Abstract
Purpose
To compare polypropylene mesh positioned onlay supported by omentum and/or peritoneum versus inlay implantation of polypropylene-based composite mesh in patients with complicated wide-defect ventral hernias.
Methods
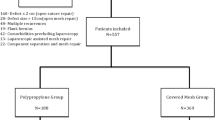
This was a prospective randomized study carried out on 60 patients presenting with complicated large ventral hernia in the period from January 2012 to January 2016 in the department of Gastrointestinal Surgery unit and Surgical Emergency of the Main Alexandria University Hospital, Egypt. Large hernia had an abdominal wall defect that could not be closed. Patients were divided into two groups of 30 patients according to the type of mesh used to deal with the large abdominal wall defect.
Results
The study included 38 women (63.3 %) and 22 men (37.7 %); their mean age was 46.5 years (range, 25–70). Complicated incisional hernia was the commonest presentation (56.7 %).The operative and mesh fixation times were longer in the polypropylene group. Seven wound infections and two recurrences were encountered in the propylene group. Mean follow-up was 28.7 months (2–48 months).
Conclusions
Composite mesh provided, in one session, satisfactory results in patients with complicated large ventral hernia. The procedure is safe and effective in lowering operative time with a trend of low wound complication and recurrence rates.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Large ventral hernias are characterized by substantial deficiency of muscular and fascial tissues leading to severe restriction of the anatomical and physiological capacities of the abdominal wall reducing the respiratory and gastrointestinal functions [1]. Incarceration is the state in which the hernia cannot be reduced back into the abdomen. It is associated with an increased risk of obstruction and strangulation. Incarcerated external hernias are the second most common cause of small intestinal obstructions [2].
Traditionally, incarcerated ventral incisional hernia, whether acute or chronic, has been treated with open surgical techniques. Moreover, some cases with strangulated ventral hernia had been treated by staged surgeries, exposing patients to repeated surgical and anesthetic stresses. Open suture repairs in those critical patients incurred a high incidence of recurrence, ranging from 25 to 52 %. Approximately, 5 % of all patients having an operation for external hernia are explored as an emergency [3].
Recently, the employment of non-absorbable meshes in complicated hernia has been accepted by many studies [4–12]—despite previous surgical obligations—showing comparable incidence of wound complications and recurrence rates. Ideal synthetic graft material should be biologically inert, strong, stable in the presence of infections, non-carcinogenic and non-allergenic, in addition to optimal host tissue integration and optimal accommodation to abdominal wall kinetics [13] this concept extends to mesh placement in acute hernia as well.
Polypropylene (PP) mesh is the most commonly used mesh for hernia repairs. Its advantages include its easy use, elasticity, strength, low rate of rejection, well-formed resistant tissue, and low cost. It can even be used in clean–contaminated and contaminated wounds [14].
Scholarly high-tech breakthrough introduced composite mesh into the medical arena characterized by having double faces. One face, with low visceral adhesion properties, intended to minimize risk of intra-abdominal adhesions and enterocutaneous fistula formation in conjunction with virtues of polypropylene augmented by widening the pores to lighten the weight [15]. However, the use of composite mesh in complicated abdominal hernia has not been studied before due to its recent launch; Proceed® in 2013 and Physiomesh® in 2015.
Repair of an abdominal incisional hernia is a difficult and challenging surgical procedure [16]. The problem becomes more strenuous by the state of complication. In the light of recent publications, the surgeon facing a complicated large defect ventral hernia enters the dilemma of the best way of repair after dealing with contents, whether to put PP mesh, a composite mesh or return to the old dictum of suture repair only.
It is with this background that we have embarked on this study to compare the classical PP mesh positioned onlay supported by underlying omentum and/or peritoneum of hernial sac versus the inlay implantation of polypropylene-based composite mesh in patients with complicated large ventral hernias.
Patients and methods
This was a prospective randomized study carried out on 60 patients presenting with complicated large ventral hernia in a 4-year period from January 2012 to January 2016 in the department of Gastrointestinal Surgery Unit and Surgical Emergency Unit of the Main Alexandria University Hospital, Faculty of Medicine, Alexandria University, Egypt. It is the largest hospital of its kind in Alexandria. It serves the population of Alexandria city and nearby governorates (El-Beheira, Kafr El-Sheikh, and Matrouh) that warrant the accumulation of a sufficient number of cases during a reasonable period of time.
Large hernia was defined by the presence of an abdominal wall defect that could not be suture repaired primarily without tension. Usually a width of 10 cm precluded direct closure. Complications of hernia included irreducibility, intestinal obstruction or strangulation of omentum and/or intestine.
Exclusion criteria encircled those younger than 18 years, uncomplicated ventral hernia, defects that can be closed without tension, poor general function according to the American Association of Anaesthesiology (ASA) score of IV or more and purulent peritonitis due to gangrenous intraperitoneal gut. The study protocol was approved by ethics committee of the Faculty of Medicine, Alexandria University. All patients were informed in advance about the procedure and possible complications and a consent was signed.
All patients were subjected to clinical examination and imaging by ultrasonography with/without computed tomography of the abdomen. Preoperative details included demographic data, co-morbid conditions, type of hernia, complication and previous hernia repair(s) if present. Operative data, defect size and operative time were recorded. Early and late postoperative complications were evaluated.
Patients were randomly divided into two equal groups of 30 patients each, according to the type of mesh used to reinforce the abdominal wall. Group A: the defect was closed by standard polypropylene mesh (Prolene, Ethicon, Summerville, NY, USA) placed over a layer of greater omentum/peritoneum. Group B: the defect was closed by PP-based composite mesh. Two types of composite mesh were used that are available in the Egyptian market: Proceed™ (Ethicon Johnson & Johnson, Somerville, NJ, USA) and Physiomesh™ (Ethicon Endo-Surgery, Johnson & Johnson, Inc., Cincinnati, OH, USA). Proceed is a flexible trilaminar mesh made of an outer layer of polypropylene, inner absorbable oxidized regenerated cellulose layer and polydioxanone layer joining both the outer and inner layers. Physiomesh™ is a lightweight macroporous monofilament mesh composed of a polypropylene mesh coated with a two monocryl (poliglecaprone 25) layers, one to each side of the polypropylene mesh bonded by polydioxanone film.
When the decision to operate is taken, a third-generation Cephalosporin with Metronidazole is given prophylactically to be continued postoperatively for 5 days. Following general anesthesia, skin disinfection and draping, a long incision overlying the sac was performed. We delayed skin excision till the end for adequate coverage. The hernial sac was dissected and defect widened to release the constriction and then the sac opened. Any adhesion between the contents and around hernial ring was lysed (Fig. 1). For incarcerated bowel, release was performed by opening up the defect at its edge without traction on the bowel itself. Viable contents were returned to the abdominal cavity while gangrenous or suspicious parts were resected and small intestinal anastomosis done. The hernial sac was preserved for possible need for closure at the end of the procedure. The tissues are then copiously irrigated with normal saline 0.9 % up to 10 L to wash any residual infection before mesh implantation in addition to change of gloves, packs and drapes.
At this stage, the width of the defect was measured and if larger than 10 cm, the case was considered eligible for the study protocol. The method of repair was chosen randomly by closed envelope technique. Half of cases (group A) were managed by omental and/or peritoneal flap interposition between a polypropylene mesh inserted as onlay mesh on abdominal wall muscle and the intraperitoneal viscera. In this technique, flaps are raised separating the subcutaneous tissue from the anterior rectus sheath, then the opposite ends of the defect are narrowed by interrupted prolene 1 sutures if possible followed by omental mobilization to cover the defect area. If sufficient enough, the omentum is sutured to the edges of the defect by Vicryl 0 interrupted sutures the whole circumference. If insufficient, an extra support was brought by mobilization of the peripheral parietal peritoneum or the use of the hernial sac to complete the shelter prior to prolene mesh placement (Figs. 2, 3).
60-year-old male patient presented with complicated incisional midline hernia with large defect after necessitating resection anastomosis of gangrenous small bowel and dissection of subcutaneous tissue from anterior rectus sheath (a, b). The defect was managed by omentum and/or hernial sac interposition between PP onlay mesh and intra-abdominal viscera (c, d)
The other group of patients (group B) was subjected to composite mesh reinforcement by Proceed or Physiomesh. The size of the mesh should overlap the defect edges by at least 5 cm, usually a 30 × 30 cm size for Proceed and 30 × 35 for Physiomesh was needed. Transfascial prolene 2/0 or 3/0 was used for mesh fixation in both types (Figs. 4, 5).
A closed suction drain (Redivac, 18 Fr) was tucked in the subcutaneous tissue and left till the daily amount was less than 30 ml. The subcutaneous tissue was closed in layers followed by skin staples. Excess unhealthy skin was sacrificed. In the immediate postoperative period, patients were assisted to ambulate early with abdominal binder. Prophylactic doses of low molecular weight heparin were given. Intra-abdominal pressure was measured by a vesical catheter if signs of abdominal hypertension are suspected.
The operative time, postoperative mortality and morbidity, hospital stay were recorded. Seroma was defined as a sterile collection of serous fluid in the operative field after drain removal. Wound infection was identified by a purulent discharge oozing from incision with or without peri-incisional redness/swelling. Follow-up was conducted by repeated clinical examination every week for the first month and then every three months for the first year. Patients were instructed to report at any time if they noticed any swelling or pain at the incision site. For these patients, ultrasonography of abdominal wall is ordered to reveal chronic collections. Chronic pain was described as dull ache related to incision site after 3 months whether requiring the consumption of pain medications or causing discomfort during daily activities. Main outcome measures were postoperative complications and hernia recurrence. Data were presented with numbers, percentage, arithmetic mean and standard deviation (SD) and were analyzed with SPSS (version 15) statistical software. P value <0.005 was significant.
Results
In this review, we enrolled 60 patients with complicated large ventral hernia due to large abdominal wall defect who were treated by mesh repair. The study group included 38 women (63.3 %) and 22 men (37.7 %); their mean age was 46.5 years (range, 25–70). Their Body Mass Index was between 30 and 35 kg/m2 in 14 patients, 35 and 40 in 19, 40 and 45 in 22 and more than 45 in 5 patients. Associated comorbidities were present in 18 patients (30 %). Thirteen patients had ASA score I, 29 had a score of II and 18 patients had a score of III.
Fourteen patients had recurrent hernia; three of them had undergone five or more previous hernia repairs. Complicated incisional hernia was the commonest presentation (33 cases); 19 after midline exploratory incision, 5 after lumbar incision for renal transplantation, 4 after right subcostal incision, 3 after pfannenstiel incision and 2 cases after Rutherford Morrison extension incision. The second common was complicated recurrent hernia observed in 14 cases (23.3 %). Patients of the two groups were homogeneous considering demographics, comorbidities and type of hernia. Both groups were compared and results are tabulated in Table 1.
Maximal defect width was used as crude reference to defect size. In group B, Proceed mesh was applied to 22 patients while Physiomesh was fixed in 8 patients as it was imported from 2015. The operative time was longer in group A and this was statistically significant. To subtract time taken during dissection and adhesiolysis, we measured the actual time taken during mesh fixation as a more accurate indicator for comparison. This time was likewise longer in PP group (group A) and the difference was statistically significant. Gangrenous bowel was found in 12 patients (20 %); 5 in group A and 7 in group B and resection anastomosis was done. Inadvertent enterotomy occurred in four patients and was repaired immediately in two patients; the other two enterotomies were included in resection anastomosis. No case of anastomotic leakage after bowel resection was recorded. Operative findings are summarized in Table 2.
Nine patients suffered from severe postoperative complications, i.e., chest infections, ischemic heart attacks and uncontrolled diabetes, for which the intensive care unit (ICU) admission was necessitated where close ventilatory and cardiovascular monitoring and support required and they discharged from ICU after 1–4 days.
Seven patients presented with wound infections and were successfully treated conservatively in six cases by appropriate antibiotics after obtaining culture and sensitivity and repeated daily dressings. In PP group, mesh removal was needed in a 65-year-old diabetic morbidly obese female patient who had strangulated parastomal hernia (intestinal resection and anastomosis) presented with deep infection extending to the mesh 2 weeks after the operation that necessitated its removal to control the infection and the patient stayed in hospital for 21 days. Seroma affected 22 patients, but was easily managed by repeated evacuation using a large wide-pore syringe and wide-spectrum antibiotic cover (the ultrasound-guided aspiration was needed in 10 cases). Table 3 illustrates demographic data of these patients.
Four patients in PP group and one in composite group developed grade II abdominal compartmental syndrome; all patients were treated conservatively with appropriate fluid therapy under ICU guidance. One patient died in group B after 5 days due to severe myocardial infarction. No case of major haematoma requiring evacuation was found. The mean hospital stay in PP group was 8.1 days, while patient of composite group stayed for a mean of 9 days with no statistically significant difference between two groups.
Follow-up duration ranged from 2 to 48 months with a mean of 28.7 months. The quality of life after surgery was good for all patients, and they were satisfied with the operation; although 10 cases reported abnormal sensation over the mesh site. Two cases in group A developed recurrence; one of them after 3 months and the other after 8 months. The cause of recurrence was attributed to wound infection and postoperative abdominal hypertension in the first case and to large defects reaching to the flanks that a sufficient peripheral overlap was impossible. On follow-up, five cases suffered mild chronic pain not interfering with daily activities; with no statistical difference between both groups. There was no incidence of chronic abdominal wall collection, adhesive intestinal obstruction or enterocutaneous fistula till the time of writing this work. Postoperative and follow-up findings are presented in Table 4.
Discussion
The feasibility and safety of the technique of omental/peritoneal interposition between a propylene mesh and viscera in both elective [17, 18] and emergency [19] situations have been reported demonstrating acceptable wound complication as well as low recurrence rates.
On the other hand, the emergence of different types of composite meshes dedicated to cover electively large abdominal wall defects seems, despite higher costs, a reasonable option. The safety of polypropylene mesh [5, 7–10] and other types [4–6, 8, 11] in complicated hernia has been well established. We hypothesized that PP-based composite mesh could also be used in this situation and we wanted to compare between both available techniques. This was our impetus to start this study. To our knowledge, this is the first randomized comparative trial comparing PP and a composite mesh in complicated large ventral hernias. Both groups were homogenous in terms of demographic data and preoperative conditions.
Many criteria have been proposed to define "large" or "complex" ventral hernia [18, 20]; however, for this study, we selected "defects that cannot be closed by direct sutures" as the first prerequisite for admission to this study. The other prerequisite was the presence of a complication in which, the surgical field is classified as class II or III according to Altemeier classification [20].
Although, by logic, large abdominal hernias should have low risk of complication by virtue of wide defect, this is not true. Adhesions form intraperitoneally between intestinal loops and omentum, causing considerable amalgam of kinked, narrowed bowels raising the possibility of eventual irreducibility, subacute intestinal obstruction and the most dreadful sequelae of ischemia, necrosis and gangrene. Adhesiolysis is an integral part of these surgeries prolonging the operative time and adding extra-risk of bowel injury. We were surprised to find a sufficient number of cases in a relatively short recruitment period. This could be attributed to long history, recurrences, associated diseases and loss of hope in overcoming this problem from the viewpoints of both surgeons and patients.
Complicated wide-defect abdominal ventral hernia presents two major challenges for the general surgeon. The first issue is the complication itself associated with tissue edema, potential infection, bowel resection and toxemia. We excluded patients with free peritonitis as the risk of infection is unbearable and it is unjustified to put any type of mesh in this septic scenario. Added to this is the problem of transmural abdominal wall insufficiency which augments the complexity of management precluding component separation.
An essential question ensues; why propylene material was chosen on behalf of other non-absorbable materials as polyester and polytetrafluoroethylene. The answer is its property of resistance to infection, on account of monofilamentous structure and large pore size allowing accessible infiltration by antibiotics and immune cells [21]. For this reason, both groups received polypropylene material either uncombined (group A) or composite (group B).
We believe that the inlay or onlay positions are the preferred mesh position in complicated cases. Many benefits can be obtained by positioning the mesh intraperitoneally; the operative time is minimized compared to other positions (onlay, retrorectal) as extensive subcutaneous/muscular dissections to raise flaps will not be needed and this has been shown by several publications [1, 22]. The learning curve is shortened and this was demonstrated by less mesh fixation time of the second group from about 60 min in first ten cases to about 35 min in the last ten cases. Consistent with Birolini et al [10] and Paajanen et al [23], retrorectal placement increases the risk of abdominal compartmental syndrome in addition to protraction of operative time.
Complementary to previous studies [5, 10, 12], showing that the application of non-absorbable mesh is safe in the presence of open bowel or colonic resection, our data showed that this role extends also to composite mesh concomitant with dealing with an acute hernia. Among 60 patients, small bowel resection was mandatory in 12 cases (20 %) and 4 inadvertent enterotomies occurred despite careful bowel reduction. Superficial wound infection was observed in 4 of them and was managed conservatively with specific antibiotics and daily dressing. It is reported that 10–15 % of all incarcerated hernias contain gangrenous bowel [24]. Undoubtedly, bowel resection converts wounds to a contaminated class III. A meta-analysis on the risk factors for mesh-related infections after hernia repair surgery found mesh infection rate to be 5 % [25]. In the multivariate analysis reported by Nieuwenhuizen et al [4], bowel resection was the major factor associated with wound infection while type of hernia and preoperative condition had no effect, even though mesh removal was necessary in only one patient after anastomotic leak and peritonitis.
Seroma was slightly more in the PP mesh group (13 versus 9) associated with subcutaneous dissection. In addition, we accord with the opinion of Pascual [26] that additional anti-adhesive layers could serve as a barrier for fluid movement, consequently lowering the risk for seroma formation. Rules to minimize this risk should be obeyed including gentle dissection, minimal use of diathermy, proper haemostasis and extended periods of closed drainage. On the other hand, inlay position helped to reduce dissection and this was attributed to the low incidence of seroma formation in their series because this maneuver creates a potential space in which a seroma can form [17, 18, 27].
Omental/peritoneal interposition was reported as an acceptable cost-effective technique in similar circumstances. Sorour [19] used onlay polypropylene mesh over an intervening layer of omentum or peritoneum in 105 emergency presenting large ventral hernias and found no recurrence and 8.5 % wound infection rate.
The use of composite mesh was useful in overcoming the problem of small size abdominal cavity with minimal increase in intra-abdominal pressure. On the other hand, placement of onlay propylene mesh necessitated the existence of adequate volume of omentum or peritoneum, a prerequisite that was not met all the time subjecting patients to potential postoperative abdominal hypertension. Furthermore, we did not come across any difficulty during closure. Indeed, resection made abdominal closure easier as it helped to reduce viable contents into the shrunken abdominal cavity. We did not face any problem in skin coverage as there was always excess skin. Indeed, composite mesh played an essential role in keeping the integrity of abdominal wall no matter the state of overlying skin, soft tissue or muscles.
The relatively low rate of infectious complications met with this study can be attributed to the administration of strong broad-spectrum antibiotics, sterile precaution before mesh placement, exclusion of those with purulent peritonitis, and resection anastomosis was only carried out in 20 % of cases. On the other hand, 36.6 % developed variable degrees of seroma to whom aspiration was performed for considerable volumes but obtaining a culture is not a routine practice in our department for all cases of postoperative seroma. Those patients were repeatedly followed for clinical and laboratory signs of infection.
The overall recurrence rate observed in the present series was 3.3, 6.6 % of group A and zero in group B after a mean follow-up period of 28.7 months. As emphasized by Sorour [19], adequate overlap of the composite mesh over the hernial defect from inside for at least 5 cm and the use of interrupted transabdominal sutures, in addition to low wound infection rates, may have contributed to the zero recurrence rate observed. It is known that PP mesh can undergo a process of retraction and size reduction up to 30 % (8, 21, 28). Cavallaro et al [28] suggested that a faulty technique and peripheral mesh deficiency were important risks for recurrence. Furthermore, Birolini et al [10] argued that technical errors, not the mesh itself, can cause wound complications as leaving a dead space, incorrect mesh placement and fixation.
Although some patients complained of postoperative pain and foreign body sensation, they declared that they were satisfied with the operation and we assume that pain is a less important aspect in life-threatening states. Risk of enterocutaneous fistula can be considered negligible in both approaches as proved in previous reports [17, 29, 30].
In the contemporary materialistic world, particularly in developing countries like Egypt, the cost is an extremely influential factor in the choice of treatment. Definitely, composite meshes are more costly; however, we believe that financial issues should not be an obstacle in the path of patient’s right to receive the best medical care possible.
Our data revealed superiority of composite mesh over the traditional PP mesh in terms of shorter operative and deployment times, fewer incidences of wound complications and recurrence. A great advantage of both techniques was the ability to treat the emergency condition in one stage as the defect is repaired simultaneously after dealing with the complicated hernia.
This study is not exempt of limitations. The small patient pool may prevent some results from reaching statistical significance level. In addition, the effect of obesity was not understood. We did not have a long-term follow-up as composite meshes are still new to the Egyptian market. Further studies are required to definitively establish the role of different types of composite meshes.
In conclusion, composite mesh deployment provides, in one session, satisfactory results in patients with complicated large abdominal wall hernia. The procedure is safe and effective in lowering operative time with a trend of low wound complication and recurrence rates. Financial resources should be targeted to supply composite mesh in emergency theaters. Interposition of omentum/peritoneum with onlay polypropylene mesh should be the second option if PP-based composite mesh is unavailable. Table 4 compares between both techniques and summarizes the results of this study.
References
Bellon JM, Contreras LA, Sabater C, Bujan J (1997) Pathologic and clinical aspects of repair of large incisional hernias after implant of a polytetrafluoroethylene prosthesis. World J Surg 21(4):402–406 (discussion 6–7)
Bell RR, Seymour NE (2005) Abdominal wall, omentum, mesentery and retroperitoneum. In: Brunicardi FC, Andersen DK, Billiar TR, Dunn DL, Hunter JH, Pollock RE (eds) Schwartz Principles of surgery, 8th edn. McGraw Hill, New York, pp 1317–1328
Watson SD, Saye W, Hollier PA (1993) Combined laparoscopic incarcerated herniorrhaphy and small bowel resection. Surg Laparosc Endosc 3(2):106–108
Nieuwenhuizen J, van Ramshorst GH, ten Brinke JG, de Wit T, van der Harst E, Hop WC et al (2011) The use of mesh in acute hernia: frequency and outcome in 99 cases. Hernia 15(3):297–300
Geisler DJ, Reilly JC, Vaughan SG, Glennon EJ, Kondylis PD (2003) Safety and outcome of use of nonabsorbable mesh for repair of fascial defects in the presence of open bowel. Dis Colon Rectum 46(8):1118–1123
Vix J, Rohr S, Bourtoul Ch (1997) The treatment of incisional and abdominal hernia with a prosthesis in potentially infected tissues—a series of 47 cases. Hernia 1:157–161
Atila K, Guler S, Inal A, Sokmen S, Karademir S, Bora S (2010) Prosthetic repair of acutely incarcerated groin hernias: a prospective clinical observational cohort study. Langenbecks Arch Surg. 395(5):563–568
Shah RH, Sharma A, Khullar R, Soni V, Baijal M, Chowbey PK (2008) Laparoscopic repair of incarcerated ventral abdominal wall hernias. Hernia 12(5):457–463
Antonopoulos IM, Nahas WC, Mazzucchi E, Piovesan AC, Birolini C, Lucon AM (2005) Is polypropylene mesh safe and effective for repairing infected incisional hernia in renal transplant recipients? Urology. 66(4):874–877
Birolini C, Utiyama EM, Rodrigues AJ Jr, Birolini D (2000) Elective colonic operation and prosthetic repair of incisional hernia: does contamination contraindicate abdominal wall prosthesis use? J Am Coll Surg 191(4):366–372
Landau O, Kyzer S (2004) Emergent laparoscopic repair of incarcerated incisional and ventral hernia. Surg Endosc 18(9):1374–1376
Kelly ME, Behrman SW (2002) The safety and efficacy of prosthetic hernia repair in clean-contaminated and contaminated wounds. Am Surg 68(6):524–528 (discussion 8–9)
Morris-Stiff GJ, Hughes LE (1998) The outcomes of nonabsorbable mesh placed within the abdominal cavity: literature review and clinical experience. J Am Coll Surg 186(3):352–367
Finan KR, Kilgore ML, Hawn MT (2009) Open suture versus mesh repair of primary incisional hernias: a cost-utility analysis. Hernia 13(2):173–182
Garcia-Moreno F, Sotomayor S, Perez-Lopez P, Perez-Kohler B, Bayon Y, Pascual G et al (2014) Intraperitoneal behaviour of a new composite mesh (Parietex Composite Ventral Patch) designed for umbilical or epigastric hernia repair. Surg Endosc 28(12):3479–3488
Szczerba SR, Dumanian GA (2003) Definitive surgical treatment of infected or exposed ventral hernia mesh. Ann Surg 237(3):437–441
Mahmoud Uslu HY, Erkek AB, Cakmak A, Sozener U, Soylu L, Turkcapar AG et al (2006) Incisional hernia treatment with polypropylene graft: results of 10 years. Hernia 10(5):380–384
Hasbahceci M, Basak F (2014) Interposition of the hernia sac as a protective layer in repair of giant incisional hernia with polypropylene mesh. Surg Today 44(2):227–232
Sorour MA (2014) Interposition of the omentum and/or the peritoneum in the emergency repair of large ventral hernias with polypropylene mesh. Int J Surg. 12(6):578–586
Slater NJ, Montgomery A, Berrevoet F, Carbonell AM, Chang A, Franklin M et al (2014) Criteria for definition of a complex abdominal wall hernia. Hernia 18(1):7–17
Lukasiewicz A, Drewa T (2014) Synthetic implants in hernia surgery. Adv Clin Exp Med 23(1):135–142
Bernard C, Polliand C, Mutelica L, Champault G (2007) Repair of giant incisional abdominal wall hernias using open intraperitoneal mesh. Hernia 11(4):315–320
Paajanen H, Laine H (2005) Operative treatment of massive ventral hernia using polypropylene mesh: a challenge for surgeon and anesthesiologist. Hernia 9(1):62–67
Brasso K, Londal Nielsen K, Christiansen J (1989) Long-term results of surgery for incarcerated groin hernia. Acta Chir Scand. 155(11–12):583–585
Mavros MN, Athanasiou S, Alexiou VG, Mitsikostas PK, Peppas G, Falagas ME (2011) Risk factors for mesh-related infections after hernia repair surgery: a meta-analysis of cohort studies. World J Surg 35(11):2389–2398
Pascual G, Sotomayor S, Rodriguez M, Bayon Y, Bellon JM (2016) Tissue integration and inflammatory reaction in full-thickness abdominal wall repair using an innovative composite mesh. Hernia 20(4):607–622
Tuveri M, Tuveri A, Nicolo E (2011) Repair of large abdominal incisional hernia by reconstructing the midline and use of an onlay of biological material. Am J Surg 202(1):e7–e11
Cavallaro G, Campanile FC, Rizzello M, Greco F, Iorio O, Iossa A et al (2013) Lightweight polypropylene mesh fixation in laparoscopic incisional hernia repair. Minim Invasive Ther Allied Technol 22(5):283–287
Muysoms FE, Miserez M, Berrevoet F, Campanelli G, Champault GG, Chelala E et al (2009) Classification of primary and incisional abdominal wall hernias. Hernia 13(4):407–414
Poelman MM, Langenhorst BL, Schellekens JF, Schreurs WH (2010) Modified onlay technique for the repair of the more complicated incisional hernias: single-centre evaluation of a large cohort. Hernia 14(4):369–374
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
MK declares no conflict of interest. HE declares no conflict of interest.
Ethical approval
The study protocol was approved by ethics committee of the Faculty of Medicine, Alexandria University.
Informed consent
All patients were informed in advance about the procedure and possible complications and a consent was signed.
Rights and permissions
About this article
Cite this article
Kassem, M.I., El-Haddad, H.M. Polypropylene-based composite mesh versus standard polypropylene mesh in the reconstruction of complicated large abdominal wall hernias: a prospective randomized study. Hernia 20, 691–700 (2016). https://doi.org/10.1007/s10029-016-1526-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-016-1526-2