Abstract
Purpose
The aim of this study was to compare perioperative results of robotic IPOM (r-IPOM) and robotic TAPP (r-TAPP) in ventral hernia repair, and to identify risk factors associated with postoperative complications.
Methods
After obtaining balanced groups with propensity score matching, the comparative analysis was performed in terms of perioperative and early outcomes. All variables were also examined in a subset analysis in patients with and without complications. Multivariable regression analysis was used to identify independent risk factors associated with the development of complications.
Results
Of 305 r-IPOM and r-TAPP procedures, 104 patients were assigned to each group after propensity score matching. There was no difference in operative times between two groups. Although postoperative complications were largely minor (Clavien–Dindo grade-I and II), the rate of complications was higher in the r-IPOM group within the first 3-weeks (33.3% in r-IPOM vs. 20% in r-TAPP, p = 0.039). At the 3-month visit, outcomes between groups were not different (p = 0.413). Emergency department re-visits within 30-days and surgical site events were also higher in the IPOM group (p = 0.028, p = 0.042, respectively). In regression analysis, the development of complications was associated with incisional hernias (p = 0.040), intraperitoneal mesh position (p = 0.046) and longer procedure duration (p = 0.049).
Conclusion
Our data suggest r-IPOM may be associated with increased complication rates in the immediate postoperative period when compared to r-TAPP. However, at 3 months, outcomes are comparable. More investigation is needed in this area, specifically with regards to long-term follow-up and multicenter data, to determine the true value of extra-peritoneal mesh placement.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Ventral hernias are one of the most common surgical procedures performed worldwide. It is estimated that the number of ventral and incisional hernias is about 300,000/year in Europe and 400,000/year in the US [1]. Despite several recent advances in the practice of hernia surgery, there remain topics of persistent debate among surgeons including; precise operative technique, defect closure, as well as mesh selection and its position [2].
Over the last 2 decades, laparoscopic IPOM (L-IPOM) repairs have gained in popularity secondary to avoidance of the wide dissection required in open surgery, and its associated wound complications [3]. The International Endohernia Society (IEHS) guidelines [4], describe both laparoscopic transperitoneal and total extra-peritoneal repairs as effective options for the treatment of small- and medium-sized ventral and incisional hernias (EHS classification [5] W1 and W2). An unanswered question, however, remains: “Can preperitoneal repairs be achieved with fewer complications and better long-term results?” [4]. The technical requirements in the execution of laparoscopic ventral hernia through a TAPP approach (L-TAPP) have made this method less popular. However, advantages of the robotic platform have renewed interest in extra-peritoneal mesh placement [6]. Our early experience with TAPP suggests that the robotic platform might enhance the feasibility of preperitoneal mesh placement (r-TAPP) [7]. A current review of the literature revealed that available data are extremely limited comparing the outcomes of L-IPOM and L-TAPP techniques [8] or r-IPOM and r-TAPP [9]. In this study, we aimed to compare r-IPOM and r-TAPP hernia repairs in terms of perioperative outcomes. We hypothesize that there is value in extra-peritoneal mesh placement, which may be observed by a difference between outcomes.
Methods
Study population and design
The data from this study were obtained from a prospectively maintained database of patients who underwent robotic procedures between February 2013 and August 2018. These data included information about demographics (age, sex), the presence of comorbidities, body mass index (BMI), and the American Society Anesthesiologists (ASA) score. Due to limited observations, clinically relevant comorbidities were grouped; such as cardiovascular or peripheral vascular disease (hypertension, hyperlipidemia, myocardial infarction, heart failure, prior heart surgery, and peripheral vascular disease), pulmonary (chronic obstructive pulmonary disease, asthma, dyspnea, pneumonia, and smoking), endocrine (diabetes or thyroid function), and neuropsychiatric (stroke, transient ischemic attack, and psychiatric disorders). For intraoperative variables, categorical data were as follows: hernia etiology (primary ventral/incisional), location of the hernia (midline/off-midline), the ability of the surgeon to close the fascial hernia defect (yes/no), type of mesh, and type of the mesh fixation (suture/tacker/both). Continuous intraoperative variables included the dimensions of the hernia defect and of the mesh itself, the operative time in minutes (console and skin-to-skin), and the estimated blood loss (EBL). The size of the hernia defect was measured according to principles outlined by the European Hernia Society [5]. Accordingly, the width of the hernia defect was defined as the greatest transverse distance in cm between the lateral margins of the hernia defect on both sides. The length of the hernia defect was defined as the greatest vertical distance in cm between the most cranial and the most caudal margin of the defect. In the case of multiple hernia defects, the width was measured between the most laterally located margins of the most lateral defect on that side. The length was between the cranial margin of the most cranial defect and the caudal margin of the most caudal defect. Mesh overlap was defined by the smallest radial distance between the edge of the defect and the edge of the mesh. Using the database, mesh overlap was calculated separately as transverse and cranio-caudal by formulas \(\left( {\frac{{{\text{width of the mesh}} - {\text{width of the defect}}}}{2}} \right)\) and \(\left( {\frac{{{\text{length of the mesh}} - {\text{length of the defect}}}}{2}} \right)\), respectively. The following formulas were used for the calculation of mesh size; \(({\text{width of the mesh }} \times {\text{length of the mesh}})\) for rectangular shaped meshes and \(\left( {\pi \times \frac{\text{width of the mesh}}{2} \times \frac{\text{length of the mesh}}{2}} \right)\) for circle- or oval-shaped meshes. The size of the hernia defect was calculated in cm2 by the formula of (\(\pi \times \frac{\text{width of the defect}}{2} \times \frac{\text{length of the defect}}{2}\)). The ratio of mesh size to defect size (M/D ratio) was also calculated.
The variables collected for perioperative data were; whether or not a procedure had to be converted to open or to a conventional laparoscopic approach, whether extensive adhesiolysis was required (> 30 min), the occurrence and type of intraoperative and postoperative complications, and the length of hospital stay in days. Postoperative pain scores were documented by the anesthesiologist using a 0–10 scoring system (0: no pain, 10: the worst pain). The last pain score was determined at the time point just prior to discharge from the postoperative care unit. Any emergency department (ED) visit within 30 days postoperatively was classified as a revisit. Data regarding complications were collected at the time of clinical visits at 3 weeks and at 3 months after the operation. All complications which occurred during the 3-month follow-up period were categorized with Clavien–Dindo classification system [10].
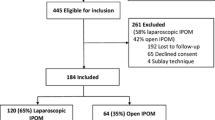
Of this cohort of robotic ventral hernia repairs, only patients who had undergone r-IPOM or r-TAPP repair were included in the study. Exclusion criteria included: patients who underwent a robotically assisted hernia repair by primary closure, extra-peritoneal onlay mesh hernia repair, hernia repair with a hybrid technique, and retrorectus/retromuscular mesh repair, or patients who underwent r-IPOM or r-TAPP concomitantly with other surgical procedures. By matching these two groups, final samples were obtained. The flowchart of patient selection is shown in Fig. 1.
Surgical technique
All operations were performed under general anesthesia with patients in the supine position. Pneumoperitoneum was set to an insufflation pressure of 15 mmHg, and this was established using a Veress needle, placed two fingerbreadths below the costal margin in the left upper quadrant. A total of three trocars were used (two working ports and a single camera port) (Fig. 2).
r-IPOM procedure
All abdominal wall adhesions were divided, when present. The hernia contents were reduced into the abdominal cavity. The peritoneum surrounding the defect was dissected. Umbilical and falciform ligaments, when in the field of mesh placement, were also dissected (Fig. 3a). The fascial defect was measured, and the transverse and cranio-caudal dimensions were recorded (Fig. 3b). Primary closure of the hernia defect was accomplished by running a long-lasting absorbable barbed suture (Stratafix 0™ on CT-1 needle, Ethicon, Somerville, NJ, USA) in reduced intraabdominal pressure (6–8 mmHg) (Fig. 3c). The same guidelines were used for laparotomy closure, which consisted of the small bite technique, taking bites of fascia of 5–8 mm and placing stitches every 5 mm in a shoelace fashion [11]. The mesh is then deployed and secured to the posterior fascia using barbed absorbable sutures (2–0 V-Loc™; Medtronic, Minneapolis, MN, USA) in running fashion or with use of absorbable tackers (AbsorbaTack™; Medtronic, New Haven, CT, USA) (Fig. 3d).
r-TAPP procedure
Using monopolar scissors and a bipolar grasper, the peritoneum was grasped and cut at least 5 cm from the defect on the side ipsilateral to the trocars to enter the preperitoneal space. Preperitoneal dissection was extended at least 5 cm in all directions around the defect to provide adequate mesh deployment (Fig. 4a). In reduced intraabdominal pressure, the hernia defect was closed with a barbed suture as described in the IPOM procedure (Fig. 4b). The mesh was secured to the posterior fascia with an absorbable suture (Fig. 4c). In cases where the integrity of the peritoneum was disrupted during development of the peritoneal pocket, tears were repaired by absorbable sutures. After adequate mesh fixation, the peritoneal flap was closed with a barbed absorbable suture (2–0 V-Loc™; Medtronic, Minneapolis, MN, USA) (Fig. 4d). Following closure of the peritoneal flap, intraabdominal pressure was again increased to asses for dehiscence of the suture-line.
After the procedures were completed, the patient-side cart was undocked. The trocars were removed and the pneumoperitoneum was released. The fascia for trocar sites 10 mm or larger was sutured to decrease the risk of future incisional hernias. Long-acting local anesthetic was injected to the trocar sites for the management of postoperative pain.
Statistical analysis
Descriptive statistics were used to summarize patient demographics, hernia features, operative characteristics, and postoperative outcomes. Categorical variables (qualitative; such as sex or hernia etiology) were presented as frequency with percentage [n (%)] and continuous variables (numerical; such as age or BMI) as mean ± SD or median (interquartile range, IQR), as appropriate. Categorical variables were analyzed using Pearson Chi-Square or Fisher’s Exact Test, and continuous variables using the Independent-Sample t test (for normal distributions) and Mann–Whitney U Test (for non-normal distributions).
Propensity score analysis
A propensity score-matched analysis was performed to obtain comparable groups (r-IPOM and r-TAPP) and eliminate selection bias. Propensity scores were estimated for all patients; these scores represent the probability of group assignment, given observed baseline covariates. After estimation of the propensity score, we matched participants using a simple 1:1 nearest neighbor matching, without replacement. We imposed a caliper of 0.20 of the standard deviation of the logit of the propensity score to obtain similar groups with respect to the set of covariates. Standardized differences were examined to compare patient features before and after matching, with imbalance being defined as an absolute value greater than 0.20 (small effect size).
The two groups were compared in terms of perioperative variables and postoperative early outcomes. All variables were also compared in a subsequent analysis of patients who developed complications and in those without complications at follow-up visits. Multivariate regression analysis was performed to determine the factors associated with the development of complications at follow-up visits.
Statistical assessments were performed using SPSS software pack (Statistical Package for Social Sciences for Windows version 22 software) and R program (version 2.15.2 for Windows). To incorporate these programs and perform propensity score matching analysis, a developer-based software providing a custom dialog in SPSS menu was used [12]. A p value of less than 0.05 was considered statistically significant.
Results
From an initial cohort of 431 consecutive patients who underwent robotic ventral hernia repair, 126 patients were excluded. Our unmatched sample included 305 patients (mean age 52.3 ± 14.4, 50.2% male) who underwent ventral hernia repair utilizing the da Vinci robotic platform. Of these, 57.7% (n = 176) underwent r-IPOM and 42.3% (n = 129) underwent r-TAPP. By matching the two techniques for demographics, preoperative risk factors, as well as hernia characteristics, 208 procedures (104 in each group) were included in the final outcome assessment (Fig. 1). After matching, we examined the overall balance to test the adequacy of our matching. The overall balance test was not significant, confirming that our groups were appropriately distributed [χ2(18) = 7.9, p = 0.98]. A second indication that our matching achieved an improved balance between cohort groups, the relative multivariate imbalance L1 measure was appropriately larger in the unmatched sample (0.966) than in the matched sample (0.952). Table 1 presents the comparison of baseline characteristics of the r-IPOM and r-TAPP groups before and after matching, with respect to standardized differences.
In terms of procedure setting, the rate of emergent repair was similar for matched groups. Although the difference in adhesiolysis that lasted more than 30 min did not reach statistical significance, it was numerically higher in r-IPOM group (7.7% in r-IPOM vs. 3.8% in r-TAPP). Primary defect closure was achieved more often in r-TAPP group as compared to r-IPOM (94.2% vs. 87.5%, respectively, p = 0.092). Even though there were no significant differences in terms of mesh length and width between the groups after matching, the median mesh size (the area of mesh) in cm2 was statistically larger in r-TAPP group (p = 0.128, p = 0.584, p = 0.022, respectively). This difference is likely secondary to calculation of the mesh areas. Rectangular shaped meshes were mostly used in the r-TAPP group rather than the r-IPOM group, where largely circular or oval-shaped meshes were employed (rectangular meshes; 44.2% in r-TAPP vs. 11.5% r-IPOM, p < 0.0001). All meshes (100%) in the r-TAPP group were secured with absorbable sutures, whereas absorbable tackers (with or without suture) were used in 8.7% of r-IPOM procedures (p = 0.003). This difference stems from our practice of abandoning tack fixation after a small initial cohort of preliminary procedures. Table 2 represents the comparison of operative details between r-IPOM and r-TAPP groups.
In consideration of mesh selection; 92.3% of r-IPOM repairs were performed with Symbotex™ (Medtronic, Minneapolis, MN, USA), 3.8% with Synecor™ (W.L. Gore & Associates Inc., Newark, DE, USA), 1.9% with Proceed™ (Ethicon, Somerville, NJ, USA), and 1.9% with Parietex™ (PCO) composite mesh (Medtronic, Minneapolis, MN, USA). In the r-TAPP group, ProGrip™ (Medtronic, Minneapolis, MN, USA) was used in 58.7%, Symbotex™ (Medtronic, Minneapolis, MN, USA) in 38.5%, and Phasix™ (Bard Davol Inc., Warwick, RI, USA) in 1%, Synecor™ (W.L. Gore & Associates Inc., Newark, DE, USA) in 1% and Synecor Pre™ (W.L. Gore & Associates Inc., Newark, DE, USA) in 1% of the procedures. Coated meshes were utilized in 69.7% of all patients, and non-coated meshes were used in 30.3%. There was no association between the use of coated or uncoated mesh and the development of complications during the study period (90-day) (p = 0.151).
In terms of intraoperative complications, serosal injury occurred in two patients (1.9%) in the r-IPOM group, and these were repaired with absorbable suture. Across cohorts, none of the operations required conversion to open or conventional laparoscopic surgery.
After the operation, there were no differences between groups in terms of analgesic medications used. The dosages of fentanyl, hydromorphone hydrochloride, and ketorolac tromethamine did not differ between groups (p = 0.150, p = 0.577, p = 0.333, respectively). The median final pain score before leaving the post-anesthesia care unit according to the 0–10 scoring system was 4 (IQR = 3–5) in the r-IPOM group and 3 (IQR = 3–4) in the r-TAPP group. There was no difference between r-IPOM and r-TAPP patients in terms of pain score at this time point (p = 0.294).
The median length of hospital stay was 0 days (IQR = 0–0) for both groups (range = 0–7 days in r-IPOM vs. 0–4 days in r-TAPP). This shows that a very large majority of patients are discharged on the same day of the procedure. The rate of patients who required overnight in-hospital admission was not different between groups (7.7% in r-IPOM vs 6.7% in r-TAPP, p = 0.789). Re-visits to the Emergency Department (ED) for any reason within 30-days were higher in the r-IPOM group as compared to the r-TAPP group (19.2% in r-IPOM vs. 8.7% in r-TAPP, p = 0.028). There was no association between same-day surgical discharge and ED re-visits (p = 0.445).
The details of complications and comparison between r-IPOM and r-TAPP techniques are given in Table 3. Accordingly, 90.4% of all patients were evaluated at a follow-up visit within 3-weeks of surgery, and the presence of any complication was higher in r-IPOM group when compared to r-TAPP group at this interval (p = 0.039). However, this difference did not persist at the 3-month follow-up visit (p = 0.413). The most frequently reported complication was pain or discomfort in any follow-up period. Of note, no patients reported pain lasting beyond their 3-month visit. Surgical site events (SSEs), including seromas, hematomas, and infections, when taken as a group, were significantly higher in the IPOM group at the initial 3-week follow-up. Taken individually, while the number of each is numerically higher in the IPOM group, secondary to the small number of occurrences, these were not individually significant.
Regarding SSEs, seromas were the most frequently observed surgical site occurrence, though none required procedural intervention. Of 3 r-IPOM patients who experienced a surgical site hematoma, one required drainage secondary to infection. The remaining two patients’ hematomas reabsorbed spontaneously. In 1 r-TAPP patient, a spontaneous rectus sheath hematoma occurred secondary to anticoagulant use. Another reported rectus sheath hematoma was observed in one patient treated with r-IPOM. As a complication, significant bleeding occurred in two patients; one r-IPOM patient with intraabdominal bleeding that required transfusion. The other hemorrhage was secondary to a duodenal ulcer in a r-TAPP patient, which required endoscopic intervention.
According to Clavien–Dindo Classification, most of the observed complications were minor (grade I and II). The distribution of complication grades was as follows; 50% grade-I, 46.9% grade-II, and 3.1% grade-III in r-IPOM group vs. 76.2% grade-I, 19% grade-II, and 4.8% grade-III score in r-TAPP group. Finally, none of the patients experienced hernia recurrence during the follow-up period of this study.
The comparison of patients with and without complications is presented in Table 4. The development of complications was associated with incisional hernias [odds ratio (OR) = 2.428, p = 0.040, 95% confidence interval (CI) 1.040–5.664], intraperitoneal mesh position (OR = 2.027, p = 0.046, 95% CI 1.013–4.059) and with longer procedure duration (console time) (OR = 1.014, p = 0.049, 95% CI 1.000–1.028) in regression analysis corrected for age, sex, and defect area.
Discussion
Laparoscopic IPOM has been utilized for ventral hernia repair since 1993 [13]. Data behind this technique demonstrate lower rates of surgical site infections and decreased hospital stay, as compared to the conventional open methods [1]. While some authors are able to achieve primary closure of the hernia defect during L-IPOM, either trans-cutaneously [14] or intra-corporeally [15], this can be a difficult task to accomplish using conventional laparoscopic instruments [9, 16]. The relative ease of intracorporeal suturing afforded by robotic platforms has gained appeal in hernia repair. This benefit is further emphasized in early reports on the feasibility of RVHR [17]. r-IPOM has evolved over the last few years as a reproducible and effective method of ventral hernia repair [18].
Preperitoneal repairs grew from the practice of IPOMs, based on the concept of utilizing the peritoneum as a barrier between the mesh and abdominal viscera, and in so doing, avoid the rare but perturbative complications of potential adhesive bowel obstructions, mesh erosion, and enterocutaneous fistula [19,20,21]. Chelala et al. [14] shared their findings in a series of 1326 L-IPOM repairs, using coated mesh. In 126 patients who underwent a second-look operation for various reasons, they noted serosal adhesions in 12.69% of patients, minor adhesions in 42.08%, and no adhesions in 45.23%. Mesh-related adhesive complications attributed to IPOM placement have caused surgeons to explore alternative methods of mesh positioning, such as TAPP or retromuscular mesh placement [8, 20,21,22,23].
In a study, Dietz et al. [24] found incisional type hernias to be associated with increased complication rates in multivariate analysis (OR 2.04; 95% CI 1.09–3.84; incisional vs. ventral hernia). In our multivariate analysis, similarly, incisional type hernias were approximately 2.5-fold more likely to develop early postoperative complications than primary ventral hernias. This is likely secondary to the increased complexity and alteration of virgin tissue planes with incisional hernias compared to primary hernias. Adhesiolysis is frequently required, thus contributing to longer operative times, which is also known to be an independent risk factor for complications [25].
In a study with a total of 279 patients, Prasad et al. [8] reported decreased complication rates, though longer operating times, in L-TAPP repair as compared to L-IPOM repair. Similarly, Kennedy et al. [9] reported no complications with r-TAPP as compared to r-IPOM in their initial experience in RVHR. While there was no difference in total operative time between the two methods in this study, console time was longer for r-TAPP. Both the above studies ascribed a difference in operative time to be on account of additional time required for preperitoneal dissection. The average operating duration of our groups was shorter than the above-mentioned studies, possibly due to the smaller hernia size of our final cohorts. Interestingly, there was no difference in terms of operative times in our cohorts (both console and skin-to-skin) between r-IPOM and r-TAPP procedures. This likely stems from the distribution of patients who required extensive adhesiolysis (more than 30 min.) (7.7% in r-IPOM vs 3.8 in r-TAPP). Moreover, our years of experience in r-TAPP may have contributed to shorter operative times. Although in the regression analysis, the length of the procedure emerged an independent risk factor associated with the development of postoperative complications, the odds ratio and confidence interval suggest that the magnitude of the effect could be virtually one-fold, which is clinically negligible. Larger studies may generate more precise effect estimates.
In terms of postoperative pain, we did not find a difference in early postoperative pain scores between the groups, similar to the findings of Prasad et al. [8]. Despite the lack of quantitative pain assessment in our follow-up, we encountered that complaints of postoperative pain or discomfort were more frequent in r-IPOM group, though this difference did not reach statistical significance. Additionally, pain or discomfort was the most frequent reason patients re-presented to the ED within 30-days of surgery, and this re-visit rate was also higher in the r-IPOM group as compared to the r-TAPP group. Prasad et al. [8] suggested transfascial sutures used in L-IPOM may contribute to increased postoperative pain. Although we did not utilize transfascial sutures in either procedure type, we did observe that r-IPOM patients were more likely to complain of pain or discomfort during their postoperative early course. This may be secondary to the need for more extensive fixation of the mesh in IPOM than TAPP irrespective to approach [6]. Limited mesh fixation is usually sufficient in TAPP repair; as the mesh is confined within a pocket created from the layers of the abdominal wall and intraabdominal forces act to hold the mesh in place [19]. Another possible contributing factor to a difference in the perception of pain or discomfort in IPOM patients relates to a potential inflammatory reaction caused by the placement of a foreign body within the peritoneal cavity. This aspect could be better investigated in the future, through the use of specific quality of life assessments, before and after surgery.
In our study, the rate of SSEs, such as seromas, hematomas, and infections, was significantly higher in the r-IPOM group, though when taken individually, these did not reach significance. The most frequently reported SSE following hernia repair is seroma formation, and this occurs in about 30% of cases [19]. Although seroma formation peaks at about postoperative day-7, its resolution is almost complete at 90-day [26]. Furthermore, seroma may be more common with L-IPOM than with L-TAPP [26]. In Prasad et al.’s series [8], authors similarly found the number of seromas were higher in the L-IPOM group, compared to L-TAPP group (8.5% vs. 5.8%), these uniformly resolved without intervention by 12 weeks. Similarly, in our study, seroma was the most frequent SSEs, and occurred more often in r-IPOM group. Hematomas were more frequent in our r-IPOM group as well. One possible explanation for this may be related to the more extensive mesh fixation in r-IPOM repairs, increasing the likelihood of inadvertently disrupting perforating vessels.
Mesh selection in TAPP repair can be affected by the integrity and quality of the peritoneum [22, 23]. In our r-TAPP group, a coated mesh was used in 39.4% of patients, because of a very thin peritoneum or the presence of peritoneal tears. However, this specific feature of mesh selection (coated/non-coated) was not associated with postoperative complications.
In TAPP repair, the risk of bowel obstruction has been suggested to increase with incomplete peritoneal flap closure or its breakdown in preperitoneal hernia repair [27]. None of our patients who underwent r-TAPP repair had a small bowel obstruction during the time of our follow-up. Meticulous flap closure and reevaluation of the peritoneal flap after this is completed are crucial points to prevent suture dehiscence and subsequent bowel entrapment.
This study’s main limitations relate to its study design, in that it is retrospective in nature, and represents only a single center’s experience. Authors attempt to minimize selection biases which arise from this design with propensity score matching; however, criticism could still be leveled at a concern for generalizability. In the future, we hope to collaborate with other institutions with the aim of representing a multicenter experience reflective of greater diversity. The lack of long-term outcomes, pain, and quality of life assessment, as well as the absence of cost analysis data are other study limitations. Preperitoneal mesh placement allows the use of less costly uncoated meshes [8], which is not examined here, and may provide additional incentive for the adoption of extra-peritoneal placement techniques. Ongoing research is needed in this cohort to provide a comparison of long-term recurrence rates in r-IPOM and r-TAPP procedures.
In conclusion, r-IPOM may be associated with increased complication rates in the early postoperative period when compared to r-TAPP in this matched analysis. Outcomes reported at the 3-month visit, however, are comparable. ED re-visits and surgical-site occurrences were also higher in IPOM patients over this time period. More investigation is needed in this area, specifically with regards to long-term follow-up and multicenter data, to determine the true value of extra-peritoneal mesh placement.
References
Sauerland S, Walgenbach M, Habermalz B, Seiler CM, Miserez M (2011) Laparoscopic versus open surgical techniques for ventral or incisional hernia repair. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.cd007781.pub2
Donkor C, Gonzalez A, Gallas MR, Helbig M, Weinstein C, Rodriguez J (2017) Current perspectives in robotic hernia repair. Robot Surg 4:57–67. https://doi.org/10.2147/RSRR.S101809
Ramshaw BJ, Esartia P, Schwab J, Mason EM, Wilson RA, Duncan TD, Miller J, Lucas GW, Promes J (1999) Comparison of laparoscopic and open ventral herniorrhaphy. Am Surg 65(9):827–831
Bittner R, Bingener-Casey J, Dietz U, Fabian M, Ferzli G, Fortelny R, Kockerling F, Kukleta J, LeBlanc K, Lomanto D, Misra M, Morales-Conde S, Ramshaw B, Reinpold W, Rim S, Rohr M, Schrittwieser R, Simon T, Smietanski M, Stechemesser B, Timoney M, Chowbey P (2014) Guidelines for laparoscopic treatment of ventral and incisional abdominal wall hernias (International Endohernia Society [IEHS])-Part III. Surg Endosc 28(2):380–404. https://doi.org/10.1007/s00464-013-3172-4
Muysoms FE, Miserez M, Berrevoet F, Campanelli G, Champault GG, Chelala E, Dietz UA, Eker HH, El Nakadi I, Hauters P, Hidalgo Pascual M, Hoeferlin A, Klinge U, Montgomery A, Simmermacher RK, Simons MP, Smietanski M, Sommeling C, Tollens T, Vierendeels T, Kingsnorth A (2009) Classification of primary and incisional abdominal wall hernias. Hernia 13(4):407–414. https://doi.org/10.1007/s10029-009-0518-x
Smith MJ (2017) Hernia surgeons embrace sublay repairs, but loyalty to IPOM remains. General surgery news, The independent monthly newspaper for general surgeons. https://www.generalsurgerynews.com/Article/PrintArticle?articleID=39071. Accessed 19 Sep 2018
Orthopoulos G, Kudsi OY (2018) Feasibility of robotic-assisted transabdominal preperitoneal ventral hernia repair. J Laparoendosc Adv Surg Tech A 28(4):434–438. https://doi.org/10.1089/lap.2017.0595
Prasad P, Tantia O, Patle NM, Khanna S, Sen B (2011) Laparoscopic ventral hernia repair: a comparative study of transabdominal preperitoneal versus intraperitoneal onlay mesh repair. J Laparoendosc Adv Surg Tech A 21(6):477–483. https://doi.org/10.1089/lap.2010.0572
Kennedy M, Barrera K, Akelik A, Constable Y, Smith M, Chung P, Sugiyama G (2018) Robotic TAPP Ventral Hernia Repair: Early Lessons Learned at an Inner City Safety Net Hospital. JSLS. https://doi.org/10.4293/jsls.2017.00070
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240(2):205–213
Muysoms FE, Antoniou SA, Bury K, Campanelli G, Conze J, Cuccurullo D, de Beaux AC, Deerenberg EB, East B, Fortelny RH, Gillion JF, Henriksen NA, Israelsson L, Jairam A, Janes A, Jeekel J, Lopez-Cano M, Miserez M, Morales-Conde S, Sanders DL, Simons MP, Smietanski M, Venclauskas L, Berrevoet F, European Hernia S (2015) European Hernia Society guidelines on the closure of abdominal wall incisions. Hernia 19(1):1–24. https://doi.org/10.1007/s10029-014-1342-5
Thoemmes F (2012) Propensity score matching in SPSS, pdf edn. University of Tubingen, Tubingen
LeBlanc KA, Booth WV (1993) Laparoscopic repair of incisional abdominal hernias using expanded polytetrafluoroethylene: preliminary findings. Surg Laparosc Endosc 3(1):39–41
Chelala E, Barake H, Estievenart J, Dessily M, Charara F, Alle JL (2016) Long-term outcomes of 1326 laparoscopic incisional and ventral hernia repair with the routine suturing concept: a single institution experience. Hernia 20(1):101–110. https://doi.org/10.1007/s10029-015-1397-y
Wiessner R, Vorwerk T, Tolla-Jensen C, Gehring A (2017) Continuous laparoscopic closure of the linea alba with barbed sutures combined with laparoscopic mesh implantation (IPOM Plus Repair) as a new technique for treatment of abdominal hernias. Front Surg 4:62. https://doi.org/10.3389/fsurg.2017.00062
Cartes JAM, Morales JM, Grau JMS (2014) Basic concepts in laparoscopic hernia repair. Advances in laparoscopy of the abdominal wall hernia. Springer, New York, pp 37–51
Gonzalez AM, Romero RJ, Seetharamaiah R, Gallas M, Lamoureux J, Rabaza JR (2015) Laparoscopic ventral hernia repair with primary closure versus no primary closure of the defect potential benefits of the robotic technology. Int J Med Robot + Comput Assist Surg 11(2):120–125. https://doi.org/10.1002/rcs.1605
Gonzalez A, Escobar E, Romero R, Walker G, Mejias J, Gallas M, Dickens E, Johnson CJ, Rabaza J, Kudsi OY (2017) Robotic-assisted ventral hernia repair: a multicenter evaluation of clinical outcomes. Surg Endosc 31(3):1342–1349. https://doi.org/10.1007/s00464-016-5118-0
Warren JA, Love M (2018) Incisional hernia repair: minimally invasive approaches. Surg Clin N Am 98(3):537–559. https://doi.org/10.1016/j.suc.2018.01.008
Hilling DE, Koppert LB, Keijzer R, Stassen LP, Oei IH (2009) Laparoscopic correction of umbilical hernias using a transabdominal preperitoneal approach: results of a pilot study. Surg Endosc 23(8):1740–1744. https://doi.org/10.1007/s00464-008-0177-5
Muysoms FE, Bontinck J, Pletinckx P (2011) Complications of mesh devices for intraperitoneal umbilical hernia repair: a word of caution. Hernia 15(4):463–468. https://doi.org/10.1007/s10029-010-0692-x
Yang PG, Tung LK (2016) Preperitoneal onlay mesh repair for ventral abdominal wall and incisional hernia: a novel technique. Asian J Endosc Surg 9(4):344–347. https://doi.org/10.1111/ases.12295
Yang GPC (2017) From intraperitoneal onlay mesh repair to preperitoneal onlay mesh repair. Asian J Endosc Surg 10(2):119–127. https://doi.org/10.1111/ases.12388
Dietz UA, Winkler MS, Hartel RW, Fleischhacker A, Wiegering A, Isbert C, Jurowich C, Heuschmann P, Germer CT (2014) Importance of recurrence rating, morphology, hernial gap size, and risk factors in ventral and incisional hernia classification. Hernia 18(1):19–30. https://doi.org/10.1007/s10029-012-0999-x
Fischer JP, Wink JD, Nelson JA, Kovach SJ 3rd (2014) Among 1706 cases of abdominal wall reconstruction, what factors influence the occurrence of major operative complications? Surgery 155(2):311–319. https://doi.org/10.1016/j.surg.2013.08.014
Bittner R, Bingener-Casey J, Dietz U, Fabian M, Ferzli GS, Fortelny RH, Kockerling F, Kukleta J, LeBlanc K, Lomanto D, Misra MC, Morales-Conde S, Ramshaw B, Reinpold W, Rim S, Rohr M, Schrittwieser R, Simon T, Smietanski M, Stechemesser B, Timoney M, Chowbey P (2014) Guidelines for laparoscopic treatment of ventral and incisional abdominal wall hernias (International Endohernia Society [IEHS])-Part 2. Surg Endosc 28(2):353–379. https://doi.org/10.1007/s00464-013-3171-5
Bittner R, Arregui ME, Bisgaard T, Dudai M, Ferzli GS, Fitzgibbons RJ, Fortelny RH, Klinge U, Kockerling F, Kuhry E, Kukleta J, Lomanto D, Misra MC, Montgomery A, Morales-Conde S, Reinpold W, Rosenberg J, Sauerland S, Schug-Pass C, Singh K, Timoney M, Weyhe D, Chowbey P (2011) Guidelines for laparoscopic (TAPP) and endoscopic (TEP) treatment of inguinal hernia [International Endohernia Society (IEHS)]. Surg Endosc 25(9):2773–2843. https://doi.org/10.1007/s00464-011-1799-6
Acknowledgements
The authors would like to thank Dr. Elif Gokcal for helping us with this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Drs. Gokcal and Morrison have no conflicts of interest or financial ties to disclose. Dr. Kudsi receives teaching course and/or consultancy fees from Intuitive, Bard, Medtronic, Gore, Optecks, Medrobotic, outside the submitted work.
Ethical approval
The Institutional Review Board approved this study.
Human and animal rights
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Gokcal, F., Morrison, S. & Kudsi, O.Y. Short-term comparison between preperitoneal and intraperitoneal onlay mesh placement in robotic ventral hernia repair. Hernia 23, 957–967 (2019). https://doi.org/10.1007/s10029-019-01946-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-019-01946-4