Abstract
Purpose
The accuracy of fully digital model–free surgical and prosthetic procedures depends on the cumulative effect and interaction of all errors gathered along the entire workflow process. In the present case series, a technique is described that increases the accuracy in the transition from the surgical to the prosthetic phase to reduce the risk of developing prosthetic complications in the case of immediate loading protocols.
Methods
Overall, 86 dental implants were placed and immediately loaded with definitive prostheses in 11 edentulous patients following computer-guided implant surgery according to a fully digital model–free workflow. The same reference template used to anchor the surgical stent during computer-aided implant placement was used to guide the insertion of the definitive abutments and to seat in the correct position the final screw-retained implant-supported fixed restoration. The template used during all surgical and prosthetic procedures, which served as a stable and reproducible connection between the digital and surgical environments, was finally removed.
Results
Healing proceeded uneventfully in all subjects. The implant survival and success rates were 100% over a minimum follow-up period of 1 year from the prosthetic loading. No biological or prosthetic complications were clinically and radiographically observed up to the last follow-up recall.
Conclusion
The use of a reference template used to transfer the digital project to the surgical field increased the accuracy and the integration of the surgical and prosthetic phases during the entire workflow.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
A prolonged average life expectancy increases the likelihood of treating patients with terminal dentition. This condition is characterized by chronic periodontal disease, unstable teeth, poor occlusal relationships, unfavourable alveolar anatomy, among others. This generalized impairment, together with a lack of stable anatomical references, makes the implant rehabilitation of this clinical condition extremely difficult.
This is particularly true in the case of a computer-guided approach, where the absence of fixed landmarks complicates the digital workflow [1, 2]. Indeed, it is generally accepted that guided surgeries are more accurate in partially edentulous patients than in fully edentulous patients, and tooth-supported guides are considered more accurate with respect to mucosa- and bone-supported templates used in fully edentulous patients [3]. Furthermore, the digital scan of edentulous arches still represents a challenge. This is explained by the difficulties in acquiring mobile soft tissues and scanning smooth-surface textures covered entirely by saliva, together with a lack of reference landmarks in edentulous jaws [4]. Finally, osteoplasty procedures performed to shape the bone architecture and normalize the vertical dimension prior to implant insertion may further contribute to losing the remaining reference points [5].
All of these factors negatively influence the accuracy of the entire workflow, which is crucial for successful implant-supported rehabilitation [6]. Deviations from the virtual project reflect the sum of all errors occurring from digital scanning and radiographic acquisitions to the transformation of the project into a surgical stent and to the improper positioning of this stent during surgery. Thus, the accuracy of computer-guided surgery depends on the cumulative effect and interaction of all errors gathered along the entire workflow process.
An inaccurate implant placement may have a detrimental impact on the prosthetic outcome of the temporary prosthesis fabricated on the basis of the virtual plan before surgery. In fact, incidences of 18.8% and 12% have been reported for early and late prosthetic complications, respectively. Such impacts occur especially when stereolithographic-guided surgery is followed by immediate provisionalization with a previously prepared fixed bridge [7]. Prosthesis fracture, screw loosening, misfit at the time of superstructure connection, and the need for extensive occlusal adjustments after placement of the superstructures have been the most commonly reported postsurgical complications [8]. Thus, prefabrication of the prosthetic restoration and correct fixation to the implants cannot be assumed to be a flawless procedure.
In this sense, difficulties in stabilizing the temporary prosthesis in the proper position during relining procedures in immediate loading protocols may play an important role in the occurrence of prosthetic complications. The critical component is the transition from the removal of the surgical guide to the fixation of the temporary prosthesis after complete loss of all reference points. To obtain the highest level of accuracy in relocating the denture on the implants, the same bone pins used during the surgical phase to anchor the guide can be employed to stabilize the prosthesis in the proper position during subsequent prosthetic procedures. This is achieved by transferring the same three-dimensional position and angulation of the guiding sleeves used to anchor the surgical stent to the temporary prosthesis by means of provisory acrylic resin guides. In this way, the position of the temporary prosthesis should be the same as that of the surgical guide. Hypothetically, this method allows the operator to constantly reproduce the transfer of data related to the fixed temporary prosthesis with the same means used for the surgical template so that the prosthesis is accurately located with respect to the implants according to the preexisting reference points [9]. However, once the surgical stent is removed, the repositioning of the bone pins in the same holes may be difficult to achieve. This is primarily explained by the fact that since errors are cumulative and interactive, each additional step that is added to the procedure may potentially increase the inaccuracy of the workflow. Other factors that might complicate the repositioning of anchor pins include bone resilience and resistance, shrinkage of the mucosa, scarce visibility due to bleeding and the bulkiness of the prosthesis, and potential interferences with implant components.
Given that all steps of the protocol have to be carefully managed to minimize inaccuracy, this report aims to present an alternative solution to increase the accuracy in the transition from the surgical to the prosthetic phase to reduce the risk of developing prosthetic complications in the case of immediate loading protocols.
Technique description
The present technique consists of an improvement to a previously reported methodology [9] based on computer-guided template-aided flapless implant placement and immediate loading protocols [6].
In brief, partially edentulous patients were enrolled if presenting with terminal dentition characterized by hopeless remaining teeth and/or implants (Fig. 1) clinically and radiographically evaluated by means of recent orthopantomographs when provided by the subject and performed within 6 months of the first appointment (Fig. 2) or directly with cone-beam computed tomography (CBCT) scanning. Additional inclusion criteria included the presence of at least 3 mm of keratinized mucosa circumferentially around the surgical site in the apico-coronal dimension and the presence of an adequate amount of bone assessed as a minimum of 1 mm buccally and palatally/lingually with respect to the planned implant diameter to avoid bone augmentation procedures. Patients with local and/or systemic diseases or conditions representing absolute contraindications to oral surgery procedures and patients with smoking habits (> 10 cigarettes/day) were excluded from the study. Patients unable to open the mouth sufficiently to accommodate the surgical tooling (at least 50 mm) were considered ineligible to participate in the study for technical reasons.
All surgical and prosthetic procedures were performed by the same operators in a private practice setting to reduce the risk of bias in the procedure. Only a limited number of patients were initially enrolled before extending the protocol to a larger number of cases. Informed consent was obtained from all individual participants included in the study before the commencement of the rehabilitation. All procedures were conducted according to the principles outlined by the Declaration of Helsinki of the World Medical Association as a statement of ethical principles for medical research involving human subjects, as revised, amended, and clarified in its 2013 version.
Pre-surgical procedures
During the first appointment, medical history and clinical and radiological evaluations were recorded to verify the eligibility of each subject. To assess the residual bone anatomy, a CBCT scan was performed according to the manufacturer’s instructions (Orthophos® SL 3D, Dentsply Sirona, Charlotte, NC, USA) with a proper field-of-view size to include both the upper and lower jaw. In the same session, enrolled patients underwent digital impression of both arches with an intraoral scanner (CEREC Omnicam, Dentsply Sirona, Charlotte, NC, USA) to record the baseline virtual occlusion registration and the occlusal vertical dimension. At this point, CBCT data in DICOM (Digital Imaging and COmmunication in Medicine) format were superimposed with STL (standard triangulation language) files obtained with the intraoral digital scan using a specific algorithm integrated in the planning software (coDiagnostiX®, Dental Wings Inc., Montreal, QC, Canada) based on the best-fit adaptation of the STL tooth anatomy and the DICOM volume of the tooth structures (Fig. 3). Finally, it was possible to virtually plan the size and position of the implants according to a prosthetically driven implant placement on the basis of a virtual wax-up representing the ideal replica of the temporary prosthesis. Conically shaped 5-degree prefabricated abutments (Ankylos® SynCone®, Dentsply Sirona, Charlotte, NC, USA) of different heights were also included in the virtual project.
The virtual wax-up was realized according to the digital smile design protocol to determine the ideal width, length, and position of the future teeth [10]. The ideal virtual plan was obtained by integrating prosthetic data with the anatomy of the patient, taking into account noble structures and hard and soft tissues.
Once the virtual project was validated by the surgeon together with the prosthodontist, it was possible to design the prosthetic substructure with the dental CAD (computer-aided design) software (exocad DentalCAD, exocad GmbH, and inLab CAD, Dentsply Sirona, Charlotte, NC, USA) realized in multidirectional interlacing layers of fibreglass and resin matrix (Trinia™, Shofu Dental Corporation, San Marcos, CA, USA). The surgical components were finally designed with the dental CAD software. In particular, the following customized bi-component templates were planned: (1) a reference stent equipped with guiding sleeves for anchor pin fixation and ball-shaped attachment for subsequent insertion of secondary stents; (2) a tooth-supported guiding stent for reference stent fixation; (3) an implant guiding stent; and (4) an abutment guiding stent. All surgical stents were realized with 3D printers (Atom US5 Ultramill, Bquadro, Asti, Italy, and D15, Yenadent, Istanbul, Turkey) and rapid prototyping techniques to transfer the virtual plan to the surgical field.
Surgical procedures
All surgical procedures were performed under local anaesthesia on an outpatient basis by the same surgical team. All surgical stents were previously sterilized with a chemical ethylene oxide solution. Patients were instructed to rinse twice daily with 10 ml of 0.2% chlorhexidine (Dentosan®, Recordati S.p.A., Milan, Italy) starting 1 week before the scheduled surgery. Antibiotic prophylaxis consisting of 2 g of amoxicillin-clavulanate (Augmentin®, GlaxoSmithKline S.p.A., Verona, Italy) was administered 1 h before surgery. Local anaesthesia was induced with Carbocaine 2% with epinephrine 1:100,000 (AstraZeneca S.p.A., Milan, Italy).
The residual teeth were used as reference points to allow correct seating of the first tooth-supported guiding stent connected to the ball-shaped attachment of the reference stent (Fig. 4). In this way, it was possible to transfer the 3D position of the reference stent planned in the virtual project to the mouth of the patient using the residual elements as fixed landmarks. The surgical stent was then secured in the proper position through guided insertion of surgical pins on the buccal side of the alveolar process. Once the reference stent was stabilized, the tooth-supported guiding stent was removed, and extractions of compromised teeth and/or implants were gently carried out, with attempts made to preserve hard and soft tissues (Fig. 5). After the tooth extractions, the implant guiding stent was connected to the reference stent to transfer the virtual 3D position of the implants to the surgical environment according to the final project. The surgical guide allowed the use of different-sized burs to switch the metallic cylinders contained in the stent. Thus, serial osteotomies were performed using disposable internal coolant drills until the planned depth was reached. It was then possible to place the implants (Ankylos® dental implant system, Dentsply Sirona, Charlotte, NC, USA) in the desired position according to the manufacturer’s instructions (Fig. 6). After removal of the implant guiding template, 100 mg of oral nimesulide (Aulin®, Helsinn Birex Pharmaceuticals Ltd., Dublin, Ireland) was administered for pain relief.
Prosthetic procedure
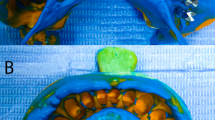
Once all fixtures were inserted with a minimum torque of 35 Ncm and the implant guiding stent removed, the reference stent was still secured in the initial position with the anchor pins. In this way, it was possible to connect the abutment guiding stent to the reference stent (Fig. 7) to screw the 5-degree abutments with the correct axial orientation and parallelism, as required by the fixed telescopic prosthesis. Serial intraoral radiographs were immediately performed to evaluate the proper adaptation of all abutments to the shoulders of the implants. Once this was successfully confirmed, the abutments were tightened according to the manufacturer’s instructions with the recommended torque for the straining screw of 15 Ncm. Subsequently, sterile prefabricated telescopic retainers in gold alloy (Ankylos® Degulor®, Dentsply Sirona, Charlotte, NC, USA) were placed firmly on the abutments (Fig. 8). At this point, the definitive prosthesis was connected to the reference stents to seat the denture on the abutments exactly in the same 3D position as that planned in the virtual environment (Fig. 9). Thus, greater accuracy and stability were provided for the entire workflow. The subsequent phases closely resembled those reported previously [5, 9] in terms of relining, finishing, and polishing (Fig. 10). Finally, the bone pins were extracted, and the reference stent was safely removed. A postoperative orthopantomograph was performed (Fig. 11).
Postoperative procedures
The patients’ postoperative pain was controlled through oral administration of 500 mg of paracetamol and 30 mg of codeine phosphate (Tachidol®, A.C.R.A.F. S.p.A., Rome, Italy) four to six times a day until resolution of the symptomatology. The patients were also asked to perform double mouth rinses with 0.2% chlorhexidine (Dentosan®, Recordati S.p.A., Milan, Italy) for 1 min twice daily for 2 weeks. A soft diet was recommended during the first month after surgery to limit occlusal loading and to reduce micromovements, which may hamper osseointegration. The patients were instructed on oral hygiene and were included in a strict implant maintenance programme consisting of professional oral hygiene recalls every 3 months. Clinical and radiological follow-up evaluations were performed every 6 months from the prosthetic loading to evaluate the survival rate, that is, whether the implant was still physically in the mouth or had been lost [11]. To be considered successful, implants were required to meet all of the following criteria: clinical stability, patient-reported functionality without any discomfort, and the absence of infection [12].
Results
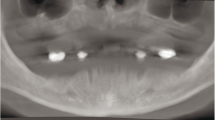
Overall, from January 2017 to January 2018, 11 patients underwent computer-aided template-guided implant placement and immediate loading and were followed for at least 1 year. A total of 7 patients presented with maxillary edentulism, 2 patients with mandibular edentulism, and 2 patients with bimaxillary edentulism. All except one patient received 6 implants per jaw. In one subject, 8 implants were inserted in the upper jaw. Overall, 86 dental implants were inserted and immediately loaded. In all patients, the final rehabilitation consisted of screw-retained implant-supported fixed dental prostheses. The healing period proceeded uneventfully, and no early surgical or prosthetic complications were observed during the initial phases. The implant survival and success rates were 100% over a minimum follow-up period of 1 year from the prosthetic loading. During the follow-up recalls, clinical and radiological evaluations were conducted to detect early signs of peri-implant disease. No clinical signs of peri-implant mucositis or peri-implantitis, such as local swelling, redness, shininess of the soft tissues, soreness and/or pain, bleeding on probing, pus discharge, presence of fistulae, and increasing peri-implant probing depths compared with baseline values registered after 1 month of healing, were observed up to the last follow-up visit (Fig. 12). Clinical examination was corroborated by radiological evaluations consisting of peri-apical and panoramic radiographs. All of the implants appeared to be appropriately integrated within the surrounding bone, with no signs of radiolucency or pathological peri-implant ridge resorption on the mesial and distal aspect (≥ 3 mm) (Fig. 13). No prosthetic complications were observed during the entire study period.
Discussion
The present technical note aims to describe a novel approach to increase the accuracy of the prosthetic phases in the case of computer-guided implant placement and immediate loading. The accuracy of the entire workflow is a crucial factor on which the long-term survival and success of implant-supported rehabilitation depend. As mentioned above, the lack of stable anatomical landmarks as in fully edentulous patients has a negative impact on the overall level of accuracy [1]. Indeed, a more accurate implant position is achieved with tooth-supported templates in partially edentulous patients [3]. Accordingly, the presence of an adjacent natural tooth at the time of implantation may increase the accuracy in completely template-guided implantations [13]. Moreover, the accuracy of computer-guided systems is further reduced in the case of implant placement in fresh extraction sockets compared with healed sites [14].
All of these potentially adverse clinical factors were encountered in the present study. Patients were enrolled if they presented with edentulous jaws characterized by hopeless teeth to be retained during the diagnostic phases until the day of surgery. Teeth were subsequently extracted intra-surgically so that implants were placed in fresh extraction sockets with no remaining reference points. Taken together, all of these clinical features constituted a relevant risk factor for accurate implant insertion. Since inaccuracies have a cumulative effect, discrepancies between the planned and actual position of implants may have dramatic consequences for the outcome of the subsequent prosthetic phase. This explains why the prosthetic advantages of guided surgery are currently still considered to be largely theoretical due to the important number of complications, especially with prostheses, that relieve these protocols [15]. Accordingly, Tahmaseb et al. reported an overall surgical and prosthetic complication rate of 36.4%, with the incidence of surgical complications being significantly lower than the prosthetic complication rate [8]. One might speculate that computer-guided surgery provides a reliable approach for implant survival; however, the adaptation of the prefabricated prosthesis is not sufficiently accurate to allow it to be a definitive prosthesis. The main prosthetic complications were prosthetic screw loosening, prosthetic misfit at the time of suprastructure connection, and prosthesis fracture, which are all strictly related to inaccurate implant insertion.
To overcome such problems and to increase the precision of guided surgery, a reference-based protocol has been introduced to integrate digitally designed surgical guides and superstructures in the case of immediate loading in fully edentulous patients [16]. In brief, reference implants were inserted before the diagnostic phase to have fixed references during the entire workflow up to the prosthetic phases. They were removed after the insertion of the last implant and removal of the surgical guide before prosthetic connection. Thus, unlike in other concepts of guided surgery, there are clear references from the beginning of the procedure to the end of the surgical phase. However, the insertion procedure of these mini-implants is an additional minor surgery for patients. To reduce morbidity and further enhance prosthetic accuracy, a different technique has been developed to find a solution that takes into account the reference points lost during the transition from the surgical guide to the fixation of the prosthesis [9]. To gain the highest level of accuracy in relocating the denture on the implants, the same position and angulation of the guiding sleeves used to anchor the surgical stent were transferred to the temporary prosthesis by means of provisory acrylic resin guides. Consequently, the same bone pins employed during the surgical phase were used to stabilize the prosthesis in the proper position during subsequent prosthetic procedures. On the other hand, even with this approach, there is still a clinical situation characterized by no references in the mouth of the patient except for the guiding holes previously drilled in the bone. In this phase, the repositioning of the bone pins to secure the prosthesis might be difficult. This is explained not only by clinical and prosthetic factors as stated previously. Each additional step potentially introduces errors that may undermine the overall level of accuracy with a cumulative effect.
Therefore, the key aspect of the technique discussed herein was the realization of a reference stent equipped with anchoring devices used to secure all the subsequent stents in the correct position based on the virtual project. In contrast to the other workflows, the stent was maintained in position up to the connection of the prosthesis. Indeed, after implant insertion, it was possible to connect the abutment guiding stent to the reference stent to screw the definitive abutments in the correct position. Following radiographic checks, the abutments were tightened, and telescopic retainers were placed on the abutments. At this point, the prosthesis was connected to the reference stents to seat the denture on the abutments exactly in the same 3D position as that planned in the virtual project. In this way, it was possible to maintain the function and the occlusal vertical dimension already present before the surgical procedure or to replicate the function and the occlusal vertical dimension virtually modified according to the digital wax-up. The secondary aim of abutment fixation was to prevent horizontal and vertical fit discrepancies that may lead to bending stresses in the implant system, contributing to a major proportion of the distortion and biomechanical complications of prostheses, and that may render the screws vulnerable to fatigue fractures and loosening because the preload is used to bring the matching surfaces at the prosthetic interface closer together. The optimal fit obtained with this technique was demonstrated by the fact that no interim prostheses were used, and the definitive prostheses could be immediately connected to the implants, saving time and money for the patient. Radiological and clinical recalls up to 1 year from the prosthetic loading strengthened and consolidated the reliability of this approach on a short-term basis.
It is worth mentioning at this point that none of the patients required osteoplastic procedures to reduce the residual alveolar ridge to increase the occlusal vertical dimension and provide space for the prosthetic components. However, the presented protocol allows the introduction of an additional template that can be screwed to the reference stent before implant insertion, guiding the osteoplastic procedure at the desired level according to the virtual project. Thus, the osteoplastic procedure can be planned in the virtual environment on the basis of the digital prosthetic wax-up while simultaneously considering the position of the implant. The virtual planning of the modified alveolar ridge with a reduced height is subsequently transferred to the surgical field by means of the additional template used to guide the clinician during the osteoplastic procedure.
It must be noted that a multidisciplinary approach including the surgeon, the prosthodontist, and qualified dental technicians is required to obtain successful results. It is also worth noting that, particularly with a digital computer-guided approach, the level of experience of the surgeon may affect the accuracy of implant placement. Greater inaccuracy has been found for inexperienced operators compared with that for experienced surgeons, especially for corono-apical [17] and bucco-lingual [18] deviations. Such discrepancies between the ideal and the achieved position of implants may lead to unwanted horizontal and vertical fit discrepancies of the prosthesis that constitute a relevant risk factor for the long-term outcome. Thus, computer-guided surgery does not completely compensate for the level of operator experience and should be used by well-trained surgeons.
The stability of the residual dentition warrants some attention. Since the position of the reference stent is strictly dependent on the correct seating of the tooth-supported template, the residual dentition obviously plays a pivotal role in the accuracy of the entire workflow from the early moments of the procedure. In the present study, all of the patients presented with at least three teeth with class I mobility according to Miller’s mobility index or with class II mobility masked by fixed prostheses that increased the stability of splinted teeth. In addition, the tooth-supported stent was designed according to the soft tissue profile of the edentulous area distally or in between the residual dentition registered with the optical scan. The extension of the tooth-supported stent to the surrounding mucosa provided additional support that was able to prevent the risk of micromovements related to tooth instability. Thus, in the present study, the mobility of the residual dentition did not constitute a specific complication that was able to influence the accuracy of the workflow. However, a severely compromised periodontally challenged dentition with class III mobility characterized by unstable anatomical landmarks might constitute a relevant risk factor that may significantly jeopardize the correct positioning of the reference stent. In such cases, traditional computer-guided approaches used to treat fully edentulous patients may be preferred to reduce the risk of inaccuracies related to excessively unstable residual teeth. Furthermore, in such cases, the use of ≥ 3 fixed intraoral reference points such as mini-implants may be considered to stabilize radiographic and surgical guides and thus improve the overall accuracy of treatment planning.
Conclusions
The reference-based protocol described herein allowed the surgical and prosthetic digital project to be transferred to the clinical environment during the entire workflow. Implants were inserted in the correct position and were immediately loaded with the definitive prosthesis with a good level of accuracy. This was supported by the fact that no surgical or prosthetic complications were clinically and radiographically observed up to 1 year after the procedure. Further clinical trials are needed to validate this technique on a long-term basis.
References
Orentlicher G, Horowitz A, Kobren L (2019) Computer-guided dental implant treatment of complete arch restoration of edentulous and terminal dentition patients. Oral Maxillofac Surg Clin North Am 31(3):399–426. https://doi.org/10.1016/j.coms.2019.03.004
Beretta M, Poli PP, Tansella S, Aguzzi M, Meoli A, Maiorana C (2020) Cast-free digital workflow for implant-supported rehabilitation in a completely edentulous patient: a clinical report. J Prosthet Dent. https://doi.org/10.1016/j.prosdent.2019.12.009
Al Yafi F, Camenisch B, Al-Sabbagh M (2019) Is digital guided implant surgery accurate and reliable? Dent Clin N Am 63(3):381–397. https://doi.org/10.1016/j.cden.2019.02.006
Patzelt SB, Vonau S, Stampf S, Att W (2013) Assessing the feasibility and accuracy of digitizing edentulous jaws. J Am Dent Assoc 144(8):914–920
Beretta M, Poli PP, Tansella S, Maiorana C (2018) Virtually guided alveolar ridge reduction combined with computer-aided implant placement for a bimaxillary implant-supported rehabilitation: a clinical report. J Prosthet Dent 120:168–172. https://doi.org/10.1016/j.prosdent.2017.11.010
Beretta M, Poli PP, Maiorana C (2014) Accuracy of computer-aided template-guided oral implant placement: a prospective clinical study. J Periodontal Implant Sci 44(4):184–193. https://doi.org/10.5051/jpis.2014.44.4.184
Schneider D, Marquardt P, Zwahlen M, Jung RE (2009) A systematic review on the accuracy and the clinical outcome of computer-guided template-based implant dentistry. Clin Oral Implants Res 20(Suppl 4):73–86. https://doi.org/10.1111/j.1600-0501.2009.01788.x
Tahmaseb A, Wismeijer D, Coucke W, Derksen W (2014) Computer technology applications in surgical implant dentistry: a systematic review. Int J Oral Maxillofac Implants 29(Suppl):25–42. https://doi.org/10.11607/jomi.2014suppl.g1.2
Baruffaldi A, Poli PP, Baruffaldi A, Giberti L, Pigozzo M, Maiorana C (2016) Computer-aided flapless implant surgery and immediate loading. A technical note. Oral Maxillofac Surg 20(3):313–319. https://doi.org/10.1007/s10006-016-0554-5
Coachman C, Calamita MA, Sesma N (2017) Dynamic documentation of the smile and the 2D/3D digital smile design process. Int J Periodontics Restorative Dent 37(2):183–193. https://doi.org/10.11607/prd.2911
ten Bruggenkate CM, van der Kwast WA, Oosterbeek HS (1990) Success criteria in oral implantology. A review of the literature. Int J Oral Implantol 7(1):45–51
Meloni SM, De Riu G, Pisano M, Tullio A (2013) Full arch restoration with computer-assisted implant surgery and immediate loading in edentulous ridges with dental fresh extraction sockets. One year results of 10 consecutively treated patients: guided implant surgery and extraction sockets. J Maxillofac Oral Surg 12(3):321–325. https://doi.org/10.1007/s12663-012-0429-8
Schnutenhaus S, Edelmann C, Rudolph H, Dreyhaupt J, Luthardt RG (2018) 3D accuracy of implant positions in template-guided implant placement as a function of the remaining teeth and the surgical procedure: a retrospective study. Clin Oral Investig 22(6):2363–2372. https://doi.org/10.1007/s00784-018-2339-8
Albiero AM, Quartuccio L, Benato A, Benato R (2019) Accuracy of computer-guided flapless implant surgery in fully edentulous arches and in edentulous arches with fresh extraction sockets. Implant Dent 28(3):256–264. https://doi.org/10.1097/id.0000000000000878
Colombo M, Mangano C, Mijiritsky E, Krebs M, Hauschild U, Fortin T (2017) Clinical applications and effectiveness of guided implant surgery: a critical review based on randomized controlled trials. BMC Oral Health 17(1):150. https://doi.org/10.1186/s12903-017-0441-y
Tahmaseb A, De Clerck R, Aartman I, Wismeijer D (2012) Digital protocol for reference-based guided surgery and immediate loading: a prospective clinical study. Int J Oral Maxillofac Implants 27(5):1258–1270
Rungcharassaeng K, Caruso JM, Kan JY, Schutyser F, Boumans T (2015) Accuracy of computer-guided surgery: a comparison of operator experience. J Prosthet Dent 114(3):407–413. https://doi.org/10.1016/j.prosdent.2015.04.004
Marei HF, Abdel-Hady A, Al-Khalifa K, Al-Mahalawy H (2019) Influence of surgeon experience on the accuracy of implant placement via a partially computer-guided surgical protocol. Int J Oral Maxillofac Implants. https://doi.org/10.11607/jomi.7480
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Baruffaldi, A., Baruffaldi, A., Baruffaldi, M. et al. A suggested protocol to increase the accuracy of prosthetic phases in case of full-arch model-free fully guided computer-aided implant placement and immediate loading. Oral Maxillofac Surg 24, 343–351 (2020). https://doi.org/10.1007/s10006-020-00849-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10006-020-00849-4