Abstract
Schizophrenia (SCZ) is a clinically and genetically heterogeneous disorder that shares genetic factors with autism spectrum disorder (ASD) and attention-deficit hyperactivity disorder (ADHD). A genome-wide association study (GWAS) differentiating ADHD from ASD was performed recently. In this study, we investigated whether polygenic risk scores (PRSs) differentiating ASD from ADHD are associated with cognitive impairments and alterations in cortical structures in SCZ patients. Based on the GWAS data (9,315 ASD and 11,964 ADHD patients), PRSs differentiating ADHD from ASD (indicating a greater risk of ADHD and a lower risk of ASD) were calculated for SCZ patients (n = 168). Cognitive performance, including verbal comprehension (VC), perceptual organization (PO), working memory (WM), and processing speed (PS), was assessed using the WAIS-III (n = 145). The surface areas and cortical thicknesses of 34 bilateral brain regions were extracted using FreeSurfer (n = 126). We examined the associations of these PRSs with cognitive performance and cortical structures in SCZ patients. Among the four cognitive domains, a higher PRS, indicating a greater risk of ADHD, was associated with impaired WM in SCZ patients (beta=-0.21, p = 0.012). A lower PRS, indicating a greater risk of ASD, was associated with decreased surface areas of the left medial orbitofrontal (beta = 0.21, p = 8.29 × 10− 4), left entorhinal (beta = 0.21, p = 0.025), left postcentral (beta = 0.18, p = 7.52 × 10− 3), right fusiform (beta = 0.17, p = 6.64 × 10− 3), and left fusiform cortices (beta = 0.17, p = 7.77 × 10− 3) in SCZ patients. A higher PRS, indicating a greater risk of ADHD, was associated with decreased cortical thickness in the bilateral transverse temporal regions (left, beta=-0.17, p = 0.039; right, beta=-0.17, p = 0.045). Our study revealed a relationship between genetic factors that differentiate ADHD patients from ASD patients and both cortical structure and cognitive performance in SCZ patients. These findings suggest that the heterogeneity of SCZ might be partly derived from genetic factors related to neurodevelopmental and psychiatric disorders other than SCZ.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Schizophrenia (SCZ) is a common, clinically and genetically heterogeneous psychiatric disorder. The lifetime morbidity rate of SCZ patients ranges from 0.5 to 1.0%, and SCZ is characterized by cognitive impairments; positive symptoms, such as hallucinations and delusions; and negative symptoms, such as blunted affect, poor rapport, and stereotyped thinking. Autism spectrum disorder (ASD) and attention-deficit hyperactivity disorder (ADHD) are common neurodevelopmental disorders. ASD affects approximately 1.0% of individuals [1] and is characterized by impaired social interactions and communication, along with restricted and repetitive behavior from early development. ADHD affects approximately 5.0% of children and 2.5% of adults and is characterized by greater inattention and impulsivity compared to individuals with typical development. Although these disorders are distinguished as different psychiatric and neurodevelopmental disorders based on their clinical symptoms according to international diagnostic criteria, the Diagnostic and Statistical Manual of Mental Disorders (DSM) and the International Classification of Diseases (ICD), the prevalence of ASD in individuals with SCZ has been reported to range from 3.4 to 52.0% [2], and the prevalence of childhood and adult ADHD in individuals with SCZ ranges from 10.0 to 57.0% [3]. This suggests considerable clinical heterogeneity among individuals with SCZ.
SCZ [4,5,6,7], ASD [8], and ADHD [9] are highly heritable disorders, with estimated heritability rates of approximately 60–90%. Large-scale genome-wide association studies (GWASs) conducted by the SCZ, ASD, and ADHD Working Group of the Psychiatric Genomics Consortium (PGC) and the Lundbeck Foundation Initiative for Integrative Psychiatric Research (iPSYCH) have identified 287, 5, and 12 distinct genome-wide-significant loci for SCZ [10], ASD [11] and ADHD [12], respectively. These disorders share a partially overlapping genetic etiology [11,12,13,14,15]. Moderately positive genetic correlations have been found between SCZ and ASD (rG=0.21) [11] and ADHD (rG=0.12) [12].
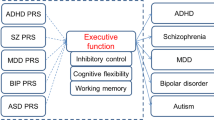
Moreover, a recent GWAS from the iPSYCH and the PGC differentiating the two neurodevelopmental disorders (ASD and ADHD) in 9,315 individuals with ASD and 11,964 individuals with ADHD identified five neurodevelopmental disorder-specific loci [16]. The genetic factor differentiating ADHD from ASD (indicating a higher risk of ADHD and a lower risk of ASD) was positively correlated with ADHD (rG=0.59) and negatively correlated with ASD (rG=-0.60), with no significant correlation with SCZ (rG=-0.03) [16]. SCZ and ADHD have shown negative genetic correlations with cognitive function [SCZ; rG=-0.46 [17], ADHD; rG=-0.41 [12]], whereas ASD has demonstrated positive genetic correlations with cognitive function (rG=0.20) [11]. Furthermore, the genetic factor differentiating ADHD from ASD was negatively correlated with several cognitive traits, including years of schooling (rG=-0.67) and intelligence (rG=-0.59) [16].
Cortical surface area and thickness are associated with increased brain function and serve as independent morphological markers of cortical structure. It has been suggested that different developmental mechanisms underlie surface area expansion and increases in thickness [18]. The SCZ, ASD, and ADHD Working Groups of the worldwide ENIGMA (Enhancing Neuro Imaging Genetics through Meta-Analysis) consortium have investigated disorder-specific abnormalities in regional surface area and cortical thickness [19,20,21]. Compared with healthy participants, individuals with SCZ exhibit a widespread smaller cortical surface area and thinner cortex [19]. Increased cortical thickness in the frontal cortex and decreased cortical thickness in the temporal cortex have been observed in individuals with ASD, with no differences in surface area compared to healthy participants [21]. Compared with healthy individuals, individuals with ADHD have a widespread decrease in cortical surface area and a partially thinner cortex, including the fusiform gyrus, precentral gyrus, and temporal pole [20]. Moreover, adults with ADHD exhibit lower cortical thickness in the orbitofrontal, inferior frontal and cingulate areas than adults with ASD [22]. Large-scale GWASs for regional cortical surface area and thickness have identified 369 genome-wide nominally significant loci related to cortical structures [18]. 26% of the variation in average cortical thickness and 34% of the variation in total surface area can be explained by common single-nucleotide polymorphisms (SNPs) [18]. Although genetic correlations of regional cortical structures with the risk of SCZ, ASD, and ADHD have been identified, e.g., SCZ and the medial orbitofrontal area (rG=0.10), ADHD and the fusiform area (rG=-0.14), and ASD and the fusiform area (rG=-0.15) [18], no study has yet investigated the genetic correlations between the genetic factor differentiating ADHD from ASD and brain cortical structures or whether this genetic factor influences cognitive functions and brain cortical structures in patients with SCZ.
Given the clinical and genetic heterogeneity of SCZ and its significant overlap with ASD and ADHD, our study focuses specifically on SCZ to better understand the distinct genetic contributions to cognitive impairments and cortical abnormalities within this population. By isolating SCZ as the primary condition, we aim to elucidate the unique and shared genetic underpinnings that differentiate it from other neurodevelopmental disorders.
The significance of this study lies in its potential to unravel the specific genetic influences on cognitive impairments and cortical abnormalities in SCZ. By exploring the polygenic risk scores (PRSs) differentiating ADHD from ASD, we aim to contribute to the understanding of the genetic architecture that impacts cognitive functions and brain structures in SCZ. This could lead to more precise diagnostic tools and personalized treatment strategies, ultimately improving outcomes for individuals with SCZ. PRSs reflect the additive effects of a large number of common SNPs associated with specific psychiatric and neurodevelopmental disorders [23]. Given that SCZ is clinically and genetically heterogeneous and shares disorder-specific genetic factors with ADHD and ASD, we hypothesized that PRSs differentiating ADHD from ASD would be associated with cognitive impairments and abnormalities in regional surface area and cortical thickness (e.g., decreased cortical thickness and surface area in the frontal cortex) in patients with SCZ. In this study, we investigated whether PRSs based on the GWAS differentiating ADHD from ASD, i.e., neurodevelopmental disorder-specific PRSs, were associated with brain cortical structures as well as cognitive function in patients with SCZ.
Methods
Discovery GWAS differentiating ADHD from ASD (ASDvs.ADHD)
To identify disorder-specific (ASD vs. ADHD) variants, including their p values and odds ratios (ORs), we utilized the publicly available GWAS dataset (ASD vs. ADHD) [16] from iPSYCH and the PGC (https://ipsych.dk/en/research/downloads). This dataset comprised 9,315 individuals with ASD and 11,964 individuals with ADHD, all of whom were of European descent [16]. ASD patients in iPSYCH through the Danish Psychiatric Central Research Register (DPCRR) were diagnosed by a psychiatrist according to the ICD, Tenth Revision (ICD-10), and included diagnoses of childhood autism developmental disorders (F84.0), atypical autism (F84.1), Asperger’s syndrome (F84.5), other pervasive developmental disorders (F84.8), and pervasive developmental disorder, unspecified (F84.9). ASD diagnosis of patients in the PGC was achieved through standard research tools, such as the Autism Diagnostic Interview-Revised (ADI-R), the Autism Diagnostic Observation Schedule (ADOS) or international diagnostic criteria [DSM, Fourth Edition (DSM-IV); ICD, Ninth Revision (ICD-9); or ICD-10], and expert clinical consensus. ADHD patients in iPSYCH through the National Psychiatric Central Research Register were diagnosed by psychiatrists at a psychiatric hospital according to the ICD-10 (F90.0). ADHD patients in the PGC were diagnosed according to the DSM, Third Edition Reserved (DSM-III-R), DSM-IV, or ICD-10. Individuals with moderate to severe mental retardation (ICD-10: F71-F79) were excluded. The participants were genotyped using different arrays for each study site. Quality control (QC) and imputation were performed for each dataset separately, as previously described [16]. For PRS analysis, SNPs with low imputation quality (INFO < 0.6) and low genotyping rates of whole subjects (< 60%) were excluded, ultimately resulting in the retention of 6,168,324 SNPs.
Target sample description
Our target sample included 168 SCZ patients (mean age ± SD: 45.1 ± 13.6 years, 76 males/92 females), all of whom were of Japanese descent with no known first- or second-degree relatives with SCZ. The demographic details are summarized in Table 1. Patients were recruited from the Schizophrenia Non-Affected Relative Project (SNARP) [24,25,26,27,28,29,30,31], and were diagnosed using unstructured clinical interviews, medical records, and clinical consensus according to the criteria in the DSM-5. The exclusion criteria included neurological or medical conditions affecting the central nervous system, such as atypical headache, head trauma, chronic lung disease, kidney or liver diseases, active cancer, cerebrovascular disease, thyroid disorders, epilepsy, seizures, substance-related disorders, steroid use, or intellectual disability. Only two SCZ patients had comorbid ASD, and no SCZ patients had comorbid ADHD. Clinical symptoms were assessed with the Positive and Negative Syndrome Scale (PANSS), and premorbid IQ was measured using the Japanese version of the National Adult Reading Test (JART) [32]. Written informed consent was obtained from all participants after the procedures were thoroughly explained. This study was performed in accordance with the World Medical Association’s Declaration of Helsinki and was approved by the Research Ethics Committees of Gifu University and Kanazawa Medical University.
Genotyping and imputation
A detailed description of the genotyping, QC and imputation procedures applied in larger samples, including the current target sample and previous participants (n = 420), to increase the reliability has been provided previously [26, 28]. Briefly, peripheral venous blood was collected from the target subjects, and genomic DNA was extracted from the whole-blood samples. Genotyping was performed using the Infinium OmniExpressExome-8 v1.4 or v1.6 BeadChips (Illumina, San Diego, CA, USA). We excluded SNPs that (i) were duplicated or ambiguous, (ii) were localized on sex chromosomes or mitochondria, (iii) deviated from Hardy-Weinberg equilibrium (HWE) (p < 1.0 × 10− 5), or (iv) had a low minor allele frequency (MAF) < 0.001. Genotype imputation was performed using the 1000 Genomes Project Phase 3 dataset as a reference panel. To obtain a highly informative SNP set, insertion‒deletion polymorphisms were excluded, and SNPs with high imputation quality (> 0.9) were retained for PRS analysis. Ultimately, 8,538,535 SNPs were retained.
PRS calculations
To remove SNPs that were in linkage disequilibrium (LD) in the target sample, the SNPs were pruned using a pairwise r2 threshold of 0.25 and a window size of 200 SNPs using PLINK v1.9 [26,27,28,29,30]. After pruning, 1,510,671 independent SNPs remained. Because common disorders are influenced by numerous SNPs across the genome, we then calculated PRSs constructed from alleles showing a nominal association with individuals (ASD vs. ADHD) in the discovery GWAS with the following PThreshold (PT) cutoff values: PT<1.00 × 10− 3, PT<0.01, PT<0.05, PT<0.1, PT<0.2, PT<0.5 and PT≤1. The PT value represents the p-value threshold for including SNPs in the PRS calculation. Since polygenic disorders are likely to involve a large number of SNPs, we employed more relaxed PT values to capture a broader range of SNPs potentially associated with the disorder. For each individual included in the target sample, a PRS was calculated by weighing the scores for “risk variants” by the logarithm of the OR (logOR) observed in the discovery dataset. The score, consisting of the number of risk variants for differentiating ADHD from ASD (0, 1, or 2) multiplied by the logarithm of the OR, was summed over all of the SNPs in seven PT-SNP sets for each individual in the target sample. A higher PRS indicated a greater risk of ADHD and a lower risk of ASD, while a lower PRS indicated a greater risk of ASD and a lower risk of ADHD.
Cognitive performance
Cognitive performance in 145 SCZ patients was assessed in four domains—verbal comprehension (VC), perceptual organization (PO), working memory (WM), and processing speed (PS)—using the Japanese version of the Wechsler Adult Intelligence Scale, third edition (WAIS-III) [33]. These cognitive domains were adjusted for age.
MRI procedure and segmentation of surface area and cortical thickness
Brain magnetic resonance imaging (MRI) was performed on 126 SCZ patients using a Siemens 3T Magnetom Trio, a Tim System (Siemens, Erlangen, Germany). High-resolution T1-weighted images were acquired with a 3D magnetization-prepared rapid gradient echo (MP-RAGE) sequence (TR = 1420 ms, inversion time = 800 ms, echo time = 2.08 ms, flip angle = 9°, resolution = 1 × 1 × 1 mm3, matrix size = 256 × 256), yielding 192 contiguous 1 mm thick slices in the sagittal plane [34,35,36,37,38,39,40]. We obtained high-resolution T1-weighted images with good contrast between gray matter and white matter in our scanning environment. We screened out subjects with MRI abnormalities, such as infarcts, hemorrhages, or brain tumors, and images with motion or metal artifacts prior to inclusion in this study. Next, the T1-weighted images were processed with FreeSurfer v6.0 using the software package’s default automated reconstruction procedure (‘recon-all’; http://surfer.nmr.mgh.harvard.edu), and surface area and cortical thickness were segmented in 34 brain regions in the right and left hemispheres. These procedures were fully automated and did not involve any manual editing of the images with tissue misclassification. All cortical parcellations were defined from the Desikan–Killiany atlas. Segmented surface area and cortical thickness were visually inspected using a 3D slicer, and there were no subjects with obviously poor segmentation.
Statistical analysis
All the statistical analyses were performed using IBM SPSS Statistics 28.0 software (IBM Japan, Tokyo, Japan). We explored the association of PRSs differentiating ADHD from ASD at PT<0.5 with cognitive performance in our target SCZ patients using linear regression analyses with cognitive function as the dependent variable, PRSs differentiating ADHD from ASD as the independent variable, and age and sex as covariates, although age was adjusted for when calculating cognitive domain scores. Following a previous study [41], we investigated the effects of PRSs differentiating ADHD from ASD based on each PT on cortical structures (surface area and cortical thickness) in our target SCZ patients using linear regression analyses with cortical structures as the dependent variable; PRSs differentiating ADHD from ASD based on each PT as the independent variable; and age, sex, age2, age×sex, and intracranial volume (ICV) as covariates for surface area or age and sex as covariates for cortical thickness. The proportion of the variance for each cortical structure explained by the PRSs was indicated by the adjusted R2. To determine the variance explained only by the PRS, we subtracted the adjusted R2 for the covariates alone from those of the models. The nominal two-tailed significance level for all the statistical tests was set at p < 0.05. A conservative Bonferroni-corrected p value threshold of p < 1.47 × 10− 3 (= 0.05/34 brain regions) was used in the PRS analysis to avoid type I errors.
Results
Associations of the PRSs differentiating ADHD from ASD (ADHDvs.ASD) with cognitive impairments in patients with SCZ
Consistent with the negative genetic correlation between the factor differentiating ADHD from ASD and cognitive impairments [16], we observed the association of the PRS differentiating ADHD from ASD at PT<0.5 with four cognitive performances—VC, PO, WM, and PS—in SCZ patients (p < 0.05). Notably, a higher PRS (indicating a greater risk of ADHD and a lower risk of ASD) was significantly correlated with impaired WM in SCZ patients (Fig. 1, beta=-0.21, p = 0.012). However, no significant correlations were found between the PRS and the other three cognitive domains (p > 0.05).
Correlations of the PRSs differentiating ADHD from ASD (ASD vs. ADHD) with working memory and the left medial orbitofrontal area in patients with SCZ. A higher PRS indicated a greater risk of ADHD and a lower risk of ASD, while a lower PRS indicated a greater risk of ASD and a lower risk of ADHD. Working memory scores and the left medial orbitofrontal area were corrected for confounding factors as covariates. The PRS differentiating ADHD from ASD was z-transformed. PRS, polygenic risk score; ADHD, attention-deficit hyperactivity disorder; ASD, autism spectrum disorder, SCZ, schizophrenia
Associations of the PRSs differentiating ADHD from ASD with surface areas in patients with SCZ
We next investigated the associations of the PRS differentiating ADHD from ASD at PT<0.5 with cortical surface area in SCZ patients (Fig. 2). The PRSs differentiating ADHD from ASD at PT<0.5 showed a nominal positive correlation with five surface areas: the left medial orbitofrontal area, left entorhinal area, left fusiform area, left postcentral area, and right fusiform area (p < 0.05, Figs. 2 and 3). Specifically, a lower PRS (indicating a greater risk of ASD and a lower risk of ADHD) was significantly associated with a decreased left medial orbitofrontal area (beta = 0.21, p = 8.29 × 10− 4) and marginally associated with a decreased left entorhinal area (beta = 0.21, p = 0.025), left postcentral area (beta = 0.18, p = 7.52 × 10− 3), right fusiform area (beta = 0.17, p = 6.64 × 10− 3), and left fusiform area (beta = 0.17, p = 7.77 × 10− 3) (Fig. 2).
Effects of PRSs differentiating ADHD from ASD at PT<0.5 on surface area and cortical thickness in 34 brain regions in each hemisphere in patients with SCZ. Effect sizes (beta values) are represented as a heatmap. Red represents a larger surface area or thicker cortical thickness, and blue represents a smaller surface area or thinner cortical thickness in patients with a greater PRS
Effects of the PRSs differentiating ADHD from ASD at various thresholds (from PT cutoff<0.001 to PT cutoff<1) on surface areas in patients with SCZ. Five surface areas that showed marginally significant correlations with the PRSs differentiating ADHD from ASD at PT<0.5 (p < 0.05) are highlighted. Each y-axis shows the adjusted R2, indicating the explanatory power of the model. Red indicates the association of the lower PRS (indicating a higher risk of ASD) with the decreased surface area. *p < 0.05, ** p < 0.01, *** p < 1.47 × 10− 3
Additionally, we examined the effect of PRSs differentiating ADHD from ASD at various PT levels (from PT<0.001 to PT≤1) on these five surface areas (Fig. 3). The PRSs differentiating ADHD from ASD were significantly positively associated with the left medial orbitofrontal area at several PT levels (p < 1.47 × 10− 3, from PT<0.05 to PT≤1, a maximum at PT<0.05: R2 = 0.053, beta = 0.24, p = 1.48 × 10− 4) and nominally positively associated with the left medial orbitofrontal area at PT<0.01 and 0.001 (1.47 × 10− 3<p < 0.05). A lower PRS differentiating ADHD from ASD at PT <0.05 was significantly correlated with a smaller left medial orbitofrontal area in patients with SCZ (Fig. 1). Among the other four surface areas, PRSs at several PT levels were nominally positively associated with the left entorhinal area, left fusiform area, left postcentral area, and right fusiform area (1.47 × 10− 3<p < 0.05). However, these associations between the PRSs and the four surface areas did not remain significant after Bonferroni correction (p > 1.47 × 10− 3). The left medial orbitofrontal area was not significantly correlated with WM in our patients (p > 0.05), suggesting independent associations of PRSs differentiating ADHD from ASD with WM and this particular cortical area.
Associations of the PRSs differentiating ADHD from ASD with cortical thickness in patients with SCZ
We investigated the associations of PRSs differentiating ADHD from ASD at PT<0.5 with cortical thickness in patients with SCZ (Figs. 2 and 4). We found that PRSs differentiating ADHD from ASD at PT<0.5 were marginally correlated with two cortical thicknesses, the bilateral transverse temporal thickness, in SCZ patients (p < 0.05, Figs. 2 and 4). The PRS was marginally negatively associated with the left transverse temporal thickness (beta=-0.17, p = 0.039) and right transverse temporal thickness (beta=-0.17, p = 0.045). There were no significant associations between PRS and other cortical thicknesses (p > 0.05).
Effects of the PRSs differentiating ADHD from ASD at various thresholds (from PT cutoff<0.001 to PT cutoff≤1) on cortical thickness in patients with SCZ. Two cortical thicknesses showing marginally significant correlations with the PRSs differentiating ADHD from ASD at PT<0.5 (p < 0.05) are highlighted. Each y-axis shows the adjusted R2, indicating the model’s explanatory power. Blue highlights the associations of a higher PRS (indicating a greater risk of ADHD) with thinner cortical thickness. * p < 0.05
Further analysis of the associations of PRSs differentiating ADHD from ASD at different PT levels (from PT<0.001 to PT≤1) with bilateral transverse temporal thickness in patients with SCZ (Fig. 4) revealed marginal associations of higher PRSs (indicative of higher ADHD risk) with decreased right transverse temporal thickness at PT<0.5 and PT≤1 (p < 0.05, a maximum at PT<0.5: R2 = 0.021, beta=-0.17, p = 0.045) and left transverse temporal thickness at PT<0.5 only (R2 = 0.024, beta=-0.17, p = 0.039). However, these associations did not remain significant after correction for multiple testing (p > 1.47 × 10− 3).
Discussion
To our knowledge, this is the first study to investigate the association of PRSs differentiating ADHD from ASD with both cortical structures and cognitive performance in patients with SCZ. Consistent with our hypothesis, a higher PRS (indicating a greater risk of ADHD) was associated with impaired cognitive function in SCZ patients. A lower PRS (indicating a greater risk of ASD) was associated with smaller surface areas in five regions (left medial orbitofrontal, left entorhinal, left postcentral, and bilateral fusiform) in SCZ patients. A greater PRS (indicating a greater risk of ADHD) was associated with thinner cortical thicknesses in two regions (bilateral transverse temporal). Notably, the association between the PRS and the left medial orbitofrontal area remained significant even after correcting for multiple testing. These findings suggest that the PRS differentiating ADHD from ASD might reflect cognitive dysfunction and specific cortical structures in SCZ patients, and patients with SCZ who are clinically and genetically heterogeneous might be stratified by the PRS.
Consistent with previous findings on the genetic correlation between ADHD and ASD differentiation and cognitive dysfunctions [16], we identified a genetic correlation between the PRS differentiating ADHD from ASD and cognitive impairment, particularly in WM, in SCZ patients. This finding is consistent with clinical observations that individuals with ADHD typically exhibit lower cognitive function, especially in WM, than do those with ASD [42,43,44]. SCZ is characterized by severe cognitive impairments, notably WM [45, 46]. These clinical cognitive findings in individuals with ADHD, ASD and SCZ might be supported by the genetic correlations: SCZ and ADHD both show negative genetic correlations with cognitive functions [12, 17], while ASD shows a positive genetic correlation with cognitive functions [11]. Additionally, the genetic factor that differentiates ADHD from ASD is negatively correlated with cognitive functions [16].
The current study demonstrated that a lower PRS differentiating ADHD from ASD (indicating a greater risk of ASD) was significantly correlated with a smaller left medial orbitofrontal area in SCZ patients. Although SCZ patients typically have a smaller medial orbitofrontal surface area than healthy individuals [19], studies on individuals with ASD have shown heterogeneous results [18, 21, 47, 48]. Some studies have shown that individuals with ASD have a smaller medial orbitofrontal surface area than healthy individuals [47, 48], while others have reported no difference between individuals with ASD and healthy individuals [18, 21]. The orbitofrontal cortex is important for decision-making, goal-directed behavior, and emotional processing of faces and is associated with emotional and social behaviors [49,50,51,52]. Damage to the orbitofrontal cortex caused by tumors, hemorrhage, ischemic stroke, or aneurysm rupture leads to irrational behavior, as individuals are unable to properly predict the consequences of choosing things in the social environment [51,52,53]. Individuals with SCZ and ASD often display impaired goal-directed decision-making [54,55,56,57] and a decreased ability to recognize emotions in others’ faces and make social judgments [58,59,60,61,62]. Our findings suggest that the PRS for differentiating ASD from ADHD might be related to social dysfunctions via the decreased medial orbitofrontal surface area in SCZ patients.
Although we focused on the associations of PRSs differentiating ADHD from ASD with brain cortical structures, it is important to consider the potential involvement of PRSs in determining shared liability of ADHD and ASD in cortical structures, particularly the orbitofrontal area, in SCZ patients. While we further explored these relationships, no significant correlations between the PRS for shared liability to ADHD and ASD and any cortical structures, including cortical thickness and surface area, were found (p > 1.47 × 10− 3).
Although it is not the main purpose of our study, to provide a baseline for comparison, we additionally explored the influences of PRSs differentiating ASD from ADHD on cognitive functions and alterations in cortical structures in 195 psychiatrically and neurodevelopmentally healthy individuals (the subject recruitment was described in previous studies [24,25,26,27,28,29,30,31]). A higher PRS, indicating a greater risk of ADHD, at PT<0.5, was nominally associated with decreased surface area of the transverse temporal region (beta=-0.16, p = 0.020) and decreased cortical thickness in the left postcentral gyrus (beta=-0.14, p = 0.049) in 175 healthy individuals, while these marginal associations did not remain significant after correction for multiple testing (p > 1.47 × 10− 3). In contrast, there were no significant associations between the PRSs and four cognitive performances—VC, PO, WM, and PS— in 153 healthy individuals (p > 0.05). The fact that we assessed healthy subjects who were carefully screened to exclude psychiatric and neurodevelopmental patients [24,25,26,27,28,29,30,31] might have contributed to the lack of these associations in the healthy subjects. Similar associations to those in SCZ patients might be obtained in the general population, including patients with psychiatric or neurodevelopmental disorders.
There are limitations in interpreting our findings. This study focused exclusively on SCZ patients, limiting the scope of understanding whether these genetic factors also contribute to stratification in other psychiatric disorders. Although we found associations between higher and lower PRSs differentiating ADHD from ASD with impaired working memory and reduced left medial orbitofrontal area, respectively, the relationships of these PRSs with the risk and progression of SCZ remain unclear. Future studies should include other psychiatric disorder groups to better elucidate the impact of these PRSs on individuals with SCZ. This would enhance our understanding of the distinct and overlapping genetic contributions to cognitive and cortical abnormalities in SCZ compared to other psychiatric disorders.
In conclusion, our study revealed associations between genetic factors differentiating ADHD from ASD and both cortical structures and cognitive performance in SCZ patients. These findings suggest that the clinical and genetic heterogeneity in SCZ patients might be influenced by genetic factors associated with other neurodevelopmental and psychiatric disorders beyond SCZ.
Data availability
No datasets were generated or analysed during the current study.
References
APA (2013) Diagnostic and statistical manual of mental disorders,Fifth Edition. Pub lisher, Washington, DC.
Zheng Z et al (2018) Association between schizophrenia and autism spectrum disorder: a systematic review and meta-analysis. Autism Res 11(8):1110–1119
Arican I et al (2019) Prevalence of attention deficit hyperactivity disorder symptoms in patients with schizophrenia. Acta Psychiatr Scand 139(1):89–96
Sullivan PF et al (2003) Schizophrenia as a complex trait: evidence from a meta-analysis of twin studies. Arch Gen Psychiatry 60(12):1187–1192
Lichtenstein P et al (2009) Common genetic determinants of schizophrenia and bipolar disorder in Swedish families: a population-based study. Lancet 373(9659):234–239
Cannon TD et al (1998) The genetic epidemiology of schizophrenia in a Finnish twin cohort. A population-based modeling study. Arch Gen Psychiatry 55(1):67–74
Hilker R et al (2018) Heritability of Schizophrenia and Schizophrenia Spectrum based on the nationwide Danish twin Register. Biol Psychiatry 83(6):492–498
Sandin S et al (2017) The heritability of Autism Spectrum Disorder. JAMA 318(12):1182–1184
Faraone SV, Larsson H (2019) Genetics of attention deficit hyperactivity disorder. Mol Psychiatry 24(4):562–575
Trubetskoy V et al (2022) Mapping genomic loci implicates genes and synaptic biology in schizophrenia. Nature 604(7906):502–508
Grove J et al (2019) Identification of common genetic risk variants for autism spectrum disorder. Nat Genet 51(3):431–444
Demontis D et al (2019) Discovery of the first genome-wide significant risk loci for attention deficit/hyperactivity disorder. Nat Genet 51(1):63–75
Smoller JW et al (2013) Identification of risk loci with shared effects on five major psychiatric disorders: a genome-wide analysis. Lancet 381(9875):1371–1379
Mullin AP et al (2013) Neurodevelopmental disorders: mechanisms and boundary definitions from genomes, interactomes and proteomes. Transl Psychiatry 3(12):e329
Mitchell KJ (2011) The genetics of neurodevelopmental disease. Curr Opin Neurobiol 21(1):197–203
Mattheisen M et al (2022) Identification of shared and differentiating genetic architecture for autism spectrum disorder, attention-deficit hyperactivity disorder and case subgroups. Nat Genet 54(10):1470–1478
Toulopoulou T et al (2010) Impaired intellect and memory: a missing link between genetic risk and schizophrenia? Arch Gen Psychiatry 67(9):905–913
Grasby KL et al (2020) The genetic architecture of the human cerebral cortex. Science 367(6484)
van Erp TGM et al (2018) Cortical brain abnormalities in 4474 individuals with Schizophrenia and 5098 control subjects via the Enhancing Neuro Imaging Genetics through Meta Analysis (ENIGMA) Consortium. Biol Psychiatry 84(9):644–654
Hoogman M et al (2019) Brain imaging of the cortex in ADHD: a coordinated analysis of large-Scale Clinical and Population-based samples. Am J Psychiatry 176(7):531–542
van Rooij D et al (2018) Cortical and subcortical brain morphometry differences between patients with autism spectrum disorder and Healthy Individuals across the Lifespan: results from the ENIGMA ASD Working Group. Am J Psychiatry 175(4):359–369
Hoogman M et al (2022) Consortium neuroscience of attention deficit/hyperactivity disorder and autism spectrum disorder: the ENIGMA adventure. Hum Brain Mapp 43(1):37–55
Purcell SM et al (2009) Common polygenic variation contributes to risk of schizophrenia and bipolar disorder. Nature 460(7256):748–752
Ohi K et al (2019) Intelligence decline between present and premorbid IQ in schizophrenia: Schizophrenia non-affected relative project (SNARP). Eur Neuropsychopharmacol 29(5):653–661
Ohi K et al (2021) Intelligence decline across major depressive disorder, bipolar disorder, and schizophrenia. CNS Spectr: 1–7
Ohi K et al (2023) Cognitive performances across individuals at high genetic risk for schizophrenia, high genetic risk for bipolar disorder, and low genetic risks: a combined polygenic risk score approach. Psychol Med 53(10):4454–4463
Ohi K et al (2020) Polygenic risk scores for late smoking initiation associated with the risk of schizophrenia. NPJ Schizophr 6(1):36
Ohi K et al (2020) Polygenetic risk scores for Major Psychiatric disorders among Schizophrenia patients, their first-degree relatives, and healthy participants. Int J Neuropsychopharmacol 23(3):157–164
Ohi K et al (2021) Polygenic risk scores differentiating Schizophrenia from Bipolar Disorder are Associated with Premorbid Intelligence in Schizophrenia patients and healthy subjects. Int J Neuropsychopharmacol 24(7):562–569
Ohi K et al (2024) Genome-wide DNA methylation risk scores for schizophrenia derived from blood and brain tissues further explain the genetic risk in patients stratified by polygenic risk scores for schizophrenia and bipolar disorder. BMJ Ment Health 27(1)
Tachi R et al (2023) Mitochondrial genetic variants associated with bipolar disorder and Schizophrenia in a Japanese population. Int J Bipolar Disord 11(1):26
Matsuoka K et al (2006) Estimation of premorbid IQ in individuals with Alzheimer’s disease using Japanese ideographic script (Kanji) compound words: Japanese version of National Adult Reading Test. Psychiatry Clin Neurosci 60(3):332–339
Wechsler D (1997) Manual for the Wechsler adult intelligence scale 3rd edition. San Antonio, TX: Pub lisher
Ohi K et al (2016) Structural alterations of the superior temporal gyrus in schizophrenia: detailed subregional differences. Eur Psychiatry 35:25–31
Ohi K et al (2017) A Brief Assessment of Intelligence Decline in Schizophrenia as represented by the difference between current and Premorbid Intellectual Quotient. Front Psychiatry 8:293
Ohi K et al (2021) Alterations in hippocampal subfield volumes among schizophrenia patients, their first-degree relatives and healthy subjects. Prog Neuropsychopharmacol Biol Psychiatry 110:110291
Ohi K et al (2022) Common brain cortical abnormality in smoking behavior and bipolar disorder: discriminant analysis using cortical thickness and surface area. Cereb Cortex 32(20):4386–4396
Fujikane D et al (2023) Higher polygenic risk scores for anxiety disorders are associated with reduced area in the anterior cingulate gyrus. J Affect Disord 320:291–297
Ohi K et al (2022) Differences in subcortical brain volumes among patients with schizophrenia and bipolar disorder and healthy controls. J Psychiatry Neurosci 47(2):E77–E85
Aoyama S et al (2023) Sex differences in brainstem structure volumes in patients with schizophrenia. Schizophrenia (Heidelb) 9(1):16
Hibar DP et al (2018) Cortical abnormalities in bipolar disorder: an MRI analysis of 6503 individuals from the ENIGMA bipolar disorder Working Group. Mol Psychiatry 23(4):932–942
Kanai C et al (2017) Cognitive profiles of adults with high-functioning autism spectrum disorder and those with attention-deficit/hyperactivity disorder based on the WAIS-III. Res Dev Disabil 61(108 – 15.
Takeuchi A et al (2013) Inhibitory function and working memory in attention deficit/hyperactivity disorder and pervasive developmental disorders: does a continuous cognitive gradient explain ADHD and PDD traits? Acta Med Okayama 67(5):293–303
Sinzig J et al (2008) Inhibition, flexibility, working memory and planning in autism spectrum disorders with and without comorbid ADHD-symptoms. Child Adolesc Psychiatry Ment Health 2(1):4
Lee J, Park S (2005) Working memory impairments in schizophrenia: a meta-analysis. J Abnorm Psychol 114(4):599–611
Kalkstein S et al (2010) Neurocognition in schizophrenia. Curr Top Behav Neurosci 4(373 – 90.
Park MTM et al (2018) Neuroanatomical phenotypes in mental illness: identifying convergent and divergent cortical phenotypes across autism, ADHD and schizophrenia. J Psychiatry Neurosci 43(3):201–212
Matsumoto J et al (2023) Cerebral cortical structural alteration patterns across four major psychiatric disorders in 5549 individuals. Mol Psychiatry
O’Doherty J et al (2001) Abstract reward and punishment representations in the human orbitofrontal cortex. Nat Neurosci 4(1):95–102
Troiani V et al (2016) Characterization of Face-Selective patches in Orbitofrontal Cortex. Front Hum Neurosci 10:279
Noonan MP et al (2017) Contrasting effects of medial and lateral Orbitofrontal cortex lesions on credit assignment and decision-making in humans. J Neurosci 37(29):7023–7035
Rudebeck PH, Rich EL (2018) Orbitofrontal cortex. Curr Biol 28(18):R1083–r8
Camille N et al (2011) Double dissociation of stimulus-value and action-value learning in humans with orbitofrontal or anterior cingulate cortex damage. J Neurosci 31(42):15048–15052
Boka E et al (2020) Ineffective risk-reward learning in schizophrenia. Psychiatry Res 293:113370
Saperia S et al (2019) Reward-driven decision-making impairments in schizophrenia. Schizophr Res 206(277 – 83.
Luke L et al (2012) Decision-making difficulties experienced by adults with autism spectrum conditions. Autism 16(6):612–621
Carlisi CO et al (2017) Shared and disorder-specific neurocomputational mechanisms of decision-making in Autism Spectrum disorder and obsessive-compulsive disorder. Cereb Cortex 27(12):5804–5816
Mandal MK et al (2023) Facial expression-based indicators of schizophrenia: evidence from recent research. Schizophr Res 252(335 – 44.
Marwick K, Hall J (2008) Social cognition in schizophrenia: a review of face processing. Br Med Bull 88(1):43–58
Webster PJ et al (2021) Review: posed vs. genuine facial emotion recognition and expression in autism and implications for intervention. Front Psychol 12:653112
Kennedy DP, Adolphs R (2012) Perception of emotions from facial expressions in high-functioning adults with autism. Neuropsychologia 50(14):3313–3319
Martínez A et al (2019) Differential patterns of visual sensory alteration underlying face emotion recognition impairment and motion perception deficits in Schizophrenia and Autism Spectrum Disorder. Biol Psychiatry 86(7):557–567
Acknowledgements
We would like to thank all individuals who participated in this study.
Funding
This work was supported by Grants-in-Aid for Scientific Research (C) (19K08081, 21K07497, and 22K07614) and Young Scientists (B) (16K19784) from the Japan Society for the Promotion of Science (JSPS); the AMED (Grant Numbers JP21uk1024002, JP22dk0307112 and JP23dk0307103); a grant from the SENSHIN Medical Research Foundation (N/A); a grant from the Uehara Memorial Foundation (N/A); a grant from the Takeda Science Foundation (N/A); a grant from the YOKOYAMA Foundation for Clinical Pharmacology (YRY-1807); a grant from the Smoking Research Foundation (N/A); a grant from the Mochida Memorial Foundation for Medical and Pharmaceutical Research (N/A); and Dean’s discretionary expenses at Gifu University graduate school and the school of medicine (2021 and 2023).
Open Access funding provided by Gifu University.
Author information
Authors and Affiliations
Contributions
KO supervised the entire project, collected the data, the genotyping, wrote the manuscript and was critically involved in the design, analysis and interpretation of the data. AK and KO were responsible for performing the literature review and data analyses and drafting the manuscript. AK, KO and TS were heavily involved in the collection of the majority of the data and intellectually contributed to data interpretation. All authors contributed to and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
This study was approved by the Research Ethics Committees of Gifu University and Kanazawa Medical University.
Informed consent
Written informed consent was obtained from all participants after the procedures were thoroughly explained.
Competing interests
The authors declare no competing interests.
Conflict of interest
There is no conflict interest for all authors.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kuramitsu, A., Ohi, K. & Shioiri, T. Associations of polygenic risk scores differentiating attention-deficit hyperactivity disorder from autism spectrum disorder with cognitive and cortical alterations in Schizophrenia patients. Eur Child Adolesc Psychiatry (2024). https://doi.org/10.1007/s00787-024-02549-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00787-024-02549-w