Abstract
Abnormal growth hormones and thyroid function may be linked to pathophysiology of attention-deficit/hyperactivity disorder (ADHD). Phthalates and bisphenol-A (BPA), two endocrine-disrupting chemicals (EDCs), may affect the human endocrine system. In this study, we aimed to perform a comprehensive investigation of whether growth hormone, thyroid function, and EDCs exhibited differential levels between ADHD patients and healthy controls. In total, 144 children with ADHD and 70 healthy control subjects were enrolled. Their endocrine systems were evaluated using the serum levels of insulin-like growth factor-1 (IGF-1), IGF-binding protein-3 (IGFBP-3), thyroid-stimulating hormone (TSH), triiodothyronine (T3), thyroxine (T4), and Free T4. The urinary levels of EDCs, including monoethyl phthalate (MEP), mono-methyl phthalate (MMP), monoethylhexyl phthalate (MEHP), mono-n-butyl phthalate (MnBP), monobenzyl phthalate (MBzP), and BPA, were also examined. Patients with ADHD had lower IGF-1 levels than healthy controls (p = 0.003), but we observed no significant difference in IGFBP-3, TSH, T3, T4, or Free T4. Compared to the control group, patients with ADHD demonstrated higher MEHP levels (p = 0.043), MnBP (p = 0.033), and MBzP (p = 0.040). Furthermore, MEHP levels (p < 0.001) and BPA levels (p = 0.041) were negatively correlated with IGF-1 levels, while IGF-1 levels were negatively correlated with principal components consisting of ADHD clinical symptoms and neuropsychological performance variables. We suggest that MEHP exposure may be associated with decreased serum levels of IGF-1 and increased risk of ADHD. The mechanism underlying this association may be important for protecting children from environmental chemicals that adversely affect neurodevelopment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Attention-deficit/hyperactivity disorder (ADHD) is one of the most common psychiatric disorders among school-aged children and adolescents [1]. Meta-analysis studies have indicated that the prevalence rate of ADHD ranges between 5 and 10% [2, 3], and a local study in Taiwan has revealed that the prevalence rates are approximately 10% [4]. Functional impairments in academic, social, and family contexts could sustain across the life span of ADHD patients [5]. Various neurobiological and environmental factors may also play a role in susceptibility to ADHD [6]. Substantial growth problems and delay of brain maturation in children with ADHD have also been observed [7, 8], causing many researchers to examine the role of the endocrine system in ADHD etiology [9, 10].
Growth hormone (GH) induces the generation of insulin-like growth factor-1 (IGF-1) in the liver and regulates the paracrine production of IGF-1 [11]. The IGF system participates in nervous system development and maintenance. In the brain, IGFs exert both paracrine and autocrine actions regulated by IGF-binding proteins and interact with various growth factor signal pathways [12]. Serum IGF-1 and IGF-binding protein (IGFBP)-3 concentration measurements can complement the assessment of GH status [13]. A previous study has indicated that prepubertal children with ADHD had normal serum IGF-I and IGFBP-3 and thyroid functions [14]. Furthermore, no significant association has been found between methylphenidate and growth markers (IGF-1, Free T4, and TSH) among ADHD children [15].
Thyroid status, which is measured using thyroid-stimulating hormone (TSH), T3, T4, and Free T4, has potential implications for the regulation of motor, cognitive, and affective functions [16]. The current literature has indicated a relationship between abnormal thyroid indices and ADHD symptoms in children [17]. Previous studies have shown that high TSH and low free T4 concentrations are associated with ADHD symptoms in healthy preschoolers [18]. However, Kuppili et al. [19] revealed that no significant differences in serum T3 or TSH were observed between ADHD cases and controls. Several studies investigated the association between maternal thyroid function and children's risk of problem behavior, in particular ADHD [20, 21]. Children exposed to the increased maternal TSH or maternal hypothyroxinemia in early pregnancy had more ADHD symptoms [22, 23].
Environmental toxicants can result in epigenetic alterations and neurodevelopmental disorders, including ADHD [6, 24, 25]. Endocrine-disrupting chemicals (EDCs) refer to exogenous substrates that alter endocrine system function and cause adverse health effects [26]. Phthalates, a class of EDCs, are widely applied in the process of various consumer products, and exposure may alter physiological or neurodevelopmental development [27]. Current epidemiological literature has shown various quantitative associations between phthalate exposure and ADHD symptoms among children [28, 29]. Di(2-ethylhexyl) phthalate (DEHP) is the most abundant phthalate in the environment and mono-(2-ethylhexyl) phthalate (MEHP) is its primary metabolite [30]. Other important phthalates include monoethyl phthalate (MEP), mono-methyl phthalate (MMP), mono-n-butyl phthalate (MnBP), monobenzyl phthalate (MBzP). MEHP concentrations have been related to child attention problems, depression, and behavioral problems [31]. Furthermore, urinary MnBP or MBzP levels exhibited positive relationships with social and behavioral abnormalities in children [32,33,34]. Bisphenol A (BPA) is a chemical that is widely used in the production of polycarbonate plastics and epoxy resins [35]. BPA is also suspected of contributing to adverse neurobehavioral outcomes, such as inattention, hyperactivity emotional symptoms, and learning disabilities [36, 37].
EDCs can interfere with the synthesis, metabolism, and actions of hormone systems, and through the action on hormone receptors and their related signaling pathways [38]. One longitudinal cohort study revealed that exposure to phthalate-tainted products could disturb the hemostasis of growth hormone and thyroid function in children [39]. Endogenous hormonal changes easily interact with hypothalamic–pituitary axis (HP axis) function, and EDCs’ exposure can alter proper HP axis function [40]. A study revealed that parabens were adversely associated with maternal thyroid hormone dysfunction and child ADHD [41]. However, a comprehensive investigation of the associations between growth hormones, thyroid function, and EDCs exposure among children with ADHD has not yet been performed.
To clarify potential relationships, we conducted a case–control study to explore whether IGF-1, IGFBP-3, TSH, T3, T4, Free T4, phthalate, and BPA demonstrated differential levels between ADHD patients and healthy controls. We further explored the inter-relationships among the aforementioned hormone indices, EDCs, and clinical measures.
Methods
Study participants
Patients with ADHD were recruited from the outpatient Department of Child Psychiatry at Chang Gung Memorial Hospital in Taiwan. All of the patients’ parents or guardians were requested to sign an informed consent. The inclusion criteria were: (a) the patient must have a clinical diagnosis of ADHD based on the Diagnostic and Statistical Manual of Mental Disorders (DSM–5) [4, 42]; (b) aged between 6 and 12; (c) drug-naïve; and (d) without a history of a co-morbid neurodevelopmental or psychiatric disorder (autism spectrum disorder [ASD], intellectual disabilities, psychotic disorders, bipolar disorder, epilepsy, or brain injury).
Healthy control subjects were defined as: (a) children who were aged between 6 and 12 and without ADHD diagnosis; (b) without a major neurodevelopmental or psychiatric disorder (such as ASD, intellectual disabilities, psychotic disorders, bipolar disorders, major depressive disorders, substance dependence, or severe head trauma). These control subjects were recruited from communities nearby Kaohsiung Chang Gung Memorial Hospital.
Laboratory testing of growth hormones and thyroid function
To measure the serum levels of IGF-1, IGFBP-3, T4, Free T4, T3, and TSH, we collected the blood samples from the participants in the next morning right after they had fasted overnight. IGF-1 levels were determined using a Human IGF-I/IGF-1 Quantikine ELISA Kit (R&D Systems, Minneapolis, MN, USA). The minimum detectable dose of human IGF-1 ranged from 0.007 to 0.056 ng/mL. IGFBP-3 levels were determined using a Human IGFBP-3 Quantikine ELISA Kit (R&D Systems, Minneapolis, MN, USA) with an assay range of 0.8–50 ng/mL. T4 levels were determined using “SIEMENS” Reagents for T4 Assay (Siemens Healthcare Diagnostics, Camberley, UK) with an assay range of 0.3–30 µg/dL (3.9–387 nmol/L). Free T4 levels were determined using an ABBOTT ARCHITECT Free T4 Reagent Kit (Lisnamuck, Longford, Co. Longford, Ireland). The ARCHITECT Free T4 assay was designed to have a Limit of Quantitation (LoQ) of ≤ 0.4 ng/dL. T3 was determined using ABBOTT ARCHITECT Total T3 (Lisnamuck, Longford, Co. Longford, Ireland). TSH levels were determined using the ADVIA Centaur TSH3-Ultra assay (Siemens Healthcare Diagnostics, Camberley, UK) with an assay range from 0.008 to 150 µIU/mL.
Laboratory testing of endocrine-disrupting chemicals
An aliquot (1.0 mL) of urine sample was first enzymatically hydrolyzed and purified using the solid-phase extraction method. Then, the phthalate metabolites in the urine were resolved with reverse-phase ultra-performance liquid chromatography. These metabolites were detected by electrospray ionization tandem mass spectrometry and quantified by the use of an isotope internal standard curve method [43]. Meanwhile, the HPLC-grade ethyl acetate was purchased from Duksan Pure Chemicals and ammonium acetate (97.0% powder) from Merck. Sigma-Aldrich was used for obtain β-Glucuronidase (≥ 85,000 units/mL) from Helix pomatia (Type H-2). The urine samples were fortified with 50 μL of internal standard (200 ng/mL, a mixture of six types of phthalate metabolites-13C12) spiking solution, 1 mL of 2 M ammonium acetate buffer solution (1.54 g of ammonium acetate/10 mL HPLC-grade water), and 20 μL of- β-Glucuronidase. Incubated for 1 h at 37 °C and then extracted twice with 4 mL of ethyl acetate, these urine samples were gently shaken a few times, and a centrifuge set at 4000 rpm for 15 min was used to separate the organic layer from the non-polar fat layer. The chromatographic separation was performed on a Shim-pack GIST C18 column (2.1 mm × 100 mm, 2 μm) from Shimadzu Co. Ltd. Subsequently, Shimadzu 8050 Triple Quad liquid chromatograph mass spectrometer equipped with a Shimadzu LC-30 series HPLC system was used for detecting target compounds. We identified the following six EDCs substrates in this study: MEP, MMP, MEHP, MnBP, MBzP, and BPA.
Clinical measurements
For both ADHD patients and healthy control subjects, the neurocognitive function were conducted by an experienced child psychologist using the Wechsler Intelligence Scale for Children–Fourth Edition (WISC-IV). Visual attention and auditory attention of the subjects were assessed using the Conners’ Continuous Performance Test 3rd Edition (Conners CPT3) and Conners’ Continuous Auditory Test of Attention™ (Conners CATA™), respectively. Behavioral symptoms were evaluated using the Swanson, Nolan, and Pelham Version IV Scale (SNAP-IV) parent form (filled by parents) and the SNAP-IV teacher form (filled by the main classroom teachers), respectively. In addition, patients were additionally interviewed by a clinician using the ADHD Rating Scale (ADHD-RS) [44].
As an individually administered and norm-referenced tool, the WISC-IV is developed to assess intelligence in children aged 6–16 years [45]. It consists of ten core and five supplemental subtests. Four factor indexes were calculated from core subtests: Verbal Comprehension Index (VCI), Perceptual Reasoning Index (PRI), Working Memory Index (WMI), and Processing Speed Index (PSI). Finally, the Full-Scale Intelligence Quotient (FSIQ) is made up of the ten core subtests [45].
The SNAP-IV form to be completed by parents or teachers is a 26-item questionnaire that evaluates ADHD symptoms and severity and needs [46]. The 26 items include nine for inattention symptoms, nine for hyperactivity/impulsivity symptoms, and eight for oppositional defiant disorder symptoms. Each item is scored from 0 to 3 on a Likert scale. Only the core ADHD symptoms (inattention and hyperactivity/impulsivity subscales) were analyzed in this study.
The Conners CPT3, usually carried out in a testing room, is a task-oriented computerized measure of attention-related problems. During the 15–20 min of test time, subjects are required to click the mouse button as quickly as possible whenever any letter, except X, is showing up on the screen. When X appears, the examinee is instructed to refrain from responding to the non-target stimulus. In general, the higher the raw scores, the poorer the performance [47]. The following parameters were used for analysis in this study: Response Style (C), Detectability (d’), Omissions, Commissions, and Hit Reaction Time (HRT).
The Conners CATA™ is a 14-min, 200-trial test to assess auditory processing and attention-related problems. During its administration, high-tone sounds either preceded by a low-tone warning sound (warned trials) or played alone (unwarned trials) are presented to the respondents. This test is used to measure the respondent’s Detectability (d’), Omissions, Commissions, Perseveration, and Hit Reaction Time (HRT) in the dimension of Inattentiveness, Impulsivity, and Sustained Attention [48].
Statistical analysis
In this study, the statistical software package SPSS, version 21.0 (SPSS Inc., Chicago, IL, USA) was applied to analyze the data. Analysis of Moment Structures (AMOS) version 24.0 was used for path analysis through structural equation modeling (SEM). Two-tailed p values of < 0.05 were considered statistically significant.
The independent t test was used to estimate the differential continuous variables between ADHD patients and healthy controls. All the EDCs, growth hormones, and thyroid hormones showed positive skewness, and arithmetic log transformations were used to generate approximate normal distributions for these levels. We used Analysis of Covariance (ANCOVA) to examine differences in EDCs and hormone levels between ADHD patients and control subjects, controlling for age, sex, urine-specific gravity, and creatinine level.
We used PCA followed by a varimax rotation to identify latent components from a multitude of ADHD-related variables (clinical symptoms and neurocognitive assessments). Subsequently, we used Pearson’s correlation to explore the inter-relationships among the EDCs, hormones, and ADHD clinical factors yielded by PCA. Based on the findings that MEHP and BPA were correlated to IGF-1, and IGF-1 was correlated to ADHD clinical features, we decided to further investigate these relationships with structural equation modeling (SEM). We performed path analysis for MEHP to IGF-1 to ADHD, and BPA to IGF-1 to ADHD. The direct and indirect effects, 95% confidence intervals (95% CIs), and significance levels (p values) were evaluated using the bootstrap method with AMOS.
Results
The characteristics of patients with 144 ADHD and 70 healthy controls are summarized in Table 1. Among the patients with ADHD, 34% of them were classified as predominantly inattentive presentation; the remaining 66% patients were classified into combined presentation or predominantly hyperactive/impulsive presentation. No significant differences in age (ADHD: 8.9 years; controls: 9.2 years), sex distribution (ADHD: 76.4% male; controls 65.7% male), height, or weight were observed between the ADHD patients and the controls. The ADHD group demonstrated inferior performance in all indexes of the WISC-IV, compared to the control group. Furthermore, ADHD patients exhibited higher severity in all the clinical ADHD symptom dimensions, including parent-rated, teacher-rated, and clinician-rated inattention scores and hyperactivity/impulsivity scores.
Figure 1 illustrates the serum levels of the growth hormones and thyroid hormones of the two participant groups. Patients with ADHD had lower IGF-1 levels than the healthy controls (141.5 ± 69.5 ng/mL vs. 182.7 ± 100.8 ng/mL, p = 0.003). After controlling for the effects of age and sex (ANCOVA), the differences in IGF-1 levels between ADHD patients and control subjects were still significant (p = 0.003). However, no significant differences in IGFBP-3, T4, Free T4, T3, or TSH were found between the ADHD group and the healthy controls.
Figure 2 displays the urine EDCs levels of the ADHD group and the control group. Compared to the control group, patients with ADHD demonstrated higher MnBP (18.1 ± 17.4 ng/mL vs. 13.6 ± 12.4 ng/mL, p = 0.033), MBzP (0.8 ± 1.7 vs. 0.5 ± 0.6 ng/mL, p = 0.040), and MEHP levels (8.0 ± 10.7 vs. 5.7 ± 5.5 ng/mL, p = 0.043). However, we observed no significant differences regarding MMP, MEP, or BPA between the ADHD and control groups. The geometric mean of each phthalate and BPA are listed in Supplementary Table 1.
Supplementary Table 2 provides the weights for the measures of the six principal components (PC) that yielded eigenvalues exceeding 1.00 and were retained for PCA. We labelled the resulting six PCs based on their component: PC1 was labelled as Clinical Symptoms; increased severity of ADHD behavioral symptom was associated with increased PC1. PC2 was labelled as Intelligence Quotient; increased scores on WISC-IV were associated with increased PC2. PC3 was labelled as Auditory Attention-Impulsivity; increased PC3 was associated with more impulsive performance of the CATA. PC4 was labelled as Visual Attention-Impulsivity; increased PC4 was related to the impulsive performance of the CPT. PC5 was labelled as Visual Attention-Sluggish; increased PC5 represented more inattention-related CPT performance. PC6 was labelled as Auditory Attention-Sluggish; increased PC6 indicated more inattention-related CATA performance.
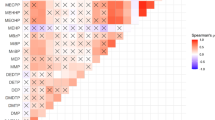
Table 2 summarizes the relationships between EDCs, growth hormones, thyroid function, and ADHD measurements among all participants. We found that MEHP levels (r = − 0.309, p < 0.001) and BPA levels (r = − 0.140, p = 0.041) were negatively correlated with IGF-1 levels. We also found that IGF-1 levels were negatively correlated with clinical symptoms (r = − 0.257, p < 0.01), Auditory Attention-Impulsivity (r = − 0.196, p < 0.01), and Visual Attention-Sluggish (r = − 0.137, p < 0.05).
Figure 3 shows the path diagram of the SEM model including the standardized estimates for the causal paths for MEHP, IGF-1, and ADHD clinical symptoms. Both estimated paths for the indirect effects were statistically significant (path from MEHP to IGF-1 levels: β = − 0.19, p = 0.005; path from IGF-1 to ADHD: β = − 0.25, p < 0.001; indirect effect: 0.05, 95% CI 0.02–0.08, p = 0.008), while the estimate of the direct effect from MEHP levels to ADHD symptoms was non-significant (path from MEHP to ADHD: β = − 0.04, p = 0.582; direct effect: − 0.04, 95% CI − 0.13–0.11, p = 0.656). Therefore, potentially, IGF-1 fully mediates the path between MEHP and ADHD clinical symptoms (the proportion mediated: 0.56). However, no significant mediating effect of IGF-1 between BPA and ADHD was found.
The SEM model for demonstrating the path analysis from MEHP, IGF-1, and ADHD clinical symptoms. The indirect effects were statistically significant (path from MEHP to IGF-1 levels: β = − 0.19, p = 0.005; path from IGF-1 to ADHD: β = − 0.25, p < 0.001; indirect effect: 0.05, 95% CIs 0.02–0.08, p = 0.008), while the direct effect from MEHP levels to ADHD symptoms was non-significant (path from MEHP to ADHD: β = − 0.04, p = 0.582; direct effect: − 0.04, 95% CIs − 0.13–0.11, p = 0.656). a,bThe values of squared multiple correlations. aThe amount of variation explained by MEHP to IGF-1 (R2 = 0.04). bThe amount of variation explained by MEHP and IGF-1 to ADHD (R2 = 0.06)
Discussion
The main findings in this study reveal that patients with ADHD had lower IGF-1 levels than healthy controls, but no significant difference in thyroid function. When compared to the control group, ADHD patients were found to have higher MEHP, MnBP, and MBzP levels. Furthermore, we observed that MEHP plays a crucial role with regard to influencing IGF-1 levels and was further linked to ADHD clinical presentations.
To the best of our knowledge, the results herein are among the first to demonstrate that IGF-1 levels in ADHD patients were significantly lower than those in control subjects, while age and height between the ADHD group and the control group did not differ significantly. Furthermore, our results indicated that IGF-1 levels showed inverse correlation with symptoms’ severity and neuropsychological deficits of ADHD. One possible explanation is that IGF-1 exerts a protective effect against the development of ADHD. However, IGFBP-3 was not associated with ADHD characteristics. Some growth deficits have been observed in children with ADHD [49]. However, a previous study revealed that serum levels of IGF-I and IGFBP-3 were within normal ranges in prepubertal children with ADHD [14]. It is worth noting that the study conducted by Bereket et al. [14] lacked a control group for direct comparison. Notably, IGF-1 is mainly bound to IGFBP-3 and acts predominantly in the proliferation and hypertrophy tissues. Furthermore, differentiation and increase height within columns of cells could be induced, and then calcify the surrounding matrix [13]. IGF-1 also exhibits cell growth stimulation and anti-apoptotic effects. A previous cohort study indicated that IGF-I was associated with intelligence quotient and brain development in childhood [50]. Taken altogether, our results imply that IGF-1 is not only crucial for bone and muscle growth, but also contributes to neurodevelopment and neuropsychological function.
Our results showed no significant difference in thyroid function between ADHD cases and controls. Thyroid status affects brain development grey matter volume and has potential implications with regard to regulating motor, cognitive, and affective functions [16]. However, whether the physical maturity related to thyroid function influences the risk for ADHD remains controversial. One previous study did not observe an association between ADHD and thyroid function [51], which is consistent with the findings in our study. Nonetheless, another study reported a significant positive association between free T3 and continuously assessed ADHD symptoms in children [17]. Among healthy preschoolers, high TSH and low free T4 concentrations are associated with ADHD symptoms [18]. Serum T4 was significantly lower in ADHD cases compared to controls, but no significant differences were found in serum T3, TSH, or cortisol levels [19]. Children with thyroid dysfunction may be more likely to display inattention, cognitive delay, labile mood, or social misbehaviors, as well as have a higher probability to be diagnosed as ADHD. However, whether thyroid function serves as a reliable biomarker of ADHD warrants further investigation.
Our results support that various phthalate compounds (i.e., MEHP, MnBP, and MBzP) may play a role in a susceptibility to ADHD. Compared with urinary levels of phthalate metabolites from Taiwanese school-age children in the previous studies [52,53,54], the measurements in the current study showed comparable values (Supplementary Table 3). Phthalate monoesters may be environmental contaminants on their own and need to be considered in health risk assessments [55]. MnBP, a major metabolite of di-n-butyl phthalate (DBP), is classified as EDCs [56]. MBzP is the major metabolite of butyl benzyl phthalate, and MEHP is most commonly used as a plasticizer and solvent in various consumer products [57]. The finding of higher MnBP values in ADHD was in line with the previous studies’ findings [25, 32, 58]. Consistent with our finding, MEHP concentrations have been previously related to child attention problems and externalizing behaviors [31]. Compelling evidence demonstrates that BPA and its analogues, belonging to endocrine disruptors, contribute to adverse health outcomes [36, 37]. However, the link between ADHD and BPA has been inconsistent among the current literature [35, 37, 59].
The results in this study revealed that MEHP was significantly negatively associated with IGF-1 levels among children. Contradictory to our finding, a previous study found a positive association between MEHP and IGF-1 in adults, but no such association was observed among youths under the age of 18 years [39]. An animal study indicated that maternal MEHP exposure induced apoptosis in cerebellar granule cells via the Phosphatidylinositol-3-kinase (PI3K)-Protein kinase B (Akt) signaling pathway, and the apoptosis could be recovered by IGF-1 [60]. Evidence has revealed that disruptions by EDCs can alter proper HP axis function, leading to disrupt the homeostasis maintenance of endocrine systems [40]. Our study is the first to provide evidence about the mediating effect of IGF-1 between MEHP and ADHD features. We assume that MEHP potentially exerts detrimental effects on IGF-I, and the decreased IGF-1 levels further links to the risk of ADHD.
This study has several limitations which should be noted. First, this study was a case–control, cross-sectional study, and thus, the causal inference of EDCs exposure, hormones secretion, and brain development could not be determined. For example, EDCs’ exposure may be related to dietary habit, lifestyles, education levels, or family socioeconomic status [61]. The association that we identified between EDCs and ADHD may not necessarily indicate that EDCs cause ADHD. Second, the sample size was relatively small in the study. Third, although we found a correlation between EDCs, growth hormones, and ADHD manifestations, the neurobiological mechanism underpinning these correlations remains undetermined. Forth, people with ASD were highly co-morbid with ADHD [62]. Although we excluded patients with ASD based on the criterion of DSM–5, ASD-related questionnaires were not administrated in this study. Finally, multiple comparisons’ corrections were not applied, and thus, the possibility of type I error could not be excluded.
In summary, this study is the first to elucidate the associations between growth hormones, thyroid function, and EDCs with regard to the susceptibility of ADHD. In accordance with our findings, we suggest that patients with ADHD had lower IGF-1 levels than healthy controls, but no significant difference in thyroid function. Compared to the control group, patients with ADHD demonstrated higher MEHP, MnBP, and MBzP levels. Furthermore, MEHP exposure may be associated with decreased serum levels of IGF-1, as well as further linked to the risk of ADHD. These results demonstrate new insight that growth hormones and environmental chemicals’ exposure, particularly MEHP, may be involved in neurodevelopment maturation.
Code availability
Requests for code can be made through the first author of this publication.
References
Posner J, Polanczyk GV, Sonuga-Barke E (2020) Attention-deficit hyperactivity disorder. Lancet 395(10222):450–462
Polanczyk GV, Salum GA, Sugaya LS, Caye A, Rohde LA (2015) Annual research review: a meta-analysis of the worldwide prevalence of mental disorders in children and adolescents. J Child Psychol Psychiatry 56(3):345–365
Thomas R, Sanders S, Doust J, Beller E, Glasziou P (2015) Prevalence of attention-deficit/hyperactivity disorder: a systematic review and meta-analysis. Pediatrics 135(4):e994–e1001
Chen YL, Chen WJ, Lin KC, Shen LJ, Gau SS (2019) Prevalence of DSM-5 mental disorders in a nationally representative sample of children in Taiwan: methodology and main findings. Epidemiol Psychiatr Sci 29:e15
Retz W, Ginsberg Y, Turner D, Barra S, Retz-Junginger P, Larsson H et al (2020) Attention-Deficit/Hyperactivity Disorder (ADHD), antisociality and delinquent behavior over the lifespan. Neurosci Biobehav Rev 120:236–248
Nilsen FM, Tulve NS (2020) A systematic review and meta-analysis examining the inter-relationships between chemical and non-chemical stressors and inherent characteristics in children with ADHD. Environ Res 180:108884
Tenore A, Tenore A (2012) A pathophysiologic approach to growth problems in children with attention-deficit/hyperactivity disorder. Endocrinol Metab Clin North Am 41(4):761–784
Rubia K, Alegria AA, Brinson H (2014) Brain abnormalities in attention-deficit hyperactivity disorder: a review. Rev Neurol 58(Suppl 1):S3-16
Fairchild G (2012) Hypothalamic-pituitary-adrenocortical axis function in attention-deficit hyperactivity disorder. Curr Top Behav Neurosci 9:93–111
Buske-Kirschbaum A, Schmitt J, Plessow F, Romanos M, Weidinger S, Roessner V (2013) Psychoendocrine and psychoneuroimmunological mechanisms in the comorbidity of atopic eczema and attention deficit/hyperactivity disorder. Psychoneuroendocrinology 38(1):12–23
Laron Z (2001) Insulin-like growth factor 1 (IGF-1): a growth hormone. Mol Pathol 54(5):311–316
Lewitt MS, Boyd GW (2019) The role of insulin-like growth factors and insulin-like growth factor-binding proteins in the nervous system. Biochem Insights 12:1–18
Blum WF, Alherbish A, Alsagheir A, El Awwa A, Kaplan W, Koledova E et al (2018) The growth hormone-insulin-like growth factor-I axis in the diagnosis and treatment of growth disorders. Endocr Connect 7(6):R212–R222
Bereket A, Turan S, Karaman MG, Haklar G, Ozbay F, Yazgan MY (2005) Height, weight, IGF-I, IGFBP-3 and thyroid functions in prepubertal children with attention deficit hyperactivity disorder: effect of methylphenidate treatment. Horm Res 63(4):159–164
Kim WJ, Bang YR, Kang JW, Yoo JH, Kim SH, Park JH (2020) Preliminary investigation of association between methylphenidate and serum growth markers in children with attention-deficit/hyperactivity disorder: a cross-sectional case-control study. Soa Chongsonyon Chongsin Uihak 31(3):154–160
Chambers T, Anney R, Taylor PN, Teumer A, Peeters RP, Medici M et al (2020) Effects of thyroid status on regional brain volumes: a diagnostic and genetic imaging study in UK Biobank. J Clin Endocrinol Metab 106(3):688–696
Albrecht D, Ittermann T, Thamm M, Grabe HJ, Bahls M, Volzke H (2020) The association between thyroid function biomarkers and attention deficit hyperactivity disorder. Sci Rep 10(1):18285
Alvarez-Pedrerol M, Ribas-Fito N, Torrent M, Julvez J, Ferrer C, Sunyer J (2007) TSH concentration within the normal range is associated with cognitive function and ADHD symptoms in healthy preschoolers. Clin Endocrinol (Oxf) 66(6):890–898
Kuppili PP, Pattanayak RD, Sagar R, Mehta M, Vivekanandhan S (2017) Thyroid and cortisol hormones in attention deficit hyperactivity disorder: a case-control study. Asian J Psychiatr 28:73–77
Drover SSM, Villanger GD, Aase H, Skogheim TS, Longnecker MP, Zoeller RT et al (2019) Maternal thyroid function during pregnancy or neonatal thyroid function and attention deficit hyperactivity disorder: a systematic review. Epidemiology 30(1):130–144
Ghassabian A, Bongers-Schokking JJ, de Rijke YB, van Mil N, Jaddoe VW, de Muinck Keizer-Schrama SM et al (2012) Maternal thyroid autoimmunity during pregnancy and the risk of attention deficit/hyperactivity problems in children: the Generation R study. Thyroid 22(2):178–186
Pakkila F, Mannisto T, Pouta A, Hartikainen AL, Ruokonen A, Surcel HM et al (2014) The impact of gestational thyroid hormone concentrations on ADHD symptoms of the child. J Clin Endocrinol Metab 99(1):E1-8
Modesto T, Tiemeier H, Peeters RP, Jaddoe VW, Hofman A, Verhulst FC et al (2015) Maternal mild thyroid hormone insufficiency in early pregnancy and attention-deficit/hyperactivity disorder symptoms in children. JAMA Pediatr 169(9):838–845
Tran NQV, Miyake K (2017) Neurodevelopmental disorders and environmental toxicants: epigenetics as an underlying mechanism. Int J Genomics 2017:7526592
Kim JI, Kim JW, Shin I, Kim BN (2021) Interaction of DRD4 methylation and phthalate metabolites affects continuous performance test performance in ADHD. J Atten Disord 25(2):161–170
Braun JM (2017) Early-life exposure to EDCs: role in childhood obesity and neurodevelopment. Nat Rev Endocrinol 13(3):161–173
Radke EG, Braun JM, Nachman RM, Cooper GS (2020) Phthalate exposure and neurodevelopment: a systematic review and meta-analysis of human epidemiological evidence. Environ Int 137:105408
Praveena SM, Munisvaradass R, Masiran R, Rajendran RK, Lin CC, Kumar S (2020) Phthalates exposure and attention-deficit/hyperactivity disorder in children: a systematic review of epidemiological literature. Environ Sci Pollut Res Int 27(36):44757–44770
Shoaff JR, Coull B, Weuve J, Bellinger DC, Calafat AM, Schantz SL et al (2020) Association of exposure to endocrine-disrupting chemicals during adolescence with attention-deficit/hyperactivity disorder-related behaviors. JAMA Netw Open 3(8):e2015041
Sears CG, Braun JM (2020) Phthalate exposure, adolescent health, and the need for primary prevention. Endocrinol Metab Clin North Am 49(4):759–770
Hu D, Wang YX, Chen WJ, Zhang Y, Li HH, Xiong L et al (2017) Associations of phthalates exposure with attention deficits hyperactivity disorder: a case-control study among Chinese children. Environ Pollut 229:375–385
Won EK, Kim Y, Ha M, Burm E, Kim YS, Lim H et al (2016) Association of current phthalate exposure with neurobehavioral development in a national sample. Int J Hyg Environ Health 219(4–5):364–371
Tsai CS, Chou WJ, Lee SY, Lee MJ, Chou MC, Wang LJ (2020) Phthalates, Para-Hydroxybenzoic Acids, Bisphenol-A, and gonadal hormones’ effects on susceptibility to attention-deficit/hyperactivity disorder. Toxics 8(3):57
Ku HY, Tsai TL, Wang PL, Su PH, Sun CW, Wang CJ et al (2020) Prenatal and childhood phthalate exposure and attention deficit hyperactivity disorder traits in child temperament: a 12-year follow-up birth cohort study. Sci Total Environ 699:134053
Mustieles V, D’Cruz SC, Couderq S, Rodriguez-Carrillo A, Fini JB, Hofer T et al (2020) Bisphenol A and its analogues: a comprehensive review to identify and prioritize effect biomarkers for human biomonitoring. Environ Int 144:105811
Arbuckle TE, Davis K, Boylan K, Fisher M, Fu J (2016) Processed data for CHMS 2007–2009: Bisphenol A, phthalates and lead and learning and behavioral problems in Canadian children 6–19 years of age. Data Brief 8:784–802
Jensen TK, Mustieles V, Bleses D, Frederiksen H, Trecca F, Schoeters G et al (2019) Prenatal bisphenol A exposure is associated with language development but not with ADHD-related behavior in toddlers from the Odense Child Cohort. Environ Res 170:398–405
Mughal BB, Fini JB, Demeneix BA (2018) Thyroid-disrupting chemicals and brain development: an update. Endocr Connect 7(4):R160–R186
Huang PC, Chang WH, Wu MT, Chen ML, Wang IJ, Shih SF et al (2020) Characterization of phthalate exposure in relation to serum thyroid and growth hormones, and estimated daily intake levels in children exposed to phthalate-tainted products: a longitudinal cohort study. Environ Pollut 264:114648
Graceli JB, Dettogni RS, Merlo E, Nino O, da Costa CS, Zanol JF et al (2020) The impact of endocrine-disrupting chemical exposure in the mammalian hypothalamic-pituitary axis. Mol Cell Endocrinol 518:110997
Baker BH, Wu H, Laue HE, Boivin A, Gillet V, Langlois MF et al (2020) Methylparaben in meconium and risk of maternal thyroid dysfunction, adverse birth outcomes, and Attention-Deficit Hyperactivity Disorder (ADHD). Environ Int 139:105716
American Psychiatric Association (2013) Diagnostic and statistical manual of mental disorders 5th ed (DSM-5). American Psychiatric Association, Washington, DC, USA
Blount BC, Milgram KE, Silva MJ, Malek NA, Reidy JA, Needham LL et al (2000) Quantitative detection of eight phthalate metabolites in human urine using HPLC-APCI-MS/MS. Anal Chem 72(17):4127–4134
Zhang S, Faries DE, Vowles M, Michelson D (2005) ADHD Rating Scale IV: psychometric properties from a multinational study as a clinician-administered instrument. Int J Methods Psychiatr Res 14(4):186–201
Baron IS (2005) Test review: Wechsler intelligence scale for children-fourth edition (WISC-IV). Child Neuropsychol 11(5):471–475
Bussing R, Fernandez M, Harwood M, Wei H, Garvan CW, Eyberg SM et al (2008) Parent and teacher SNAP-IV ratings of attention deficit hyperactivity disorder symptoms: psychometric properties and normative ratings from a school district sample. Assessment 15(3):317–328
Tu MC, Lo CP, Huang CF, Huang WH, Deng JF, Hsu YH (2018) Visual attention performances and related cerebral microstructural integrity among subjects with subjective cognitive decline and mild cognitive impairment. Front Aging Neurosci 10:268
Rassovsky Y, Alfassi T (2018) Attention improves during physical exercise in individuals with ADHD. Front Psychol 9:2747
Lahti J, Raikkonen K, Kajantie E, Heinonen K, Pesonen AK, Jarvenpaa AL et al (2006) Small body size at birth and behavioural symptoms of ADHD in children aged five to six years. J Child Psychol Psychiatry 47(11):1167–1174
Gunnell D, Miller LL, Rogers I, Holly JM, Team AS (2005) Association of insulin-like growth factor I and insulin-like growth factor-binding protein-3 with intelligence quotient among 8- to 9-year-old children in the Avon Longitudinal Study of Parents and Children. Pediatrics 116(5):e681-686
Elia J, Gulotta C, Rose SR, Marin G, Rapoport JL (1994) Thyroid function and attention-deficit hyperactivity disorder. J Am Acad Child Adolesc Psychiatry 33(2):169–172
Bao J, Zeng XW, Qin XD, Lee YL, Chen X, Jin YH et al (2015) Phthalate metabolites in urine samples from school children in Taipei, Taiwan. Arch Environ Contam Toxicol 69(2):202–207
Huang PC, Tsai CH, Chen CC, Wu MT, Chen ML, Wang SL et al (2017) Intellectual evaluation of children exposed to phthalate-tainted products after the 2011 Taiwan phthalate episode. Environ Res 156:158–166
Huang PC, Tsai CH, Liang WY, Li SS, Pan WH, Chiang HC (2015) Age and gender differences in urinary levels of eleven phthalate metabolites in general Taiwanese population after a dEHP Episode. PLoS ONE 10(7):e0133782
Weiss JM, Gustafsson A, Gerde P, Bergman A, Lindh CH, Krais AM (2018) Daily intake of phthalates, MEHP, and DINCH by ingestion and inhalation. Chemosphere 208:40–49
Meeker JD (2012) Exposure to environmental endocrine disruptors and child development. Arch Pediatr Adolesc Med 166(10):952–958
Reinsberg J, Wegener-Toper P, van der Ven K, van der Ven H, Klingmueller D (2009) Effect of mono-(2-ethylhexyl) phthalate on steroid production of human granulosa cells. Toxicol Appl Pharmacol 239(1):116–123
Kim BN, Cho SC, Kim Y, Shin MS, Yoo HJ, Kim JW et al (2009) Phthalates exposure and attention-deficit/hyperactivity disorder in school-age children. Biol Psychiatry 66(10):958–963
Engel SM, Villanger GD, Nethery RC, Thomsen C, Sakhi AK, Drover SSM et al (2018) Prenatal phthalates, maternal thyroid function, and risk of attention-deficit hyperactivity disorder in the norwegian mother and child cohort. Environ Health Perspect 126(5):057004
Fu Y, Dong J, Wang J, You M, Wei L, Fu H et al (2018) Developmental exposure to Di-(2-ethylhexyl) phthalate induces cerebellar granule cell apoptosis via the PI3K/AKT signaling pathway. Exp Neurobiol 27(6):472–488
Gari M, Koch HM, Palmke C, Jankowska A, Wesolowska E, Hanke W et al (2019) Determinants of phthalate exposure and risk assessment in children from Poland. Environ Int 127:742–753
Antshel KM, Russo N (2019) Autism spectrum disorders and ADHD: overlapping phenomenology, diagnostic issues, and treatment considerations. Curr Psychiatry Rep 21(5):34
Acknowledgements
The authors would like to thank Professor Wei-Tsun Soong for granting us the use of the Chinese version of the K-SADS and Professor Shur-Fen Gau for granting our use of the Chinese version of the SNAP-IV.
Funding
This work was supported by the Chang Gung Memorial Hospital Research Projects (phthalates and BPA screening was funded by CMRPG8K1281; growth hormones and thyroid function assessments were supported by CMRPG8J0361).
Author information
Authors and Affiliations
Contributions
WLJ participated in interpreting data, reviewing references, and drafting the manuscript. YHH, WJC, SYL, and HYC participated in data collection and patient recruitment. CCC and HRC contribute equally to this study, and they participated in protocol development and revised the manuscript. All authors read and approved the final manuscript and contributed to the drafting and revising of the paper.
Corresponding author
Ethics declarations
Conflicts of interest
All authors declare no conflicts of interest.
Ethics approval
This study was approved by the Chang Gung Memorial Hospital review board (IRB No. 201900376A3).
Consent to participate
We obtained a copy of written informed consent from each of all the participants, including 144 patients with ADHD and 70 healthy control subjects.
Consent for publication
All authors consented for publication.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Wang, LJ., Huang, YH., Chou, WJ. et al. Interrelationships among growth hormone, thyroid function, and endocrine-disrupting chemicals on the susceptibility to attention-deficit/hyperactivity disorder. Eur Child Adolesc Psychiatry 32, 1391–1401 (2023). https://doi.org/10.1007/s00787-021-01886-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00787-021-01886-4