 TSX-101A (Toshiba Medical Systems, Tokyo, Japan).
Statistical analysis
All statistical analyses were performed with Dr. SPSS II for Windows. The data are expressed as mean ± SD. Differences between groups were assessed using the Mann–Whitney U test or Chi-square test as appropriate. Univariate and multivariate analyses of the factors associated with CACS were performed. Sex (male), age, dialysis vintage, presence of DM, smokers, urine volume ≥100 ml/day, administration of antihypertensives, administration of active vitamin D3, administration of cinacalcet, administration of phosphate binders, hemoglobin, and creatinine, albumin-adjusted calcium (Ca), phosphate (P), iPTH, uric acid, albumin, low-density-lipoprotein cholesterol (LDL-C), β2-microglobulin (β2M), CRP in sera, and nPCR were independent variables for CACS in the univariate analyses. Multivariate analysis was performed using all of the variables that were found to be significantly associated with the CACS in the univariate analyses.
Results
Clinical characteristics of the patients are shown in Table 1. All of the subjects (n = 207) were Japanese, and there were 149 men (72 %) and 58 women (28 %). The mean age and dialysis vintage of all patients were 64 ± 14 years and 94 ± 88 months, respectively. The patients’ underlying diseases included chronic glomerulonephritis in 95 patients (45.9 %), diabetic nephropathy in 72 (34.8 %), hypertensive nephrosclerosis in 19 (9.2 %), autosomal dominant polycystic kidney disease (ADPKD) in 5 (2.4 %), other diseases in 9 (4.3 %) and unknown in 7 (3.4 %). Present or past smokers numbered 83 (40.1 %), and 65 patients (31.4 %) had ≥100 ml urine/day. Antihypertensives were used by 153 patients (73.9 %). Calcium carbonate, sevelamer and/or lanthanum carbonate were used by 139 (67.1 %), 66 (31.9 %) and 49 patients (23.7 %), respectively. Intravenous administrations of maxacalcitol and calcitriol were applied in 59 (28.5 %) and 11 patients (5.3 %), respectively. Oral calcitriol, alfacalcidol and falecalcitriol were used by 22 (10.6 %), 25 (12.1 %) and 2 patients (1.0 %), respectively. The mean dosages of intravenous administration of drugs were as follows: maxacalcitol at 9.0 ± 6.0 μg/week or calcitriol at 1.6 ± 1.2 μg/week. The mean oral calcitriol dosage was 1.9 ± 0.8 μg/week, that for alfacalcidol was 2.4 ± 1.1 μg/week and that for falecalcitriol was 2.1 ± 0 μg/week.
CACS and biochemical characteristics of the patients are shown in Table 2. Coronary artery calcifications were observed in 192 (92.8 %) of the patients. The mean CACS in MHD patients was 1828.3 ± 2191.1 Hounsfield units (H) and 130 out of 207 patients (62.8 %) showed CACS ≥400 H, which corresponds to the highest score according to the algorithm by Agatston et al. [13]. In terms of the mean values, anemia, mineral metabolism such as serum P, serum Ca, Ca × P product, iPTH and lipid metabolism including total cholesterol, HDL-C and LDL-C were well managed in the patients. Means of blood urea nitrogen, serum creatinine, creatinine index, β2M and CRP in sera were also not high in the patients. Mean serum albumin and nPCR were slightly low, but mean GNRI was within normal limits and severe malnutrition was not suggested in the study patients.
The results of univariate and multivariate analyses of the factors associated with CACS in the 207 MHD patients are shown in Table 3. In univariate analysis, age, dialysis vintage, the presence of DM, administration of active vitamin D3, creatinine and albumin in sera were observed to be significantly associated with CACS. In multivariate analysis, only age (β = 0.298, p < 0.001), dialysis vintage (β = 0.321, p < 0.001), presence of DM (β = 0.215, p < 0.01) and the administration of active vitamin D3 (β = −0.234, p < 0.001) remained significant independent factors for CACS in the MHD patients.
Table 4 shows a comparison of characteristics, medications, CACS and biochemical data related to bone mineral disorders in MHD patients with or without administration of active vitamin D3. Patients with administration of active vitamin D3 showed significantly lower CACS compared with patients without it (1349.6 ± 1635.0 vs. 2475.6 ± 2646.6 H, p < 0.05). However, patients with administration of active vitamin D3 showed slightly but significantly higher serum phosphate (5.4 ± 1.3 vs. 4.9 ± 1.4 mg/dl, p < 0.05), Ca × P product (50.0 ± 12.0 vs. 45.9 ± 13.3, p < 0.05) and iPTH (183.0 ± 147.6 vs. 116.6 ± 108.7 pg/ml, p < 0.001) than those without its administration. The frequency of cinacalcet use was significantly higher in patients with active vitamin D3 than in those without it (32 vs. 2 %, p < 0.01). There were no significant differences in age, dialysis vintage, frequency of DM, serum Ca level and the administration of phosphate binders and antihypertensives between the two groups.
Patients with only active vitamin D3 were 87 and patients with active vitamin D3 plus cinacalcet were 32. Compared with patients with only active D3, patients with active vitamin D3 plus cinacalcet showed higher CACS (1112.7 ± 1455.4 vs. 1993.6 ± 1927.1 H, p < 0.05), less frequency of diabetes (36.8 vs. 9.4 %), longer dialysis vintage (73.3 ± 67.1 vs. 165.7 ± 110.7 months, p < 0.001), higher serum phosphate (5.1 ± 1.1 vs. 6.0 ± 1.3 mg/dl, p < 0.01) and higher Ca × P product (47.7 ± 11.1 vs. 56.3 ± 12.2, p < 0.001) in our study. Age (64.0 ± 13.9 vs. 61.0 ± 12.9), administration of phosphate binders or antihypertensives, corrected serum calcium (9.3 ± 0.7 vs. 9.5 ± 0.9 mg/dl) and iPTH (172.6 ± 144.5 vs. 211.2 ± 154.5 pg/ml) were not significantly different in patients with only active vitamin D3 and patients with active vitamin D3 plus cinacalcet in our study.
Discussion
The present study showed high values of CACS (≥400 H) in 62.8 % of the MHD patients, in agreement with many previous reports [14, 15]. Consistent with previous reports [14], age, dialysis vintage and presence of DM were significant risk factors for increased CACS in MHD patients in this study, and we found that the administration of active vitamin D3 was also a significant factor for decreased CACS in MHD patients.
Among traditional risk factors for vascular calcification [3], we failed to find associations between CACS and dyslipidemia, and smoking. Three randomized control trials reported that lipid-lowering treatment was not effective for CVD risk reduction [16]. However, subanalysis of the German Diabetes and Dialysis Study (4D) showed that treatment with a statin significantly reduced composite CVD endpoint by 41 % in a subgroup with LDL-C higher than 145 mg/dl at baseline [17]. Our result that lipid abnormality was not a risk factor for CACS in MHD may have been derived from the lower serum lipid levels including LDL-C (82.0 ± 24.2 mg/dl) in this study. Consistent with our results, Pencak et al. also reported that smoking is not a significant risk factor for CACS in HD patients [3].
Among the many uremia-related so-called novel risk factors, high serum Ca and P levels, and a high serum Ca × P product, as well as secondary hyperparathyroidism, are probably the most important pathogenic factors in vascular calcification, and the transformation of vascular smooth muscle cells into osteoblast-like cells seems to be a key element in the pathogenesis of vascular calcification in the presence of calcium and phosphorus deposition [18, 19]. However, there are several reported studies that failed to demonstrate such a relationship [3, 20, 21], and we also failed to demonstrate significant associations between CACS and serum P, Ca and iPTH in this study. This difference may be due to the serum P level attained and the type and dose of phosphate binders. In the past few years, an improvement of mineral disturbance management has been obtained by dose reduction of calcium carbonate and active vitamin D3, and introduction of sevelamer hydrochloride, lanthanum carbonate and cinacalcet. Thus, serum P, Ca, iPTH and Ca × P product levels were not so high in our patients, as shown in Table 2. As another uremia-related factor, an association between inflammation and CACS has also been reported [3, 20, 21]. CRP and nutritional markers such as serum albumin, serum creatinine, GNRI and nPCR were not determinants of CACS in our study, which may be a result of the strict exclusion criteria.
This study indicated that the administration of active vitamin D3 is protective factor for coronary artery calcification in MHD patients. Consistent with previous report about a slow progression of aortic arch calcification with higher dose of 1 alfa-hydroxy vitamin D3 in hemodialysis patients [7], our results obtained using more accurate CACS with MDCT further support the assertion that active vitamin D3 treatment may have a protective effect against vascular calcification in MHD patients. The beneficial effect of active vitamin D3 on CACS in this study may have been partly due to the low doses of active vitamin D3 [5]. Recently, Lau et al. demonstrated that the administration of active vitamin D3 and its analog decreases aortic calcification in association with increases in two potent calcification inhibitors: the secreted form of Klotho, which in turn enhances phosphaturia correction of hyperphosphatemia, and vascular osteopontin, in mice with CKD [22]. Our human study showed an association between the administration of active vitamin D3 and decreased CACS, but significantly higher serum P levels with significantly higher Ca × P product were observed in patients with the administration of active vitamin D3 than in those without it. Thus, further studies are required to determine whether lower serum P levels with active vitamin D3 derived from increasing Klotho expression may decrease aortic calcification, even in dialysis patients, since the majority of dialysis patients are anuric. A historical cohort study showed definitive evidence that chronic HD patients in the group that received injectable vitamin D3 had a significant survival advantage over patients who did not receive it [23]. It is worth noting that vitamin D-mediated local factors actively mediated the inhibition of vascular calcification [24].
It is reported that treatment with active vitamin D may lower plasma PTH, but often raises serum calcium and/or phosphorus concentrations, changes that have been implicated in the development of cardiovascular calcification in hemodialysis patients [5, 25]. In contrast, cinacalcet reduces plasma PTH while modestly lowering serum calcium and phosphorus concentrations [26]. The effect of active vitamin D plus cinacalcet on vascular calcification was expected [5], but patients with active vitamin D3 plus cinacalcet showed similar corrected serum calcium levels and higher serum phosphate levels with higher CACS compared with patients with active vitamin D3 in our study. We considered that the longer dialysis vintage may affect the higher CACS in patients with active vitamin D3 plus cinacalcet. Furthermore, numbers of patients with active vitamin D3 plus cinacalcet in our study were too small to prove the effect of cinacalcet.
The limitation of this study is that it is a small observational study, and not about intervention study of active vitamin D. Thus, we could not assess the dose–response effect and sort different effects of active vitamin D receptor activators in CACS of MHD patients. We also could not completely exclude sources of bias by the therapeutic agents other than active vitamin D3 in our patients, but the higher frequency of cinacalcet use in patients with active vitamin D group may not largely contribute to low CACS, since only 32 (15.5 %) patients received cinacalcet in our study.
In conclusion, older age, longer duration of dialysis and diabetes mellitus are risk factors and administration of active vitamin D3 is protective factor for coronary artery calcification in MHD patients.
References
Goodman WG, Goldin J, Kuizon BD, et al. Coronary artery calcification in young adults with end-stage renal disease who are undergoing dialysis. N Engl J Med. 2000;342:1478–83.
Zheng CM, Lu KC, Wu CC, Hsu YH, Lin YF. Association of serum phosphate and related factors in ESRD-related vascular calcification. Int J Nephrol. 2011;. doi:10.4061/2011/939613.
Pencak P, Czerwieńska B, Ficek R, et al. Calcification of coronary arteries and abdominal aorta in relation to traditional and novel risk factors of atherosclerosis in hemodialysis patients. BMC Nephrol. 2013;. doi:10.1186/1471-2369-14-10.
Mathew S, Lund RJ, Chaudhary LR, Geurs T, Hruska KA. Vitamin D receptor activators can protect against vascular calcification. J Am Soc Nephrol. 2008;19:1509–19.
Raggi P, Chertow GM, Torres PU, et al. The ADVANCE study: a randomized study to evaluate the effects of cinacalcet plus low-dose vitamin D on vascular calcification in patients on hemodialysis. Nephrol Dial Transplant. 2011;26:1327–39.
Chertow GM, Block GA, Correa-Rotter R, et al. Effect of cinacalcet on cardiovascular disease in patients undergoing dialysis. N Engl J Med. 2012;367:2482–94.
Ogawa T, Ishida H, Akamatsu M, et al. Relation of oral 1alpha-hydroxy vitamin D3 to the progression of aortic arch calcification in hemodialysis patients. Heart Vessel. 2010;25:1–6.
Toussaint ND, Lau KK, Polkinghorne KR, Kerr PG. Attenuation of aortic calcification with lanthanum carbonate versus calcium-based phosphate binders in haemodialysis: a pilot randomized controlled trial. Nephrol (Carlton). 2011;16:290–8.
Drüeke TB, Massy ZA. Phosphate binders in CKD: bad news or good news? J Am Soc Nephrol. 2012;23:1277–80.
Park MY, Choi SJ, Kim JK, et al. Use of multidetector computed tomography for evaluating coronary artery disease in patients undergoing dialysis. Nephrol Carlton. 2011;16:285–9.
Fukagawa M, Yokoyama K, Koiwa F, et al. Clinical practice guideline of chronic kidney disease-mineral and bone disorder. Ther Apher Dial. 2013;17:247–88.
Yamada K, Furuya R, Takita T, et al. Simplified nutritional screening tools for patients on maintenance hemodialysis. Am J Clin Nutr. 2008;87:106–13.
Agatston AS, Janowitz WR, Hildner FJ, et al. Quantification of coronary artery calcium using ultrafast computed tomography. J Am Coll Cardiol. 1990;15:827–32.
Floege J, Ketteler M. Vascular calcification in patients with endstage renal disease. Nephrol Dial Transplant. 2006;19:V59–66.
Ribeiro S, Ramos A, Brandao A, et al. Cardiac valve calcification in haemodialysis patients: role of calcium–phosphate metabolism. Nephrol Dial Transplant. 1998;13:2037–40.
Shoji T, Abe T, Matsuo H, et al. Committee of renal and peripheral arteries, Japan atherosclerosis society: chronic kidney disease, dyslipidemia, and atherosclerosis. J Atheroscler Thromb. 2012;19:299–315.
März W, Genser B, Drechsler C, et al. German diabetes and dialysis study investigators. Atorvastatin and low-density lipoprotein cholesterol in type 2 diabetes mellitus patients on hemodialysis. Clin J Am Soc Nephrol. 2011;6:1316–25.
Shroff R, Long DA, Shanahan C. Mechanistic insights into vascular calcification in CKD. J Am Soc Nephrol. 2013;24:179–89.
Nitta K. Vascular calcification in patients with chronic kidney disease. Ther Apher Dial. 2011;15:513–21.
Nitta K, Akiba T, Suzuki K, et al. Assessment of coronary artery calcification in hemodialysis patients using multi-detector spiral CT scan. Hypertens Res. 2004;27:527–33.
Ohtake T, Ishioka K, Honda K, et al. Impact of coronary artery calcification in hemodialysis patients: risk factors and associations with prognosis. Hemodial Int. 2010;14:218–25.
Lau WL, Leaf EM, Hu MC, et al. Vitamin D receptor agonists increase klotho and osteopontin while decreasing aortic calcification in mice with chronic kidney disease fed a high phosphate diet. Kidney Int. 2012;82:1261–70.
Teng M, Wolf M, Ofsthun MN, et al. Activated injectable vitamin D and hemodialysis survival: a historical cohort study. J Am Soc Nephrol. 2005;16:1115–25.
Zittermann A, Schleithoff SS, Koerfer R. Vitamin D and vascular calcification. Curr Opin Lipidol. 2007;18:41–6.
Fishbane S, Shapiro WB, Corry DB, et al. Cinacalcet HCl and concurrent low-dose vitamin D improves treatment of secondary hyperparathyroidism in dialysis patients compared with vitamin D alone: the ACHIEVE study results. Clin J Am Soc Nephrol. 2008;3:1718–25.
Torres PU. Cinacalcet HCl: a novel treatment for secondary hyperparathyroidism caused by chronic kidney disease. J Ren Nutr. 2006;16:253–8.
Acknowledgments
We thank Dr. Masahiro Ishine and Mr. Kenji Mizuno for the expert imaging techniques. This study was supported by the private foundation of Ichiyokai Harada Hospital.
Conflict of interest
All the authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Nishizawa, Y., Mizuiri, S., Yorioka, N. et al. Determinants of coronary artery calcification in maintenance hemodialysis patients. J Artif Organs 18, 251–256 (2015). https://doi.org/10.1007/s10047-015-0823-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10047-015-0823-3