Abstract
Background
Hernia repairs are a commonly performed surgical procedure and the Shouldice Repair of inguinal hernias has been well described before in terms of its outcomes. However, the purpose of this paper was to understand what experts from Shouldice Hospital consider to be the essential steps to the Shouldice Method.
Methods
Utilizing a Delphi Methodology, surgeons at Shouldice Hospital who are considered content experts, provided their answers on what is essential to the Shouldice Method. The median, interquartile range, and percent agreement from the responses as well as the Delphi’s overall Cronbach’s Alpha were determined. All Delphi items were ranked on a five-point Likert scale and consensus was reached when Cronbach’s Alpha was ≥ 0.8. The items from the survey that ranked as 5-completely agree or 4-partially agree by ≥ 80% of participants on the five-point Likert scale were included in the final framework.
Results
The final consensus for the Shouldice Method included 39 items with 7 overarching steps: preoperative preparation of the patient, anesthetic component, incision and nerve identification, treatment of the cremasteric muscles, hernia identification and treatment, reconstruction of the posterior wall, and post-operative management of patients.
Conclusion
The results of this consensus provide a step-by-step approach to the Shouldice Method, as well as information that is timely and can be utilized by surgeons incorporating non-mesh hernia repairs into their practice.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Inguinal herniorrhaphy is a commonly completed surgical procedure and performed globally more than 20 million times annually [1]. There have been various types of repairs described over the years utilizing both open and laparoscopic techniques [2]. Specifically, from an open approach both tissue and mesh repair procedures have been documented, such as the Lichtenstein, McVay, Bassini, and Shouldice [2].
The most frequently observed post-operative outcomes in hernia surgery have been recurrence rates, chronic pain, and more recently quality of life measures [3, 4]. Each type of repair has varying published outcomes in these regards. Nevertheless, the most widely accepted and commonly documented tissue repair has been the Shouldice Repair. The current HerniaSurge guidelines recommend the Shouldice technique in non-mesh inguinal hernia repairs [1].
The steps and history of the Shouldice Repair have been described in many papers over the years [5,6,7,8]. This paper however, intends to provide a clear, concise, and consistent technical framework from Shouldice Hospital surgeons, who themselves have completed a large number of procedures utilizing the Shouldice Method. We feel this is important, as published outcomes of the Shouldice Repair have varying results in the literature [7, 9, 10]. Although this is likely multifactorial, one feature not to be overlooked is that the technique may not be completely followed and that perhaps modifications are being made [9, 11].
Therefore, the objective of this paper was to understand what expert surgeons from the Shouldice Hospital consider essential to the Shouldice Method as it relates to repairing primary inguinal hernias, as well as provide an original consensus paper on the Shouldice Method. In this paper, the Shouldice Method encompasses the technical steps as well as patient care.
Methods
Delphi technique
The Delphi technique is a commonly known and widely used technique for achieving consensus among a group of experts [12], particularly in health-related research [13]. The four pillars of the Delphi technique are: anonymous participation, iterations with interim feedback, the use of experts and statistical aggregation [14,15,16].
Expert participants
An invitation to participate in this project was sent to surgeons at Shouldice Hospital that had worked or were still working at the hospital from January 2016 to August 2021. These individuals were deemed as experts and invited to participate if they had each performed at least 1000 repairs. Regardless of previous experience and education, each new surgeon at Shouldice Hospital undergoes prescribed training to understand and familiarize themselves with the appropriate repair technique. Study participation was voluntary, anonymous to the other Delphi recipients, and the data was coded for analysis to further guard participant identity.
Administration of the Delphi
The study survey was designed using the Delphi technique methodology [17] and sent to participants utilizing a web-based survey tool (Simple Survey version 5.10.0 available at https://www.simplesurvey.com). The Delphi was created using previous publications written by Shouldice Hospital surgeons and after careful review and consensus discussion, by the authors, of which items to include in the preliminary Delphi.
There were two rounds of the Delphi sent to participants and only those that answered the first round were sent the second. The first Delphi contained 48 items all under the seven key overarching steps and the second Delphi had 49 items under the same key steps. The second Delphi provided the participants with the median, interquartile range, as well as any additional items brought up by participants in the first round. All of the questions were asked in both the first and second Delphi with the addition of one question in the second, which was regarding the opening of the transversalis fascia (step 6d). The participants received two email reminders and the second round was sent out 1 month after the first.
Ranking and determination of consensus
All Delphi items were ranked on a five-point Likert scale and consensus was reached when Cronbach’s Alpha was ≥ 0.8. The Cronbach’s alpha value of 0.8 was chosen because it is considered to be the ideal value and falls between the 0.7 level that is acceptable [18] and 0.95 which can indicate redundancy [19]. The Cronbach’s alpha can be used for its ability to evaluate the reliability of data collected through the Delphi and be informative for discussing the consistency of the items within the Delphi [20]. For the purposes of this paper, Cronbach’s alpha is used to indicate the level of consistency in responses by the expert participants. As Alpha approaches 1.0 there is consistency in the responses of participants which suggests consensus [20].
Framework inclusion
Once consensus was achieved by the participants for the Delphi (Cronbach’s alpha ≥ 0.80), the final framework was determined by assessing each sub-step for positive, negative, or neutral agreement. Each sub-step was ranked 1 (completely disagree), 2 (partially disagree), 3 (neutral), 4 (partially agree), and 5 (completely agree) by participants. The items ranked on the 5-point Likert Scale as 5 or 4 by ≥ 80% of participants were included in the final framework [22] as this indicated a positive consensus had been reached [17, 22, 23]. The Likert Scale ratings of 1 and 2 were indicative of a negative consensus and ratings of 3 presented a neutral consensus, therefore these ratings were not included in the final framework [17].
Statistical analysis
Results from the Delphi were gathered, deidentified, and inputted into Microsoft Excel (2019). The median, interquartile range, and percent agreement were completed in excel and the overall Cronbach’s Alpha was determined using the statistical software R 2021 (R: A Language and Environment for Statistical Computing, R Foundation for Statistical Computing, Vienna, Austria) [24].
Results
Participants
Thirteen participants were invited to participate in round 1 and the eleven that submitted responses participated in round 2. The median number of surgeries for the surgeons who took part in the Delphi was around 7000. On average the expert participants completed 600–700 surgeries per year at the Shouldice Hospital.
Consensus framework on operative steps
The final framework of the Shouldice Method was made up of seven key steps (Table 1) and 39 elements within these steps. The Cronbach’s alpha increased by 0.03 between the two Delphi iterations. The overall consensus was found to have a Cronbach’s alpha of 0.81. The results of the second Delphi and what is included in the final framework of the Shouldice Method can be found in Table 2.
Discussion
Using a consensus-based methodology we clarified and explained through the perspective and collective knowledge of Shouldice Hospital experts what the essential steps are for a Shouldice Method. The information provided here is important for those that wish to understand, perform and incorporate the Shouldice Method into their practice with the expectations of appropriate outcomes.
Step one of the Shouldice Method is the preoperative preparation of the patient, and this includes the clinical diagnosis of an inguinal hernia, patient prehabilitation, preoperative weight control, and setting patient expectations.
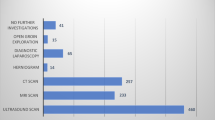
The participating experts had agreed that clinical diagnosis is the preferred method to determine the presence of a hernia in the context of undergoing surgery and when using the Shouldice Method. In their experience results from ultrasound or MRI can be misinterpreted, would not change the management plan (outside of specific circumstances or recurrent presentation), and are often unreliable for diagnosing hernias in the absence of an appropriate history and physical examination. Some of the experts in this project suggested that in certain and specific circumstances, such as multiple recurrences or when there is clinical uncertainty, the use of diagnostic imaging may be of use in combination with physical examination. This experience is concurrent with the current HerniaSurge guidelines [1] as well as findings in the literature [26,27,28,29,30,31].
General patient prehabilitation includes optimizing patient comorbidities as well as improving baseline fitness and exercise tolerance. The consensus among this group of experts on general prehabilitation and weight control preoperatively was that any improvements are beneficial and important to the Shouldice Method. Across a variety of surgical procedures prehabilitation and weight reduction are seen as a benefit in preparing the patient for surgery as well as recovery afterwards [32,33,34,35,36,37]. The use of prehabilitation and weight reduction at Shouldice Hospital has been referenced for many years [5, 7, 8, 38,39,40].
To set patient expectations involves an explanation of the operative steps of the Shouldice Method, risks, benefits and alternatives, as well as the patient process from admission to discharge. This detailed communication is not unique to Shouldice Hospital but has been apart of the patient care for many years and is considered important by experts to the Shouldice Method. A study done in 2019 on cancer patients undergoing surgery [41], concluded that the standard of care should include preoperative patient orientation to minimize anxiety. Other studies also presented lowered anxiety, as well as higher satisfaction and better prognosis due to preoperative patient education [42,43,44].
Not included in the final framework were the recommendations to stop or reduce tobacco, cannabis, and alcohol use prior to surgery because they are not unique to the Shouldice Hospital. These recommendations are commonly made [45,46,47] and the experts here believe they should be followed but that it is also important to consider the essentiality of a repair regardless of adherence to these recommendations, as well as to work with patients through compromise and informed consent when making decisions.
Step two of the Shouldice Method is the anesthetic component
The experts in this project reached consensus and remarked that the use of local anesthesia is essential to the Shouldice Method and they agreed that the use of local anesthesia in combination with either conscious sedation or general anesthesia is important to the Shouldice Method. However, it is more common to use a local anesthesia with conscious sedation. This is concurrent with the 2018 HerniaSurge guidelines [1], which recommend local anesthesia for treatment of unilateral primary inguinal hernias for all adults. The experts in this project also commented that the use of general anesthesia should be reserved for specific circumstances (such as multiple recurrences) where conscious sedation is less appropriate. Studies have been completed with evidence to support local anesthesia as being more cost effective [48], providing earlier patient mobilization and hospital discharge [49], lower early post-operative pain and post-operative nausea [49, 50], and higher patient satisfaction [51, 52]. At Shouldice Hospital the use of local anesthesia continues to be the preferred approach and its use has been widely documented over the years [5, 7, 8, 38,39,40]
Step three of the Shouldice Method are the incision and nerve identification steps
The experts came to the consensus that an oblique inguinal incision must be made and the incision should allow for appropriate visualization from above the internal ring to the pubis when performing the Shouldice Method. The rationale from experts is that when performing this type of open repair, the incision must be adequate enough to see the anatomy properly (femoral and inguinal regions) and complete the repair satisfactorily [7, 8, 40]. Former Shouldice Hospital surgeons have described the location of the incision to be along the line of the inguinal canal [39], starting midway between the anterior superior iliac spine and internal ring then extending to the public tubercle [7] or paralleling the groin crease [8]. Some of our experts noted that it is also important to tailor the groin incision to the patient’s anatomy (i.e., size of hernia and body stature).
The development of an adequate external oblique aponeurotic flap as well as opening the cribriform fascia to identify the presence of a femoral hernia were included by the experts in the Shouldice Method because they can help relieve tension over the dissection, as well as prevent any recurrences that were missed hernias during the index operation. A study published in 2002, showed results where there was a 15-fold greater incidence of femoral hernia after inguinal hernia repair compared to the occurrence of a primary femoral hernia [53]. Additional steps and reasoning for identifying occult femoral defects have been well documented in other publications [7, 8, 39].
There was consensus among the experts that it is important to identify, isolate, and preserve the ilioinguinal and iliohypogastric nerves, whenever possible when performing the Shouldice Method. Experts have also advised that when there is a risk of entrapment, the deliberate sacrifice of the nerves may need to be done. These practices are in keeping with recent guidelines in the context of inguinal hernia repair [1] and are well documented as being done as part of the Shouldice Repair [7, 8, 39].
Step four of the Shouldice Method relates to the treatment of the cremasteric muscles
The consensus on the handling of the cremasteric muscles for a Shouldice Method were (1) they are split open, (2) the medial cremasteric muscle as well as the posterior cremasteric vessels are resected, and (3) the Genital Branch of the Genito Femoral nerve, in combination with the lateral cremasteric muscles are divided. The splitting of the cremasteric muscle opens up the cord area and allows for clear identification and visualization of hernia anatomy (i.e., sac), this is important specifically in the context of small indirect hernia sacs. This can also improve the floor repair and help identify occult direct hernias. In males, the distal portion is fixed during the external oblique closure and this is done to keep the testicle in place. The treatment of the cremasteric muscle and development of these procedures by Shouldice surgeons have been previously documented [8, 38, 39].
Step five of the Shouldice Method is the hernia identification and treatment step
This group of experts came to the consensus that the important steps to indirect hernia identification and treatment involved identifying and treating cord lipomas, indirect hernia sacs, peritoneal protrusions, and possible interstitial hernias. The first part of this step involves identifying and resecting cord lipomas and the observations made by the experts in this project were that the resection of cord lipomas allowed for a better repair of the internal ring, but one has to be mindful of vascularity and any risk of damage to cord structures. The experts commented that if it is seen as unsafe to resect the cord lipomas, they should be reduced, however, most agreed that almost all should be resected. The following part was the identification, dissection, and reduction of a peritoneal protrusion, which is done medial to the vas deferens at the level of the internal ring to rule out the presence of a small or occult indirect hernia. The next inclusion in the Shouldice Method is the mobilization and handling of the indirect hernia sac. This involves the identification, isolation and dissection beyond the internal ring, to fully mobilize and deal with the indirect hernia sac, which should either be reduced or excised. Either reducing or excising is appropriate based on the clinical situation and discretion of the surgeon. The final part of this step was to identify possible interstitial hernias that surround the internal ring or in other locations where they can be commonly found, which is often superior and medial to the internal ring, separated by a muscular bridge from indirect hernias. These hernias may be uncommon but can contribute to recurrences if they were missed at the time of the initial surgery [8]. Identifying these possible hernias is completed by visually assessing the muscle wall superiorly and laterally to the internal ring [7]. The reason for identifying and freeing these structures are to ensure there is no development of an indirect hernia leading to a recurrence [8].
Step six of the Shouldice Method is the reconstruction of the posterior wall
The first few items of the reconstruction of the posterior wall that are important for a Shouldice Method are the adequate dissection of the tissues overlying the pubis to allow for the superior part of the pubic tubercle to be easily seen and palpated, the opening of the transversalis fascia just lateral to the medial abdominal wall muscles, the development of the posterior rectus plane, and the opening of the transversalis fascia from the pubic tubercle to the internal ring. This allows for the visualization of a direct hernia [7, 40] and for a secondary exam of the femoral space to check for any defects, which as discussed earlier is important in reducing early recurrences.
The consensus on the closure of the hernia defect for the Shouldice Method was that it should be done in four layers and using permanent monofilament material, which has been recommended in the past [7, 8, 40]. The Shouldice Hospital has previously reported the use of stainless-steel wire because of its bacterial resistance and excellent strength [7, 8, 40]. These same publications reported a disadvantage to using this material for surgeons and hospitals more broadly, as it can cause frustration due to kinks and breakage if mishandled and it is difficult to procure [7, 8].
The following parts of this step relating to the four lines of repair have been well documented in previously published articles [5, 7, 8, 40] and are all important to the Shouldice Method. The first line of repair should bring together the transversalis fascia and the medial abdominal wall muscles, as well as include the proximal cremasteric stump (from lateral and posterior cremasteric muscles). This is important as it aids in the recreation of the internal ring as well set the foundation for a strong repair. The second line of the repair brings together the medial flap (transversus abdominus, internal oblique arch, and rectus) down to the shelving edge of the inguinal ligament. The third line of the repair should bring together the more superficial layers of the transversus abdominus, internal oblique arch, and rectus to the shelving edge of the inguinal ligament. In regards to the fourth line of repair, it should bring together the anterior wall medial muscles and a more superficial portion of the shelving edge of the inguinal ligament/external oblique fascia. The experts involved in this project commented that the third and fourth layer help create a tension free second layer, but in recurrent hernias or patients with a significant prior surgery those layers may not always be completed. The final part of this step was that the diameter of the internal ring should be tested and should appropriately surround the cord without compressing its structure.
It is important to note that in a previous step the femoral region is manually checked by the surgeon as to not miss a femoral hernia by opening of the cribriform fascia. Some surgeons at Shouldice Hospital may do one of these checks or both but the consensus is that the femoral space is always checked regardless of the method.
Step seven of the Shouldice Method is the post-operative management of patients at Shouldice Hospital
The first part included in the Shouldice Method was the early ambulation and physical activity of patients post-operatively. Many previous reports have explained the history of early ambulation as well as the benefit and confidence to resuming normal activities as part of the Shouldice Hospital procedure [7, 8]. The second and third important inclusions are adequate post-operative pain management, simply with oral medication as well as opioid sparing practices during the hospital course. By providing oral pain medication during the hospital stay, patients are able to be comfortable enough for early ambulation while restricting or eliminating the use for opioids.
Additional inclusions in the final Shouldice Method were patients as teachers and overall patient interaction. Previous articles on the Shouldice Repair, have explained how patients as teachers and patient interactions can provide them with knowledge, comfort, confidence, as well as reduced anxiety surrounding surgery and recovery [8].
The final part of step seven that was included in the Shouldice Method was the practice of opioid sparing on discharge. Due to the growing association between excessive opioid prescribing and opioid misuse and associated morbidities [54], the traditional routine of prescribing opioids after surgery to treat pain is being replaced with opioid sparing practices and multimodal analgesia management [55,56,57]. The individual and societal benefits to opioid sparing practices have been reported across a variety of surgical procedures [58, 59].
The experts here had commented that ambulation immediately post-operatively has a good psychological benefit on the patient’s confidence that movement will not hurt the repair, but patient safety and level of mobilization immediately after surgery needs to be considered. Massage therapy is also excluded from the final framework and this was most often commented to be because there is not enough data or publications to directly link the benefit of massage therapy to healing.
Limitations
There are limitations within this project. We had two experts that did not participate in the Delphi (only 11 out of 13 completed both iterations) and perhaps their responses may have impacted a few of the included or excluded components, particularly those that were on the cusp of inclusion and increased the reliability of the Delphi methodology [13, 60, 61]. Regardless, these were not the mainstays of the Shouldice Method and thus would not have changed the overall direction of the consensus. The results presented here included experts from a single center, and although this was mitigated by having multiple surgeons with varying levels of expert experience and ages, this may be a constraint and make the results less generalizable. However, the main purpose of this study was to replicate the steps of this technique in a real world setting into the practice of surgeons by leaning on content experts from a center of excellence. Another limitation was that the study recruited surgeons that had been working at Shouldice Hospital since 2016 onwards—perhaps there could be a slight deviation over time of the original technique. Although this too is mitigated as many of the participants had been working here for a prolonged period of time up to and including 2016 and onwards. In this article the Shouldice Method is applied to inguinal hernia repair (indirect and direct), we did not expand the Delphi to include associated or isolated femoral/interstitial hernias, nor indications/surgical limitations of the Shouldice Method during the operation. In cases where a secondary femoral/interstitial hernia is detected, the surgeon will take into consideration the size and contents of the defect as well as patient characteristics before deciding the best way to repair. The majority of primary inguinal hernias are candidates for the Shouldice Method and any limitations to that are decided on an individual patient basis. Some of the aforementioned aspects that were not covered in this article will be explored in future research.
Conclusions
The objective of this project was to provide a clear and concise paper on what content experts consider to be the essential steps of a Shouldice Method as it relates to the repair of inguinal hernias. This article is unique as it provides the methods for pre- and post-operative patient care, focuses on essential steps of an inguinal hernia repair, and provides a consensus from a high-volume center that created the technique. The results of this consensus will allow for a better understanding of the care and techniques that make up the Shouldice Method and allow other surgeons to incorporate this into their practice.
Data availability
Not applicable.
Code availability
Not applicable.
References
The HerniaSurge Group (2018) International guidelines for groin hernia management. Hernia 22(1):1–65
Lau WY (2002) History of treatment of groin hernia. World J Surg 26:748–759
Rogmomi C, Cuccurullo D, Borsoi L, Bonavina L, Asti E, Crovella F, Bassi UA, Carbone G, Guerini F et al (2020) Clinical outcomes and quality of life associated with the use of a biosynthetic mesh for complex ventral hernia repair: analysis of the “Italian Hernia Club” registry. Nature Publishing Groups Research, Berlin
Van Veen RN, Wijsmuller AR, Vrijland WW, Hop WC, Lange JF, Jeekel J (2007) Long-term follow up of a randomized clinical trial of non-mesh versus mesh repair of primary inguinal hernia. Br J Surg Soc LTD 94:506–510. https://doi.org/10.1002/bjs.5627
Welsh DRJ and Alexander MAJ (1993) The shouldice repair. Surg Clin North Am 73(3):451–469
Bendavid R (1992) The merits of the shouldice repair. Probl Gen Surg 12(1):105–109
Shouldice EB (2003) The shouldice repair for groin hernias. Surg Clin N Am 83:1163–1187
Shouldice EB (2010) Surgery illustrated-surgical atlas. the shouldice natural tissue repair for inguinal hernia. BJUI 105:428–439
Lorenz R, Arlt G, Fortelny R, Gorjanc J, Koch A, Morrison J, Oprea V, Campanelli G (2020) Shouldice standard 2020: review of the current literature an results of an international consensus meeting. Hernia 25(5):1199–1207
Malik A, Bell CM, Stukel TA, Urbach DR (2016) Recurrence of inguinal hernias repaired in a large hernia surgical speciality hospital and general hospitals in Ontario. Can J Surg 59(1):19–25
Szasz P, Spencer Netto F, Hospital S (2021) Shouldice Hospital comments on “Shouldice standard 2020: review of current literature and results of an international consensus meeting.” Hernia 25:1375–1376
Hasson F, Keeney S, McKenna H (2000) Research guidelines for the delphi survey technique. J Adv Nurs 32(4):1008–1015
Penciner R, Langhan T, Lee R, Mcewen J, Woods RA, Bandiera G (2011) Using a Delphi process to establish consensus on emergency medicine clerkship competencies. Med Teach 33(6):333–339
Hsu CC, Sandford BA (2007) The delphi technique: making sense of consensus. Pract Assess Res Eval 12(10):1–8
Goodman CM (1987) The delphi technique: a critique. J Adv Nurs 12(6):729–734
Rowe GW, G, (1999) The delphi technique as a forecasting tool: issues and analysis. Int J Forecast 15:353–375
Szasz P, Louridas M, de Montbrun S, Harris KA, Grantcharov TP (2016) Consensus-based training and assessment model for general surgery. BJS 103:763–771
Ursachi G, Horodnic IA, Zait A (2015) How reliable are measurement scales? External factors with indirect influence on reliability estimators. Proc Econ Financ 20:679–686
Hulin C, Netemeyer R, Cudeck R (2001) Can a reliability coefficient be too high? J Consum Psychol 10(1):55–58
Barbera J, Nailbert N, Komperda R, Pentecost TC (2021) Clarity on Cronbach’s alpha use. J Chem Educ 98:257–258
Graham B, Regehr G, Wright JG (2003) Delphi as a method to establish consensus for diagnostic criteria. J Clin Epidemiol 56:1150–1156
Zevin B, Levy JS, Satava RM, Grantcharov TP (2012) A consensus-based framework for design, validation, and implementation of simulation-based training curricula in surgery. J Am Coll Surg 215(4):580–586
Palter VN, MacRae HM, Grantcharov TP (2021) A consensus-based framework for design, validation, and implementation of simulation-based training curricula in surgery. J Am Coll Surg 215(4):580–586
R Core Team (2021). R: a language and environment for statistical computing. R Foundation for Statistical Computing, Vienna https://www.R-project.org/
WHO handbook for guideline development—2nd ed. (ISBN 978924154896 0) © World Health Organization 2014, 9789241548960_chap16_eng.pdf (who.int). Accessed June 10 2022
Lilly MC, Arregui ME (2002) Ultrasound of the inguinal floor for the evaluation of hernias. Surg Endosc 16:659–662
Bradley M, Morgan D, Pentlow B, Roe A (2003) The groin hernia—an ultrasound diagnosis? Ann R Coll Surg Engl 85:178–180
Light D, Ratnasingham K, Banerjee A, Cadwallader R, Uzzaman MM, Gopinath B (2011) The role of ultrasound scan in the diagnosis of occult inguinal hernias. Int J Surg 9:169–172
KaLok Lee R, Griffith JF, Wing Hung Ng A (2015) High Accuracy of ultrasound in diagnosing the presence and type of groin hernia. J Clin Ultrasound 43:538–547
Kwee RM, Kwee TC (2018) Ultrasonography in diagnosing clinically occult groin hernia: systematic review and meta-analysis. Eur Radiol 28:4550–4560
Naidoo P, Levett K, Lord S, Meagher A, Williams N, Aczel T (2020) How often are patients with clinically apparent inguinal hernias referred to a surgeon accompanied with an ultrasound? A prospective multicentre study. Aust Health Rev 45(1):36–41
Hughes MJ, Hackney RJ, Lamb PJ, Wigmore SJ, Christopher Deans DA, Skipworth RJE (2019) Prehabilitation before major abdominal surgery: a systematic review and meta-analysis. World J Surg. https://doi.org/10.1007/s00268-019-04950-y
Giesche F, Niederer D, Banzer W, Vogt L (2020) Evidence for the effects of prehabilitation before ACL reconstruction on return to sport related and self reported knee function a systematic review. PLoS ONE 15(10):e0240192. https://doi.org/10.1371/journal.pone.0240192
Delaney L, Howard R, Palazzolo K, Ehlers AP, Smith S, Englesbe M, Dimick JB, Telem DA (2021) Outcomes of a presurgical optimization program for elective hernia repairs among high-risk patients. JAMA Netw Open 4(11):e2130016. https://doi.org/10.1001/jamanetworkopen.2021.30016
Trepanier M, Minnella EM, Paradis T, Awasthi R, Kaneva P, Schwartzman K, Carli F, Fried GM, Feldman LS, Lee L (2019) Improved disease-free survival after prehabilitation for colorectal cancer surgery. Ann Surg 270(3):493–501
Ravanbakhsh S, Batech M, Tejirian T (2015) Increasing body mass index is inversely related to groin hernias. Am Surg 81(10):1043–1046
Majumder A, Fayezizadeh M, Neupane R, Elliott HL, Novitsky YW (2016) Benefit of multimodal enhanced recovery pathway in patients undergoing open ventral hernia repair. J Am Coll Surg 222:1106–1115
Glassow F (1973) The surgical repair of inguinal and femoral hernias. CMA. Journal 108:308–313
Welsh DRJ (1974) Inguinal hernia repair: a contemporary approach to a common procedure. Mod Med 1:49–54
Bendavid R (1993) The shouldice operation. Ann Ital Chir 1:151–156
Lemos MF, Lemos-Neto SV, Barrucand L, Vercosa N (2019) Preoperative education reduces preoperative anxiety in cancer patients undergoing surgery: usefulness of the self-reported Beck anxiety inventory. Braz J Anesthesiol 69(1):1–6
Peng F, Peng T, Yang Q, Liu M, Chen G, Wang M (2020) Preoperative communication with anesthetists via anesthesia service platform (ASP) helps alleviate patients’ preoperative anxiety. Sci Rep 10(1):18708
Heather MA, Charlotte D, Mckelvie R, Hirsh J, Rush B (2000) Effect of a preoperative intervention on preoperative and postoperative outcomes in low-risk patients awaiting elective coronary artery bypass graft surgery. Ann Intern Med 133:253–262
Healy KM (1968) Does preoperative instruction make a difference? Am J Nurs 68:62–67
Avishai E, Yeghiazaryan K, Golubnitschaja O (2017) Impaired wound healing: facts and hypotheses for multi-professional considerations in predictive, preventive and personalised medicine. EPMA J 8(1):23–33. https://doi.org/10.1007/s13167-017-0081-y
Mills E, Eyawo O, Lockhard I, Kelly S, Wu P, Ebbert JO (2011) Smoking cessation reduces postoperative complications: a systematic review and meta-analysis. Am J Med 124(2):144–154
Khurana VG (2021) Adverse impact of smoking on the spine and spinal surgery. Surg Neurol Int 12:118. https://doi.org/10.25259/SNI_6_2021
Nordin P, Zetterstrom H, Carlsson P et al (2007) Cost-effectiveness analysis of local, regional and general anesthesia for inguinal hernia repair using data from a randomized clinical trail. Br J Surg 94(4):500–505. https://doi.org/10.1002/bjs.5543
Joshi GP, Rawal N, Kehlet H et al (2012) Evidence-based management of postoperative pain in adults undergoing open inguinal hernia surgery. Br J Surg 99(2):168–185. https://doi.org/10.1002/bjs.7660
Nordin P, Zetterstrom H, Gunnarsson U, Nilsson E (2003) Local, regional, or general anaesthesia in groin hernia repair: multicentre randomized trail. Lancet 362:853–858. https://doi.org/10.1016/s0140-6736%2803%2914339-5
Song D, Greilich NB, White PF, Watcha MF, Tongier WK (2000) Recovery profiles and costs of anesthesia for outpatient unilateral inguinal herniorrhaphy. Aanesth Analg 91(4):876–881
Ozgun H (2002) Comparison of local, spinal, and general anesthesia for inguinal herniorrhaphy. Eur J Surg 168:455–459. https://doi.org/10.1097/00132586-198804000-00042
Mikkelsen T, Bay-Nielsen M, Kehlet H (2002) Risk of femoral hernia after inguinal herniorrhaphy. Br J Surg 89(4):486–488
Neumann MS, Bateman BT, Wunsch H (2019) Postoperative pain management and opioids 2. Lancet 393:1547–1557
Schwenk ES, Mariano ER (2018) Designing the ideal perioperative pain management plan starts with multimodal analgesia. Korean J Anesthesiol 71(5):345–352. https://doi.org/10.4097/kja.d.18.00217
Connolly NC (2018) Real-world insights on the use of transversus abdominis plane black with liposomal bupivacaine in the multimodal management of somatic versus visceral pain in the colorectal surgery setting. J Pain Res 11:1141–1146
Charipova K, Gress KL, Urits I, Viswanath O, Kaye AD (2020) Maximization of non-opioid multimodal analgesia in ambulatory surgery centers. Cureus 12(9):E10407. https://doi.org/10.7759/CUREUS.10407
Gabriel RA, Swisher MW, Sztain JF, Furnish TJ, Ilfeld BM, Said ET (2019) State of the art opioid-sparing strategies for post-operative pain in adults’ surgical patients. Expert Opin Pharmacother 20(8):949–961
Morin C, Patel Y, Javid M, Tevis SE, Fortes T, Flom P, Andaz C, Manasseh DM, Borgen P, Rojas KE (2021) Opioid-Sparing multimodal analgesia protocol for lumpectomy patients results in superior postoperative pain control. Ann Surg Oncol 28:5855–5864
de Villiers MR, de Villiers PJ, Kent AP (2005) The Delphi technique in health sciences education research. Med Teach 27(7):639–643
Fink A, Kosecoff J, Chassin M, Brook RH (1984) Consensus methods: characteristics and guidelines for use. Am J Public Health 74(9):979–983
Acknowledgements
We would like to thank the surgeons from Shouldice Hospital that participated in this project as well as the hospital staff in IT that provided support during the project. The authors would also like to acknowledge the contributions of Dr. E.B. Shouldice, who had passed away before the publication of this paper.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by MM, FACSN, and PS. The first draft of the manuscript was written by MM and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Mainprize M, Spencer Netto FAC, Degani C, and Szasz P declare that they have no conflict of interests.
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Mainprize, M., Spencer Netto, F.A.C., Degani, C. et al. The Shouldice Method: an expert’s consensus. Hernia 27, 147–156 (2023). https://doi.org/10.1007/s10029-022-02658-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-022-02658-y