Abstract
Objectives
The primary aim of this study was to identify the incisional hernia rate after temporary loop ileostomy closure. Secondary outcomes were determining the risk factors linked to this incisional hernia, which could improve the patient selection for mesh prophylaxis.
Methods
Retrospective cohort study of all consecutive patients with temporary loop ileostomy reversal through a peristomal incision from 1st January 2011 to 1st January 2017 at our centre. Data were extracted from electronic clinical records: baseline patient characteristics, surgical factors and postoperative events. CT scans performed during follow-up were precisely analysed. Survival analysis was applied to identify risk factors for hernia development.
Results
129 patients were analysed of whom 15 (11.6%) developed an incisional hernia at previous ileostomy site. The median time for incisional hernia development was 11 months (IQR = 7–21) and the median follow-up time was 37 months (IQR = 22–57). The identified patient risk factors for hernia development in survival analysis were female sex, older age, higher Body Mass Index, clinically significant parastomal hernia, clinically detectable midline incisional hernia and major postoperative complications ranked as Clavien–Dindo grade III and IV.
Conclusions
Incisional hernia after temporary loop ileostomy is a relevant problem that affects at least one in every ten patients. The previously cited risk factors might favour its development, therefore the use of a prophylactic mesh should be considered in those high-risk patients.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Background
The confection of a temporary loop ileostomy is a frequently used surgical technique in colorrectal surgery, made to reduce the morbidity associated to high-risk anastomosis leak. Short-term complications after ileostomy closure include leakage of the new anastomosis and surgical site infection (SSI) of previous ileostomy site. Long-term adverse events involve the development of an incisional hernia after ileostomy closure. The initially estimated rate was 4% [1] with a high variability among different studies (0–50%). However, more recent articles quantified the incisional hernia rate after ileostomy closure between 5% [2] and 23.9% [3].
Risk factors for incisional hernia in previous ileostomy site detected until date were: higher body mass index (BMI) [2, 4, 5], lower age, open surgery, longer reversal time and a history of previous hernias [4], a higher blood pressure at preoperative assessment [3, 5], colorectal cancer surgery [5] and midline incisional hernia [3]. Purse-string skin closure has shown a reduction in SSI rates [6], but his effect over future hernia rates remains unknown.
Given the relevance of the problem, some authors began to reinforce the ileostomy closure with the placement of a prophylactic mesh, achieving hernia rates around 5% [7,8,9]. Nevertheless, the systematic use of mesh at the time of stoma closure has yet to be clarified by further studies.
Objectives
The primary aim of this study was to identify the incisional hernia rate after ileostomy closure, defined according to the European Hernia Society (EHS) [10] as “any abdominal wall gap with or without a bulge in the area of a postoperative scar perceptible or palpable by clinical examination or imaging”. Secondary outcomes were determining the risk factors linked to this incisional hernia, which could improve the patient selection for mesh prophylaxis.
Methods
This article was written according to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies [11].
Study design
Single-institution retrospective cohort study.
Setting and participants
All consecutive patients with temporary loop ileostomy reversal through a peristomal incision from 1st January 2011 to 1st January 2017 at a tertiary hospital. Patients were identified through a research in the clinical history records.
Excluded patients were those lost to follow-up, deceased within 30 days after surgery and those with a new stoma formation in previous ileostomy site within 30 days after the first surgery.
Follow-up
Patients were followed until the development of a hernia in previous ileostomy site, their last contact with the institution, new stoma creation in previous ileostomy site 30 days after stoma closure or the death of the patient.
Variables
Data were extracted from electronic medical records: age at ileostomy closure time, sex, Body Mass Index, comorbidity and ASA category, indication of the temporary loop stoma, time to stoma reversal, type of surgical approach, presence of parastomal or midline incisional hernia, and kind of skin closure. The analysed data during follow-up were: postoperative complications according to Clavien–Dindo classification [12], SSI according to the Centers for Disease Control (CDC) definitions [13] with the treatment given to the SSI and incisional hernia in previous ileostomy site during follow-up.
The CT scans done to the patient were analysed from the ileostomy creation until the end of follow-up. In those patients in whom an incisional hernia was detected, CT scans were reviewed in detail to establish the approximate date of hernia formation.
Bias
There might be a selection bias since not every patient underwent a CT scan. The indication of the image studies was given by the baseline pathology of the patient, not by their inclusion in the study.
Study size
Most of previous articles quantified the hernia after ileostomy closure between 11.1% [14] and 14.9% [4]. Therefore, a minimum of 100 participants was needed to have at least 10 events of interest (hernia at the former ileostomy site) to analyse the risk factors.
Statistical analysis
Categorical variables were described as percentages. Quantitative variables were described with mean and standard deviation if they followed a normal distribution and with median and interquartile range (IQR) if they followed a non-normal distribution.
To analyse the risk factors for incisional hernia development, survival analysis was applied. Log-rank test was used for dichotomous categorical variables and Cox-model regression for polytomous categorical and quantitative variables. Hazard ratios and their 95% confidence intervals (CI 95%) were calculated with Cox-model regression. p < 0.05 was considered statistically significant.
The analysis was performed with IBM® SPSS Statistics 23®.
Results
Participants
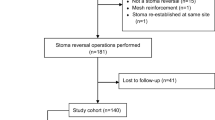
133 patients met inclusion criteria. 4 patients were excluded. Therefore, 129 patients were analysed (Fig. 1).
Baseline characteristics at the moment of stoma closure are shown in Table 1.
20 patients of the total (15.5%) had a clinically detectable parastomal hernia before stoma closure or noticed during ileostomy reversal surgery. 84 patients underwent a CT scan prior to stoma closure and of those, 50 of them (59.5%) had a radiologically detectable parastomal hernia.
During follow-up, 18 patients (13.9%) developed a clinically noticeable midline incisional hernia. The rate of a CT scan measurable midline incisional hernia was higher, with a total of 54 hernias among 120 patients with CT scans, which offers a rate of 45%.
Surgical factors are shown in Table 2.
The rates of early and late postoperative events after ileostomy closure are listed in Table 3.
15 patients (11.6%) developed an incisional hernia in previous ileostomy site. Only 3 (3.1%) of them were diagnosed by clinical examination only. 120 patients underwent a CT scan examination during their follow-up and of those, 15 (12.4%) of them had a hernia at the former stoma site. The median time for incisional hernia development was 11 months (IQR = 7–21). The median follow-up time was 37 months (IQR = 22–57). The Kaplan-Meier curve demostrating the ileostomy site incisional hernia developement is given in Fig. 2.
For our cohort, the identified risk factor for ileostomy site incisional hernia are resumed in Table 4. Patient risk factors for hernia development in survival analysis were female sex (HR 6.13 95% CI 1.95–19.23), age (HR 1.068 95% CI 1.012–1.127) and Body Mass Index (HR 1.218 95% CI 1.082–1.371). Clinically significant parastomal hernia prior to or noted during ileostomy closure was also a risk factor for hernia development (HR 4.16 95% CI 1.48–11.72). Those who had a clinically detectable midline incisional hernia were in an increased risk of ileostomy-site hernia (HR 5.05 95% CI 1.79–14.21). Patients with major postoperative complications, ranked as Clavien–Dindo III and IV, were in a higher risk of hernia (HR 3.95 95% CI 1.10–14.19).
Discussion
Key results
The incisional hernia rate after ileostomy closure was 11.6% with a median time for incisional hernia development of 11 months (IQR = 7–21). Some risk factors were identified: older age, female sex, higher Body Mass Index, clinically detectable parastomal hernia, clinically detectable midline incisional hernia and the presence of postoperative complications grade III and IV according to Clavien–Dindo classification.
Strengths and limitations
One of the strengths of this study is the inclusion of a heterogeneous population sample, and not only patients with rectal cancer. Another aspect is that this study follows the recommendations given by the European Hernia Society [15] with a long follow-up period and the use of abdominal CT scan for the evaluation of the abdominal wall in the majority of the subjects. The main limitation of the study is a wide range in the confidence intervals due to a low rate of events in the patient’s sample, which also prevents from performing a multivariate analysis.
Interpretation
In our study, the incisional hernia rate after temporary ileostomy reversal was 11.6%. This is consistent with the rates found by De Keersmaecker et al. (11.1%) [14], Brook et al. (13.5%) [5] and Fazekas et al. (14.9%) [4]. Consequently, we consider the real rate of ileostomy site hernia as 10–15%, higher than rate offered by De Robles et al. (5%) [2] and lower than the one reported by Kaneko et al. (23.9%) [3].
For our cohort, an older age and female sex were risk factors for hernia development. These results are consistent with those offered by others studies about midline incisional hernia [16]. However, they differ from the findings of Fazekas et al. [4], in which a younger age was a risk factor for incisional hernia. Body Mass Index remains as a risk factor for hernia at ileostomy site, as previously affirmed by Brook et al. [5] and De Robles et al. [2].
In our patients, none of their comorbidities was a hernia risk factor, and neither oncological surgery was linked to future hernia development. Interestingly, the intervention of patients with inflammatory bowel disease did not have a higher incisional hernia rate.
Clinically detected parastomal hernia prior to stoma reversal or discovered during ileostomy closure surgery was a statistically significant risk factor. Therefore, the treatment of these parastomal hernias should be taken into consideration, and probably a mesh might be required.
Classifying postoperative adverse events according to Clavien–Dindo classification [12] allowed this study to identify grade III (requiring surgical, endoscopic or radiological intervention) and grade IV (life-threatening complications requiring intensive care management) complications as variables associated with a higher risk of ileostomy-site incisional hernia. Thus, we suggest that patients requiring reintervention may benefit from the placement of a prophylactic mesh.
For our cohort, neither skin-closure (log-rank = 0.497), postoperative SSI (log-rank = 0.073) or the treatment given to the SSI (log-rank = 0.564), were statistically associated with incisional hernia. Currently, purse-string closure is known as a protection factor for surgical site infection after stoma closure, as stated by Rondelli et al. [6] and Hajibandeh et al. [17]. However, purse-string closure had not shown any reduction in future hernia development in the randomized control trials made until date [18, 19]. In these studies, this variable was a secondary outcome, so new studies should be initiated to address this topic.
Recognising the relevance of incisional hernia after ileostomy closure, some authors began to place a prophylactic mesh during ileostomy reversal, showing their results in non-randomized trials. Liu et al. [7] reduced the incisional hernia rate from 36.1% to 6.4% with an onlay polypropylen mesh. Moreover, Maggiori et al. [8] achieved a 3% hernia rate starting from 19% with a retromuscular biological mesh. Besides, Warren et al. [9] diminished the incisional hernia rate from 13 to 0% with either a retromuscular or preperitoneal polypropylene mesh, although their results were not statistically significant. Further evidence is expected to be collected from the randomized controlled ROCSS [20] and ILEOCLOSE [21] trials.
Meanwhile, according with the results from our study we suggest that a prophylactic mesh might be used in those patients with a higher risk of incisional hernia after ileostomy closure: older patients, females, higher BMI, those with a clinically detectable parastomal hernia and those with major postoperative complications. Moreover, if a midline incisional hernia is detected during follow-up, the presence of an ileostomy site hernia should be considered prior to surgical repair, given the association between them.
Conclusion
Incisional hernia after temporary loop ileostomy is a relevant problem that affects at least one in every ten patients. In this study we identified female sex, older age, higher Body Mass Index, clinically significant parastomal hernia, clinically detectable midline incisional hernia and major postoperative complications ranked as Clavien–Dindo grade III and IV as risk factors for hernia development. Therefore the use of a prophylactic mesh should be considered in those high-risk patients.
References
Bhangu A, Nepogodiev D, Futaba K (2012) Systematic review and meta-analysis of the incidence of incisional hernia at the site of stoma closure. World J Surg 36(5):973–983
De Robles MS, Bakhtiar A, Young CJ (2019) Obesity is a significant risk factor for ileostomy site incisional hernia following reversal. ANZ J Surg 89:399–402
Kaneko T, Funahashi K, Ushigome M et al (2018) Incidence of and risk factors for incisional hernia after closure of temporary ileostomy for colorectal malignancy. Hernia 23:743–748
Fazekas B, Fazekas B, Hendricks J et al (2017) The incidence of incisional hernias following ileostomy reversal in colorectal cancer patients treated with anterior resection. Ann R Coll Surg Engl 99(4):319–324
Brook AJ, Mansfield SD, Daniels IR et al (2018) Incisional hernia following closure of loop ileostomy: the main predictor is the patient, not the surgeon. Surgeon 16(1):20–26
Rondelli F, Franco L, Balzarotti Canger RC et al (2018) Purse-string closure versus conventional primary closure of wound following stoma reversal: meta-analysis of randomized controlled trials. Int J Surg 52:208–213
Liu DSH, Banham E, Yellapu S (2013) Prophylactic mesh reinforcement reduces stomal site incisional hernia after ileostomy closure. World J Surg 37(9):2039–2045
Maggiori L, Moszkowicz D, Zappa M et al (2015) Bioprosthetic mesh reinforcement during temporary stoma closure decreases the rate of incisional hernia: a blinded, case-matched study in 94 patients with rectal cancer. Surgery 158(6):1651–1657
Warren JA, Beffa LR, Carbonell AM et al (2018) Prophylactic placement of permanent synthetic mesh at the time of ostomy closure prevents formation of incisional hernias. Surgery 163(4):839–846
Muysoms FE, Miserez M, Berrevoet F et al (2009) Classification of primary and incisional abdominal wall hernias. Hernia 13(4):407–414
von Elm E, Altman DG, Egger M et al (2007) Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. BMJ 335(7624):806–808
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240(2):205–213
National Healthcare Safety Network, Centers for Disease Control and Prevention (2017) Surgical site infection (SSI) event. http://www.cdc.gov/nhsn/pdfs/pscmanual/9pscssicurrent.pdf. Accesed 1 Mar 2019
De Keersmaecker G, Beckers R, Heindryckx E et al (2016) Retrospective observational study on the incidence of incisional hernias after reversal of a temporary diverting ileostomy following rectal carcinoma resection with follow-up CT scans. Hernia 20(2):271–277
Muysoms FE, Antoniou SA, Bury K et al (2015) European Hernia Society guidelines on the closure of abdominal wall incisions. Hernia 19(1):1–24
Itatsu K, Yokoyama Y, Sugawara GH et al (2014) Incidence of and risk factors for incisional hernia after abdominal surgery. BJS 101:1439–1447
Hajibandeh S, Hajibandeh S, Kennedy-Dalby A et al (2018) Purse-string skin closure versus linear skin closure techniques in stoma closure: a comprehensive meta-analysis with trial sequential analysis of randomised trials. Int J Colorectal Dis 33(10):1319–1332
Camacho-Mauries D, Rodriguez-Díaz JL, Salgado-Nesme N, González QH, Vergara-Fernández O (2013) Randomized clinical trial of intestinal ostomy takedown comparing pursestring wound closure vs conventional closure to eliminate the risk of wound infection. Dis Colon Rectum 56(2):205–211
Sureshkumar S, Jubel K, Ali MS et al (2018) Comparing surgical site infection and scar cosmesis between conventional linear skin closure versus purse-string skin closure in stoma reversal—a randomized controlled trial. Cureus 10(2):e2181
ClinicalTrials.gov (2019) Bethesda (MD): National Library of Medicine (US). Identifier: NCT02238964, Reinforcement of Closure of Stoma Site (ROCSS). https://clinicaltrials.gov/ct2/show/NCT02238964. Accessed 17 Mar 2019
ClinicalTrials.gov (2019) Bethesda (MD): National Library of Medicine (US). Identifier: NCT02226887, Prophylaxis of Ileostomy Closure Site Hernia by Placing Mesh (ILEOCLOSE). https://clinicaltrials.gov/ct2/show/NCT02226887. Accessed 17 Mar 2019
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Barranquero, Tobaruela, Bajawi, Muñoz, Die Trill, Garcia-Perez declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the Institutional Research Committee (Comité de Ética de la Investigación con Medicamentos, 050-19 resolution) and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Human and animal rights
This article does not contain any studies with animals performed by any of the authors.
Informed consent
Informed consent was obtained from all participants before ileostomy closure. Permission to omit the informed consent for analysis of the already available data was obtained from the Institutional Research Committee (050-19 resolution).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Barranquero, A.G., Tobaruela, E., Bajawi, M. et al. Incidence and risk factors for incisional hernia after temporary loop ileostomy closure: choosing candidates for prophylactic mesh placement. Hernia 24, 93–98 (2020). https://doi.org/10.1007/s10029-019-02042-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-019-02042-3