Abstract
Purpose
Laparoscopic contralateral patent processus vaginalis (CPPV) repair in children is debatable due to the high CPPV rate, but low metachronous contralateral inguinal hernia (MCIH) rate. We conducted this study to find risk factors for MCIH.
Method
We conducted a prospective, observational trial with patients recruited from Shanghai Children’s Hospital. Eligible participants were patients under 16 years old with unilateral inguinal hernia whose parents did not opt for simultaneous CPPV repair. The subjects were followed for 24 to 34.1 months. Patients who developed MCIH were analyzed to identify the relationship between CPPV and MCIH.
Results
Between October 17, 2018, and July 31, 2019, we included 184 patients and 182 completed follow-up. MCIH occurred in ten patients, of which 7 (7.53%) had CPPV and three (3.37%) had no CPPV. Univariate analysis showed that age (p = 0.025, OR = 0.938) and CPPV diameter (p = 0.003, OR = 1.783) were related to the development of MCIH. In multivariate analysis, only diameter of CPPV (p = 0.008, OR = 1.411) was associated with MCIH. The receiver operating characteristic (ROC) curve was used to test, and it was found that when the diameter of CPPV was greater than 4 mm, the Youden index was the highest, with a specificity of 62.8% and a sensitivity of 100%.
Conclusion
The incidence of MCIH was not statistically higher in patients with CPPV compared with those without CPPV, so there is no indication for routine CPPV repair. The risk of MCIH development increases with CPPV diameter. 4 mm is the optimal cutoff point. Large CPPVs (> 4 mm) could be treated to prevent future hernias.
Trial registration
The Chinese Clinical Trial Registry (www.chictr.org.cn), number ChiCTR2000041307.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Inguinal hernia (IH) is one of the most common diseases in pediatric surgery with an overall rate of 0.8–4.4% [1], and 75–90% of these patients have unilateral inguinal hernia (UIH) [2, 3]. Children with UIH have a chance of subsequently developing metachronous contralateral inguinal hernia (MCIH). Whether to explore the contralateral side in children with UIH has been debated for decades. Surgeons commonly practice contralateral exploration in children due to the high reported incidence of a contralateral patent processus vaginalis (CPPV) and an increased risk of general anesthesia in the very young. Then surgeons noted that only few CPPV might develop into a clinical hernia, and routine exploration would put both testicles and both vas deferens at risk. Because of this fact, many surgeons have abandoned routine contralateral exploration.
With introduction of laparoscopic hernia repair in children, CPPV exploration and ligation have become easier without the need for additional incisions. A large amount of literature report that CPPV ligation can prevent MCIH [4,5,6,7] and consider this to be a major benefit of laparoscopic hernia repair. However, the laparoscopic CPPV rates (28%–66%) [8,9,10,11] are much higher than MCIH rates (2.4% to 13.9%) [4, 6, 12, 13]. Therefore, one would need to perform 4–21 operations to prevent one future hernia. Whether or not to repair CPPV simultaneously in children with UIH is still controversial. We do not consider yes or no as the best answer. It is essential to identify the exact relationship between CPPV and MCIH to select the best strategy to balance the risks and benefits. Therefore, we performed a prospective observational study in pediatric patients with UIH to detect the relationship between CPPV and MCIH.
Methods
Study design and participants
We conducted a prospective observational trial with patients recruited from Shanghai Children’s Hospital. This trial was approved by the Research Ethics Review Committee of Shanghai Children’s Hospital, Shanghai Jiao Tong University (2018RY028-E01).
Patients were eligible for inclusion if they were younger than 16 years and had a primary unilateral inguinal hernia. Exclusion criteria were bilateral inguinal hernia, recurrent inguinal hernia, incarcerated inguinal hernia, ultrasound identified CPPV, or one or more of the following diseases in their medical history: inguinal region surgery, long-term constipation, chronic cough, ascites, abdominal wall deformity, and urinary tract malformation. Patients were recruited from the general surgery clinics. Patients who visited the outpatient clinic with a unilateral inguinal hernia received an information package about our trial. All patients whose guardians consented to participate were included in this trial, and all guardians provided written informed consent.
Procedures
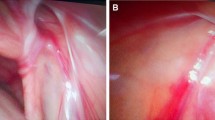
Patients included in this trial received laparoscopically extraperitoneal high ligation of the hernia sac and detection of the contralateral side. Three consultant surgeons from the general surgery department of Shanghai Children’s Hospital took part in this trial. All surgeons had previous experience of at least 5 years of laparoscopic hernia repair. At the start of the study, all three surgeons were invited to specific trial training sessions to ensure that all participating surgeons would use the same standardized techniques to measure an internal orifice and to close an inguinal hernia. All operations were performed on patients under general anesthesia. An extraperitoneal high ligation of the hernia sac by a non-absorbable, silk braided suture of thickness 2/0 (Mersilk suture) was performed with two 3-mm trocars placed paraumbilical, one was for the camera, and the other was for the assistant instrument. The pneumoperitoneum pressures were between 8 and 10 mmHg according to the ages of the children. An aseptic paper ruler was placed into the abdominal cavity through the operative trocar to measure the longest diameter of the internal orifice (Figure 1), accurate to millimeters. The type of internal orifice was classified as opening, membraniform, and semi-membraniform (Figure 2). There was no special postoperative treatment. All patients got into the follow-up schedule.
Different types of internal orifices. a Opening type of internal orifice, which was not covered by peritoneum; b semi-membraniform type of internal orifice, part of which was covered by peritoneum; c1 membraniform type of internal orifice, which was covered by peritoneum; c2 when lifting the membrane covering the membraniform-type internal orifice, a CPPV was evident
Outcomes
The end point was defined as the incidence of MCIH at 24 months postoperatively. Since MCIH is a life-long event, we reported the complete follow-up results (24–34.1 months). We contacted these patients through a telephone follow-up schedule since not all patients could come back to our hospital for follow-up and reoperation (if necessary). We called back all the patients’ parents at 3, 6, 12, and 24 months postoperatively and asked them the following questions:
-
1.
Is there a hernia recurrence on the same side? If yes, when did it happen? Have the patient received another surgery?
-
2.
Does a contralateral hernia develop after surgery? If yes, when did it happen? Have the patients received another surgery?
In case of any doubt, the patients would be asked to go back to our hospital for examination, and supplementary inguinal ultrasound, if necessary.
Statistical analysis
All data that may be related to MICH were collected, such as age, sex, BMI, side of hernia, type and diameter of internal orifice on the hernia side, type and diameter of internal orifice on the CPPV side.
Continuous data were analyzed using two-sample t test (if with equal variances and normally distributed) or Mann–Whitney U test (if non-normally distributed). Chi-square test was used to determine the significance of differences in the incidence of CPPV regarding sex and side. Fisher’s exact test was used to determine the significance of differences in the MCIH incidence regarding CPPV. Time to MCIH development was estimated by means of the Kaplan–Meier estimator. The formal test for difference between the patients with CPPV and patients without CPPV was done with the log-rank test. Univariate and multivariate logistic regression analyses were used to identify the risk factors for MICH. All tests were two-sided and p < 0⋅050 was considered statistically significant. The optimal cutoff point to repair CPPV was estimated and evaluated the sensitivity and specificity by receiver operating characteristic (ROC) curves. The study was registered at Chinese Clinical Trail Registry (www.chictr.org.cn), number ChiCTR2000041307.
Results
Between October 17, 2018, and July 31, 2019, the study group identified 546 potentially eligible cases of unilateral hernia, and 184 patients gave their consent and received laparoscopic unilateral hernia repair and CPPV detection (Figure 3). The main reason patients refused to participate in the trial was fear of developing MCIH. 94 patients with CPPV and 90 without CPPV were identified. During follow-up, two patients were lost after 1 week postoperative interview, one with CPPV, the other without CPPV. They were excluded from the analysis of the incidence of MCIH and recurrence of hernia.
Most participants were male (Table 1) and the median age was 31 months (range 2–134 months, IQR 15–60). Most patients were healthy, except two boys who were underweight (BMI were 12.0 and 12.2, respectively), and one boy and one girl who were obese (BMI were 29 and 28.3 respectively). There were 111 initial right hernias and 73 left hernias. CPPV was found in 94 children (60 with right hernias and 33 with left hernias, 80 males and 14 females) during the operation. The CPPV rate was 51.09%. The diameter of the internal orifice on the hernia side (11.46 ± 3.75 mm, range 5–23) was almost three times that of the CPPV side (3.98 ± 2.10 mm, range 1–10) (p < 0.001). The minimum diameter of the internal orifice on the hernia side was 5 mm. The median follow-up time was 27.9 months (range 24•0–34•1, IQR 26.5–31.3). Three patients had recurrence hernia (1.65%), while ten patients had MCIH (5.49%). Patients developed MCIH after a median of 8.5 months (IQR 4.0–12•8) after their surgery. Patients with CPPV developed MCIH earlier than patients without CPPV. MCIH occurred in patients with CPPV after an average of 8.7 months (IQR 4.0–12.0) and in the patients without CPPV after an average of 12.3 months (IQR 4.0–27.0). The onset of MCIH development in patients with CPPV started 1.0 month after surgery versus 4.0 months in patients without CPPV. Eight of ten patients developed MCIH within 12 months after operations, but one in 15 months and one in 27 months. Of the 10 patients who developed MCIH, 6 had received a second surgery, 3 with groin bulge only once and 1 new onset didn't have a second surgery. Two of ten patients had incarcerated hernias. There was no postoperative complication.
We divided the patients into two groups: CPPV group and non-CPPV group. There were no significant differences in sex, age, height, weight, BMI for age and laterality between the two groups (Table 2), which means that the demographic characters and the side of the initial hernia cannot predict CPPV. The opening type internal orifice dominated on the hernia side in both groups [85 (94.44%) versus 91 (96.81%)]. There was no difference in the diameter of the hernia side internal orifice between patients with and without CPPV (p = 0.49). Three patients (3.37%) without CPPV and seven (7.53%) with CPPV developed MCIH.
Univariate analysis (Table 3) showed that age (p = 0.025, OR = 0.938) and the diameter of CPPV (p = 0.003, OR = 1.783) were related to the development of MCIH. Sex (p = 0.998), side (p = 0.174), BMI (p = 0.41), the type and diameter of the internal orifice on the hernia side (p = 0.999, p = 0.497), and the type of CPPV (p = 0.591) were not related to MCIH. Then variables with statistically significant differences in univariate analysis were included in multivariate analysis, and the results showed that only the diameter of CPPV (p = 0.008, OR = 1.411) was related to the development of MCIH. That is, the risk of developing MCIH increases with CPPV diameter. The receiver operating characteristic curve (ROC curve) was used to detect the efficacy of CPPV diameter in predicting MCIH, and the results showed that the area under the curve (AUC) was 87.3% (95%CI: 0.788–0.933) (Figure 4). When the diameter of the CPPV is greater than 4 mm, the Youden index is the largest, which is 0.6279, the specificity is 62.8%, and the sensitivity is 100%.
The diameter of CPPV could predict MCIH development in children with CPPV. When the diameter of the CPPV was greater than 4 mm, the Youden index was largest (0.6279). The sensitivity was 100%, and the specificity was 62.8%. CPPV patent processus vaginalis, MCIH metachronous contralateral inguinal hernia
Discussion
This is the first prospective study to explore the relationship between the diameter of the internal orifice of CPPV and MCIH. The study has shown that the diameter of CPPV is closely related to the development of MCIH. CPPVs larger than 4 mm should be treated to prevent future hernia, especially in patients younger than 3 years.
In this study, the incidence of MCIH after 24–34.1 months was 5.49% (10/182), which was similar to the findings of several meta-analyses (5.6–6%) [13,14,15]. A lot of publications limited to retrospective studies supported CPPV as a risk factor for MCIH [4, 5]. All the results were gained from a comparison of traditional open herniotomy and laparoscopic hernia repair: patients with unilateral hernia who received open procedures had a higher incidence of MCIH compared with patients who received laparoscopic repairs of hernia and CPPV [6, 12]. Maddox and Smith reported a prospective study and claimed that laparoscopic findings (CPPV) failed to predict which CPPV would subsequently would develop into a MCIH [16]. They did laparoscopic detection through the hernia sac, which could not get accurate results because of the view angle and lack of assistant instruments. These results vary widely, and the treatment of CPPV is also controversial. Some surgeons insist that CPPV closure reduces the rate of subsequent MCIH and risks of strangulation and incarceration, while others consider this strategy results in overtreatment and increases potential operative risks, including injury of the vas deferens, spermatic vessel, changes in the angle of vas deferens and testicular atrophy. In this study, the incidence of MCIH in patients with CPPV was not statistically higher than that in patients without CPPV (7.53% vs 3.37%, p = 0.33), so routine CPPV repair is not indicated.
The significant difference between this study and previous studies was that the diameter of CPPV was taken into analysis, and we found that large CPPV (> 4 mm) may be a risk factor for MCIH. Patients with CPPV larger than 4 mm had a high tendency (7/39, 17.95%) to develop MCIH. CPPV diameter greater than 4 mm was reasonably accurate in predicting MCIH (A = 0.873), with a specificity of 62.8% and a sensitivity of 100%. Large CPPV (> 4 mm) should be treated at the same time when performing laparoscopic hernia repair to prevent future MCIH and potential incarceration. No patients with CPPV smaller than 4 mm developed MCIH postoperatively in this study. Small CPPV (≤ 4 mm) should not be treated, because the patient cannot benefit from the operation and may bear additional surgical risks and pay more. Using 4 mm as the surgical standard for CPPV could reduce unnecessary CPPV ligation by 60%. Until now, there has been only one study that mentioned the relationship between the diameter of CPPV and MICH. Christine Burgmeier and colleagues considered that the contralateral internal rings smaller than 2 mm were unlikely to cause a hernia and thus were left open [17], but they did not provide any evidence.
All patients who developed MICH in this study were younger than 3 years old, ranging from 6 to 29 months. There was a significant difference in age between patients with and without MICH. It seems that young children are more likely to develop MICH, which was similar to findings from studies by Yanan Li and colleagues [18]. The reason is uncertain. The incidence of CPPV was similar in patients younger than 3 years and older than 3 years in this study (53.3% vs 48.1%), so CPPV was not the reason. We think the reason may be related to the strength of the abdominal muscles. Older children have stronger abdominal muscles, which may be similar to adults. Autopsy data suggested that 15–30% of adults with a CPPV do not have a hernia [19].
Although without significant difference, patients with initial left-sided hernias had a higher incidence of MICH, which was more than twice that of patients with right-sided hernias. This result was similar to most of the reports [13, 15, 18, 20,21,22]. Interestingly, right-sided hernias had a slightly higher incidence of CPPV than left-sided hernia (63.83% vs 36.17%) in this study, which was opposite to the incidence of MCIH. This result suggests that CPPV is not the only factor in the development of MCIH, which is also supported by the possibility of MICH in patients without CPPV. Patients with opening type internal orifices were more likely to develop MCIH than patients with other types (17.65% vs 5.41% vs 0), but there was no significant difference. Logically, it is because there is no obstruction in the opening type and it is easier for the contents of the abdominal cavity to enter the inguinal canal. We need more cases to identify this hypothesis.
In this study, three patients without CPPV developed MCIH. MCIH following negative laparoscopic evaluation for CPPV has been described before in the literature [23,24,25]. We could not explain it at present. We think that some inguinal hernias may be a developmental disease. In our study, patients without CPPV developed MCIH later than patients with CPPV. In one patient who developed MCIH with an initial size of 5 mm CPPV was found to enlarge to 9 mm during the second surgery. The membraniform and semi-membraniform may be two stages in one process. The incidence of MCIH following negative CPPV was 3.37% and similar to findings from the study by Yuk Him Tam and colleagues (3.1%) [23]. They considered the development of MCIH in patients without CPPV as a result of the false-negative laparoscopic evaluation. In our study, negative CPPV was a true negative, because we defined it strictly and used grasp forceps to help identify even tiny CPPV. Yuk Him Tam and colleagues defined CPPV by an open tunnel without identifiable termination to the peritoneal sac in the inguinal canal, while we defined CPPV by no contiguous peritoneum around the spermatic cord structures at the level of internal orifice. A slight peritoneum protrusion toward the inguinal canal was considered as a CPPV in this study.
A limitation of our study was insufficient cases for risk factors related to age, laterality, and CPPV type. This study was not powered to determine whether age, laterality, and CPPV type are risk factors for MCIH development. Although the sample size is a bit small, we can get important hints from this study. This method of studying the risk factors of MCIH in children is feasible. Another limitation of our study is that no information was recorded on eligible patients who did not participate in the study, which could lead to potential selection bias.
In conclusion, this study shows that the incidence of MCIH was not statistically higher in patients with CPPV compared with those without CPPV, and therefore routine CPPV repair is not recommended. However, a close relationship between the diameter of CPPV and the development of MCIH was revealed for the first time. The risk of developing MCIH increases with the diameter of the CPPV, 4 mm is the optimal cutoff point. Young age (< 3 years), opening type CPPV and left-sided hernias may be risk factors of MCIH. Due to the low incidence of MCIH, CPPV treatment should be selectively performed. Therefore, we advocate that small CPPV (≤ 4 mm) should not be repaired, while larger than 4 mm CPPV could be treated to prevent future hernia, especially in patients younger than 3 years old.
References
Miltenburg DM, Nuchtern JG, Jaksic T, Kozinetiz C, Brandt ML (1998) Laparoscopic evaluation of the pediatric inguinal hernia–a meta-analysis. J Pediatr Surg 33:874–879
Rowe MI, Copelson LW, Clatworthy HW (1969) The patent processus vaginalis and the inguinal hernia. J Pediatr Surg 4:102–107
Ein SH, Njere I, Ein A (2006) Six thousand three hundred sixty-one pediatric inguinal hernias: a 35-year review. J Pediatr Surg 41:980–986
Liu J, Wu X, Xiu W, Hao X, Zhao J, Wei B, Dong Q (2020) A comparative study examining laparoscopic and open inguinal hernia repair in children: a retrospective study from a single center in China. BMC Surg 20:244
Nakashima M, Ide K, Kawakami K (2019) Laparoscopic versus open repair for inguinal hernia in children: a retrospective cohort study. Surg Today 49:1044–1050
Zhao J, Chen Y, Lin J, Jin Y, Yang H, Wang F, Zhong H, Zhu J (2017) Potential value of routine contralateral patent processus vaginalis repair in children with unilateral inguinal hernia. Br J Surg 104:148–151
Muensterer OJ, Gianicolo E (2019) Contralateral processus closure to prevent metachronous inguinal hernia: a systematic review. Int J Surg 68:11–19
Saha N, Biswas I, Rahman MA, Islam MK (2013) Surgical outcome of laparoscopic and open surgery of pediatric inguinal hernia. Mymensingh Med J 22:232–236
Endo M, Watanabe T, Nakano M, Yoshida F, Ukiyama E (2009) Laparoscopic completely extraperitoneal repair of inguinal hernia in children: a single-institute experience with 1257 repairs compared with cut-down herniorrhaphy. Surg Endosc 23:1706–1712
Esposito C, Montinaro L, Alicchio F, Scermino S, Basile A, Armenise T, Settimi A (2009) Technical standardization of laparoscopic herniorraphy in pediatric patients. World J Surg 33:1846–1850
Chan KL, Tam PK (2004) Technical refinements in laparoscopic repair of childhood inguinal hernias. Surg Endosc 18:957–960
Zhu LL, Xu WJ, Liu JB, Huang X, Lv ZB (2017) Comparison of laparoscopic hernia repair and open herniotomy in children: a retrospective cohort study. Hernia 21:417–423
Wenk K, Sick B, Sasse T, Moehrlen U, Meuli M, Vuille-dit-Bille RN (2015) Incidence of metachronous contralateral inguinal hernias in children following unilateral repair—a meta-analysis of prospective studies. J Pediatr Surg 50:2147–2154
Kantor N, Travis N, Wayne C, Nasr A (2019) Laparoscopic versus open inguinal hernia repair in children: which is the true gold-standard? A systematic review and meta-analysis. Pediatr Surg Int 35:1013–1026
Nataraja RM, Mahomed AA (2011) Systematic review for paediatric metachronous contralateral inguinal hernia: a decreasing concern. Pediatr Surg Int 27:953–961
Maddox MM, Smith DP (2008) A long-term prospective analysis of pediatric unilateral inguinal hernias: should laparoscopy or anything else influence the management of the contralateral side? J Pediatr Urol 4:141–145
Burgmeier C, Dreyhaupt J, Schier F (2014) Comparison of inguinal hernia and asymptomatic patent processus vaginalis in term and preterm infants. J Pediatr Surg 49:1416–1418
Li Y, Wu Y, Wang C, Wang Q, Zhao Y, Ji Y, Xiang B (2019) Incidence of pediatric metachronous contralateral inguinal hernia and the relationship with contralateral patent processus vaginalis. Surg Endosc 33:1087–1090
Rathauser F (1985) Historical overview of the bilateral approach to pediatric inguinal hernias. Am J Surg 150:527–532
Nassiri SJ (2002) Contralateral exploration is not mandatory in unilateral inguinal hernia in children: a prospective 6-year study. Pediatr Surg Int 18:470–471
Ron O, Eaton S, Pierro A (2007) Systematic review of the risk of developing a metachronous contralateral inguinal hernia in children. Br J Surg 94:804–811
Zamakhshardy M, Ein A, Ein SH, Wales PW (2009) Predictors of metachronous inguinal hernias in children. Pediatr Surg Int 25:69–71
Tam YH, Wong YS, Pang KK, Tsui SY, Mou JW, Houben CH, Chan KW, Lee KH (2013) Unexpected metachronous hernia development in children following laparoscopic unilateral hernia repair with negative evaluation for contralateral patent processus vaginalis. J Laparoendosc Adv Surg Tech A 23:287–290
Watanabe T, Yoshida F, Ohno M, Mori M, Tomita H, Ukiyama E, Nakano M, Endo M (2016) Morphology-based investigation of metachronous inguinal hernia after negative laparoscopic evaluation—is it acquired indirect inguinal hernia? J Pediatr Surg 51:1548–1551
Zhong H, Wang F (2014) Contralateral metachronous hernia following negative laparoscopic evaluation for contralateral patent processus vaginalis: a meta-analysis. J Laparoendosc Adv Surg Tech A 24:111–116
Funding
This study was funded by Shanghai Municipal Commission of Health and Family Planning (grant number 20184Y0260).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Linlin Zhu, Zhibao Lv, Xingzhao Chen, Weijue Xu, Jiangbin Liu, Xiong Huang and Jing Xiong. The first draft of the manuscript was written by Linlin Zhu and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Linlin Zhu, Zhibao Lv, Xingzhao Chen, Weijue Xu, Jiangbin Liu, Xiong Huang and Jing Xiong declare that they have no conflict of interest.
Ethical approval
This trial was approved by the Research Ethics Review Committee of Shanghai Children’s Hospital, Shanghai Jiao Tong University (2018RY028-E01).
Human and animal rights
All procedures were approved by the Research Ethics Review Committee of Shanghai Children’s Hospital, Shanghai Jiao Tong University. This article does not contain any studies with animals performed by any of the authors.
Informed consent
All guardians who agreed to participate in this study provided written informed consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Zhu, L., Chen, X., Xu, W. et al. The relationship between contralateral patent processus vaginalis and metachronous contralateral inguinal hernia in children with unilateral inguinal hernia: a prospective observational study. Hernia 26, 1161–1168 (2022). https://doi.org/10.1007/s10029-022-02638-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-022-02638-2