Abstract
Background
The measurement of hemoglobin (Hb) concentrations in breast cancer by near-infrared spectroscopy is useful for the assessment of responses to neoadjuvant chemotherapy (NAC). However, the chest wall muscles may affect this measurement. We corrected Hb concentrations based on the skin-to-chest wall distance. Corrected Hb was compared with uncorrected Hb as a marker of treatment responses in breast cancer patients.
Methods
We measured total Hb (tHb) in breast cancer using a near-infrared time-resolved spectroscopy system in 10 patients before chemotherapy and after the first and second courses of NAC. To assess the skin-to-chest wall distance and thickness of tumors, ultrasound images were obtained using an ultrasonography probe with the spectroscopic probe. Net tHb (tHbnet) was calculated by subtracting tHb in normal breast tissue from cancer tHb. Patients underwent positron emission tomography with [18F] fluorodeoxyglucose (FDG) before chemotherapy and after the second course of NAC. FDG uptake was evaluated using the maximum standardized uptake value (SUVmax).
Results
tHb, tHbnet, and SUVmax in cancer significantly decreased in the course of chemotherapy. The change in tHbnet was larger than that in tHb. Although a correlation was not observed between the change in tHb and that in SUVmax, a positive correlation was noted between the change in tHbnet and that in SUVmax.
Conclusions
Corrections by the skin-to-chest wall distance in spectroscopy led to the change in Hb concentrations being more similar to that in FDG uptake after NAC in breast cancer. tHbnet has potential as a reliable biomarker of breast cancer.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
1 Introduction
Neoadjuvant chemotherapy (NAC) is the standard treatment for locally advanced breast cancer and a standard option for early breast cancer depending on the histological subtype [1]. Disease-free survival and overall survival are equivalent in patients treated with the same adjuvant or neoadjuvant regimen [1]. However, NAC is a useful treatment for downsizing tumors and increasing breast conservation rates [1, 2]. Previous studies demonstrated that the response to NAC is a predictor of long-term outcomes, and a pathological complete response is associated with improved disease-free survival and overall survival [1, 3].
The accurate assessment of the effects of NAC leads to an appropriate treatment strategy for breast cancer. Ultrasonography and MRI have been used to monitor treatment responses. Ultrasonography is an easy and non-invasive modality; however, fibrotic changes after chemotherapy are difficult to differentiate from residual tumors. The diagnostic accuracy of contrast-enhanced MRI is high. However, the use of contrast media and associated costs make MRI difficult to repeat.
Positron emission tomography (PET) using [18F] fluorodeoxyglucose (FDG) is used for staging, evaluating responses to treatments, and predicting the prognosis of various cancers [4,5,6,7]. FDG-PET is also useful for monitoring treatment responses in breast cancer [8,9,10,11]. The accumulation of FDG depends on the metabolic activity of the lesion and may be a more suitable indicator of therapeutic responses than morphological changes [12,13,14]. FDG uptake has been reported to predict pathological responses [15, 16]. However, FDG-PET is also difficult to repeat because of the high associated costs and radiation exposure.
Near-infrared diffuse optical spectroscopy and diffuse optical tomography have been developed for the detection of primary cancer [17,18,19,20] and monitoring of responses after neoadjuvant chemotherapy in breast cancer [21,22,23,24]. Since these are not expensive procedures and do not expose patients to radiation, frequent measurements are possible.
We measured the optical properties of breast cancer using a near-infrared time-resolved spectroscopy system. We demonstrated that measurements were influenced by the chest wall muscles in a manner that depended on the skin-to-chest wall distance, and to reduce the effects of the chest wall, we proposed a subtraction method [25]. The net hemoglobin (Hb) concentration in cancer was calculated by subtracting Hb in normal breast tissue.
In the present study, Hb in breast cancer was measured in the course of NAC and corrected Hb was compared with uncorrected Hb as a marker of treatment responses. TRS was compared with FDG-PET in monitoring the response of breast cancer to NAC.
2 Patients and methods
2.1 Patient characteristics
We measured optical properties and FDG uptake in 11 patients with breast cancer before and after NAC between April 2014 and October 2016. We excluded one patient whose ultrasonography data were not recorded. We enrolled 10 patients. The mean age of the patients was 50.5 years with a range between 39 and 67 years. Five patients were pre-menopausal and five were post-menopausal. Three patients had more than one tumor. One tumor was excluded because it was mostly occupied by a cystic component. Therefore, we analyzed 10 patients and 14 tumors. The median thickness of tumors was 13.5 mm with a range between 6 and 23 mm. All tumors were invasive ductal carcinoma.
The study protocol was approved by the Ethical Review Committee of Hamamatsu University School of Medicine. All patients provided written informed consent.
2.2 Chemotherapy
Patients received four courses of FEC (fluorouracil 500 mg/m2, epirubicin 100 mg/m2, cyclophosphamide 500 mg/m2, every 3 weeks) followed by four courses of docetaxel or a combination of docetaxel and trastuzumab. One patient received two courses of docetaxel and two courses of FEC instead of docetaxel after four courses of FEC.
The optical properties of cancer were measured before chemotherapy, after the first course, and after the second course of FEC. Patients underwent FDG-PET before chemotherapy and after the second course of FEC. Blood samples were obtained before every course of chemotherapy.
2.3 Near-infrared time-resolved spectroscopy
We used a single-channel time-resolved spectroscopy system with near-infrared light of three wavelengths: 758 nm, 795 nm, and 833 nm (TRS-20SH, Hamamatsu Photonics KK, Hamamatsu, Japan). The principle of the measurements was described in detail previously [25]. The distance between the light source and detector was 3 cm. The absorption coefficient and reduced scattering coefficient were obtained at each wavelength. The concentrations of oxygenated and deoxygenated Hb were calculated from the absorption coefficient at each wavelength after subtracting water and lipid absorption in breast tissue. Because we could not measure the amounts of water and lipid only using three wavelengths, we used the mean values of water and lipid for normal breast tissue, which were 18.7% and 66.1%, respectively [26]. In our prior study, there was no significant difference between the result tHb obtained using the mean values of water and lipid for normal breast tissue and for breast cancer (about 1.6% on average). Based on the result, we calculated tHb concentration in breast cancer using the value for normal breast tissue to simplify the analysis. The concentration of total Hb (tHb) was the sum of the concentrations of oxygenated and deoxygenated Hb.
To assess the skin-to-chest wall distance and thickness of tumors, ultrasound images were obtained using an ultrasonography system (EUB-7500, Hitachi Medical Corporation, Tokyo, Japan) with a linear probe (EUP-L65, Hitachi Medical Corporation). The spectroscopic probe was attached to the ultrasound probe in a rectangular direction. A skin-to-chest wall distance of more than 36 mm was assumed to be 37 mm in one patient because the maximal depth was initially set at 36 mm. A previous study revealed that when the skin-to-chest wall distance was 20 mm or more, the influence of the chest wall was negligible and the tHb concentration was constant.
We measured tHb prior to the treatment, 3 weeks after the first infusion of FEC, and 3 weeks after the second infusion of FEC. The spectroscopic probe attached to the ultrasound probe was lightly placed above the tumor, and optical parameters and ultrasound images were obtained. The optical parameters of normal breast tissue were measured in the contralateral breast.
We defined net tHb (tHbnet) by subtracting tHb in normal breast tissue at the same skin-to-chest wall distance as cancer from tHb in cancer. tHb in normal breast tissue was obtained from fitting curves of tHb concentrations as a function of the skin-to-chest wall distance. Curves were generated in our previous study [25].
Changes in tHb and tHbnet were shown by the percentage of the change between the baseline and post-chemotherapy.
2.4 FDG-PET
After fasting for at least 6 h, patients received an intravenous injection of FDG (4.0 MBq/kg). None of the patients had blood glucose levels that exceeded 200 mg/dl. After a 60-min uptake period, image acquisition was performed using a PET system combined with a 16-slice CT scanner (TruePoint Biograph16, Siemens Healthineers, Erlangen, Germany). Tumor FDG uptake was quantified by the maximum standardized uptake value (SUVmax). FDG-PET was evaluated prior to the treatment and 3 weeks after the second infusion of FEC. The change in SUVmax was shown by the percentage of the change between the baseline and post-therapy.
2.5 Statistical analysis
Statistical analyses were performed using Microsoft Excel (Microsoft Corporation, Redmond, WA, USA) and StatFlex version 6.0 (Artech Co., Ltd., Osaka, Japan). Differences in blood Hb and SUVmax in cancer before and after two courses of chemotherapy were assessed using the Wilcoxon signed-rank test. Differences between tHb and tHbnet before chemotherapy, after one course, and after two courses of chemotherapy in cancer were evaluated using Dunn’s test. Pearson’s correlation coefficient analysis and simple regression were used to assess the relationship between ΔtHb and ΔSUVmax and between ΔtHbnet and ΔSUVmax. Differences in the correlation coefficients of the regression lines obtained from ΔtHb and ΔtHbnet were assessed by testing the t value. P < 0.05 was considered to be significant.
3 Results
tHb in normal breast tissue plotted on the reference curve obtained from our previous study (Fig. 1). Baseline blood Hb was 13.1 g/dl (median) and decreased to 11.5 g/dl (median) after two courses of FEC (P < 0.01). However, breast tHb did not significantly decrease after two courses of FEC. Cancer tHb plotted above the curve, even after two courses of FEC (Fig. 2).
tHb of normal breast tissue in pre-menopausal patients (a) and post-menopausal patients (b). The reference curve was obtained from our previous study [25]. tHb at the baseline and after one and two courses of chemotherapy plotted on the curve
tHb of breast cancer in pre-menopausal patients (a) and in post-menopausal patients (b). The reference curve represents the tHb of normal breast tissue obtained in our previous study [25]. The tHb of all cancers plotted above the curve
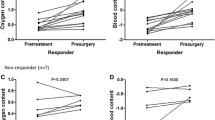
Although the decrease in tHb in cancer was small after one course of chemotherapy, tHbnet in cancer significantly decreased (P < 0.05) (Fig. 3). tHb and tHbnet in cancer both decreased after two courses (P < 0.01). ΔtHb between the baseline and after two courses of chemotherapy was − 14.7 ± 8.2% (mean ± SD) and ΔtHbnet was − 40.0 ± 13.1% (mean ± SD). The change in tHbnet was significantly larger than that in tHb (P < 0.001). SUVmax in cancer decreased after two courses of chemotherapy (P < 0.001) (Fig. 4). The thickness of the tumor also decreased after two courses of chemotherapy (P < 0.01) (Fig. 5).
A correlation was not observed between ΔtHb and ΔSUVmax. On the other hand, a positive correlation was noted between ΔtHbnet and ΔSUVmax (P < 0.05) (Fig. 6). The regression coefficient of the ΔtHbnet regression was slightly larger than that of ΔtHb.
4 Discussion
We herein proposed tHbnet, which reflects the skin-to-chest wall distance. Since tHbnet is calculated by subtracting tHb in normal breast tissue from cancer tHb, tHb in normal breast tissue is essential. tHb was lower in post-menopausal patients than in pre-menopausal patients; therefore, we used reference curves for pre- and post-menopausal patients individually [25]. tHb in normal breast tissue in the present study plotted on the lines that were generated in our previous study, showing the reliability of the curves. Although blood Hb decreased after chemotherapy, tHb in normal breast tissue did not change after two courses of chemotherapy. Spectroscopy may not be sensitive for small changes in blood Hb. No significant differences between pre- and post-chemotherapy, suggesting that it is justifiable to apply the same curves before and after two courses of chemotherapy. However, tHb in normal breast tissue may decrease after several courses of NAC. Therefore, we need to carefully observe tHb in normal breast tissue when we apply this subtraction method to that situation.
All cancer cases had tHb above the reference curves, which coincided with the previous study. In the course of chemotherapy tHbnet showed a stronger correlation with FDG uptake than uncorrected tHb. The decrease observed in tHbnet, even after the first course of NAC, and the positive correlation between the change in tHbnet and that in FDG uptake indicate that tHbnet is a good marker of treatment responses. FDG-PET shows glycolytic activity in cancer, while Hb concentrations reflect blood volumes. Spectroscopy is more easily performed than FDG-PET and may provide a different aspect of proliferation other than glycolytic activity.
There were some limitations in the present study. The number of patients was small. Furthermore, we did not compare changes in tHb or tHbnet with pathological changes. Difficulties are associated with performing an interim pathological examination. FDG-PET was instead used as the comparison.
Previous studies showed that FDG-PET predicts responses to neoadjuvant chemotherapy in breast cancer [8,9,10,11]. Another limitation is that we assumed that the water and lipid contents of cancer were constant. To calculate Hb accurately, we need to assess the water and lipid contents of cancer patients individually. We have recently developed a spectroscopic device that used six wavelengths (762 nm, 802 nm, 838 nm, 908 nm, 936 nm and 976 nm) to measure water and lipid contents in addition to tHb concentration [27]. We are planning to conduct measurement with this system.
In conclusion, corrections by the skin-to-chest wall distance in spectroscopy resulted in the change in Hb concentrations being more similar to that in FDG uptake after NAC in breast cancer. tHbnet has potential as a reliable biomarker of breast cancer.
Change history
14 December 2022
A Correction to this paper has been published: https://doi.org/10.1007/s10043-022-00775-8
References
Kaufmann, M., Hortobagyi, G.N., Goldhirsch, A., Scholl, S., Makris, A., Valagussa, P., Blohmer, J.U., Eiermann, W., Jackesz, R., Jonat, W., Lebeau, A., Loibl, S., Miller, W., Seeber, S., Semiglazov, V., Smith, R., Souchon, R., Stearns, V., Untch, M., von Minckwitz, G.: Recommendations from an international expert panel on the use of neoadjuvant (primary) systemic treatment of operable breast cancer: an update. J. Clin. Oncol. 24(12), 1940–1949 (2006). https://doi.org/10.1200/jco.2005.02.6187
Mieog, J.S., van der Hage, J.A., van de Velde, C.J.: Preoperative chemotherapy for women with operable breast cancer. Cochrane Database Syst. Rev. 2, CD005002 (2007). https://doi.org/10.1002/14651858.CD005002.pub2
Kong, X., Moran, M.S., Zhang, N., Haffty, B., Yang, Q.: Meta-analysis confirms achieving pathological complete response after neoadjuvant chemotherapy predicts favourable prognosis for breast cancer patients. Eur. J. Cancer (Oxford, England). 47(14), 2084–2090 (2011 (1990). https://doi.org/10.1016/j.ejca.2011.06.014
Antoch, G., Saoudi, N., Kuehl, H., Dahmen, G., Mueller, S.P., Beyer, T., Bockisch, A., Debatin, J.F., Freudenberg, L.S.: Accuracy of whole-body dual-modality fluorine-18-2-fluoro-2-deoxy-d-glucose positron emission tomography and computed tomography (FDG-PET/CT) for tumor staging in solid tumors: comparison with CT and PET. J. Clin. Oncol. 22(21), 4357–4368 (2004). https://doi.org/10.1200/jco.2004.08.120
Fletcher, J.W., Djulbegovic, B., Soares, H.P., Siegel, B.A., Lowe, V.J., Lyman, G.H., Coleman, R.E., Wahl, R., Paschold, J.C., Avril, N., Einhorn, L.H., Suh, W.W., Samson, D., Delbeke, D., Gorman, M., Shields, A.F.: Recommendations on the use of 18F-FDG PET in oncology. J. Nucl. Med. 49(3), 480–508 (2008). https://doi.org/10.2967/jnumed.107.047787
Weber, W.A.: Use of PET for monitoring cancer therapy and for predicting outcome. J. Nucl. Med. 46(6), 983–995 (2005)
Weber, W.A., Figlin, R.: Monitoring cancer treatment with PET/CT: does it make a difference? J. Nucl. Med. 48(Suppl 1), 36 s–44 (2007) s
Wahl, R.L., Jacene, H., Kasamon, Y., Lodge, M.A.: From RECIST to PERCIST: evolving considerations for PET response criteria in solid tumors. J. Nucl. Med. 50(Suppl 1), 122 s–150 (2009). https://doi.org/10.2967/jnumed.108.057307 s ).
Mghanga, F.P., Lan, X., Bakari, K.H., Li, C., Zhang, Y.: Fluorine-18 fluorodeoxyglucose positron emission tomography-computed tomography in monitoring the response of breast cancer to neoadjuvant chemotherapy: a meta-analysis. Clin. Breast Cancer. 13(4), 271–279 (2013). https://doi.org/10.1016/j.clbc.2013.02.003
Duch, J., Fuster, D., Munoz, M., Fernandez, P.L., Paredes, P., Fontanillas, M., Guzman, F., Rubi, S., Lomena, F.J., Pons, F.: 18F-FDG PET/CT for early prediction of response to neoadjuvant chemotherapy in breast cancer. Eur. J. Nucl. Med. Mol. Imaging. 36(10), 1551–1557 (2009). https://doi.org/10.1007/s00259-009-1116-y
Kumar, A., Kumar, R., Seenu, V., Gupta, S.D., Chawla, M., Malhotra, A., Mehta, S.N.: The role of 18F-FDG PET/CT in evaluation of early response to neoadjuvant chemotherapy in patients with locally advanced breast cancer. Eur. Radiol. 19(6), 1347–1357 (2009). https://doi.org/10.1007/s00330-009-1303-z
Wahl, R.L., Zasadny, K., Helvie, M., Hutchins, G.D., Weber, B., Cody, R.: Metabolic monitoring of breast cancer chemohormonotherapy using positron emission tomography: initial evaluation. J. Clin. Oncol. 11(11), 2101–2111 (1993). https://doi.org/10.1200/jco.1993.11.11.2101
Chen, L., Yang, Q., Bao, J., Liu, D., Huang, X., Wang, J.: Direct comparison of PET/CT and MRI to predict the pathological response to neoadjuvant chemotherapy in breast cancer: a meta-analysis. Sci. Rep. 7(1), 8479 (2017). https://doi.org/10.1038/s41598-017-08852-8
Pahk, K., Kim, S., Choe, J.G.: Early prediction of pathological complete response in luminal B type neoadjuvant chemotherapy-treated breast cancer patients: comparison between interim 18F-FDG PET/CT and MRI. Nucl. Med. Commun. 36(9), 887–891 (2015). https://doi.org/10.1097/mnm.0000000000000329
Andrade, W.P., Lima, E.N., Osorio, C.A., do Socorro Maciel, M., Baiocchi, G., Bitencourt, A.G., Fanelli, M.F., Damascena, A.S., Soares, F.A.: Can FDG-PET/CT predict early response to neoadjuvant chemotherapy in breast cancer? Eur. J. Surg. Oncol. 39(12), 1358–1363 (2013). https://doi.org/10.1016/j.ejso.2013.08.025
Ueda, S., Saeki, T., Shigekawa, T., Omata, J., Moriya, T., Yamamoto, J., Osaki, A., Fujiuchi, N., Misumi, M., Takeuchi, H., Sakurai, T., Tsuda, H., Tamura, K., Ishida, J., Abe, Y., Imabayashi, E., Kuji, I., Matsuda, H.: 18F-fluorodeoxyglucose positron emission tomography optimizes neoadjuvant chemotherapy for primary breast cancer to achieve pathological complete response. Int. J. Clin. Oncol. 17(3), 276–282 (2012). https://doi.org/10.1007/s10147-011-0287-2
Tromberg, B.J., Pogue, B.W., Paulsen, K.D., Yodh, A.G., Boas, D.A., Cerussi, A.E.: Assessing the future of diffuse optical imaging technologies for breast cancer management. Med. Phys. 35(6), 2443–2451 (2008). https://doi.org/10.1118/1.2919078
Ueda, Y., Yoshimoto, K., Ohmae, E., Suzuki, T., Yamanaka, T., Yamashita, D., Ogura, H., Teruya, C., Nasu, H., Ima, E., Sakahara, H., Oda, M., Yamashita, Y.: Time-resolved optical mammography and its preliminary clinical results. Technol. Cancer Res. Treat. 10(5), 393–401 (2011). https://doi.org/10.7785/tcrt.2012.500217
Fantini, S., Sassaroli, A.: Near-infrared optical mammography for breast cancer detection with intrinsic contrast. Ann. Biomed. Eng. 40(2), 398–407 (2012). https://doi.org/10.1007/s10439-011-0404-4
Wu, T., Feng, J.C., Tuerhong, S., Wang, B., Yang, L., Zhao, Q., Dilixiati, J., Xu, W.T., Zhu, L.P.: Ultrasound-guided diffuse optical tomography for differentiation of benign and malignant breast lesions: a meta-analysis. J. Ultrasound Med. 36(3), 485–492 (2017). https://doi.org/10.7863/ultra.16.03063
Ueda, S., Yoshizawa, N., Shigekawa, T., Takeuchi, H., Ogura, H., Osaki, A., Saeki, T., Ueda, Y., Yamane, T., Kuji, I., Sakahara, H.: Near-infrared diffuse optical imaging for early prediction of breast cancer response to neoadjuvant chemotherapy: a comparative study using 18F-FDG PET/CT. J. Nucl. Med. 57(8), 1189–1195 (2016). https://doi.org/10.2967/jnumed.115.167320
Nakamiya, N., Ueda, S., Shigekawa, T., Takeuchi, H., Sano, H., Hirokawa, E., Shimada, H., Suzuki, H., Oda, M., Osaki, A., Saeki, T.: Clinicopathological and prognostic impact of imaging of breast cancer angiogenesis and hypoxia using diffuse optical spectroscopy. Cancer Sci. 105(7), 833–839 (2014). https://doi.org/10.1111/cas.12432
Tromberg, B.J., Zhang, Z., Leproux, A., O’Sullivan, T.D., Cerussi, A.E., Carpenter, P.M., Mehta, R.S., Roblyer, D., Yang, W., Paulsen, K.D., Pogue, B.W., Jiang, S., Kaufman, P.A., Yodh, A.G., Chung, S.H., Schnall, M., Snyder, B.S., Hylton, N., Boas, D.A., Carp, S.A., Isakoff, S.J., Mankoff, D.: Predicting responses to neoadjuvant chemotherapy in breast cancer: ACRIN 6691 trial of diffuse optical spectroscopic imaging. Cancer Res. 76(20), 5933–5944 (2016). https://doi.org/10.1158/0008-5472.can-16-0346
Zhi, W., Liu, G., Chang, C., Miao, A., Zhu, X., Xie, L., Zhou, J.: Predicting treatment response of breast cancer to neoadjuvant chemotherapy using ultrasound-guided diffuse optical tomography. Transl. Oncol. 11(1), 56–64 (2018). https://doi.org/10.1016/j.tranon.2017.10.011
Yoshizawa, N., Ueda, Y., Nasu, H., Ogura, H., Ohmae, E., Yoshimoto, K., Takehara, Y., Yamashita, Y., Sakahara, H.: Effect of the chest wall on the measurement of hemoglobin concentrations by near-infrared time-resolved spectroscopy in normal breast and cancer. Breast Cancer (Tokyo, Japan). 23(6), 844–850 (2016). https://doi.org/10.1007/s12282-015-0650-7
Cerussi, A., Shah, N., Hsiang, D., Durkin, A., Butler, J., Tromberg, B.J.: In vivo absorption, scattering, and physiologic properties of 58 malignant breast tumors determined by broadband diffuse optical spectroscopy. J. Biomed. Opt. 11(4), 044005 (2006). https://doi.org/10.1117/1.2337546
Ohmae, E., Yoshizawa, N., Yoshimoto, K., Hayashi, M., Wada, H., Mimura, T., Suzuki, H., Homma, S., Suzuki, N., Ogura, H., Nasu, H., Sakahara, H., Yamashita, Y., Ueda, Y.: Stable tissue-simulating phantoms with various water and lipid contents for diffuse optical spectroscopy. Biomed. Opt. Express. 9(11), 5792–5808 (2018). https://doi.org/10.1364/BOE.9.005792
Acknowledgements
This study was partly supported by JSPS KAKENHI Grant numbers 15K19781, 26282144 and 17H03591.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
S. Ueda has research funding from Hamamatsu Photonics K.K. T. Saeki received honoraria for a speech from Ono Pharmaceutical Co., Ltd., Kyowa Hakko Kirin Co., Ltd., Taiho Pharmaceutical Co., Ltd., and Novartis Pharma K.K., T. Saeki has research funding from Ono Pharmaceutical Co., Ltd., Kyowa Hakko Kirin Co., Ltd., Taiho Pharmaceutical Co., Ltd., and Chugai Pharmaceutical Co., Ltd. H. Sakahara has research funding from Hamamatsu Photonics K.K. Y. Ueda, K. Yoshimoto, T. Mimura, E. Ohmae, and H. Wada are employees of Hamamatsu Photonics K.K. No other potential conflict of interest relevant to this article was reported.
Additional information
The original publication has been revised due to errors in Equations appearing Sections 2.3 and 2.4.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Asano, Y., Yoshizawa, N., Ueda, Y. et al. Correction by the skin-to-chest wall distance in near-infrared spectroscopy and assessment of breast cancer responses to neoadjuvant chemotherapy. Opt Rev 26, 111–117 (2019). https://doi.org/10.1007/s10043-018-0486-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10043-018-0486-4