Abstract
Purpose
In Japan, inguinal hernia repair is widely performed with local anesthesia. The objective of this study was to evaluate safety and efficacy of intravenous dexmedetomidine as a sedation agent with local anesthesia in inguinal hernia repair.
Methods
We performed this randomized, single-blind study for 200 patients who were scheduled to undergo inguinal hernia repair with local anesthesia. Patients were randomly divided into two groups (dexmedetomidine group: Group D, midazolam group: Group M). The primary outcome was to evaluate the safety of intravenous dexmedetomidine. Secondary outcomes were to analyze results of operators’ surveys and patients’ questionnaires and evaluate implementation of conscious sedation.
Results
Incidence of respiratory depression was significantly higher in Group M than Group D (p = 0.03). Other adverse events examined did not differ significantly. All three operators’ questionnaires indicated that results were better in Group D than Group M. More than 70% of patients in both groups were satisfied with the surgery. More than 80% of Group D patients and 74% of Group M patients achieved a state of conscious sedation.
Conclusion
This study demonstrated that intravenous dexmedetomidine during hernia repair with local anesthesia is safe and the results were satisfactory to both operators and patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Inguinal hernia is one of the most common conditions encountered in the field of general surgery, and its repair is one of the basic operations performed by surgeons [1]. In Japan, inguinal hernia repair is widely performed with local anesthesia. It is safe, easy to perform, economical with a short hospital stay, and is minimally invasive to organs [2, 3]. However, patients under local anesthesia tend to be anxious and fearful about pain, intraoperative sounds, and smells. To solve this problem, we have performed hernia repair with intravenous midazolam as a conscious sedation agent for patients under local anesthesia.
In 2014, the use of dexmedetomidine for patients under local anesthesia was covered by insurance in Japan. The combination of intravenous dexmedetomidine and local anesthesia is feasible in the implementation of conscious sedation [4, 5]. The ability to communicate with the patient during the operation is an advantage of local anesthesia. For example, by requesting patients to apply abdominal pressure, we can confirm whether the repair is sufficient or not. Conscious sedation with light sleep would not inhibit this advantage [6].
We hypothesized that the combination of intravenous dexmedetomidine and local anesthesia would facilitate inguinal hernia repair. However, there has been no report of an evaluation of the safety and efficacy of dexmedetomidine with local anesthesia during inguinal hernia repair. We designed a randomized controlled trial to compare dexmedetomidine and midazolam with local anesthesia in inguinal hernia repair and to examine the safety and efficacy of intravenous dexmedetomidine as a sedation agent in terms of the incidence of adverse events.
Patients and methods
This randomized, single-blind study of 200 patients was performed in Toyohashi Municipal Hospital during the period from March 2014 to January 2016. The study protocol was approved by the institutional review board (No. 157) and registered at the University Hospital Medical Information Network (UMIN000013468).
Patients
The main inclusion criteria were age 20–85 years, the presence of a single-sided primary inguinal hernia, and undergoing elective surgical repair using the tension-free technique with local anesthesia. Excluded were those with a serious systemic complication, a mental or neurologic disorder affecting the mental state, or a femoral hernia. All patients provided written informed consent to participate in this study prior to surgery. In our department, we always reach a decision to perform surgical operation only after definitely diagnosing inguinal hernia. Therefore, when the diagnosis is difficult to reach, we examine the patients with CT or US. Thus, no patient with unclear diagnosis underwent the surgery in this study but was kept watchful waiting.
Patients were randomly divided into two groups of 100 patients each by the envelope method. Group D received intravenous dexmedetomidine, and Group M received intravenous midazolam. Figure 1 is a flow diagram of the analysis.
Operative procedure
Surgeons performed operations using the Mesh-Plug or Ultrapro Hernia System (UHS) for inguinal hernia repair. In most cases, indirect hernias were repaired by the Mesh-Plug operation, and direct hernias were repaired by UHS; however, selection of the method was left to the discretion of the operator. We describe below a typical operation that we performed for inguinal hernia repair in 8 periods.
Period 1: Enter operating room and begin monitoring.
Period 2: Infusion of dexmedetomidine is started in Group D at a dose of 3 µg/kg/h for 10 min. Intravenous midazolam 2 mg is administered in Group M slowly over a period up to 1 min. Five minutes after the start of drug injection, we perform local anesthesia with surgical site and ilioinguinal nerve block using a mixture of 0.5% lidocaine and 0.75% bupivacaine.
Period 3: Ten minutes after the start of drug injection, the flow rate of dexmedetomidine is changed to 0.4 µg/kg/h in Group D.
Period 4: Operation started.
Period 5: Spermatic cord is separated from inguinal canal. (We always follow this procedure to avoid damage to the cord.)
Period 6: Separation of the hernia sac and insertion of a Plug or UHS.
Period 7: When suturing a Plug or fixing the UHS, we request the patient to apply abdominal pressure.
Period 8: Suturing the fascia of external oblique. In Group D, injection of dexmedetomidine is stopped. Surgery is completed. During the operation, we could change the flow rate of dexmedetomidine, using additional sedation agent or injection of additional local anesthetic depending on the needs of the patients.
Depth of sedation was assessed using the Observer’s Assessment of Alertness/Sedation Scale (OAA/S) (Table 1) during the 8 above-mentioned periods.
The following adverse events were recorded: hypertension, hypotension, bradycardia, respiratory depression, restlessness, etc. During the surgery, the operators and the nurses carefully controlled the vital parameters, though control by the experts was preferable. Mainly, the nurse administered the drugs by the operator’s judgement if needed.
After the operation, we administered a questionnaire to the patients that elicited information about intraoperative memory, pain, anxiety, satisfaction, etc. Operators also completed a questionnaire.
Adverse events
Major adverse events were defined and dealt with as follows.
Respiratory depression was defined as follows: respiratory rate < 8 bpm, 25% decrease from before administration, SpO2 < 90%, decrease by 10% from before administration or oxygen administration was required [7, 8]. Respiratory depression was resolved with oxygen administration, stimulation for awakening or watchful waiting by the operator’s judgement. Hypotension was defined as follows: systolic blood pressure < 80 mmHg, decrease by 30% from before administration or diastolic blood pressure < 50 mmHg. Hypotension was resolved with fluid administration or use of vasopressor (ephedrine or phenylephrine) by the operator’s judgment. Bradycardia was defined as follows: heart rate < 40 bpm or decrease by 30% from before administration. Bradycardia was resolved with decreasing or stopping administration rate of dexmedetomidine or administration of atropine by the operator’s judgement. Hypertension was defined as follows: systolic blood pressure > 180 mmHg, increase by 30% from before administration or diastolic blood pressure > 110 mmHg. Hypertension was resolved with adjusting or stopping administration rate of dexmedetomidine or administration of nicardipine by the operator’s judgement. Delirium was defined as follows: the patient was uncontrollable and needs to be dealt with. Delirium was resolved with physical restraint or by the administration of additional sedatives at the operator’s judgement.
Other adverse events were also resolved by the operator’s judgement as in daily medical practice.
Statistical analysis
When a sedation agent is used in a surgery with local anesthesia, most frequent and most critical adverse event is respiratory depression including apnea, desaturation, and decrease of respiratory rate. Based on our experience, we hypothesized the frequency of respiratory depression of dexmedetomidine and midazolam injection was 40 and 50%, respectively. A sample size of 77 subjects per group was necessary to demonstrate a statistical significance for respiratory depression at α of 0.05 and 1 − β of 0.8 (δ = 0.10). Accordingly, we thought 2 × 100 patients were enough for this study.
Data were analyzed using IBM SPSS Statistic version 21 software (IBM SPSS Inc., Chicago, IL, USA). Student’s t test was used for comparison of the means (age, body weight, operating time, blood loss, dose of local anesthesia). The Chi-square test was used for categorical data (patients’ characteristics, adverse events). Mann–Whitney’s U test was used for the ordinal scale. p value of < 0.05 was considered significant.
Results
During the study period, 200 patients were screened for eligibility, and all 200 patients were randomized either to Group D or Group M. Subsequently, one Group D patient and three Group M patients were excluded from the analysis (Figure 1).
Characteristics of patients
Characteristics of the two groups were comparable (Table 2).
In Group D, repair was undertaken in 71 patients by Mesh-Plug and in 28 patients by the UHS. In Group M, repair was done in 72 patients by Mesh-Plug and in 25 patients by UHS. In Group D, 72 patients had an indirect hernia, 24 patients had a direct hernia and 3 patients had a mixed hernia. In Group M, 75 patients had an indirect hernia, 16 patients had a direct hernia and 6 patients had mixed hernia. The two groups did not differ significantly with regard to operative procedures and the distribution of hernia classifications. Age, sex and body weight also did not differ significantly between the two groups.
In group M, eight patients were administered additional midazolam according to operators’ instructions. In group D, one patient was administered propofol for the conversion into general anesthesia because of the necessity of intraperitoneal procedure.
Adverse events
Adverse events such as respiratory depression, hypertension, hypotension, bradycardia and delirium were recorded (Table 3). The incidence of respiratory depression was significantly higher in Group M than in Group D (p = 0.03). There were no significant between-group differences in the other adverse events examined. Hypotension and bradycardia had a higher incidence in Group D, but without significance.
All adverse events could be safely resolved according to prearranged procedures.
Questionnaires for operators
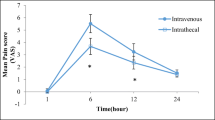
The OAA/S scale was recorded and analyzed (Fig. 2). In the 5 min after and 10 min after the start of drug injection (Periods 2 and 3), the start of surgery (Period 4), the time when we request patients to apply abdominal pressure (Period 7) and the end of the surgery (Period 8), there were the following significant differences between the two groups. Sedation was deeper 5 and 10 min after the start of drug injection and the start of surgery in Group M (p < 0.001). The time to request patients to apply abdominal pressure and the end of the surgery were related to deeper sedation in Group D (p = 0.028). During the surgery, more than 80% of the Group D patients and 74% of Group M patients were in a state of conscious sedation (OAA/S Scale: 3–4) [9].
As for the duration of surgery and dose of local anesthesia, there were no significant differences between the two groups. Blood loss was significantly less in Group D (p = 0.01, Table 2).
There were significant differences in the impression of the patients’ pain, ease of operation and satisfaction with sedation between the two groups (Fig. 3). The results of all three questionnaires were significantly more favorable for Group D (p = 0.02, < 0.01 and < 0.01).
Questionnaires for patients
The results of questionnaires about intraoperative memory, pain, anxiety and satisfaction with the surgery were analyzed, with no significant between-group differences shown (Fig. 4). More than 70% of the patients in both groups were satisfied with the surgery.
Discussion
Our study demonstrated that intravenous dexmedetomidine with local anesthesia could be a comparable sedation agent compared to intravenous midazolam in cases of inguinal hernia repair and resulted in less respiratory depression. Conscious sedation and acceptable satisfaction were achieved with that agent.
Dexmedetomidine has been used in intensive care units as a sedation agent. However, its use in surgery has increased mainly in cases of local anesthesia or spinal anesthesia [7, 8, 10,11,12,13]. Dexmedetomidine, the selective α2 adrenoceptor agonist, is known not only to be a sedative agent but also to have effects of analgesia, bradycardia, hypotension, etc. [4, 5, 14]. Intravenous dexmedetomidine is feasible for the implementation of conscious sedation for patients under local anesthesia.
Midazolam is widely used as a sedative agent during surgery. Intravenous midazolam has features that include rapid onset and rapid recovery [15, 16]. However, midazolam is well known to cause respiratory depression, restlessness and disinhibition [16, 17]. If these adverse events occur intraoperatively, continuation of the surgery may become difficult.
In cases of inguinal hernia repair with local anesthesia, conscious sedation and a little analgesia are considered to be reasonable. Conscious sedation helps ascertain the position of the hernia orifice or success in sufficient repair. The effect of analgesia may relieve intraoperative pain [18, 19]. Intravenous dexmedetomidine could provide ideal sedation with local anesthesia, which is why we designed this randomized controlled trial.
In this trial, several adverse events were recorded. In previous studies, dexmedetomidine was shown to have little ventilator effects [4, 20]. In this study, respiratory depression was recorded in 36% of Group D patients, a rate that might be considered to be slightly high. However, in Group M, respiratory depression was recorded in about half of the patients, which showed a significant difference between the two groups. All patients who had respiratory depression recovered by just watchful waiting, verbal contact or oxygen administration. Especially in Group D, most patients experienced a light sleep; therefore, they rapidly recovered from respiratory depression by calling their name and by the request of deep breathing. Compared with intravenous midazolam, intravenous dexmedetomidine was safer and more acceptable in terms of respiratory depression.
Hypotension (8%) and bradycardia (14%) were recorded in Group D. As we had expected, there was a higher incidence of these cardiovascular events in Group D than in Group M [10], but the difference was not significant. If we had randomized more patients, it may have reached significant. However, all of these adverse events were safely resolved. From these viewpoints, the safety of dexmedetomidine was confirmed.
The OAA/S scale is a reliable and sensitive tool to measure the level of alertness during sedation [9]. We believe that conscious sedation is the best type of intraoperative sedation with local anesthesia. The concomitant use of intravenous dexmedetomidine was reported to be feasible in the implementation of conscious sedation [4, 5]. In fact, in this study, more than 80% of Group D patients were in a state of conscious sedation during the surgery compared with only 72% of Group M patients. The features of midazolam were quicker onset and deeper sedation than that of dexmedetomidine. This study demonstrated that using intravenous dexmedetomidine is superior from the viewpoint of implementation of conscious sedation.
In using an intraoperative sedative, operators’ satisfaction is also important. The results of our questionnaire showed that the operators were highly satisfied with intravenous dexmedetomidine. The operators of Group D patients expressed a high satisfaction level and felt that the operation was easier. About 95% of the operators of Group D patients expressed complete or partial satisfaction with the sedation during surgery in contrast with 79% of those with Group M patients. Patients’ satisfaction is also important. Interestingly, in contrast to operators’ satisfaction, results of the patients’ questionnaires were similar in both groups. Conscious sedation may not necessarily result in patients’ satisfaction. Amnestic effect of midazolam may work on the patients in a positive way [21]. However, more than 70% of the patients in both groups were satisfied with the surgery.
As for the limitation of this study, we could give three points. The first limitation of this study was its single-blinded design. Although the patients were blinded, the operators were not blinded. Different ways of administration made it difficult to be double-blinded, and midazolam and dexmedetomidine had different patterns of the rapidity of the effects. This may affect the operators’ impression and may cause measurement bias in the results of the operators’ questionnaire. The second limitation of this study was single institutional study. For evaluating the safety and feasibility, it is possible that there would be a bias. To attain more reliable results, multi-institutional trails may be necessary. The third was the choice of midazolam for comparison with dexmedetomidine. Propofol is another good sedative with local anesthesia [13, 22]. In our country, however, the use of propofol as a sedative agent is limited to the condition with mechanical ventilation and cannot be covered in patients with local anesthesia by the Japanese national health insurance. In addition, midazolam has been commonly used with local anesthesia. Therefore, we compared dexmedetomidine and midazolam.
We performed a randomized controlled trial to compare dexmedetomidine and midazolam as sedation agents with local anesthesia in inguinal hernia repair. Our analysis demonstrated that intravenous dexmedetomidine is safe to use with local anesthesia and may enhance the operators’ satisfaction by inducing conscious sedation in their patients. This result may be directly applicable to other surgeries with local anesthesia.
In conclusion, the results of this randomized study demonstrate that intravenous dexmedetomidine during hernia repair with local anesthesia is safe and that both operators and patients are satisfied with its use.
References
Huntington CR, Wormer BA, Cox TC, Blair LJ, Lincourt AE, Augenstein VA et al (2015) Local anesthesia in open inguinal hernia repair improves postoperative quality of life compared to general anesthesia: a prospective, international study. Am Surg 81:704–709
Nordin P, Hernell H, Unosson M, Gunnarsson U, Nilsson E (2004) Type of anaesthesia and patient acceptance in groin hernia repair: a multicentre randomised trial. Hernia 8:220–225
Callesen T, Bech K, Kehlet H, The Hvidovre Hospital Hernia Group (1998) The feasibility, safety and cost of infiltration anaesthesia for hernia repair. Anaesthesia 1998(53):31–35
Hall JE, Uhrich TD, Barney JA, Arain SR, Ebert TJ (2000) Sedative, amnestic, and analgesic properties of small-dose dexmedetomidine infusions. Anesth Analg 90:699–705
Aantaa R, Jalonen J (2006) Perioperative use of alpha2-adreno-ceptor agonists and the cardiac patient. Eur J Anesthesiol 23:361–372
American Society of Anesthesiologists Task Force on Sedation, and Analgesia by Non-Anesthesiologists (2002) Practice guidelines for sedation and analgesia by non-anesthesiologists. Anesthesiology 96:1004–1017
Alhashemi JA (2006) Dexmedetomidine vs midazolam for monitored anaesthesia care during cataract surgery. Br J Anaesth 96:722–726
Kaya FN, Yavascaoglu B, Turker G, Yildirim A, Gurbet A, Mogol EB et al (2010) Intravenous dexmedetomidine, but not midazolam, prolongs bupivacaine spinal anesthesia. Can J Anaesth 57:39–45
Chernik DA, Gillings D, Laine H, Hendler J, Silver JM, Davidson AB et al (1990) Validity and reliability of the observer’s assessment of alertness/sedation scale: study with intravenous midazolam. J Clin Psychopharmacol 10:244–251
Cheung CW, Ying CL, Chiu WK, Wong GT, Ng KF, Irwin MG (2007) A comparison of dexmedetomidine and midazolam for sedation in third molar surgery. Anaesthesia 62:1132–1138
Aantaa RE, Kanto JH, Scheinin M, Kallio AM, Scheinin H (1990) Dexmedetomidine premedication for minor gynecologic surgery. Anesth Analg 70:407–413
McCutcheon CA, Orme RM, Scott DA, Davies MJ, McGlade DP (2006) A comparison of dexmedetomidine versus conventional therapy for sedation and hemodynamic control during carotid endarterectomy performed under regional anesthesia. Anesth Analg 102:668–675
Ma XX, Fang XM, Hou TN (2012) Comparison of the effectiveness of dexmedetomidine versus propofol target-controlled infusion for sedation during coblation-assisted upper airway procedure. Chin Med J 125:869–873
Kamibayashi T (2000) Clinical uses of α2-adrenergic agonists. Anesthesiology 93:1345–1349
Aun C, Flynn PJ, Richards J, Major E (1984) A comparison of midazolam and diazepam for intravenous sedation in dentistry. Anesthesia 39:589–593
Mattila MJ, Mattila ME, Olkkola KT, Scheinin H (1991) Effect of dexmedetomidine and midazolam on human performance and mood. Eur J Clin Pharmacol 41:217–223
Robin C, Trieger N (2002) Paradoxical reactions to benzodiazepines in intravenous sedation: a report of 2 cases and review of the literature. Anesth Prog 49:128–132
Gurbet A, Basagan-Mogol E, Turker G, Ugun F, Kaya FN, Ozcan B (2006) Intraoperative infusion of dexmedetomidine reduces perioperative analgesic requirements. Can J Anaesth 53:646–652
Jaakola ML, Salonen M, Lehtinen R, Scheinin H (1991) The analgesic action of dexmedetomidine—a novel alpha 2-adrenoceptor agonist in healthy volunteers. Pain 46:281–285
Belleville JP, Ward DS, Bloor BC, Maze M (1992) Effects of intravenous dexmedetomidine in humans. Anesthesiology 77:1125–1133
Glass PS, Bloom M, Kearse L, Rosow C, Sebel P, Manberg P (1997) Bispectral analysis measures sedation and memory effects of propofol, midazolam, isoflurane, and alfentanil in healthy volunteers. Anesthesiology 86:836–847
White PF, Negus JB (1991) Sedative infusions during local and regional anesthesia: a comparison of midazolam and propofol. J Clin Anesth 3:32–39
Author information
Authors and Affiliations
Contributions
All authors conceived the study concept and study design. TM and TA performed compilation and synthesis of the data. TM and TA carried out statistical analysis. TK, KH, YS, MY, TA and NY supervised the research project. All authors participated in interpretation of the results and writing of the report, and approved the final version.
Corresponding author
Ethics declarations
Conflict of interest
All authors declare no conflict of interest.
Ethical approval
The study was approved by the institutional review board of Toyohashi Municipal Hospital (No. 157).
Human and animal rights
This article does not contain any studies with animals performed by any of the authors.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Mishina, T., Aiba, T., Hiramatsu, K. et al. Comparison between dexmedetomidine and midazolam as a sedation agent with local anesthesia in inguinal hernia repair: randomized controlled trial. Hernia 22, 471–478 (2018). https://doi.org/10.1007/s10029-017-1680-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-017-1680-1