Abstract
Objective
This study was conducted with the aim to establish standard technique of closed reduction (CR) and compare functional outcomes in patients of moderately displaced unilateral extracapsular condylar fractures.
Material and methods
This study is a retrospective randomized controlled trial, conducted at a tertiary care hospital setting from August, 2013 to November, 2018. Patients of unilateral extracapsular condylar fractures with ramus shortening < 7mm and deviation < 35° were divided in two groups by drawing lots and were treated by dynamic elastic therapy and maxillomandibular fixation (MMF). Mean and standard deviation were calculated for quantitative variables, and one way analysis of variance (ANOVA) and Pearson’s Chi-square test were used to determine significance of outcomes between two modalities of CR. P value < 0.05 was taken as significant.
Results
The numbers of patients treated by dynamic elastic therapy and MMF were 76 (38 in each group). Out of which 48 (63.15%) were male and 28 (36.84%) were female. The ratio of male to female was 1.7:1. The mean ± standard deviation (SD) of age was 32 ± 9.57 years. In patients treated by dynamic elastic therapy, the mean ± SD (at 6-month follow-up) of loss of ramus height (LRH), maximum incisal opening (MIO) and opening deviation were 4.6mm ± 1.08mm, 40.4mm ± 1.57mm and 1.1mm ± 0.87mm respectively. Whereas, LRH, MIO and opening deviation were 4.6mm ± 0.85mm, 40.4mm ± 2.37mm and 0.8mm ± 0.63mm respectively by MMF therapy. One-way ANOVA was statistically insignificant (P value > 0.05) for above mentioned outcomes. Pre-traumatic occlusion was achieved in 89.47% of patients by MMF and in 86.84% patients by dynamic elastic therapy. Pearson’s Chi-square test was statistically insignificant (p value < 0.05) for occlusion.
Conclusion
Parallel results were obtained for both modalities; thus, the technique as dynamic elastic therapy, which promotes early mobilization and functional rehabilitation, can be favored as standard technique of closed reduction for moderately displaced extracapsular condylar fractures. This technique eases patients’ stress associated with MMF and prevents ankylosis.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Mandible is the second most common adult facial bone that fractures in the maxillofacial area, comprising 15.5–59% of all maxillofacial fractures [1]. Mandible can be fractured at the symphysis, para-symphysis, body, angle, ramus, condyle, coronoid and dentoalveolar regions. The fracture of these anatomical sites has been correlated to mechanism of injury by many studies [2]. The thinnest part of the mandible is the condyle. The proportion of condyle fractures accounts for 17.5–52% of all mandible fractures [3]. Fracture of the mandibular condyle is defined as any fracture which is located above the mandibular foramen and runs from within or above the angle of the mandible into the sigmoid notch or the condylar head [4]. Condylar fractures can be extracapsular or intracapsular, undisplaced, deviated, displaced or dislocated [5]. It can occur by direct or indirect trauma, and the displacement of the fracture is determined by direction, degree, magnitude and the precise point of application of the force, as well as state of dentition and occlusal position [6]. The consequences of condyle fractures range from esthetic compromise to functional impairment such as limited mouth opening, facial deformity, TMJ disorders, malocclusion and ankylosis, in turn affecting the physiological and mental health of patient [5]. Thus, the role of timely competent intervention for management of mandibular condyle fractures cannot be negated [7]. The success of intervention will depend on anatomical reduction of fractures, normal range of mandibular motion, occlusion and absence of postoperative pain [8]. The principal treatment modalities for management of condyle fractures are non-surgical and surgical. Nonsurgical options include conservative management (analgesia, soft diet and clinical monitoring) and closed reduction (CR) with rigid or elastic maxillomandibular fixation (MMF). Whereas, surgical management is based on endoscopic or open reduction and internal fixation (ORIF) [9]. This brings us to the ongoing dilemma since decades, about the right choice of treatment for mandibular condyle fractures [10]. Several studies have endorsed CR as first line of management for condyle fractures, considering its non-invasiveness as compared to potential complications of surgical treatment [11], while many surgeons may now consider ORIF as the “golden standard” for both displaced or dislocated condylar head and neck fractures in adults [12]. However, according to AAOMS 2017 the indications for CR and ORIF of mandibular condyle fractures are listed in Table 1 [13]. Also, absolute and relative indications for ORIF by Zide and Kent are given in Table 2 [13].
According to Asim et al., CR should be only restricted to cases with loss of ramus height (LRH) less than 2mm and less than 10° of deviation of mandibular condyle. Whereas, LRH more than 7mm and condylar deviation more than 35° mandate ORIF [14,15,16]. Even with these clarities about treatment of condyle fractures provided by literature, we again reached the point of controversy in situations when moderate category cases present, those with LRH between 2 and 7mm and deviation between 10 and 35° [17].
A systematic review suggests considerable diversity in the protocols of CR with multiple treatment modalities existing in literature for management of mandibular condyle fractures [11]. CR technique for condylar fracture treatment lacks uniform protocols, resulting in heterogenous sequelae. The outcomes of CR technique will be more positive if these standards can be established [18]. Thus, this study aims to assess functional outcomes of moderately displaced unilateral extracapsular mandibular condyle fractures treated by two modalities of closed reduction.
Material and methods
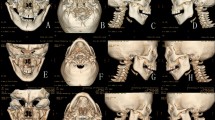
This retrospective randomized controlled trial was conducted at a tertiary care hospital setting from August, 2013 to November, 2018 after permission from institutional review boards of the research and ethics committee (reference no. LMDC/FD/1826/12). Sample size of 76 patients was calculated with 95% confidence level, 1% margin of error and taking magnitude of mean shortening of ramus length 5.75 ± 4.4mm in patients with unilateral mandibular condyle fractures after closed reduction, as post-operative ramus shortening influences all functional and esthetic outcomes of condylar fracture [19]. Written informed consent was taken from all participants of study with information about need for 6-month follow-up. Ascending ramus height was calculated on OPG by using the method described by Palmieri et al. [20]. A horizontal reference line was drawn through both gonial angles, and a tangent to the superior point of the condyle measured along the ramus indicated the height of the ramus. LRH was calculated by subtracting the ramus height on fractured side from non-fractured side. Deviation of condyle on fractured side was calculated by the angulation between the midline axis of the displaced superior fragment and the midline axis of the caudal fragment, assessed on posteroanterior (PA) view of mandible. Vertical and angular measurements on orthopantomogram (OPG) are acceptable provided the patient’s head is positioned properly in the equipment, whereas, horizontal measurements tend to be unreliable because of nonlinear variation in magnification at different object depth [21]. Radiograph was taken by single technician, complying with the regulations and guidelines of clinical trials, including good clinical practice (GCP) guidelines [22, 23].
Inclusion criteria of study was as follows:
-
1.
Patients between age 18 and 50 years of both genders
-
2.
All unilateral, displaced extracapsular condylar fractures with (angle ≤ 35°) on PA view of mandible and ramus shortening ≤ 7mm on OPG.
-
3.
Sufficient dentition to reproduce the occlusal relationships.
-
4.
Patient’s consent to participate.
Exclusion criteria of study was:
-
1.
All patients that conformed to the criteria of Zide and Kent for absolute and relative indications of ORIF.
-
2.
Patients with pre-existing pathological conditions of temporomandibular joints on history and radiographs.
-
3.
Patients in which closed reduction is contraindicated such as mentally unstable or uncooperative patients.
-
4.
Unilateral condylar fractures associated with other facial or mandibular fractures.
-
5.
Unilateral condylar fractures with history of trauma > 2 weeks
All patients excluded from study had surgical treatment.
-
6.
Patients who did not present for 6-month follow-up were excluded from study.
After obtaining informed written consent from participants, demographic data regarding name, age, gender, contact details, followed by history of trauma, time elapsed since fracture and medical history were recorded. Patients were then clinically and radiographically assessed. To ensure randomization, selection of patients for the two treatment modalities was done by opening lots in sealed envelope.
Group A comprised of patients treated by dynamic elastic modality. Erich’s arch bar was secured on maxillary and mandibular arch with 26-gauge stainless steel wire under local anesthesia (2% lignocaine with 1:100,000 epinephrine).
Phase 1: Elastics 6.5-oz 3/16 -inch were placed (Class II ipsilateral to fracture, class I contralaterally) for 2 weeks. Class III elastics were placed on contralateral side to injury in case of severe displacement. Patients were placed on liquid diet.
Phase 2: After 2 weeks, centric occlusion and opening deviation were assessed, and elastics 6.5-oz 1/4 -inch were placed class I bilaterally, in case of no discrepancy. Otherwise, initial orientation of elastics was continued for another week. The orientation of elastics and the number of luges engaged was adjusted based on intercuspation and opening deviation.
Phase 3: From fifth week onward, all patients were advised mouth opening exercises and lateral excursions under guidance of elastics. Duration of treatment was approximately 6 weeks. Post-operatively all patients were advised physiotherapy three times a day for 2–3 months until significant mouth opening was achieved.
Patients allocated in group B were treated by maxillomandibular fixation (MMF). In this technique, Erich’s arch bar was secured on maxillary and mandibular arch in same way as Group A.
Phase 1: MMF was done using 26-gauge stainless steel wire for 2 weeks, and patients were advised liquid diet.
Phase 2: After 2 weeks, 6.5-oz 3/16 -inch elastics were placed in patients (Class II ipsilateral to fracture, class I contralaterally), if no deformity was noted, with continuation of blended liquid diet.
Phase 3: After total treatment time of 4 weeks, supportive elastics were placed in class I orientation bilaterally for 7–10 days. If patients showed any discrepancy in occlusion and opening deviation in these stages, then orientation of elastics in that stage was maintained for another week. This was followed by physiotherapy three times a day for 2–3 months until significant mouth opening was achieved.
Postoperatively, clinical and radiographic evaluation was performed by single observer, who was blinded to groups. Patients were advised OPG and PA view of mandible at 6-month postoperative follow-up. At this appointment, ascending ramus height was calculated on the fractured and non-fractured sides by using trace paper and ruler. Comparison of ramus height was done between two sides of mandible and LRH calculated. Assessment of outcomes of MMF and dynamic elastic modalities was also part of this follow-up appointment. The maximum inter-incisal opening (MIO) was the distance between incisal edges of maxillary and mandibular central incisor teeth on maximal mouth opening, measured by ruler. Estimation of midline discrepancy from facial midline was done to signify deviation of mandible on mouth opening, whereas, post-operative malocclusion was assessed by Singh V and colleagues modified scoring method (i.e. 1: Pre-trauma occlusion. 2: Mild malocclusion that required occlusal adjustment by spot grinding of teeth, 3: Gross malocclusion that required ORIF). Data analysis was performed using Microsoft excel for Mac version 16.56 (2021 Microsoft). Mean and standard deviation were calculated for quantitative variables like age, loss of ramus height (LRH), MIO and deviation of mandible on opening. One-way analysis of variance (ANOVA) was applied to determine which of the two modalities of closed reduction had significant impact on post-operative LRH, MIO and mandibular deviation. Pearson’s Chi-square test was used to explore the association between two techniques and occlusion. P value < 0.05 was considered significant.
Results
The numbers of patients treated for moderately displaced unilateral extracapsular condyle fractures by two different techniques of CR were 76. Out of which 48 (63.15%) were male and 28 (36.84%) were female. The ratio of male to female was 1.7:1. The mean ± standard deviation (SD) of age was 32 ± 9.57 years. The mean and SD of post-operative outcomes at 6-month follow-up are given in Table 3.
One-way ANOVA was applied to determine association between dynamic elastic and MMF techniques of CR with post-operative outcomes. The association of LRH, MIO and mandibular deviation with two techniques of CR was statistically insignificant p value > 0.05 as shown in Tables 4, 5 and 6 respectively. Pearson’s Chi-square test was used to find relation between post-operative occlusion and two treatment techniques. P value was again insignificant.
Discussion
There are many studies in literature comparing anatomical reduction, functional outcomes as well as quality of life after CR and ORIF techniques of mandibular condyle fracture management [8, 9, 12, 24, 25]. Function as defined by dictionary Webster (Merriam-Webster, 1970) is “designed or developed chiefly from the point of view of use.” Thus, functional outcomes are those results which allow a person to participate purposefully in various life activities [26]. The indications for CR and ORIF have been defined by literature, [13] but there still exists a controversial case presentation scenario of unilateral mandibular condyle fractures, with post-trauma LRH between 2 and 7mm and condylar mediolateral deviation between 10 and 35°. This scenario can be characterized as moderately displaced mandibular condyle fracture. In this scenario, both CR and ORIF techniques have been used by surgeons for management of adult mandibular condyle fractures [27]. Rastogi et al. [28] and Danda et al. [29] found that there is no significant difference between the outcomes of CR and ORIF. Rozeboom et al. also reported good outcomes with both techniques in moderately displaced mandibular condyle fractures [30]. Generally, it is always preferred to avoid surgery and its complications; additionally, ORIF is associated with expensive hardware, hospitalization, long general anesthesia time and sick leave costs [30].
There is also variation in literature regarding type of CR technique used [31] like intermaxillary fixation followed by functional follow-up, dynamic elastic therapy or functional treatment [31,32,33]. In developing countries like ours, many people cannot withstand the treatment cost for ORIF. Therefore, this study was conducted to compare two techniques of CR, in order to establish a uniform protocol of CR that provides better functional outcomes.
The mean LRH on fractured side with dynamic elastic therapy and MMF were 4.6mm ± 1.08mm and 4.6mm ± 0.85mm respectively. Kobayashi et al. reported LRH for unilateral condylar fractures treated by MMF and measured on 3D-CT as 4.1mm ± 3.1mm [34] which coincides with results of our study. Contradictory to this study, Eckelt et al. reported 5.75mm ± 4.4 mm [24], and Singh et al. reported 5.68mm ± 2.93mm [35] of LRH with MMF technique. LRH reported by Khiabani et al. [36] (5.30mm ± 0.75mm) with dynamic elastic therapy also differs from our study.
The mean MIO after dynamic elastic therapy was 40.4mm ± 1.57mm and after MMF was 40.4mm ± 2.37mm. These findings depict that adequate MIO was achieved with both techniques, as mouth opening >35mm is considered a successful outcome according to literature [9, 37,38,39,40]. Similar finding was also reported by Eckelt et al. (40.9mm ± 6.7mm) by MMF [24]. Contrary to results of this study, Singh et al. reported MIO at 6 months to be 33.54mm ± 1.89mm [35], and Rozeboom et al. stated 53.3mm ± 7.4mm [30] by MMF. With dynamic elastic therapy, Niezen et al. reported higher post-operative MIO inconsistent to this study as 52.6mm [41], while MIO reported by Khiabani et al. [36] (44mm ± 2.31mm) coincides with the current study.
Deviation on mandibular opening in this study after MMF (0.8mm ± 0.63mm) coheres with Singh et al. (1.18mm ± 1.29mm) [35] and Asim et al. (1.09mm ± 1.60mm) [16]. In contrast, Eckelt et al. reported higher deviation (3.1 mm) [24]. Whereas, mandibular deviation by dynamic elastic therapy in this study was 1.1mm ± 0.87mm, which is close to 0.8 ± 3.61 reported by Khiabani et al. [36].
Pre-traumatic occlusion in this study was achieved in 89.47% of patients by MMF, close to findings of Rozeboom et al. (91.7%) [30], Madadian et al. (90.96%) [9] and Singh et al. (91%) [35]. A systematic review reported that recovery of occlusion is between 76 and 100% by MMF [11]. Whereas, current study reveals that pre-traumatic occlusion after dynamic elastic therapy was observed in 86.84% of patients. In contrast, Niezen et al. reported occlusal discrepancy in 76% of patients by functional therapy [42].
Considering the limitations, a larger sample size with longer follow-up may yield significant outcome. Further comparisons with open reduction and internal fixation technique for treatment of moderately displaced unilateral/bilateral extracapsular condylar fracture can broaden the scope of the study.
Conclusion
The close treatment techniques analyzed in this study are based on limited period of fixation of jaws versus functional treatment. Outcomes of both techniques turned out to be very similar in all parameters compared. Therefore, priority should be given to technique that promotes function, as early mobilization of jaw is recommended, thus warranting functional rehabilitation. Moreover, longer period of fixation is associated with increased risk of ankylosis with intracapsular, extracapsular and displaced fractures [43]. Also, there is a recent shift of trend towards less rigid fixation and more functional techniques.
References
Shah N, Patel S, Sood R, Mansuri Y, Gamit M, Rupawala T (2019) Analysis of mandibular fractures: a 7-year retrospective study. Ann Maxillofac Surg 9(2):349–354. https://doi.org/10.4103/ams.ams_22_19
Afrooz PN, Bykowski MR, James IB, Daniali LN, Clavijo-Alvarez JA (2015) The epidemiology of mandibular fractures in the United States, Part 1: A review of 13,142 cases from the US National Trauma Data Bank. J Oral Maxillofac Surg 73(12):2361–2366. https://doi.org/10.1016/j.joms.2015.04.032
Chang SP, Yang Y, Shi LQ, Liu YW, Liu Y, Ma Q (2018) Modification of the measurement of the major variables in mandibular condylar fractures: angulation of sidewards displacement and shortening of the height of the ramus. Br J Oral Maxillofac Surg 56(2):113–119. https://doi.org/10.1016/j.bjoms.2017.12.003
Neff A, Cornelius C-P, Rasse M, Torre D, Audigé L (2014) The comprehensive AOCMF classification system: condylar process fractures—level 3 tutorial. Craniomaxillofac Trauma Reconstr 7(1_suppl):44–58. https://doi.org/10.1055/s-0034-1389559
Choi K-Y, Yang J-D, Chung H-Y, Cho B-C (2012) Current concepts in the mandibular condyle fracture management Part I: Overview of condylar fracture. Arch Plast Surg 39(04):291–300. https://doi.org/10.5999/aps.2012.39.4.291
Sawazaki R, Lima Júnior SM, Asprino L, Moreira RWF, de Moraes M (2010) Incidence and patterns of mandibular condyle fractures. J Oral Maxillofac Surg 68(6):1252–1259. https://doi.org/10.1016/j.joms.2009.03.064
Fama F et al (2017) Maxillofacial and concomitant serious injuries: an eight-year single center experience. Chin J Traumatol 20(1):4–8. https://doi.org/10.1016/j.cjtee.2016.11.003
Al-Moraissi EA, Ellis E (2015) Surgical treatment of adult mandibular condylar fractures provides better outcomes than closed treatment: a systematic review and meta-analysis. J Oral Maxillofac Surg 73(3):482–493. https://doi.org/10.1016/j.joms.2014.09.027
Madadian MA, Simon S, Messiha A (2020) Changing trends in the management of condylar fractures. Br J Oral Maxillofac Surg 58(9):1145–1150. https://doi.org/10.1016/j.bjoms.2020.07.035
Rozeboom A, Dubois L, Bos R, Spijker R, de Lange J (2017) Open treatment of unilateral mandibular condyle fractures in adults: a systematic review. Int J Oral Maxillofac Surg 46(10):1257–1266. https://doi.org/10.1016/j.ijom.2017.06.018
Rozeboom AVJ, Dubois L, Bos RRM, Spijker R, de Lange J (2017) Closed treatment of unilateral mandibular condyle fractures in adults: a systematic review. Int J Oral Maxillofac Surg 46(4):456–464. https://doi.org/10.1016/j.ijom.2016.11.009
Neff A (2019) Open reduction and internal fixation in temporomandibular joint traumatology: current concepts and future perspectives. SDS 2019. https://doi.org/10.20517/2573-0002.2018.27
Ganesh Sriraam K, Vignesh KRA (2021) Diagnosis and management of mandibular condyle fractures. In: Sridharan G (ed) Oral and maxillofacial surgery. IntechOpen. https://doi.org/10.5772/intechopen.93795
Karan A et al (2019) Condylar fractures: Surgical versus conservative management. Ann Maxillofac Surg 9(1):15. https://doi.org/10.4103/ams.ams_157_17
Merlet F-L et al (2018) Outcomes of functional treatment versus open reduction and internal fixation of condylar mandibular fracture with articular impact: a retrospective study of 83 adults. J Stomatol Oral Maxillofac Surg 119(1):8–15. https://doi.org/10.1016/j.jormas.2017.10.007
Asim MA, Ibrahim MW, Javed MU, Zahra R, Qayyum MU (2019) Functional outcomes of open versus closed treatment of unilateral mandibular condylar fractures. J Ayub Med Coll Abbottabad 31(1):67–71
Vincent AG, Ducic Y, Kellman R (2019) Fractures of the mandibular condyle. Facial Plast Surg 35(06):623–626. https://doi.org/10.1055/s-0039-1700888
Manuel MLB, Prabhu D Complications of unilateral condylar fracture. IJRTI 6(3):49–54 Available: http://www.ijrti.org/papers/IJRTI2103011.pdf
Nitzan DW, Palla S (2017) ‘Closed reduction’ principles can manage diverse conditions of temporomandibular joint vertical height loss: from displaced condylar fractures to idiopathic condylar resorption. J Oral Maxillofac Surg 75(6):1163.e1–1163.e20. https://doi.org/10.1016/j.joms.2017.01.037
Palmieri C, Ellis E III, Throckmorton G (1999) Mandibular motion after closed and open treatment of unilateral mandibular condylar process fractures. J Oral Maxillofac Surg 57:764–776
Yanez-Vico RM, Iglesias-Linares A, Torres-Lagares D, Gutierrez-Perez JL, Solano-Reina E (2010) Diagnostic of craniofacial asymmetry. Literature review. Med Oral:e494–e498. https://doi.org/10.4317/medoral.15.e494
“ICH Expert Working Integrated addendum to ICH E6 (R1): guideline for good clinical practice E6 (R2).” Jun. 11, 2015.
Larheim TA, Svanaes DB, Johannessen S (1984) Reproducibility of radiographs with the orthopantomograph 5: tooth-length assessment. Oral Surg Oral Med Oral Pathol 58(6):736–741. https://doi.org/10.1016/0030-4220(84)90045-8
Eckelt U et al (2006) Open versus closed treatment of fractures of the mandibular condylar process—a prospective randomized multi-centre study. J Craniomaxillofac Surg 34(5):306–314. https://doi.org/10.1016/j.jcms.2006.03.003
Naik K, Lee KC, Torroni A (2020) Does open reduction and internal fixation provide a quality-of-life benefit over traditional closed reduction of mandibular condyle fractures? J Oral Maxillofac Surg 78(11):2018–2026. https://doi.org/10.1016/j.joms.2020.07.014
Frattali C (1998) Assessing functional outcomes: an overview. Semin Speech Lang 19(03):209–221. https://doi.org/10.1055/s-2008-1064045
Han X, Shao X, Lin X, Gui W, Zhang M, Liang L (2020) Open surgery versus closed treatment of unilateral mandibular condyle fractures. J Craniofac Surg 31(2):484–487. https://doi.org/10.1097/SCS.0000000000006080
Rastogi S, Sharma S, Kumar S, Reddy MP, Niranjanaprasad Indra B (2015) Fracture of mandibular condyle—to open or not to open: an attempt to settle the controversy. Oral Surg Oral Med Oral Pathol Oral Radiol 119(6):608–613. https://doi.org/10.1016/j.oooo.2015.01.012
Danda AK, Muthusekhar MR, Narayanan V, Baig MF, Siddareddi A (2010) Open versus closed treatment of unilateral subcondylar and condylar neck fractures: a prospective, randomized clinical study. J Oral Maxillofac Surg 68(6):1238–1241. https://doi.org/10.1016/j.joms.2009.09.042
Rozeboom AVJ et al (2018) Clinical outcomes in the treatment of unilateral condylar fractures: a cross-sectional study. Int J Oral Maxillofac Surg 47(9):1132–1137. https://doi.org/10.1016/j.ijom.2018.05.021
Kamel GN, De Ruiter BJ, Baghdasarian D, Mostafa E, Levin A, Davidson EH (2019) Establishing a protocol for closed treatment of mandibular condyle fractures with dynamic elastic therapy. Plast Reconstr Surg Glob Open 7(12):e2506. https://doi.org/10.1097/GOX.0000000000002506
Lee J-S et al (2014) Anatomical and functional recovery of intracapsular fractures of the mandibular condyle: analysis of 124 cases after closed treatment. Maxillofac Plast Reconstr Surg 36(6):259–265. https://doi.org/10.14402/jkamprs.2014.36.6.259
Vernhet E, De Boutray M, Hoarau R, Jammet P, Galmiche S, Breton I (2019) Exclusive functional treatment for mandibular condylar fractures. J Oral Maxillofac Surg 77(12):2523.e1–2523.e8. https://doi.org/10.1016/j.joms.2019.06.188
Kobayashi T et al (2021) Identification of malocclusion risk factors after closed treatment of condylar fractures using a novel three-dimensional computed tomography approach. J Oral Sci 63(3):283–285. https://doi.org/10.2334/josnusd.20-0600
Singh V, Bhagol A, Goel M, Kumar I, Verma A (2010) Outcomes of open versus closed treatment of mandibular subcondylar fractures: a prospective randomized study. J Oral Maxillofac Surg 68(6):1304–1309. https://doi.org/10.1016/j.joms.2010.01.001
Khiabani K, Zinhaghayegh B, Amirzade-Iranaq MH (2021) Does dynamic intermaxillary fixation with elastics improve outcomes following unilateral condylar fracture? J Oral Maxillofac Surg 79(1):192–199. https://doi.org/10.1016/j.joms.2020.08.040
Nogami S, Yamauchi K, Kataoka Y, Takano H, Yamashita Y, Takahashi T (2014) Clinical comparison between arthrocentesis and conventional conservative treatment with maxillomandibular fixation for unilateral high condylar fractures. J Oral Rehabil 41(2):141–147. https://doi.org/10.1111/joor.12124
Sforza C, Ugolini A, Sozzi D, Galante D, Mapelli A, Bozzetti A (2011) Three-dimensional mandibular motion after closed and open reduction of unilateral mandibular condylar process fractures. J Craniomaxillofac Surg 39(4):249–255. https://doi.org/10.1016/j.jcms.2010.06.005
De Riu G, Gamba U, Anghinoni M, Sesenna E (2001) A comparison of open and closed treatment of condylar fractures: a change in philosophy. Int J Oral Maxillofac Surg 30(5):384–389. https://doi.org/10.1054/ijom.2001.0103
Shen L, Li P, Li J, Long J, Tian W, Tang W (2014) Management of superolateral dislocation of the mandibular condyle: a retrospective study of 10 cases. J Craniomaxillofac Surg 42(1):53–58. https://doi.org/10.1016/j.jcms.2013.02.002
Niezen ET, Stuive I, Post WJ, Bos RRM, Dijkstra PU (2015) Recovery of mouth-opening after closed treatment of a fracture of the mandibular condyle: a longitudinal study. Br J Oral Maxillofac Surg 53(2):170–175. https://doi.org/10.1016/j.bjoms.2014.11.007
Niezen ET, Bos RRM, de Bont LGM, Stegenga B, Dijkstra PU (2010) Complaints related to mandibular function impairment after closed treatment of fractures of the mandibular condyle. Int J Oral Maxillofac Surg 39(7):660–665. https://doi.org/10.1016/j.ijom.2010.03.015
Anyanechi CE (2015) Temporomandibular joint ankylosis caused by condylar fractures: a retrospective analysis of cases at an urban teaching hospital in Nigeria. Int J Oral Maxillofac Surg 44(8):1027–1033. https://doi.org/10.1016/j.ijom.2015.05.003
Author information
Authors and Affiliations
Contributions
All authors contributed to study conception and design. Material preparation and data collection were performed by FAC, FA and TR. Data analysis and first draft of manuscript was written by SM. Critical review was done by AS and NZ. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of Lahore Medical & Dental College (reference no. LMDC/FD/1826/12).
Consent to participate
Written informed consent was obtained from all individual participants included in the study.
Consent for publication
This study does not contain any individual person’s data in any form (including individual details, images or videos).
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sohail, A., Chishti, F.u.d.A., Manzar, S. et al. Can dynamic elastic therapy be established as the standard protocol of closed reduction for moderately displaced extracapsular condylar fractures?. Oral Maxillofac Surg 28, 385–391 (2024). https://doi.org/10.1007/s10006-023-01154-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10006-023-01154-6