Abstract
Purpose
Aim of this study was to analyse feasibility, safety and effectiveness of laparoscopic transperitoneal hernia repair (TAPP) approach to inguinal hernias in the emergency setting, with a longer follow-up than the studies present in literature.
Methods
We retrospectively analysed all patients who underwent emergency TAPP hernia repair in San Marco Hospital (Zingonia, Italy), from September 2010 to June 2020. A prospectively collected database of 685 consecutive TAPP hernia repair was reviewed. Feasibility and safety were evaluated through operative time, conversion rate, perioperative mortality, morbidity and prosthesis infection rate. Effectiveness was assessed by recurrence and complication rate, acute (during admission) and chronic (during follow-up) pain by Visual Analogic Scale (VAS), and recovery to normal activity in a long-term follow-up (mean period 1718 days).
Results
The final study group included 47 patients. The mean age was 59.6 years (range 22–89), 29 patients were male and 18 were female. The mean operation time was 64 min. Two cases were converted to open approach (4%). In four cases bowel resection became necessary (8.5%). Appendicectomy and omentectomy occurred once and twice, respectively (2% and 4%), and orchiectomy was required in two patients (4%). Seroma was the only postoperative complication that we registered in four patients. During a mean follow-up period of 1718 days, there was no recurrence of the hernia or other complications. Five patients referred mild occasional groin pain (VAS < 3), with quick relief without taking any pain killers.
Conclusion
TAPP approach is a safe, feasible and effective therapeutic option for groin hernias in emergency setting. No recurrence or severe complications were reported in over 4 years of follow-up.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Laparoscopic transabdominal preperitoneal procedure for inguinal hernia repair has been proven to be an effective technique in elective surgery, as an alternative to the standard open approach [1,2,3]. Nevertheless, there is low-quality, limited evidence about the choice of the upfront therapeutic approach to emergency groin hernias [3]. The current state of research agrees that diagnostic laparoscopy should be performed first in case of incarcerated groin hernia [4,5,6]. In fact, transabdominal preperitoneal repair (TAPP) has proved to be safe and effective in the emergency setting but with a maximum follow-up period of three years [7,8,9,10,11,12,13,14]. Aim of this study was to assess the effectiveness of TAPP repair for the treatment of incarcerated and strangulated inguinal hernias, with a follow-up longer than the one described to date.
Methods
We retrospectively analysed our prospectively collected database of patients undergoing TAPP repair in the Department of General Surgery (Policlinico San Marco, Zingonia-Osio Sotto (BG) Italy) from September 2010 to June 2020. All patients who underwent urgent TAPP repair for incarcerated and strangulated inguinal hernias were included in the final study group.
Collected data included age, sex, body mass index (BMI), comorbidities, professional activity, type of hernia and modality and timing of surgical interventions. TAPP technique was adopted in every incarcerated and strangulated groin hernia, except for patients with anaesthesiologic contraindications or very big scrotal hernias. Informed consent was obtained from all patients. The rate of recurrence, complications, chronic pain, and recovery to normal activity was carried out by surgical examination or with telephone surveys during a long-term follow-up.
Surgical technique
All surgeries were carried out under general anaesthesia after intravenous antibiotic prophylaxis with cefazolin 2 g. Patients were kept in the Trendelemburg position. A Veress needle was used to induce pneumoperitoneum up to 12 mm Hg pressure. Peri-umbelical access for the 30° videocamera was placed through a 10 mm trocar and other two operative trocars were placed: a 12 mm trocar on one side and a 5 mm trocar on the other side of the abdomen, depending on the side of the hernia. After examination of the abdominal cavity, the first step of TAPP procedure is the reduction of the hernia sac and its contents; if this step is difficult, an enlargement of the hernia ring is necessary. In indirect groin hernias, the hernia ring is cut in a ventro-lateral direction, whilst in direct or femoral hernias, it is cut in a ventro-medial direction. This is done to avoid lesions of the spermatic cord or epigastric and femoral vessels. The hernia defect is then repaired with TAPP technique: the parietal peritoneum is incised, the hernia sac is reduced, the preperitoneal space and Cooper ligament are exposed, funiculus’ elements or round ligament are parietalised. A polypropylene lightweight (LWM) mesh of 15–10 cm is placed in the preperitoneal space, and is then fixed to the Cooper’s ligament and to the anterior abdominal wall with either fibrin glue if the hernia defect is smaller than 2.5–3 cm or with tacks (Protacks, Endo Hernia, EMS-Endoscopic Multifeed Stapler) or both if the hernia defect is over than 2.5–3 cm, especially in direct hernias. Finally, the peritoneum is closed with a running suture. A resection may be necessary depending on the vitality of the strangulated organs.
Results
From September 2010 to June 2020, 47 acutely incarcerated and strangulated inguinal hernias underwent TAPP repair in our Department of General Surgery. In the same period, 685 patients with inguinal hernias underwent elective surgery with TAPP technique.
The mean age of included patients was 59.6 years (22–89 years), 29 (62%) patients were men, and 18 (38%) women. The mean BMI was 24.9 kg/m2 (mean height 1.70 m and mean weight 72 kg). Among our patients, ten were smokers (21%) and eight had chronic constipation (17%). Professional activities of the patients were analysed: 23 patients were retired (49%), 14 had sedentary (30%), 5 medium-heavy (10.5%) and 5 heavy activities (10.5%) (see Table 1).
Inguinal hernioplasty was performed on the right side in 25 patients (53%), on the left in 14 (30%) and bilateral in 8 (17%). In all cases of bilateral hernioplasty, hernia was incarcerated only on one side, but both were treated at the same time to avoid subsequent hospitalisation and surgery. Including bilateral hernias, a total of 55 hernias were treated: 49 (89%) were primitive, while 6 (11%) recurrent; 12 (22%) were direct, 22 (40%) indirect, 7 (13%) both direct and indirect, 2 (3.5%) obturator, 9 (16%) femoral, 2 (3.5%) both femoral and direct, 1 (2%) femoral and indirect (see Table 2).
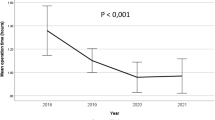
The mean surgery time was 64 min (25–120 min); and was performed under general anaesthesia in all cases. Two cases (4%) were converted to open surgery for the difficulties in performing the bowel resection. In four cases (8.5%) resection was needed for the occurrence of an ischaemic bowel tract: two with laparoscopic surgery, while the other two were converted into open surgery through a median suprapubic mini-laparotomy. During interventions, appendicectomy was performed in one patient (2%), and omentectomy in two cases (4%), as they were found ischaemic after being strangulated in the hernial orifice. In two cases (4%) an orchiectomy was required for an undescended and ischaemic testicle. In all cases a polypropylene lightweight mesh (LWM) was positioned and fixed. The hernia defect was smaller than 2.5–3 cm in 20 patients (42.5%) and the mesh was fixed with fibrin glue; instead, in 27 patients (57.5%) the hernia defect was larger, and the mesh was fixed with tacks or tacks and glue: in two cases (4%) with EMS (Endoscopic Multifeed Stapler), in 4 (8.5%) with Endo Hernia stapler, in 14 (30%) with Pro-Tacks, and in seven cases (15%) with both Pro-Tacks and fibrin glue. The rate of postoperative morbidity was 8.5% for four cases of seroma that occurred and resolved within the first post-operative month. In one case, surgical removal of seroma was necessary due to its size. No post-operative mortality was observed. The mean time of the hospitalisation was 3.2 days. No cases of mesh or wound infections were reported after surgery (see Table 3).
During a mean follow-up period of 1718 days (4.7 years) (264–3875 days), no cases of recurrence or long-term complications were observed. All patients recovered to normal activities in few weeks. Up to now, five patients referred occasional groin pain associated with abdominal strain but without groin swelling, the pain referred was very low (VAS < 3 in all cases) and with quick relief, without taking any pain killer tablet. In these cases, recurrence was excluded after surgical assessment. Eight patients (17%) were lost at follow-up because of death that occurred at least 8 months after surgery; we observed that death occurred in elderly patients (median age 82 years) complicated by several comorbidities: two patients died of cancer, three of pneumonia, one of respiratory failure after COVID-related interstitial pneumonia, one of heart attack and one of post-traumatic cardiac arrest. Just one case of contralateral elective groin hernia repair after the emergency surgery was reported. One woman had two pregnancies without any complication (see Table 4).
Discussion
Laparoscopic approach for inguinal hernia has several advantages over open techniques, allowing a reduction of acute and chronic postoperative pain, a shorter convalescence, and a faster return to normal activities, moreover, there is evidence in its indication in bilateral and recurrent hernias [15,16,17].
Reduced use of the TAPP procedure for treating emergency inguinal hernias has already been reported during the 18th Congress of the European Association of Endoscopic Surgeons (Ginevra, Switzerland, 2010), where one hundred surgeons responded to 19 questions of a survey. In this survey 66% of surgeons preferred an open approach for incarcerated hernias and 74% for strangulated hernias. However, those who answered the laparoscopic approach, preferred TAPP to TEP [18].
The first laparoscopic treatment of an incarcerated inguinal hernia was reported in 1993 [19]. The European Association for Endoscopic Surgery in 2013 established that incarcerated inguinal hernias can be treated laparoscopically [20]. The required expertise in laparoscopic dissection and hernia reduction could be a reason for lower rates of TAPP practice [7, 8], as well as the long learning curve required to perform it safely and rapidly [12]. Nevertheless, laparoscopic approach offers some advantages. First, during laparoscopy it is easier to establish and monitor visceral vitality, especially colour change, peristalsis and bowel viability [9, 13, 21]. Moreover, the increased surgical time in case of laparoscopy can provide a sufficient recovery period for the incarcerated organs, so that it is possible to avoid unnecessary resection, differently from open procedures, where there is less time to take a decision about bowel resection [11, 13, 22]. In the present study, only four patients (8.5%) required resection, consistently with other studies present in literature [9, 23]. Finally, laparoscopic approach offers a satisfactory exploration of the abdominal cavity, making the assessment of any other associated defects, such as unacknowledged contralateral hernias, easier [12, 13].
The feasibility of this approach is difficult to estimate because no unbiased, validated systems have been introduced yet, but it is reasonable to consider the conversion rate and operative time. Conversion to open surgery is crucial as soon as resection reveals to be problematic or significant bowel distension occurs. In this study, we reported four cases of bowel resection: two of which were performed laparoscopically and two requiring conversion into open surgery, through a median suprapubic mini-laparotomy. Conversion into open surgery is recommended when the bowel is fully distended, to avoid mesh infection, because in this case performing intra-abdominal mechanical anastomosis exposes to high risk of intraperitoneal spreading of its content. Our conversion rate (4%) is low, consistent with previous literature, and so is the operative time described in the present study [7,8,9,10,11,12,13,14].
The safety of the technique is revealed by the extremely low rate of complications. Moreover, no severe complications were reported. In fact, only four cases of seroma were reported in our series, whilst literature describes rare occurrences of wound infection, scrotal hematoma, urinary retention, and cord induration [7,8,9,10,11,12,13,14]. All our urgency surgeries analysed were performed by surgeons with large experience in TAPP technique. While in the past the use of mesh in emergent setting was discouraged for the fear of severe infections, an increasing body of evidence has denied this hypothesis [7,8,9,10,11,12,13,14]. Compared to open hernia repair, laparoscopic approach carries the risk of blind insertion of the Veress needle into a viscus or a vessel. However, this chance has already been proved to be reduced by the introduction of open Hasson port and subsequent pneumoperitoneum insufflation [7]. In our surgical unit we always use the Veress needle, but we have never had iatrogenic lesions, because all the interventions were performed by surgeons with complete learning curve in laparoscopic surgery in a high-volume laparoscopic centre.
Some studies have supposed that fibrin glue for mesh fixation could guarantee lower incidence of post-operative pain compared with staples fixation, without compromising safety and effectiveness [14, 24,25,26,27,28,29]. However, our subgroup analysis could not show relevant differences between the two mesh fixation methods. Our choice of mesh fixation depends on the size of hernia defect. No postoperative cases of acute pain were reported after the use of tacks, and this could be due to the attention that is placed in their positioning.
Literature is strongly limited regarding long-term results of emergency groin hernia repair: until our research, the longest follow-up time was 3 years [10, 13]. Indeed, our study is the first that has extended this period to 4.7 years (exactly 1718 days), in a range from 264 to 3875 days. During this time, none of our patients had long-term recurrences or complications. The 8 cases (19%) of death occurred in the follow-up were not directly associable with our emergency treatment, the shorter follow-up registered (264 days) is one of these cases. Compared to the state of research, rate of recurrences ranged from 0 to 5%, and no complication after the first post-operative month occurred [7,8,9,10,11,12,13,14]. These data highlight that TAPP approach in urgent groin hernias leads to a low rate of recurrence and complications, whether in a short- or long-term follow-up.
The single contralateral groin hernia repair after the emergency surgery highlighted that this approach is effective in avoiding subsequent surgical procedure. This evidence directly derives from the extended view given by laparoscopic technique.
Up to now, only few articles have focussed on the opportunity of TEP technique in urgent inguinal hernias [7]. Not only, but evidence on the safety technique has also not been very consistent [30, 31]. In fact, TEP technique is more challenging than TAPP in case of big sac to be reduced and does not offer a wide view as well as the opportunity to monitor visceral vitality.
In a recent paper by M. E. Peña et al., postoperative long-term outcomes after elective laparoscopic inguinal hernia repair were analysed [32]. In this study, an increase in recurrence rate was found (from 1.5 to 2.6%) after extending the postoperative follow-up from 2 to 5 years. Moreover, smoking habit of the patients and limited surgical expertise on TAPP approach were described as significant risk factors of recurrence. This result was not corroborated by the outcomes of our series.
Conclusions
TAPP approach is a safe, feasible and effective therapeutic option for emergency groin hernias, with low complication and no recurrence rate on long-term follow-up (up to 4.7 years). Further comparative studies with other surgical techniques are required to assess the best therapeutic approach in this setting.
Data availability
The data sets supporting the results of this article are included within the article in the additional files.
References
Perko Z, Rakić M, Pogorelić Z, Družijanić N, Kraljević J (2011) Laparoscopic transabdominal preperitoneal approach for inguinal hernia repair: a five-year experience at a single center. Surg Today 41(2):216–221. https://doi.org/10.1007/s00595-010-4266-4
HerniaSurge Group (2018) International guidelines for groin hernia management. Hernia 22(1):1–165
Scheuermann U, Niebisch S, Lyros O, Jansen-Winkeln B, Gockel I (2017) Transabdominal Preperitoneal (TAPP) versus Lichtenstein operation for primary inguinal hernia repair—a systematic review and meta-analysis of randomized controlled trials. BMC Surg 17(1):55
Köckerling F, Schug-Pass C (2014) Tailored approach in inguinal hernia repair—decision tree based on the guidelines. Front Surg 20(1):20. https://doi.org/10.3389/fsurg.2014.00020
Bittner R, Arregui ME, Bisgaard T, Dudai M, Ferzli GS, Fitzgibbons RJ et al (2011) Guidelines for laparoscopic (TAPP) and endoscopic (TEP) treatment of inguinal Hernia [International Endo hernia Society (IEHS)]. Surg Endosc 25:2773–2843. https://doi.org/10.1007/s00464-011-1799-6
Poelman MM, vanden Heuvel B, Deelder JD, Abis GSA, Beudeker N, Bittner R et al (2013) EAES Consensus Development Conference on endoscopic repair of groin hernias. Surg Endosc 27:3505–3519. https://doi.org/10.1007/s00464-013-30001-9
Deeba S, Purkayastha S, Paraskevas P, Athanasiou T, Darzi A, Zaachiarakis E (2009) Laparoscopic approach to incarcerated and strangulated inguinal hernias. JSLS 13:327–331
Siow SL, Mahendran HA, Hardin M, Chea CH, Nik Azim NA (2013) Laparoscopic transabdominal approach and its modified technique for incarcerated scrotal hernias. Asian J Surg 36(2):64–68
Legnani GL, Rasini M, Pastori S, Sarli D (2008) Laparoscopic trans-peritoneal hernioplasty (TAPP) for the acute management of strangulated inguino-crural hernias: a report of nine cases. Hernia 12(2):185–188
Liu J, Shen Y, Nie Y, Zhao X, Wang F, Chen J (2021) If laparoscopic technique can be used for treatment of acutely incarcerated/strangulated inguinal hernia? World J Emerg Surg 16(1):5. https://doi.org/10.1186/s13017-021-00348-1
Leibl BJ, Schmedt CG, Kraft K, Kraft B, Bittner R (2001) Laparoscopic transperitoneal hernia repair of incarcerated hernias: is it feasible? Surg Endosc 15:1179–1183
Rebuffat C, Galli A, Scalambra MS, Balsamo F (2006) Laparoscopic repair of strangulated hernias. Surg Endosc 20(1):131–134. https://doi.org/10.1007/s00464-005-0171-0
Mancini R, Pattaro G, Spaziani E (2019) Laparoscopic trans-abdominal preperitoneal (TAPP) surgery for incarcerated inguinal hernia repair. Hernia 23(2):261–266
Shuo Y, Guangyong Z, Cujhong J, Jinxin C, Yilin Z, Yingmo S, Minggang W (2016) Transabdominal preperitoneal laparoscopic approach for incarcerated inguinal hernia repair. Medicine (Baltimore) 95(52):e5686
Neumayer L, Giobbie-Hurder A, Jonasson O et al (2004) Open mesh versus laparoscopic mesh repair of inguinal hernia. N Engl J Med 350:1819–1827
McCormack K, Scott NW, Go PM, Ross S, Grant AM, EU Hernia Trialists Collaboration (2003) Laparoscopic techniques versus open techniques for inguinal hernia repair. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD001785
Hallén M, Bergenfelz A, Westerdahl J (2008) Laparoscopic extraperitoneal inguinal hernia repair versus open mesh repair: longterm follow-up of a randomized controlled trial. Surgery 143:313–317
Morales-Conde S, Socas M, Fingerhut A (2012) Endoscopic surgeons’ preferences for inguinal hernia repair: TEP, TAPP, or OPEN. Surg Endosc 26(9):2639–2643. https://doi.org/10.1007/s00464-012-2247-y
Watson SD, Saye W, Hollier PA (1993) Combined laparoscopic incarcerated herniorrhaphy and small bowel resection. Surg Laparosc Endosc 3:106–108
Poelman MM, van den Heuvel B, Deelder JD, Abis GS, Beudeker N, Bittner R et al (2013) EAES Consensus Development Conference on endoscopic repair of groin hernias. Surg Endosc 27:3505–3519
Jagad RB, Shah J, Patel GR (2009) The laparoscopic trans peritoneal approach for irreducible inguinal hernias: perioperative outcome in four patients. J Minim Access Surg 5(2):31–34
Scierski A (2004) Laparoscopic operations of incarcerated inguinal and femoral hernias. Wiad Lek 57:245–248
Ishihara T, Kubota K, Eda N, Ishibashi S, Haraguchi Y (1996) Laparoscopic approach to incarcerated inguinal hernia. Surg Endosc 10:1111–1113. https://doi.org/10.1007/s004649900254
Andresen K, Fenger AQ, Burcharth J, Pommergaard HC, Rosenberg J (2017) Mesh fixation methods and chronic pain after transabdominal pre-peritoneal (TAPP) inguinal hernia surgery: a comparison between fibrin sealant and tacks. Surg Endosc 31(10):4077–4084
Harsløf S, Krum-Møller P, Sommer T, Zinther N, Wara P, Friis- Andersen H (2018) Effect of fixation devices on post-operative pain after laparoscopic ventral hernia repair: a randomized clinical trial of permanent tacks, absorbable tacks, and synthetic glue. Langenbecks Arch Surg 403(4):529–537
Phillips AW, Viswanath YKS, Burns JK, Hall CEJ, Horgan AF (2014) Use of fibrin glue for fixation of mesh and approximation of peritoneum in transabdominal pre-peritoneal (TAPP) inguinal hernia repair: technical feasibility and early surgical outcomes. Surg Laparosc Endosc Percutan Tech 24(2):e43–e45
Wilson P, Hickey L (2019) Laparoscopic transabdominal pre-peritoneal (TAPP) groin hernia repair using n-butyl-2-cyanoacrylate (Liquiband®Fix8TM) for mesh fixation and peritoneal closure: learning experience during introduction into clinical practice. Hernia 23(3):601–661
Lovisetto F, Zonta S, Rota E, Mazzilli M, Bardone M, Bottero L, Faillace G, Longoni M (2007) Use of human fibrin glue (Tissucol) versus staples for mesh fixation in laparoscopic transabdominal pre-peritoneal hernioplasty: a prospective, randomized study. Ann Surg 245(2):222–231
Ielpo B, Nuñez J, Ferri V, Silva J, Quijano Y, Vicente E, Caruso R, Giuliani A, Pellino G (2021) Laparoscopic inguinal hernia repair: cost-effectiveness analysis of trend modifications of the technique. Updates Surg. https://doi.org/10.1007/s13304-021-01005-7
Ferzli G, Shapiro K, Chaudry G, Patel S (2004) Laparoscopic extraperitoneal approach to acutely incarcerated inguinal hernia. Surg Endosc 18:228–231
Saggar VR, Sfrangi R (2005) Endoscopic totally extraperitoneal repair of incarcerated inguinal hernia. Hernia 9:120–124
Peña ME, Dreifuss NH, Schlottmann F, Sadava EE (2019) Could long-term follow-up modify the outcomes after laparoscopic TAPP? A 5-year retrospective cohort study. Hernia 23(4):693–698. https://doi.org/10.1007/s10029-019-01953-5
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest and no funding.
Ethical approval
Approval from the institutional review board was not required for this study.
Human and animal rights
The present study has been conducted in accordance with the ethical standards of the Institutionals and National responsible committees.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Zanoni, A.A.G., Delcarro, A., Ciccarese, F. et al. Laparoscopic transperitoneal hernia repair (TAPP) in emergency: long-term follow-up in a high volume centre. Hernia 26, 1063–1068 (2022). https://doi.org/10.1007/s10029-021-02516-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-021-02516-3