Abstract
Background
To evaluate and compare accuracy in position and inclination of a single-tooth implant placement using tooth-supported surgical drill guide (SDG) and surgical drill guide with implant insertion guide (SDIG) in fully digital workflow.
Materials and methods
Thirty partially single edentulous patients were recruited. After randomization, participants were divided into 2 groups equally. The first group underwent implant placement through SDG only, while the second group was subjected to SDIG. All procedure proceeded under a fully digital workflow as the combination of digital scanning from an intraoral scanner, 3D radiographic images from cone-beam computed tomography (CBCT), implant planning software, and a 3D manufacturing machine. A post-operative CBCT was performed to compare the deviations (7 parameters) between planned and actual implant positions.
Results
The mean global deviations at the shoulder and apex were 0.74 ± 0.36 and 1.29 ± 0.61 mm, respectively in the SDG group and 0.48 ± 0.22 mm and 0.71 ± 0.31 mm, respectively in the SDIG group. Likewise, the other parameters in the SDIG group showed fewer deviations than SDG for all measurements. Statistically significant differences were indicated by all parameters except for the horizontal deviation at the implant shoulder (p < .05).
Conclusion
In single-tooth implant placement with a tooth-supported guide using a computer-assisted (static) system with the SDIG could reduce deviations of actual implant position when compared with using SDG only. Besides, guided implant surgery by fully digital workflow is a practical procedure and provides precise implant position regarding the prosthetic-driven concept.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Dental implants are efficient with widespread use these days. They can restore the masticatory function and maintain an aesthetic appearance while also providing predictable outcomes with high long-term success rates [1, 2]. Several factors affect the treatment outcome and two of the most important are implant position and angulation.
Prosthetic planning before implant surgery is now recognized and acknowledged to be a crucial and important aspect of success. Determination of implant location, position, angulation regarding definitive prosthesis provides a better treatment outcome for optimal function, aesthetics, and also implant longevity [3]. Disregarding prosthetic-driven implant concepts often leads to a compromised final prosthesis that can have an adverse effect on long-term implant success with unfavorable biomechanics and poor aesthetics [4,5,6].
Several methods have been developed for placing dental implants. Initially, free-hand placement was used without any guides until surgical drilling templates were invented. Integration of three-dimensional (3D) radiographic images from CBCT has now improved the accuracy of implant surgery compared with traditional techniques [7, 8]. The combination of digital intraoral scanning models, 3D radiographic images from CBCT, implant planning software, and 3D manufacturing machines now offers full digital workflow in computer-assisted implant placement. This technique is increasingly used and will become the norm in the future.
Computer-assisted implant placement can be divided into static and dynamic systems [9]. A static system transfers the planned implant position to the actual sites through intraoral surgical templates, while a dynamic system communicates through optical tracking devices and computer-aided navigation technologies. Operators can alter the drilling angulation and implant position in real time during the surgery. Static template-based guidance is preferred to the dynamic system because of its simplicity, practical usage, friendly cost, and reduced patient’s mouth opening clearance [10]. Static computer-guided systems can be categorized in terms of protocol and type of surgical templates. Some systems use only a surgical drill guide (SDG), whereas others also allow the insertion of implants through a guided template, defined as “surgical drill guide with implant insertion guide” (SDIG) [11].
Fabrication of the digital surgical guide requires computer-aided design and computer-aided manufacturing (CAD/CAM) technology [12,13,14]. Intraoral models and 3D radiographic images are superimposed on each other using 3D implant planning software to simulate the final restoration, to plan the implant position, and to design the surgical template. Then, rapid prototype 3D printing is used to produce the guides and transfer the planned implant position using a prosthetic-driven concept to the actual surgical site through surgical templates.
Digital guided surgery offers several advantages such as optimal and precise implant position harmonizing with definitive restoration [15], a minimally invasive approach, and faster surgery [16, 17]. Digital guided surgery also minimizes operator errors by dentists with limited experience of implant placement [18] and reduces the possibility of damaging the surrounding critical anatomical structures [19]. This technique allows a proper fit with the primary stability of the implant after placement [20].
However, some doubts have been raised concerning the accuracy of computer-guided implant surgery. Accuracy in guided implant surgery is defined as matching the planned implant position in the 3D-planning software with the actual implant position at the surgical site [21]. Comparison between the planned and placed implant positions is often conducted by a pre-operative and post-operative CBCT scan. The accuracy of the implant position is commonly evaluated by three discrepancies in three dimensions as deviation at the entry point, deviation at the apex, and deviation of the implant long axis (angular deviation).
Computer-guided implant surgery has been investigated and improved over the past two decades. A number of studies have assessed the accuracy of computer-guided surgical templates that still show some discrepancies [12, 17, 22,23,24], while others indicated that the clinician can slightly alter the implant position while inserting the implant into the bone [25,26,27]. A discrepancy might occur in this step; therefore, using a digital implant insertion guide after the surgical drill guide may reduce this alteration. Studies of the comparison between computer-assisted implant surgery with and without an implant guide have not provided conclusive results. Some measured discrepancies were based on bone-mucosal-supported guides that provide a less precise measurement than tooth-supported surgical guides [28]. The most recent studies have assessed in cadavers or in vitro models [11, 22, 23] and few have evaluated the accuracy of a fully digital system [29].
The purpose of the study was to evaluate and compare accuracy in position and inclination of a single-tooth implant placement using SDG and SDIG with full digital workflow.
Materials and methods
This randomized clinical trial study was approved by the Human Experimentation Committee, Faculty of Dentistry, Chiang Mai University, and registered in the Thai Clinical Trial Registry (No. TCTR 20,200,128,003). The study conformed to the World Medical Association (WMA) Declaration of Helsinki. All patients gave informed consent prior to participation in the study. The consort 2010 checklist for reporting a randomized trial was also used.
Preparation
Sample size calculation and selection of participants
Participants were recruited at the Centre of Excellence for Dental Implantology, Faculty of Dentistry, Chiang Mai University. The sample size was calculated using the mean and standard deviation (SD) of the global deviation at the implant apex based on the results of our pilot study. The significance level (α) was set at 0.05 and the power of the test (1-β) was set at 80%. Each group was made up of 15 participants with inclusion and exclusion criteria shown in Table 1.
Examination and planning procedure
Firstly, pre-operative cone-beam computed tomography (CBCT) was recorded by DentiiScan© (NECTEC, Bangkok, Thailand). After that, an oral optical scanner (Planmeca Emerald™, Planmeca Co., Ltd., Helsinki, Finland) was used to collect intraoral 3D images. The digital imaging and communications in medicine (DICOM) files from CBCT and the intraoral 3D model were merged through Planmeca Romexis™ software (Planmeca Co., Ltd., Helsinki, Finland). Then, a virtual tooth wax-up and implant position were determined in accordance with the prosthetic-driven concept (Fig. 1) as the “planned implant position.”
Randomization
A subject identification number was given to each participant. A blinded investigator (WE) (who was not involved in the screening, treatment, follow-up, data collection, or analysis) used computer software to randomize the subject identification numbers into two groups equally. The first group underwent implant placement through a surgical drill guide (SDG) only, while the second group was subjected to a surgical drill guide and implant insertion guide (SDIG). This information was placed in sealed envelopes.
Surgical template fabrication
After the implant position was determined, drill guides were designed and fabricated using a 3D printer. All the templates were conducted with tooth-supported guides. The sealed envelopes were opened during this step and if the patient was in the SDIG group, the implant insertion guide was produced additionally.
Surgical procedures and data collection
The static computer-guided surgical system used in this procedure had surgical templates with sleeves of an increasing diameter for both drilling and insertion. In group I, only surgical drill guides were used with insert implant fixture to bone by free-hand technique, whereas in group II both drill guides and implant insertion guide were used for implant loading. The surgical treatments were performed by one of the investigators (PK).
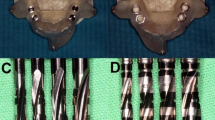
Group I: SDG group (n=15)
All the surgeries were identically operated. The surgery was performed under local anesthesia using 4% articaine with epinephrine 1:100,000. A full-thickness flap was reflected and surgical drill guides were used only for osteotomy preparation. The implant bed was prepared using a round bur, a pilot drill with a diameter of 2.0 mm, and matching twist drills. The implant (NOVEM®, Novem Innovations Co., Ltd., Chiang Mai, Thailand) was inserted into the bone by free-hand manipulation (Fig. 2a). Then, the implant was closed with a cover screw and gingival suturing.
Post-operative CBCT was taken since post-operative DICOM files were used in the analysis procedure.
Group II: SDIG group (n=15)
The protocol was the same as for group I but both the implant osteotomy drilling and implant insertion were performed through the guides (Fig. 2b).
Data analysis and evaluation
Comparison between the planned and placed implant positions was determined in Planmeca Romexis™ software (Planmeca Co., Ltd., Helsinki, Finland) by means of pre- and post-operative CBCT superimposition (Fig. 3). Measurement was performed by an investigator (CN) using Image J software (National Institute of Health (NIH) and the Laboratory for Optical and Computational Instrumentation (LOCI, Wisconsin, USA). Three measurements were used for the evaluation.
Deviation at implant shoulder and apex
Discrepancies were measured for the six parameters shown in Fig. 4 as:
-
Base vertical deviation (mm)
-
Base horizontal deviation (mm)
-
Base global deviation (mm)
-
Apical vertical deviation (mm)
-
Apical horizontal deviation (mm)
-
Apical global deviation (mm)
Deviation parameters between the planned implant position (blue) and placed implant position (yellow): (a) base horizontal deviation (mm); (b) base vertical deviation (mm); (c) base global deviation (mm); (d) apical horizontal deviation (mm); (e) apical vertical deviation (mm); (f) apical global deviation (mm); α, angular deviation (degrees)
Angular deviation
The angle of the long axis between the planned and placed implant positions (degrees) is shown in Fig. 4.
Direction of implant deviation at shoulder and apex
Data and Statistical analysis
After embedding the data with code No.001 to 030, the results were transferred to the investigator for measurement. All data parameters of both groups were evaluated. The Shapiro–Wilk test was used to evaluate normal data distribution. Then, statistical analysis was performed using an independent sample T-test for comparison using SPSS 26 (IBM SPSS, Chicago, IL, USA). Differences at p < 0.05 were considered statistically significant.
Results
Initial enrollment of 47 patients was performed by visual screening. After CBCT scanning, 17 patients were excluded because of insufficient bone width or height. The total number of participants in this study was 30. The patients were recruited after the permission of the ethics committee. After randomization, participants were randomized and divided into the SDG group and SDIG group equally. Each patient received an implant for anterior tooth or premolar replacement between January 31, 2020, and June 30, 2020. The SDG group contained seven males and eight females with a mean age of 43.9 (21–64). Meanwhile, the SDIG group contained eight males and seven females with a mean age of 45.2 (21–65) (Table 2).
Analyses of deviations in each group are presented in Table 3. On average, the SDIG group showed statistically significant less deviations than the SDG for all outcomes. The horizontal deviation on implant shoulder level nevertheless did not reach statistical significance (p < 0.05).
Patterns of dispersion in both groups did not clearly delineate the exact directions of deviation but dispersions in the SDG group were wider and more variable than in the SDIG group in many cases, especially at the implant apex. Mean and SD of global deviation at the implant apex were used to calculate the power of the study using G*Power (Version 3.1.9.4). The result was 0.94 at 0.05 α probability level.
Discussion
This randomized clinical trial for a fully digital workflow aimed to measure and compare the accuracy between two surgical guide systems. Evaluations of discrepancy in computer-aided implant surgery have been conducted for decades, initially using in vitro techniques and then cadavers. Tahmaseb et al. [22] proposed that static measurements should be performed in clinical studies because the lack of cadaver movement and the absence of blood and saliva in models were different from real situations. Therefore, here, a clinical study using a tooth-supported guide surgical template was performed to provide the most precise measurement [23].
The comparison showed that using a drill guide together with an implant insertion guide reduced discrepancies in all measurements. On average, the SDIG group showed less deviations than the SDG for all outcomes. The mean horizontal deviation at implant in the SDIG group (0.64 ± 0.37 mm) was less than in the SDG group (1.17 ± 0.68 mm). On the contrary, the horizontal deviation on implant shoulder level did not reach statistical significance (p < 0.05). Patterns of dispersion in both groups did not clearly delineate the exact directions of deviation but dispersions in the SDG group were wider and more variable than in the SDIG group in many cases, especially at the implant apex. All previous studies concerning the accuracy of static surgical guides found higher horizontal deviation at the implant apex than the shoulder because the metal sleeve required a tolerance space for the drilling bur during osteotomy [30, 31]. Higher horizontal deviation occurred with increased distance of the drilling tip from the sleeve. Van Assche and Quirynen [32] and Koop et al. [31] indicated this as one of the several influencing factors. Another interesting factor was the slope of the alveolar ridge, higher resistance of cortical bone, and bone density at the surgical site [33]. Hence, the implant insertion guide was invented in the hope that it might help to control the implant position and direction during insertion. Results showed that using the implant insertion guide for loading the implant diminished horizontal deviation at the implant apex.
Due to the vertical stop of the implant insertion guide, vertical discrepancies in the SDIG group (0.20 ± 0.13 mm) were less than in the SDG group (0.37 ± 0.27 mm). Statistical analysis showed significant differences in both implant shoulder and apex; however, the mean vertical discrepancy between these two groups was only 0.16 mm. This was explained by the limited drilling length and surrounding reference points as follows. Firstly, even though the drill guide was only used in the SDG group, the depth of implant insertion was limited by the length of drilling burs and their stoppers in osteotomy preparation. Secondly, the cementoenamel junction (CEJ) level of the adjacent teeth or bone level at the surgical site could be used as a reference point for the implant insertion stop [34]. For further evaluation, the box plot in Fig. 5 shows that the apical vertical discrepancy in the SDG group was more variable than in the SDIG group. This implied that the possibility of error could be reduced by using an additional implant insertion guide.
The most discrepancy in all measurements was global deviation. Basically, this value resulted from the combination of vertical and horizontal deviation. Several pieces of literature used global deviation and angular deviation for presenting the accuracy of implant placement. The study of Kuhl et al. [11] analyzed the accuracy of guides, which is similar to our study but performed in cadavers. They also used the angular deviation and global deviation at the implant shoulder and apex to explain their study. They reported mean deviation in each parameter as 4.3 degrees, 1.56 mm and 1.84 mm respectively for the SDG group and 3.6 degrees, 1.52 mm and 1.55 mm for the SDIG group, and concluded that there were no statistical differences between both groups. These three parameters showed fewer deviations in our study, with statistically significant differences between the SDG and SDIG groups. Possible reasons are that their study used a tooth-tissue supported guide and placed multiple implants simultaneously in each cadaver, while different template fabrication procedures were also followed.
The accuracy of computer-assisted static implant placement has greatly improved in accordance with two systematic reviews. Schneider et al. [35] analyzed studies between 2002 and 2009 and summarized that the deviation of computer-assisted (static) systems at the entry point or implant shoulder was 1.07 mm with 1.63 mm at the apex. The mean angular deviation was 5.26 degrees. Tahmaseb et al. [36] analyzed studies conducted from 2011 to 2016. They reported increasing accuracy of this static system over time as 0.9 mm, 1.2 and 3.3 degrees, respectively. Similarly, our study demonstrated that using a static surgical guide in a fully digital system for implant placement provided an acceptable result. Increased accuracy might result from applying the knowledge garnered from numerous previous studies and new surgical guide processing technologies to improve and develop the digital-assisted implant surgical system.
As mentioned before, this study proceeded under a fully digital workflow as the combination of digital scanning from an intraoral scanner, 3D radiographic images from CBCT, implant planning software, and a 3D manufacturing machine [37]. All procedures were performed by digital computer technologies at every step. The digital guide from this study can be used for implants without following conventional procedures of oral impression and model pouring. Digitally guided implant surgery can accumulate errors and deviations from the transformation of data into a guide composed of errors during image acquisition, data processing in software, and surgical template fabrication [21, 38]. Hence, this study also showed the efficiency of a fully digital system that has been continuously replacing the conventional procedure over time.
This study considered only one type of several static guide systems as the tube and drill, while the surgical drill guide and insertion guide were separated. In some systems, these two guides were combined into a single guide and this might provide different results. All implants were placed in the anterior or premolar region due to avoidance of error from limited mouth opening problem. The results of our study indicated the efficiency of a fully digital system for implant placement using a drill guide together with an implant insertion guide. This reduced the possibility of error and provided an acceptable deviation in all directions.
The measurement of the study was a two-dimensional measurement from the computer software which is the limitation of the study. The three-dimensional measurement software is required for future study to verify the accuracy of the SDG and SDIG.
Further studies could investigate the accuracy in more sophisticated procedures such as multiple implant placements, inadequate bone quantity, poor bone quality, immediate implant placement, or flapless surgery. Evaluating the accuracy in these different surgeries as well as using the surgical drill guide with implant insertion guide would be helpful for simple implant placement and also for more varied and complex cases.
Conclusion
Within the limitation of the study, in single-tooth implant placement, it may be concluded that the usage of SDIG reduced deviations of actual implant position when compared with using SDG only. Besides, guided implant surgery by fully digital workflow is a practical procedure and provides precise implant position regarding the prosthetic-driven concept.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- CBCT:
-
Cone-beam computed tomography
- DICOM:
-
Digital imaging and communications in medicine
- SDG:
-
Surgical drill guide
- SDIG:
-
Surgical drill guide with an implant insertion guide
References
Moraschini V, Poubel LA, Ferreira VF, Barboza ES (2015) Evaluation of survival and success rates of dental implants reported in longitudinal studies with a follow-up period of at least 10 years: a systematic review. Int J Oral Maxillofac Surg 44(3):377–388
Howe M-S, Keys W, Richards D (2019) Long-term (10-year) dental implant survival: a systematic review and sensitivity meta-analysis. J Dent 84:9–21
Raikar S, Talukdar P, Kumari S, Panda SK, Oommen VM, Prasad A (2017) Factors affecting the survival rate of dental implants: a retrospective study. J Int Soc Prev Community Dent 7(6):351–355
Widmann G, Bale RJ (2006) Accuracy in computer-aided implant surgery–a review. Int J Oral Maxillofac Implants 21(2):305–313
Kopp KC, Koslow AH, Abdo OS (2003) Predictable implant placement with a diagnostic/surgical template and advanced radiographic imaging. J Prosthet Dent 89(6):611–615
el Askary AS, Meffert RM, Griffin T (1999) Why do dental implants fail? Part I Implant Dent 8(2):173–185
Younes F, Cosyn J, De Bruyckere T, Cleymaet R, Bouckaert E, Eghbali A (2018) A randomized controlled study on the accuracy of free-handed, pilot-drill guided and fully guided implant surgery in partially edentulous patients. J Clin Periodontol 45(6):721–732
Smitkarn P, Subbalekha K, Mattheos N, Pimkhaokham A (2019) The accuracy of single-tooth implants placed using fully digital-guided surgery and freehand implant surgery. J Clin Periodontol 46(9):949–957
Jung RE, Schneider D, Ganeles J, Wismeijer D, Zwahlen M, Hammerle CH et al (2009) Computer technology applications in surgical implant dentistry: a systematic review. Int J Oral Maxillofac Implants 24(Suppl):92–109
Katsoulis J, Pazera P, Mericske-Stern R (2009) Prosthetically driven, computer-guided implant planning for the edentulous maxilla: a model study. Clin Implant Dent Relat Res 11(3):238–245
Kuhl S, Zurcher S, Mahid T, Muller-Gerbl M, Filippi A, Cattin P (2013) Accuracy of full guided vs. half-guided implant surgery. Clin Oral Implants Res 24(7):763–9
Nickenig HJ, Wichmann M, Hamel J, Schlegel KA, Eitner S (2010) Evaluation of the difference in accuracy between implant placement by virtual planning data and surgical guide templates versus the conventional free-hand method - a combined in vivo - in vitro technique using cone-beam CT (Part II). J Craniomaxillofac Surg 38(7):488–493
Van Assche N, van Steenberghe D, Guerrero ME, Hirsch E, Schutyser F, Quirynen M et al (2007) Accuracy of implant placement based on pre-surgical planning of three-dimensional cone-beam images: a pilot study. J Clin Periodontol 34(9):816–821
Orentlicher G, Abboud M (2011) Guided surgery for implant therapy. Oral Maxillofac Surg Clin North Am 23(2):239 56-v–vi
Becker CM, Kaiser DA (2000) Surgical guide for dental implant placement. J Prosthet Dent 83(2):248–251
Wittwer G, Adeyemo WL, Schicho K, Gigovic N, Turhani D, Enislidis G (2006) Computer-guided flapless transmucosal implant placement in the mandible: a new combination of two innovative techniques. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 101(6):718–723
Pettersson A, Komiyama A, Hultin M, Nasstrom K, Klinge B (2012) Accuracy of virtually planned and template guided implant surgery on edentate patients. Clin Implant Dent Relat Res 14(4):527–537
Van de Wiele G, Teughels W, Vercruyssen M, Coucke W, Temmerman A, Quirynen M (2015) The accuracy of guided surgery via mucosa-supported stereolithographic surgical templates in the hands of surgeons with little experience. Clin Oral Implants Res 26(12):1489–1494
Bornstein MM, Al-Nawas B, Kuchler U, Tahmaseb A (2014) Consensus statements and recommended clinical procedures regarding contemporary surgical and radiographic techniques in implant dentistry. Int J Oral Maxillofac Implants 29(Suppl):78–82
van Steenberghe D, Naert I, Andersson M, Brajnovic I, Van Cleynenbreugel J, Suetens P (2002) A custom template and definitive prosthesis allowing immediate implant loading in the maxilla: a clinical report. Int J Oral Maxillofac Implants 17(5):663–670
Vercruyssen M, Hultin M, Van Assche N, Svensson K, Naert I, Quirynen M (2014) Guided surgery: accuracy and efficacy. Periodontol 2000 66(1):228–46
Tahmaseb A, Wismeijer D, Coucke W, Derksen W (2014) Computer technology applications in surgical implant dentistry: a systematic review. Int J Oral Maxillofac Implants 29(Suppl):25–42
Raico Gallardo YN, da Silva-Olivio IRT, Mukai E, Morimoto S, Sesma N, Cordaro L (2017) Accuracy comparison of guided surgery for dental implants according to the tissue of support: a systematic review and meta-analysis. Clin Oral Implants Res 28(5):602–612
Platzer S, Bertha G, Heschl A, Wegscheider WA, Lorenzoni M (2013) Three-dimensional accuracy of guided implant placement: indirect assessment of clinical outcomes. Clin Implant Dent Relat Res 15(5):724–734
Arisan V, Karabuda ZC, Ozdemir T (2010) Accuracy of two stereolithographic guide systems for computer-aided implant placement: a computed tomography-based clinical comparative study. J Periodontol 81(1):43–51
Behneke A, Burwinkel M, Behneke N (2012) Factors influencing transfer accuracy of cone beam CT-derived template-based implant placement. Clin Oral Implants Res 23(4):416–423
Cassetta M, Di Mambro A, Di Giorgio G, Stefanelli LV, Barbato E (2015) The influence of the tolerance between mechanical components on the accuracy of implants inserted with a stereolithographic surgical guide: a retrospective clinical study. Clin Implant Dent Relat Res 17(3):580–588
Ozan O, Turkyilmaz I, Ersoy AE, McGlumphy EA, Rosenstiel SF (2009) Clinical accuracy of 3 different types of computed tomography-derived stereolithographic surgical guides in implant placement. J Oral Maxillofac Surg 67(2):394–401
Derksen W, Wismeijer D, Flügge T, Hassan B, Tahmaseb A (2019) The accuracy of computer-guided implant surgery with tooth-supported, digitally designed drill guides based on CBCT and intraoral scanning. A prospective cohort study 30(10):1005–1015
Van Assche N, Vercruyssen M, Coucke W, Teughels W, Jacobs R, Quirynen M (2012) Accuracy of computer-aided implant placement. Clin Oral Implants Res 23(Suppl 6):112–123
Koop R, Vercruyssen M, Vermeulen K, Quirynen M (2013) Tolerance within the sleeve inserts of different surgical guides for guided implant surgery. Clin Oral Implants Res 24(6):630–634
Van Assche N, van Steenberghe D, Quirynen M, Jacobs R (2010) Accuracy assessment of computer-assisted flapless implant placement in partial edentulism. J Clin Periodontol 37(4):398–403
Ozan O, Orhan K, Turkyilmaz I (2011) Correlation between bone density and angular deviation of implants placed using CT-generated surgical guides. J Craniofac Surg 22(5):1755–1761
Mailoa J, Fu JH, Chan HL, Khoshkam V, Li J, Wang HL (2015) The effect of vertical implant position in relation to adjacent teeth on marginal bone loss in posterior arches: a retrospective study. Int J Oral Maxillofac Implants 30(4):931–936
Schneider D, Marquardt P, Zwahlen M, Jung RE (2009) A systematic review on the accuracy and the clinical outcome of computer-guided template-based implant dentistry. Clin Oral Implants Res 20(Suppl 4):73–86
Tahmaseb A, Wu V, Wismeijer D, Coucke W, Evans C (2018) The accuracy of static computer-aided implant surgery: a systematic review and meta-analysis. Clin Oral Implants Res 29(Suppl 16):416–435
Bencharit S, Staffen A, Yeung M, Whitley D 3rd, Laskin DM, Deeb GR (2018) In vivo tooth-supported implant surgical guides fabricated with desktop stereolithographic printers: fully guided surgery is more accurate than partially guided surgery. J Oral Maxillofac Surg 76(7):1431–1439
Zhou W, Liu Z, Song L, Kuo CL, Shafer DM (2018) Clinical factors affecting the accuracy of guided implant surgery-a systematic review and meta-analysis. J Evid Based Dent Pract 18(1):28–40
Acknowledgements
The authors would like to thank Dr. Walita Narkbuakaew (National Science and Technology Development Agency, Thailand) for introducing the methodological data analysis and measurements. Additionally, sample size calculation and statistical analysis were performed with the support of Dr. Thanapat Sastraruji (Faculty of Dentistry, Chiang Mai University, Chiang Mai, Thailand).
Funding
This study was supported by the fund from the faculty of dentistry, Chiang Mai University.
Author information
Authors and Affiliations
Contributions
C.N. performed a clinical study, analyzed, interpreted the data, and wrote the first draft of the manuscript. W.A. read, corrected, and proved the manuscript. P.K. performed the study design, approved the data analyzed, and finalized the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This randomized clinical trial study was approved by the Human Experimentation Committee, Faculty of Dentistry, Chiang Mai University, and registered in the Thai Clinical Trial Registry (No. TCTR 20200128003).
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Ngamprasertkit, C., Aunmeungthong, W. & Khongkhunthian, P. The implant position accuracy between using only surgical drill guide and surgical drill guide with implant guide in fully digital workflow: a randomized clinical trial. Oral Maxillofac Surg 26, 229–237 (2022). https://doi.org/10.1007/s10006-021-00975-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10006-021-00975-7