Abstract
Purpose
This study aimed to compare the three-dimensional volumetric changes of human maxillary sinuses after reconstruction using 5 different bone grafts.
Patients and methods
Patients underwent unilateral maxillary sinus bone height reconstruction using 5 bone substitutes allocated in different groups as follows: group 1 was grafted with autogenous bone graft alone; group 2 with beta-tricalcium phosphate (β-TCP); group 3 with β-TCP + autogenous bone graft 1:1; group 4 with bioactive glass; and group 5 with bioactive glass + autogenous bone graft 1:1. The patients were submitted to cone beam computed tomography in two periods: 15 days after the surgical procedure (T1) and after 6 months (T2). The results were evaluated as the formula T2-T1 expressing the three-volumetric changes of the biomaterials in elapsed time.
Results
The resorption rate of autogenous bone graft was −630.699 ± 300.9 mm3; in the β-TCP group, it was −315.772 ± 125.6 mm3; in the group with β-TCP + autogenous bone graft 1:1, it was −336.205 ± 195.7 mm3; and in groups with bioactive glass and with the addition of autogenous bone graft 1:1, it was −428.878 ± 311.6 mm3 and −576.917 ± 471.6 mm3, respectively, without statistical difference (p = 0.167). Pearson’s correlated test revealed a strong correlation as well as a progressive resorption of the grafts during bone healing.
Conclusion
The similar outcomes for the three-dimensional volumetric changes using the bone substitutes evaluated after 6 months of bone healing suggest that all these grafts can be performed to maxillary sinus reconstruction.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Oral rehabilitation using dental implants in the posterior maxilla is often limited because of the residual bone height resulting from physiological events such as alveolar process resorption and maxillary sinus pneumatization after dental extractions. To reverse these events, it is necessary to use effective and predictable surgical procedures and conduct research on alternate biomaterials [1].
There is no consensus found in the literature regarding the best bone substitute, although the use of autogenous bone grafting has been highlighted because of its osteogenic, osteoinductive, and osteoconductive properties [2]. However, having a secondary surgical site can cause sequelae such as edema, pain, and neurosensory disturbances [3]. To mitigate these sequelae, several biomaterials, which present suitable alternatives for oral rehabilitation with dental implants, have been studied [4].
Bioactive glass and beta-tricalcium phosphate (β-TCP) are biomaterials that have been widely used in bone reconstruction [5, 6]. Although these bone substitutes are not osteogenic or osteoinductive, several studies have indicate that they yield suitable results for maxillary sinus height reconstruction because of their osteoconductive properties [7,8,9,10].
There is limited literature available regarding the comparison of these biomaterials when used alone or with autogenous bone grafts, particularly for evaluating three-dimensional volumetric changes in the maxillary sinuses using dental implants. Importantly, a dental professional should be able to assess shrinkage of the bone graft(s) after the period of healing. Cone beam computed tomography (CBCT) can provide three-dimensional evaluation with high precision and a low dose of radiation compared with other computed tomography.
This study aimed to compare the three-dimensional volumetric changes of human maxillary sinuses after reconstruction using 5 different biomaterials for posterior dental implant placement.
Material and methods
Human subjects
This study was in accordance with the ethical standards of the institutional and national research committee approved with the number 47711015.4.0000.5420 by Plataforma Brasil/CONEP, with the 1964 Helsinki declaration and its later amendments. Quality assessment was carried out according to the CONSORT Statement’s RCT checklist [11] (Fig. 1).
Number of samples to be evaluated and randomization
The number of maxillary sinuses to be reconstructed for each group was determined using a power test using SPSS version 22.0 (IBM Corporation, Armonk, NY, USA) based on previously published results [12] as follows: a standard deviation of 9.57, an average difference of 11.9%, a significance level of 5%, and 95% power in a one-tailed hypothesis test. A clinical assistant assigned the groups for each graft material to be used via random draw.
Inclusion and exclusion criteria
Each patient underwent CBCT (i-CAT; Image Sciences International, Hatfield, PA, USA) of the maxilla and mandible to identify pathologies and anatomical structures prior to surgery. Patients without uncontrolled systematic disease who decided to undergo rehabilitation for posterior maxillary edentulism with dental implants were included. Patients with residual dental roots in maxillary sinuses, those who had previously received radiation to the head and neck region, those who had uncontrolled periodontal disease, those who were smokers, and those who had paranasal sinuses diseases were excluded. Fifty-eight patients from Araçatuba Dental School ambulatory - UNESP were elected to participate of this research. However, 40 patients with unilateral maxillary sinus bone height deficiency were selected and 18 were excluded.
Groups formation
The following 5 groups were created, with 8 maxillary sinuses in each group:
-
Group 1: 8 maxillary sinuses using autogenous bone grafts (control group)
-
Group 2: 8 maxillary sinuses using only β-TCP (ChronOS; DePuy Synthes, Paoli, CA, USA)
-
Group 3: 8 maxillary sinuses using 1:1 β-TCP + autogenous bone grafts
-
Group 4: 8 maxillary sinuses using only bioactive glass (Biogran®; Biomet 3i, Warsaw, IN, USA)
-
Group 5: 8 maxillary sinuses using 1:1 bioactive glass + autogenous bone grafts
Surgical procedure
All surgical procedures were performed under local anesthesia using lidocaine 2% with adrenaline 1:100,000 (DFL – Jacarépaguá, Rio de Janeiro/Brazil). The autogenous bone grafts were harvested according to the procedure reported by Pereira et al. [3] and milled with a bone crusher (Neodent, Curitiba/Brazil). The maxillary sinus reconstructions were performed using a procedure described by Boyne and James [12]. To reduce pain, 500 mg of paracetamol was prescribed 4 times a day, and 500 mg of amoxicillin was prescribed 3 times a day to reduce the chance of infection.
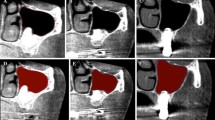
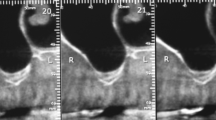
Volumetric analysis
Three weeks after the first surgical procedure, patients underwent CBCT of the face, standardized with 14-bit gray scale and 0.25 mm voxels (T1). The scanner was programmed to use 120 kVp, 5 mA, and 20 s of exposure. DICOM data were reconstructed using OsiriX 4.1.2, 32-bit software (OsiriX Foundation, Geneva, Switzerland); the image orientation was standardized according to the study by Spin-Neto et al. [13]. An additional CBCT was performed on each patient after 6 months of bone healing but prior to the dental implant placement (T2) to determine the volumetric changes using the formula T2-T1. Eighty examinations were performed: 40 for T1 and 40 for T2. The standardization of image orientation, application of contrast and filters, and analysis of volume data acquisition were performed according to the procedure described by Gorla et al. [14]. The T1 and T2 results were calculated and the resorption average was expressed in cubic millimeter. One researcher with previous training performed all evaluations. To demonstrate the relationship between the bone graft volume changes and elapsed time, 30% of the measures were recalculated after 1 month and then evaluated using Pearson’s correlation test.
Statistical analysis
The homoscedasticity of the measures was verified using the Kolmogorov–Smirnov test. The comparison among the groups was performed using analysis of variance (ANOVA) followed by Tukey’s pos hoc test (SPSS version 22.0; IBM Corporation, Armonk, NY, USA). A priori, p < 0.05 was defined as significant.
Results
Forty patients (30 female and 10 male) presenting age ranging from 30 to 63 years old underwent maxillary sinus bone augmentation using the biomaterial purposed.
Volumetric analysis
The resorption rate for autogenous bone graft was −630.699 ± 300.9 mm3 (Table 1); in the β-TCP group, it was −315.772 ± 125.6 mm3 (Table 2); in β-TCP + autogenous bone graft 1:1, it was −336.205 ± 195.7 mm3 (Table 3); and in groups with bioactive glass and its addition with autogenous bone graft 1:1, it was −428.876 ± 311.6 mm3 and −576.917 ± 471.6 mm3, respectively (Tables 4 and 5, respectively). In one sample from the group with bioactive glass added to autogenous bone graft 1:1, bone augmentation (91.680 mm3) was observed. There was no statistical significance among the groups according to the ANOVA test (p = 0.167) (Fig. 2). The Pearson correlated test revealed the following: r = 0.95 for group autogenous bone graft; r = 0.88 for group β-TCP; r = 0.87 for group β-TCP + autogenous bone graft 1:1; and r = 0.81 for groups bioactive glass and bioactive glass + autogenous bone graft 1:1, demonstrating a strong correlation as well as a progressive resorption of the grafts during bone healing.
Discussion
The main concern with oral bone reconstruction is the maintenance of the bone grafts for posterior rehabilitation with dental implants. The dental professional has to understand that the three-dimensional bone volume grafted change over time is physiological. The choice of the ideal biomaterial is important due to the maintenance of a minimum volume which can allow the dental implants placement. With this, the present research could demonstrate that the bone volume changing for the biomaterials evaluated it’s physiological corroborating with previous literature [14, 15].
Many researchers have studied the histological behavior of β-TCP and new bone formation in maxillary sinus bone augmentation [16,17,18,19]. According to Kurcku et al. [20], β-TCP is a rapidly resorbable biomaterial that can aid in bone formation. According to Pereira et al., 47.6% new bone formed in reconstructed maxillary sinuses was in sinuses grafted with β-TCP; similar results have been found by Szabó et al. (38.34%) and Suba et al. (34.7%) [7, 19, 21]. Bioactive glass is an osteoconductive bone substitute with a different type of resorption. Previous literature has described chemical dissolution in addition to particle breakage, which creates a suitable environment for bone formation [22]. The literature reports that 35.6 to 45.6% of bone formation occurs after maxillary sinus reconstruction using bioactive glass [8, 23]. The present study demonstrates that despite the bone graft resorption, the literature confirms suitable histological results for the biomaterials evaluated, making it possible to receive dental implants.
he use of autogenous bone grafts combined with others biomaterials has been defended in literature because of the addition of pluripotential cells as osteoblasts and mesenchymal cells [4] [7, 24]. When a 1:1 β-TCP + autogenous bone graft was used to reconstruct maxillary sinuses, 25.4% of new bone formed was found; however, the tridimensional volumetric changes compared to those noted with the use of autogenous bone grafts alone were similar [15]. The use of 1:1 bioactive glass + autogenous bone grafts yielded better results than those reported in the literature as reported by Menezes et al. [25]. They demonstrated 45.8% bone formation in human maxillary sinuses and an average of 37.9% of bone volume change. The present study shows that the combination of either bone substitute with autogenous bone grafts in a 1:1 proportion have suitable results compared to autogenous bone grafts alone. Further, the physiological resorption in groups with the mixture of autogenous bone graft 1:1 corroborated with that described in previous literature.
The literature reports the use of non-resorbable biomaterials in order to avoid the resorption as well as repneumatization [26, 27]. Nkenke and Stelzle [28] showed that the bone graft resorption does not influence on dental implant survival using autogenous bone graft or bone substitutes. In the present study, the resorption rates for the bone grafts tested presented similar outcomes with the autogenous bone graft. Thus, the use of mixing bone grafts has its use reduced for specific cases as the necessity to increase the amount of bone graft or, in cases with few maxillary sinus bone floor remaining due to the decrease of pluripotent cells, supply for the bone substitute healing.
As limitations for this research, only bone volume changing was studied in the present research. Thus, future studies in order to determine the dental implants survivor placed in these bone grafts can answer the success rate in a long-time period.
Conclusion
The similar outcomes for the three-dimensional volumetric changes using the bone substitutes evaluated after 6 months of bone healing suggest that all these grafts can be performed to maxillary sinus reconstruction. However, the present research evaluated only bone graft resorption being required further researches to answer the biological behavior of the 5 bone substitutes studied.
References
Wallace SS, Froum SJ (2003) Effect of maxillary sinus augmentation on the survival of endosseous dental implants. A systematic review. Ann Periodontol 8:328–343
Schlegel KA, Fichtner G, Schultze-Mosgau S, Wiltfang J (2003) Histologic findings in sinus augmentation with autogenous bone chips versus a bovine bone substitute. Int J Oral Maxillofac Implants 18:53–58
Pereira RS, Pavelski MD, Griza GL, Boos F, Hochuli-Vieira E (2019) Prospective evaluation of morbidity in patients who underwent autogenous bone-graft harvesting from the mandibular symphysis and retromolar regions. Clin Implant Dent Related Res 21:753–757
Rickert D, Slater JJRH, Meijer HJA, Vissink A, Raghoebar GM (2012) Maxillary sinus lift with solely autogenous bone compared to a combination of autogenous bone and growth factors or (solely) bone substitutes. A systematic review. Int J Oral Maxillofac Surg 41:160–167
Stiller M, Rack A, Zabler S, Goebbels J, Dalugge O, Jonscher S et al (2009) Quantification of bone tissue regeneration employing beta-tricalcium phosphate by three-dimensional non-invasive synchrotron micro-tomography - a comparative examination with histomorphometry. Bone 44:619–628
Cordioli G, Mazzocco C, Schepers E, Brugnolo E, Majzoub Z (2001) Maxillary sinus floor augmentation using bioactive glass granules and autogenous bone with simultaneous implant placement - clinical and histological findings. Clin Oral Implants Res 12:270–278
Szabo G, Huys L, Coulthard P, Maiorana C, Garagiola U, Barabas J et al (2005) A prospective multicenter randomized clinical trial of autogenous bone versus beta-tricalcium phosphate graft alone for bilateral sinus elevation: histologic and histomorphometric evaluation. Int J Oral Maxillofac Implants 20:371–381
Tadjoedin ES, de Lange GL, Lyaruu DM, Kuiper L, Burger EH (2002) High concentrations of bioactive glass material (BioGran) vs. autogenous bone for sinus floor elevation. Clin Oral Implants Res 13:428–436
Turunen T, Peltola J, Yli-Urpo A, Happonen RP (2004) Bioactive glass granules as a bone adjunctive material in maxillary sinus floor augmentation. Clin Oral Implants Res 15:135–141
Schulze-Spate U, Dietrich T, Kayal R, H H, J D, Z S et al (2012) Analysis of bone formation after sinus augmentation using beta-tricalcium phosphate. Compend Contin Educ Dent:5
Schulz KF, Altman DG, Moher D, Group C (2010) CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. BMJ 340:c332
Boyne PJ, James RA (1980) Grafting of the maxillary sinus floor with autogenous marrow and bone. J Oral Surg 38:613–616
Spin-Neto R, Stavropoulos A, Pereira LAVD, Marcantonio E, Wenzel A (2013) Fate of autologous and fresh-frozen allogeneic block bone grafts used for ridge augmentation. A CBCT-based analysis. Clin Oral Implants Res 24:167–173
Gorla LF, Spin-Neto R, Boos FB, Pereira Rdos S, Garcia-Junior IR, Hochuli-Vieira E. Use of autogenous bone and beta-tricalcium phosphate in maxillary sinus lifting: a prospective, randomized, volumetric computed tomography study.
Dos Santos PR, Boos FB, Gorla LF, Garcia IR Jr, Okamoto R, Hochuli-Vieira E (2016) Maxillary sinus elevation surgery with ChronOS and autogenous bone graft: analysis of histometric and volumetric changes. Int J Periodontics Restorative Dent 36:885–892
Dos Santos PR, Boos FB, Gorla LF, Garcia IR Jr, Okamoto R, Hochuli-Vieira E (2017) Maxillary sinus elevation surgery with ChronOS and autogenous bone graft: immunohistochemical assessment of RUNX2, VEGF, TRAP, and osteocalcin. Int J Periodont Restorative Dent 37:e321–e327
Knabe C, Koch C, Rack A, Stiller M (2008) Effect of beta-tricalcium phosphate particles with varying porosity on osteogenesis after sinus floor augmentation in humans. Biomaterials 29:2249–2258
Martinez AFJ, Saiz E, Guitian F (2010) Maxillarysinus floor augmentation on humans: packing simulations and 8 months histomorphometric comparative study of anorganic bone matrix and beta-tricalcium phosphate particles as grafting materials. Mater Sci Eng C Mater Biol Appl 30:763–769
Pereira RS, Gorla LF, Boos F, Okamoto R, Garcia Junior IR, Hochuli-Vieira E (2017) Use of autogenous bone and beta-tricalcium phosphate in maxillary sinus lifting: histomorphometric study and immunohistochemical assessment of RUNX2 and VEGF. Int J Oral Maxillofac Surg 46:503–510
Kurkcu M, Benlidayi ME, Cam B, Sertdemir Y. Anorganic bovine-derived hydroxyapatite vs beta-tricalcium phosphate in sinus augmentation: a comparative histomorphometric study. J Oral Implantol 2012;38 Spec No:519-526.
Suba Z, Takacs D, Matusovits D, Barabas J, Fazekas A, Szabo G (2006) Maxillary sinus floor grafting with beta-tricalcium phosphate in humans: density and microarchitecture of the newly formed bone. Clin Oral Implants Res 17:102–108
Veis AADN, Parisis NA, Tsirlis AT, Karanikola TG, Printza DV (2006) Bone regeneration around implants using spherical and granular forms of bioactive glass particles. Implant Dent 15:386–394
Pereira RD, Menezes JD, Bonardi JP, Griza GL, Okamoto R, Hochuli-Vieira E (2017) Histomorphometric and immunohistochemical assessment of RUNX2 and VEGF of Biogran (TM) and autogenous bone graft in human maxillary sinus bone augmentation: a prospective and randomized study. Clin Implant Dent Relat Res 19:867–875
Cosso MG, de Brito RB, Jr., Piattelli A, Shibli JA, Zenobio EG. (2014) Volumetric dimensional changes of autogenous bone and the mixture of hydroxyapatite and autogenous bone graft in humans maxillary sinus augmentation. A multislice tomographic study. Clin Oral Implants Res 25:1251–1256
Menezes JD, Pereira RDS, Bonardi JP, Griza GL, Okamoto R, Hochuli-Vieira E (2018) Bioactive glass added to autogenous bone graft in maxillary sinus augmentation: a prospective histomorphometric, immunohistochemical, and bone graft resorption assessment. J Appl Oral Sci 26:e20170296
Hallman M, Nordin T (2004) Sinus floor augmentation with bovine hydroxyapatite mixed with fibrin glue and later placement of nonsubmerged implants: a retrospective study in 50 patients. Int J Oral Maxillofac Implants 19:222–227
Kim YK, Yun PY, Kim SG, Kim BS, Ong JL (2009) Evaluation of sinus bone resorption and marginal bone loss after sinus bone grafting and implant placement. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 107:e21–e28
Nkenke E, Stelzle F Clinical outcomes of sinus floor augmentation for implant placement using autogenous bone or bone substitutes: a systematic review. Clin Implant Dent Relat Res 20:124–133
Funding
Scholarship grant PICPq 2020/21 and FAPESP (Programa Jovens Talentos 2020) E-26/201/739/2020.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
The present study was in accordance with ethical standard of the institutional human research committee of the Universidade Estadual Paulista UNESP – Faculdade de Odontologia de Araçatuba with number 47711015.4.0000.5420 and with the Helsinki declaration of 1964 and its later amendments or comparable ethical standards.
Conflicts of interest
The authors declare no conflict of interest.
Informed consent
Informed consent was obtained from all participants of the present study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
(DOC 218 kb)
Rights and permissions
About this article
Cite this article
Menezes, J.D., Pereira, R.d., Santos, A.M.d. et al. Three-dimensional volumetric changes of 5 different bone grafts in human maxillary sinuses reconstruction: a randomized clinical study. Oral Maxillofac Surg 25, 541–547 (2021). https://doi.org/10.1007/s10006-021-00940-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10006-021-00940-4