Abstract
Purpose
An association of anxiety with surgical outcomes has been suggested, including with open ventral hernia repair (OVHR). This study examines the interaction of multiple comorbidities, including anxiety, depression, chronic pain, and hernia characteristics with outcomes after OVHR.
Methods
Patients with anxiety were identified in an existing, prospectively collected, data set of OVHR with preoperative work-up including CT scans (2007–2018). A patient with a diagnosis or prescription for anxiolytics, anti-depressants, or narcotics was considered to have anxiety, depression, or chronic pain, respectively. Hernia characteristics were analyzed using 3D volumetric software. Univariate and multivariate analyses were performed to assess for the impact of anxiety on surgical outcomes.
Results
A total of 1178 OVHRs were identified. The diagnosis of anxiety (23.9%) was associated with female gender (29.1% females vs. 16.9% males, p = 0.002), depression (56.7 vs. 18.8%, p < 0.0001), preoperative chronic pain (43.6 vs. 26.9%, p < 0.0001), COPD, arrhythmia, history of MRSA, and sleep apnea (p ≤ 0.05 all values). Patients with anxiety had larger hernia volume and defect size, and were more likely to undergo component separation, with higher rates of wound complication and intervention for pain (p ≤ 0.05 all values). After multivariate analysis controlling for multiple potentially confounding factors, the comorbidities of anxiety, depression, and preoperative chronic pain were not found to be significantly associated with adverse outcomes.
Conclusions
The diagnosis of anxiety is associated with preoperative comorbidity, surgical complexity, and adverse outcomes after OVHR. However, when comorbidities are controlled for, the diagnosis of anxiety, depression or preoperative pain does not independently predict adverse outcomes. In this context, anxiety may be considered a marker of patient comorbidity in a complex patient population.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The association of psychological diagnosis with outcomes after surgery has been an object of study for decades. The estimated global prevalence of anxiety is 7.3%–16.2%, accounting for the 6th leading cause of disability worldwide [1-3]. Anxiety disorders share the characteristics of excessive fear and apprehension, with related behavioral disturbances. Generalized anxiety disorder is characterized by over 6 months of excessive and/or persistent worrying which causes significant distress or impairment [4]. The traits of depression, anxiety, and chronic pain are considered correlated, with depression and anxiety associated with development and persistence of both acute and chronic pain [5, 6]. This has important implications for management of surgical patients, as these diagnoses may impact postoperative resolution of symptoms. In 1986, Taenzer et al. established an association between patient trait anxiety and postoperative outcomes of anxiety, depression, and chronic pain after cholecystectomy [7], a finding which Mertens et al. has since repeated [8]. With several publications suggesting a connection between diagnoses of anxiety and experience of postoperative pain, a patient’s perioperative experience may be influenced by pre-existing diagnoses of depression, anxiety and/or chronic pain [9].
Apart from the association of preoperative with postoperative psychological diagnosis, the association of preoperative depression and anxiety with morbidity and mortality after cardiac intervention has been suggested. After cardiac surgery, this includes increased length of stay, persistence of post-surgical pain, and higher rates of readmission, morbidity, mortality [10-12]. The causative link of these adverse outcomes is not yet elucidated, as differences in outcomes persist even after controlling for higher rates of COPD, hypertension, tobacco use, and obesity in patients with anxiety [12]. This correlation of anxiety with patient comorbidity and adverse outcomes has been occasionally duplicated in non-cardiac surgery [13].
In the setting of hernia repair, the association of preoperative symptoms with postoperative pain and quality of life has been well established [14-17]. However, few studies have investigated the relationship of chronic pain, anxiety, and depression with adverse outcomes after surgical intervention. In 2018, Neff et al. established an association of anxiety with longer length of stay and higher readmission rates after hernia repair, but this association was not present after controlling for multiple confounding comorbidities [18]. Here we aim to examine the relationship of preoperative psychological diagnoses, specifically anxiety, depression and pain, on outcomes after open ventral hernia repair (OVHR).
Methods
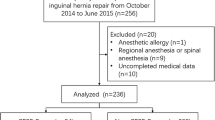
A prospective, hernia-specific, institutional database was queried for patients undergoing open ventral hernia repair (OVHR) from 2007 to 2018. Patients were identified who had one adequate preoperative CT scan within 1 year of OVHR. Adequate CT scans included the entirety of the abdomen, pelvis, and hernia sac. For the purpose of this study, a diagnosis of anxiety was defined as an existing prescription for anxiolytics for anxiety disorder, or a documented diagnosis of anxiety in the medical record. Preoperative chronic pain was defined as an existing opioid prescription and/or relationship with pain specialist before operative intervention. Postoperative intervention for pain was defined as referral to a pain specialist and/or procedural intervention such as suture injection or surgery for continued pain. Demographics, operative and hernia details, and outcomes were reviewed. The outcomes of interest were wound complication, readmission, reoperation, hernia recurrence, and percutaneous drain placement, as well as systemic complications such as pneumonia, reintubation, sepsis, urinary tract infection, cardiac dysrhythmias. This study was approved by the Institutional Review Board of Carolinas Medical Center.
3D CT measurements
Analysis of CT scans was performed with Terarecon software Aquarius, iNtuition Edition version 4.4.13. This three-dimensional volumetric software outlines the abdominal wall and captures intra-abdominal fat volume (IAV), subcutaneous fat volume (SQV), and hernia volume (HV). Calculations were performed and corrected by a blinded reviewer for each patient. To ensure reviewer accuracy, two independent, blinded reviewers measured a subset of 100 patients and found excellent concordance between results. The hernia defect was measured in length and width for each patient. Based on prior studies, the abdominal compartment was measured from the top of the diaphragm to the superior border of the pubic symphysis [19]. The hernia volume (HV) was calculated from the top of the hernia sac or defect to the bottom of the hernia sac or defect, whichever was greater. When the sac overhung the pubic symphysis, it was measured from the most inferior point. The ratio of hernia volume-to-intra-abdominal volume was calculated (HV:IAV).
Statistical analysis
Standard statistical methods were utilized to analyze data in the SAS® Program version 9.4 (SAS, Cary, NC, USA). Means and standard deviations were utilized to describe continuous variables and counts and percentages were used for categorical variables. T-tests and Wilcoxon–Mann Whitney tests were used to compare continuous variables. Chi-square and Fisher’s exact tests were used to compare categorical variables. Statistical significance was set at p ≤ 0.05.
Multivariate analysis was performed to control for potential confounding factors including BMI, defect size, hernia volume, anxiety, sex, asthma, arrhythmia, COPD, depression, MRSA, preoperative chronic pain, number of previous surgeries, and case contamination. Variables used in multivariate logistic regression were selected based on factors identified as statistically different between groups in univariate analysis (p < 0.05), and factors known to potentially influence operative outcomes based on prior hernia studies. The level of significance was set at p < 0.05 for all comparisons.
Results
A total of 1,178 OVHR patients were identified who met inclusion criteria. Mean age was 58.5 ± 12.4 years, mean BMI 34.2 ± 7.7 kg/m2, and 57.8% of patients were female. The diagnosis of anxiety was present in 23.9% of patients (n = 282), with significant differences in comorbidities between groups. Patients with the diagnosis of anxiety were more likely to be female (29.1% females vs. 16.9% males), had a higher number of previous abdominal surgeries (3.2 ± 1.6 vs. 2.9 ± 1.4, p = 0.002), to have depression (56.7 vs. 18.8%, p < 0.0001), and to have preoperative chronic pain (43.6 vs. 26.9%, p < 0.0001). Patients with anxiety also had higher rates of COPD, arrhythmia, history of MRSA, and sleep apnea (Table 1). There was no difference in BMI, chronic steroid use, diabetes, or history of tobacco use between patients who did and did not have the diagnosis of anxiety (Table 1).
Upon review of hernia and CT characteristics, patients with anxiety had larger mean defect area (166.6 ± 144.0 vs. 145.5 ± 133.9 cm2, p = 0.04) and larger mean hernia volume (1,131.9 ± 1,525.4 cm3, p = 0.05 vs. 912.8 ± 1218.3) (Table 2). There was no difference in history of previous hernia recurrence, number of prior hernia repairs, subcutaneous fat volume, or intra-abdominal volume. In the operating room, patients with anxiety were more likely to undergo component separation (55.3 vs. 46.3%, p = 0.008), with advancement flaps (70.2 vs. 62.5%, p = 0.02). They also had higher rates of case contamination, which approached statistical significance (30.9 vs. 25.1%, p = 0.06) (Table 3).
After OVHR, patients with anxiety had a higher rate of wound complication (38.3 vs. 31.2%, p = 0.03), longer length of stay (9.1 ± 9.8 vs. 8.0 ± 6.0 days, p = 0.002), and were more likely to require intervention for pain (24.1 vs. 15.5%, p = 0.009). There was no difference in readmission, reoperation, or recurrence, or of systemic complications such as pneumonia, reintubation, or septicemia (Table 4).
A multivariate analysis was performed to control for the multiple potential confounding factors in this analysis (Table 5). The comorbidities of anxiety, depression, hernia volume, arrhythmia, history of MRSA infection, and preoperative chronic pain were not found to be significantly associated with reoperation, readmission, recurrence, wound complication, systemic complications, pneumonia, reintubation, septicemia or postoperative intervention for pain. Wound complications were found to be associated with BMI (OR 1.07, CI 1.05–1.09), female sex (OR 1.41, CI 1.02–1.94), COPD (OR 2.74, CI 1.47–4.16), and wound contamination (OR 2.13, CI 1.53–2.96). Reoperation for hernia-related complications was associated with defect size (PR 1.02, CI 1.01–1.03) and asthma (OR 1.54, CI 1.03–2.28). Readmission was associated with BMI (OR 1.02, CI 1.01–1.04), female gender (OR 1.77, CI 1.25–2.51), COPD (OR 1.86, CI 1.12–3.10), and wound contamination (OR 1.66, CI 1.17–2.35). Hernia recurrence was also associated with wound contamination (OR 3.74, CI 2.38–5.88).
Discussion
This study demonstrates a significant difference in preoperative comorbidity and surgical outcomes between patients with and without the diagnosis of anxiety. However, this difference does not seem to be directly attributable to the diagnosis of anxiety. Patients with anxiety are more likely to be female, with the diagnosis of COPD, depression, MRSA, sleep apnea, and preoperative chronic pain. They have larger hernia volume and defect size, a higher number of previous abdominal surgeries, are more likely to have case contamination, and to undergo component separation and/or advancement flap. In the setting of these significant comorbidities, it is unsurprising that patients with anxiety have greater length of stay, wound complication, and postoperative intervention for pain.
When the potentially confounding comorbidities in the anxiety patient population are controlled for, anxiety, depression, and pain are not found to be independent predictors of adverse outcomes after OVHR. These patients are significantly more complex, and thus experience adverse outcomes at a higher rate. Previous studies have noted this correlation of patient comorbidity with anxiety, but have often found a persistent association of anxiety with patient outcomes after controlling for such comorbidities [10-13].
With 23.9% incidence, this patient population has a higher rate of preoperative anxiety than other surgical and non-surgical populations. This includes worldwide estimates which place the baseline rate of anxiety disorders at approximately 7.3–16.2% [1, 3], and studies with similar inclusion criteria which found a rate of 15.6% in the general surgery and hernia population [13, 18]. It is unclear what the source of this high rate of anxiety is, though it may be attributable to the significantly comorbid population and the high percentage of patients with previously failed hernia repairs referred to a tertiary hernia center [20, 21]. As anxiety is persistently associated with a more comorbid patient population, this study is not structured to examine “cause or effect” of this relationship. Anxiety disorder is associated with adrenergic overproduction of cortisol and other stress hormones which do impact immunologic and inflammatory responses [22]. We cannot determine whether the chronic stress associated with anxiety has led to increased patient comorbidity, or if chronic illness and/or multiple hospitalizations have led to or exacerbated the diagnosis of anxiety disorder.
Although this is a prospective data set, an important limitation of this study is the retrospective nature of data capture of anxiolytic medications. This does not capture the treatment duration, compliance, or severity of anxiety disorder experienced by the patient, all of which can impact outcomes [12]. A similar lack of information is available on the diagnosis of depression and chronic pain, as the record of active prescriptions and/or diagnosis is presumed to represent the patients’ current state at the time of surgery. Finally, the outcome of intervention for chronic pain is a high standard, and likely does not reflect any continued discomfort or dissatisfaction of patients who did not follow-up at this tertiary hernia center or did not deem their symptoms worthy of pursuit for intervention.
The potential benefits of pre and postoperative intervention for anxiety, chronic pain, and depression in surgical patients can extend well beyond psychological well-being. The intervention of choice in patients identified as anxious in the perioperative setting is cognitive behavioral therapy (CBT). CBT is often specifically targeted to management of the stressors and outcomes associated with surgery and has been demonstrated to improve general and operation-specific outcomes in surgical populations. Patients with kinesiophobia after total knee arthroplasty significantly benefit from CBT, with decreased kinesiophobia, pain catastrophizing, and joint inhibition for over 6 months after intervention [23]. After cardiac surgery, CBT has been shown to improve quality of life and heart rate variability [24]. Preoperative intervention with CBT has been associated with improvement in anxiety, depression, and quality of life, as well as readmission and length of stay after prostatectomy, breast cancer, and CABG [25-27]. Validated screening tools for identification of patients at risk for anxiety and associated complications include the State Trait Anxiety Inventory, and the Hospital Anxiety and Depression Trial [5, 8, 12, 28, 29]. After identification of this higher-risk population, appropriate pre and postoperative intervention has the potential to improve length of stay, readmission, quality of life, the development of chronic pain, and multiple other relevant surgical outcomes.
The diagnosis of anxiety and/or use of anxiolytic medications is associated with increased preoperative comorbidity, more extensive surgical intervention, and adverse outcomes of wound complications, length of stay, and intervention for pain in patients undergoing open ventral hernia repair. However, when comorbidities are controlled for, the diagnosis of anxiety does not independently predict these adverse outcomes. As the etiology of the observed relationship between anxiety and patient comorbidity is not fully elucidated, the diagnosis of anxiety may be considered a marker of patient comorbidity in a baseline complex population.
References
Baxter AJ, Scott KM, Vos T, Whiteford HA (2013) Global prevalence of anxiety disorders: a systematic review and meta-regression. Psychol Med 43:897–910. https://doi.org/10.1017/S003329171200147X
Baxter AJ, Vos T, Scott KM et al (2014) The global burden of anxiety disorders in 2010. Psychol Med 44:2363–2374. https://doi.org/10.1017/S0033291713003243
Kessler RC, Aguilar-Gaxiola S, Alonso J et al (2009) The global burden of mental disorders: an update from the WHO World Mental Health (WMH) surveys. Epidemiol Psichiatr Soc 18:23–33
American Psychiatric Association (2013) Diagnostic and Statistical Manual of Mental Disorders. American Psychiatric Association, Philadelphia
Lerman SF, Rudich Z, Brill S et al (2015) Longitudinal associations between depression, anxiety, pain, and pain-related disability in chronic pain patients. Psychosom Med 77:333–341. https://doi.org/10.1097/PSY.0000000000000158
Erdogan E, Ozenc E (2018) Factors associated with acute and chronic pain after inguinal herniorraphy. Rom J Anaesth Intensive Care 25:31–35. https://doi.org/10.21454/rjaic.7518.251.oze
Taenzer P, Melzack R, Jeans ME (1986) Influence of psychological factors on postoperative pain, mood and analgesic requirements. Pain 24:331–342
Mertens MC, Roukema JA, Scholtes VPW, De Vries J (2011) Trait anxiety predicts outcome 6 weeks after cholecystectomy. A prospective follow-up study. Ann Behav Med 41:264–269. https://doi.org/10.1007/s12160-010-9245-x
Hah JM, Bateman BT, Ratliff J et al (2017) Chronic opioid use after surgery. Anesth Analg 125:1733–1740. https://doi.org/10.1213/ANE.0000000000002458
Tully PJ, Baker RA, Knight JL (2008) Anxiety and depression as risk factors for mortality after coronary artery bypass surgery. J Psychosom Res 64:285–290. https://doi.org/10.1016/j.jpsychores.2007.09.007
Tully PJ, Baker RA, Turnbull D, Winefield H (2008) The role of depression and anxiety symptoms in hospital readmissions after cardiac surgery. J Behav Med 31:281–290. https://doi.org/10.1007/s10865-008-9153-8
Williams JB, Alexander KP, Morin J-F et al (2013) Preoperative anxiety as a predictor of mortality and major morbidity in patients aged %3e70 years undergoing cardiac surgery. Am J Cardiol 111:137–142. https://doi.org/10.1016/j.amjcard.2012.08.060
Ward N, Roth JS, Lester CC et al (2015) Anxiolytic medication is an independent risk factor for 30-day morbidity or mortality after surgery. Surgery 158:420–427. https://doi.org/10.1016/j.surg.2015.03.050
Belyansky I, Tsirline VB, Klima DA et al (2011) Prospective, comparative study of postoperative quality of life in TEP, TAPP, and modified Lichtenstein repairs. Ann Surg 254:705–709. https://doi.org/10.1097/SLA.0b013e3182359d07
Groene SA, Heniford DW, Prasad T et al (2016) Identifying effectors of outcomes in patients with large umbilical hernias. Am Surg 82:613–621
Tsirline VB, Colavita PD, Belyansky I et al (2013) Preoperative pain is the strongest predictor of postoperative pain and diminished quality of life after ventral hernia repair. Am Surg 79:829–836
Groene SA, Prasad T, Lincourt AE et al (2016) Prospective, multi-institutional surgical and quality-of-life outcomes comparison of heavyweight, midweight, and lightweight mesh in open ventral hernia repair. Am J Surg 212:1054–1062. https://doi.org/10.1016/j.amjsurg.2016.09.003
Neff C, Totten C, Plymale M et al (2018) Associations between anxiolytic medications and ventral hernia repair. Herina 22:753–757. https://doi.org/10.1007/s10029-018-1766-4
Agnew SP, Small W, Wang E et al (2010) Prospective measurements of intra-abdominal volume and pulmonary function after repair of massive ventral hernias with the components separation technique. Ann Surg 251:981–988. https://doi.org/10.1097/SLA.0b013e3181d7707b
Schlosser KA, Arnold MR, Kao AM et al (2018) Building a multidisciplinary hospital-based abdominal wall reconstruction program. Plast Reconstr Surg 142:201S–208S. https://doi.org/10.1097/PRS.0000000000004879
Colavita PD, Walters AL, Tsirline VB et al (2013) The regionalization of ventral hernia repair: occurrence and outcomes over a decade. Am Surg 79:693–701
Heim C, Ehlert U, Hellhammer DH (2000) The potential role of hypocortisolism in the pathophysiology of stress-related bodily disorders. Psychoneuroendocrinology 25:1–35
Cai L, Gao H, Xu H et al (2018) Does a program based on cognitive behavioral therapy affect kinesiophobia in patients following total knee arthroplasty? A randomized, controlled trial with a 6-month follow-up. J Arthroplasty 33:704–710. https://doi.org/10.1016/j.arth.2017.10.035
Beresnevaitė M, Benetis R, Taylor GJ et al (2016) Impact of a cognitive behavioral intervention on health-related quality of life and general heart rate variability in patients following cardiac surgery: an effectiveness study. Psychosomatics 57:605–615. https://doi.org/10.1016/j.psym.2016.04.004
Parker PA, Pettaway CA, Babaian RJ et al (2009) The effects of a presurgical stress management intervention for men with prostate cancer undergoing radical prostatectomy. J Clin Oncol 27:3169–3176. https://doi.org/10.1200/JCO.2007.16.0036
Dao TK, Youssef NA, Armsworth M et al (2011) Randomized controlled trial of brief cognitive behavioral intervention for depression and anxiety symptoms preoperatively in patients undergoing coronary artery bypass graft surgery. J Thorac Cardiovasc Surg 142:e109–e115. https://doi.org/10.1016/j.jtcvs.2011.02.046
Matthews H, Grunfeld EA, Turner A (2017) The efficacy of interventions to improve psychosocial outcomes following surgical treatment for breast cancer: a systematic review and meta-analysis. Psychooncology 26:593–607. https://doi.org/10.1002/pon.4199
Wilson CJ, Mitchelson AJ, Tzeng TH et al (2016) Caring for the surgically anxious patient: a review of the interventions and a guide to optimizing surgical outcomes. Am J Surg 212:151–159. https://doi.org/10.1016/j.amjsurg.2015.03.023
Osborne RH, Elsworth GR, Sprangers MAG et al (2004) The value of the Hospital Anxiety and Depression Scale (HADS) for comparing women with early onset breast cancer with population-based reference women. Qual Life Res 13:191–206. https://doi.org/10.1023/B:QURE.0000015292.56268.e7
Funding
This research has no direct funding to disclose.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
B. Todd Heniford MD is a speaker with Allergan and an advisory for WL Gore. Vedra A. Augenstein MD is a speaker with Allergan, Intuitive, Acelity. Kathryn A. Schlosser MD, Sean R. Maloney MD, and Tanushree Prasad have no disclosures.
Ethical approval
This study was approved by the Internal Review Board of the Carolinas Medical Center and adheres to ethical, human, and animal rights standards therein.
Human and animal rights
All the procedures performed in the study were in accordance with the ethical standards of the institutional review board of the Carolinas Medical Center and with the 1964 Helsinki Declaration and its later amendments.
Informed consent
For this retrospective review, formal consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Schlosser, K.A., Maloney, S.R., Prasad, T. et al. The impact of preoperative anxiety, depression, and chronic pain on outcomes in abdominal wall reconstruction. Hernia 23, 1045–1051 (2019). https://doi.org/10.1007/s10029-019-02059-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-019-02059-8



