Abstract
Current pharmacological approaches have failed to provide complete remission for patients with Attention-Deficit/Hyperactivity Disorder (ADHD). This study aimed to evaluate the efficacy and tolerability of resveratrol (that have been shown to have antioxidative, anti-inflammatory, and anti-apoptotic effects) as an adjunct to methylphenidate in pharmacologic treatment of ADHD. This 8-week, double-blinded, placebo-controlled trial randomized 66 participants to receive either 500 mg/day resveratrol or matched placebo in addition to methylphenidate. ADHD symptoms were evaluated in the patients using the Parent and Teacher versions of ADHD-Rating Scale (ADHD-RS) at three measurement points with time intervals of 4 weeks. Furthermore, the tolerability of the treatment strategies was systematically compared. Repeated measures analysis demonstrated a significant effect for time–treatment interaction on all three subscales of the Parent ADHD-RS during the trial period (total: p = 0.015; inattention: p = 0.032; hyperactivity/impulsivity: p = 0.036). Nevertheless, the effect for time–treatment interaction was not significant for the Teacher version of ADHD-RS (total: F = 0.81, df = 1.33, p = 0.401; inattention: F = 0.57, df = 1.37, p = 0.507; hyperactivity/impulsivity: F = 0.65, df = 1.34, p = 0.466). The frequencies of complications in the treatment groups were similar. Resveratrol administration for a duration of 8 weeks improved characteristic symptoms in patients with ADHD according to their parents. Further investigations containing larger sample sizes, longer supplementation periods, and dose–response evaluations are required to replicate these findings in ADHD children more confidently.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Attention-Deficit/Hyperactivity Disorder (ADHD) is a heterogeneous neurodevelopmental condition characterized by age-inappropriate behaviors including inattention, hyperactivity, and impulsivity maintained for at least 6 months [1]. ADHD is one of the most prevalent psychiatric disorders affecting 3–7% of children and adolescents worldwide [2]. ADHD accounts for a remarkable proportion of familial, psychosocial, and academic problems if untreated. Moreover, it has been realized that 60–80% of childhood onset ADHD persist into adulthood [3].
Currently, pharmacotherapy is considered as the most effective approach for alleviating ADHD symptoms [4]. Pharmacotherapy in ADHD patients comprises administration of stimulant and non-stimulant medications. Particularly, methylphenidate is the most extensively prescribed medication for ADHD patients with generally safe and highly effective properties [5]. Nevertheless, these agents are not always promising as 10–30% of the patients exhibit intolerable adverse events or resistant symptoms [6, 7]. Hence, investigations on novel or complementary treatment strategies seem to be mandatory.
The exact etiology of ADHD is still unclear. However, the primary deficits in either specific regions (the prefrontal cortex, caudate, and cerebellum) or their linking networks in the brain (dopaminergic and noradrenergic systems) have been extensively addressed in ADHD [5]. Moreover, patients with ADHD have been shown to have lower concentrations of brain-derived neurotrophic factor (BDNF) [8]. Recently, there has been a growing concept that oxidative and inflammatory pathways contribute to the mediation of aforementioned pathologies in brain of patients with ADHD [9]. Oxidative mechanisms can easily affect the brain due to its high oxygen consumption and high lipid but relatively low antioxidant concentrations [10].
Resveratrol (3,5,4′-trihydroxystilbene) is a natural stilbenoid polyphenol that can be found in dietary resources such as peanuts, the skin of red grapes, red wine, and berries [11]. Numerous studies have investigated the beneficial effects of resveratrol showing antioxidative, anti-inflammatory, and anti-apoptotic characteristics [12, 13]. Furthermore, resveratrol can easily access the brain through the blood–brain barrier due to its lipophilic structure and exert aforementioned beneficial effects [14]. There is increasing interest regarding the use of nutritional components in treatment of neuropsychiatric disorders due to their multiple neuroprotective effects. The neuroprotective effects of resveratrol in Alzheimer’s, Huntington’s, and Parkinson’s disease have been confirmed [15,16,17]. More recently, the beneficial effects of resveratrol in a variety of neuropsychiatric disorders and their related conditions have also been addressed such as anxiety, depression, sleep disturbance, and fatigue [18,19,20].
We designed this randomized, double-blinded, placebo-controlled trial using the Parent and Teacher versions of ADHD-Rating Scale for eight weeks since no study has evaluated the efficacy and tolerability of resveratrol add-on to methylphenidate in drug-naïve patients with ADHD. The objective of the current study stems from our hypothesis that resveratrol adjunct to methylphenidate improves the ADHD symptoms without exerting significant side effects.
Methods
Trial design and oversight
This study was an 8-week, single-center, randomized, parallel group, double-blind placebo-controlled trial conducted from January 2019 to January 2020 with outpatients of the child and adolescent clinics at the Roozbeh Psychiatric Hospital affiliated with Tehran University of Medical Sciences (TUMS). The trial was in consistence with the Declaration of Helsinki and its consecutive revisions and the protocol was approved by the Institutional Review Board (IRB) of TUMS (IR.TUMS.VCR.REC.1397.502). After a complete explanation of the procedures and purpose of the study, written informed consent was acquired from either patients’ parents or their legal guardian. Patients and their guardian were aware of their freedom to withdraw from the trial without any negative effect on their treatment plan. The trial was registered in the Iranian registry of clinical trials (www.irct.ir; trial identifier with the IRCT database: IRCT20090117001556N115).
Participants
Patients were recruited from drug naïve outpatients aged 6–12 years who met the criteria for the diagnosis of ADHD according to the Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-5) supported by the Kiddie Schedule for Affective Disorders and Schizophrenia (KSADS) and clinical evidence [21]. Children were excluded from the trial if they had any psychiatric comorbidity except for Oppositional Defiant Disorder (ODD). Other exclusion criteria were history or current diagnosis of pervasive developmental disorder; presence of any medical condition such as uncontrolled seizures, cardiac and/or brain abnormalities, and impaired liver function; weight less than 13.5 kg; mental retardation (defined as intelligence quotation below 70); history of allergy to either resveratrol or methylphenidate; use of any medication that might affect the psychiatric condition of the patients in the last 2 weeks; history of drug abuse or dependency in the past 6 months. In particular, resting pulse rate, systolic blood pressure, and liver function test of the eligible participants were defined to be in the normal range.
Intervention
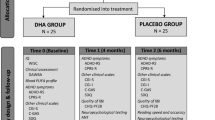
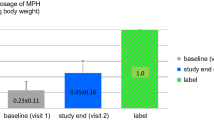
Eligible subjects were randomly assigned to two separate groups receiving 0.3–1.5 mg/kg/day methylphenidate hydrochloride (MPH; Ritalin; Novartis, Switzerland) in two equal doses at 30 min before breakfast and lunch. Methylphenidate was titrated up during the trial according to the following protocol: for the first and second weeks of the trial, 10 mg/day and 20 mg/day of methylphenidate were administered, respectively, followed by a maintenance dose of 20 mg/day from week 3 until the end of the trial. Patients who weighed more than 30 kg received a maintenance dose of 30 mg/day. Resveratrol (ACER, Tehran, Iran; 500 mg/day) was started as an add-on to MPH for one of the groups while the other group received 500 mg/day of starch as placebo. From the first day of trial, both resveratrol and placebo were administered in two separate doses of 250 mg before breakfast and bedtime. Medication adherence was tightly controlled by weekly comparison of tablet counts with parent reports of medication intake.
Outcome
Main ADHD symptoms of the patients were evaluated using the Teacher and Parent versions of ADHD-RS-IV, which have been extensively utilized in school-age children and are considered valid measurement tools for detecting behavioral abnormalities [1, 7, 22]. Guardians and teachers of the patients were interviewed at baseline and weeks 4 and 8 of the trial. Additionally, they were asked to complete the relevant ADHD-RS-IV questionnaire during the interviews. Primary outcome measure was alteration in total scores of the parent and the teacher ADHD-RS-IV from baseline to week 8, while the secondary outcome was defined as the change in subscores of the questionnaires.
Tolerability
All participants underwent complete physical examination, Electrocardiogram (ECG), liver function tests, and complete blood count (CBC) evaluations at the screening session prior to the beginning of the trial. Body weight and vital signs of the subjects were monitored at each visit. Moreover, adverse events were systematically detected throughout the trial using a 25-item checklist of probable side effects by a child psychiatrist at each visit [23,24,25]. Furthermore, participants and their parents were asked to inform the research team in case of any unexpected complication during the trial period.
Randomization, allocation concealment, and blinding
Patients were randomly allocated to treatment groups by a computer-generated random queue (blocks of 4 and an allocation ratio of 1:1). The allocation was carried out using sealed opaque envelopes with an aluminum foil inside to ensure that the contents are not detectable even in intense light. Resveratrol and placebo tablets were completely identical in all their properties including size, shape, color, and smell. The medication distributors, participants and their guardians, research coordinators, and the outcome assessors were all blinded to allocation.
Sample size
A minimal sample size of 56 (28 in each group) was calculated based on the assumption of a clinically significant difference of 4 and a standard deviation of 5 on the Teacher and Parent ADHD-RS according to our previous trials, an attrition rate of 10%, a power of 90%, and a two-tailed significance level of 0.05. In the current trial, we provided a lager sample size (33 patients for each group) to increase the statistical power.
Statistical analysis
All analyses were performed using the Statistical Package of Social Science Software (SPSS version 24; IBM Company), considering a p value level of 0.05 or below as significant. The Shapiro–Wilk test and probability graphs tested normality of the baseline data. Categorical variables were reported in percentage (%), while continuous data were represented as mean ± SD. Baseline data were compared between groups using the independent samples t test with Levene’s test for equality of variance for normally distributed variables and the Mann–Whitney U test for non-parametric conditions. For the general linear model (GLM) repeated measures analysis of ANOVA, the groups and the measurement points were defined as between-subject and within-subject factors, respectively. GLM analysis was used to compare scores of the Parent and Teacher ADHD-RS-IV subscales between the trial groups during the study course. The GLM-related degrees of freedom were corrected by the Greenhouse–Geisser test when the Mauchy’s test of sphericity was significant. Finally, the Fisher’s exact test was conducted to compare frequency of adverse events between groups.
Results
Baseline characteristics of the participants
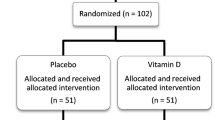
Out of 90 children screened for the trial, 66 patients met the inclusion criteria and were randomized into two arms to receive either methylphenidate + Placebo (n = 33) or methylphenidate + resveratrol (n = 33). 60 participants completed the trial as 3 patients from each group withdrew from the trial before week 4 (Fig. 1). As described in Table 1, all of the baseline characteristics of the subjects were similar between treatment groups (p values > 0.05) (Table 1).
The parent ADHD-RS
The parent ADHD-RS Fig. 2 represents changes in the Parent ADHD-RS subscales during 8 weeks of study. GLM analysis of repeated measures demonstrated that effects of time (Greenhouse–Geisser corrected: F = 550.02, df = 1.50, p < 0.001, partial ɳ2 = 0.91) and time–treatment interaction (F = 5.08, df = 1.50, p = 0.015, partial ɳ2 = 0.08) for the total score were significant showing that the treatment groups differed significantly from each other across the trial period on the total Parent ADHD-RS-IV scores. Similarly, the two-way ANOVA indicated significant effects of time–treatment interaction (hyperactivity/impulsivity: F = 3.99, df = 1.38, p = 0.036, partial ɳ2 = 0.06; inattention: F = 3.88, df = 1.61, p = 0.032, partial ɳ2 = 0.06) for scores of hyperactivity/impulsivity and inattention subscales, proposing that the groups had different behavior in both ADHD symptoms during the study course (Fig. 3) (Table 2).
The teacher ADHD-RS
Repeated measures analysis of ANOVA on total subscale of the Teacher ADHD-RS revealed significant effect for time (Greenhouse–Geisser corrected: F = 29.29, df = 1.33, p < 0.001, partial ɳ2 = 0.34), whereas the effect for time–treatment interaction was not significant (Greenhouse–Geisser corrected: F = 0.81, df = 1.33, p = 0.401, partial ɳ2 = 0.01), indicating that the alterations in the Teacher ADHD-RS total score were similar for both treatment groups. Moreover, the effect of time–treatment interaction for the inattention and hyperactivity/impulsivity subscales represented similar behaviors (inattention: F = 0.57, df = 1.37, p = 0.507, partial ɳ2 = 0.01; hyperactivity/impulsivity: F = 0.65, df = 1.34, p = 0.466, partial ɳ2 = 0.01).
Adverse events
According to the independent samples t test, subjects of the resveratrol group had a statistically similar body weight as the placebo group [mean difference (confidence interval) = 1.63 (− 1.56 to 4.83), F = 2.54, t (58) = 1.02, p = 0.311]. As listed in Table 3, different types of side effects with mild to moderate severity were identified during the trial. The most common complications in both groups were decreased appetite (Resveratrol: 20%; Placebo: 26.7%) and headache (Resveratrol: 16.6%; Placebo: 23.3%). The Fisher exact test analysis demonstrated no significant difference between frequencies of detected side effects in the groups (p values > 0.05) (Table 3).
Discussion
In the current study, we have demonstrated that adding resveratrol to methylphenidate as an adjuvant medication is beneficial and well tolerated in patients with ADHD. Patients treated with resveratrol had significantly improved symptoms according to the parent ADHD-RS total score, inattention and hyperactivity/impulsivity subscores (p = 0.015, 0.032 and 0.036, respectively). However, observed improvements in the Teacher ADHD-RS were not significantly different between the two groups probably due to overcrowded classrooms (with up to 35 students in a class), and therefore lack of enough time for teachers to detect changes in each student’s behavior. Moreover, both treatment options were well tolerated, safe, and similar regarding the observed side effects. Since patients were assigned to the treatment arms randomly and baseline characteristics were not significantly different, the improved ADHD symptoms can be attributed to the beneficial effects of resveratrol.
It has been shown that in patients with ADHD, the cerebellum, caudate, and prefrontal cortex are the most affected areas [26]. These regions are believed to be associated with controlling behavior, attention, and thought processes [26]. Dopamine and noradrenaline are the two main neurotransmitters involved in these networks [5]. The most common treatments for ADHD are stimulants such as amphetamines and methylphenidates besides non-stimulant agents such as clonidine and atomoxetine [5, 27]. These drugs increase the extracellular level of dopamine and noradrenaline via several mechanisms such as acting on the transporters and inhibiting the reuptake of the mentioned neurotransmitters, acting on presynaptic and postsynaptic receptors, provoking direct release of presynaptic neurotransmitters, and inhibiting monoamine oxidase (MAO). Although these medications are widely used, they can be accompanied with various side effects. Besides, long-term effects of these drugs on patients’ social and occupational functioning can be debated [28, 29]. Therefore, there has been tremendous effort to find adjuvant therapies affecting other pathways in order to add to the effectiveness of conventional treatments.
There has been a trend in psychiatry to evaluate the immune-mediated pathways such as oxidative stress (OS) in the pathophysiology of diseases. For instance, analyzing data from 23 studies has revealed that depression has a well-established association with elevated oxidative stress and lower antioxidant levels [30]. This association was also observed in bipolar patients, in which a higher level of nitric oxide, DNA/RNA damage and lipid peroxidation were reported compared to healthy individuals [31]. In this regard, studies have proposed a role of OS in the etiology of ADHD. A meta-analysis by Joseph and colleagues has suggested that patients with ADHD have normal levels of antioxidants; however, they are faced with oxidative damage due to their insufficient response to OS [32]. On this subject, it has been shown that omega-3 levels are lower in ADHD patients compared to healthy controls and its dietary supplements can result in modest improvements in these patients [33]. Zinc was also proposed as supplementary medication in patients with ADHD [22]. Although the evidence on the efficacy of the two aforementioned supplementation is not convincing and needs further attention, other anti-inflammatory and antioxidant dietary supplementations should also be evaluated for their beneficial effects on ADHD symptoms.
Resveratrol (3,4′,5-trihydroxystilbene) is a phytoalexin that is found in various plants including grapes, berries, and peanuts [34]. It is known to act as an antioxidant agent giving rise to neuroprotective and anti-inflammatory effects [35]. Therefore, it has attracted a lot of research attention especially in diseases concerning the nervous system and inflammation. It has been shown that resveratrol modulates the activity of SIRT1, PCG-1α, and AMPK, which are involved in the initiation of neurologic disorders [34]. In this regard, caloric restriction could postpone the onset of these diseases and resveratrol can mimic the effects of caloric restriction by increasing the activity of deacetylases sirtuins, mostly SIRT1 [36, 37]. Moreover, AD patients treated with resveratrol have been shown to have decreased activity of matrix metalloproteinase-9 (MMP-9), which is associated with pathologic extracellular matrix degeneration observed in AD [38]. Besides, it has been indicated that resveratrol is able to regulate the impaired autophagy that is present in AD [39]. Although we have not evaluated the molecular pathways of resveratrol in the current study, some of the shared mechanisms could justify the effectiveness of resveratrol as an adjuvant therapy in ADHD patients.
Other than the mentioned deficits observed in patients with ADHD, it has been shown that brain-derived neurotrophic factor (BDNF) is lower in these patients [8]. BDNF has been identified to be critical for synaptic plasticity, neuroprotection, and important tasks such as memory and learning [40]. It has been shown that OS might significantly alter the level of BDNF and subsequently cause brain damage [41]. In this regard, animal studies have suggested that treatment with resveratrol could up-regulate BDNF levels [42], which might be one of the mechanisms responsible for the observed results of our study. On another note, dopamine is the key affected neurotransmitter in ADHD patients [43]. Avshalumov and colleagues indicated that increased hydrogen peroxide level is associated with suppressed dopamine release in the striatum [44]. Furthermore, excess OS is involved in dopaminergic neuron degeneration [45] and modulates dopamine receptor function [46]. Although the exact link between OS and pathologic changes in ADHD patients is not fully understood yet, restricting these changes by administrating antioxidant agents such as resveratrol might be beneficial in patients.
Although this study has several advantages such as having a double-blinded and placebo-controlled design, rigorous adjustment for baseline variables and novelty, some limitations should be considered to prevent overgeneralization of the findings. First, molecular biomarkers and neurotransmitters were not investigated in our study. Second, our follow-up period was not extensive. Third, larger sample size seems necessary to provide a better insight into the extent of improvement in ADHD symptoms following resveratrol adjunctive therapy. Moreover, evaluating Teacher ADHD-RS in classrooms with fewer students would probably yield more reliable results in this regard. Fourth, a diverse nutritional status of the patients might have affected the findings of this study. Finally, cognitive assessment of attention in ADHD children and adolescents could provide better insight into this condition. Hence, results of this trial must be considered as preliminary.
In conclusion, the current study provides evidence supporting a beneficial and safe role for the administration of resveratrol as an adjuvant therapy in management of patients with ADHD. Future studies with larger sample sizes and longer follow-up periods could confirm these observations and possibly shed light on the underlying pathways.
References
Dehbozorghi S, Bagheri S, Moradi K, Shokraee K, Mohammadi MR, Akhondzadeh S (2019) Efficacy and safety of tipepidine as adjunctive therapy in children with attention-deficit/hyperactivity disorder: randomized, double-blind, placebo-controlled clinical trial. Psychiatry Clin Neurosci 73:690–696. https://doi.org/10.1111/pcn.12913
Rowland AS, Skipper BJ, Umbach DM, Rabiner DL, Campbell RA, Naftel AJ, Sandler DP (2015) The prevalence of ADHD in a population-based sample. J Atten Disord 19:741–754. https://doi.org/10.1177/1087054713513799
Castells X, Blanco-Silvente L, Cunill R (2018) Amphetamines for attention deficit hyperactivity disorder (ADHD) in adults. Cochrane Database Syst Rev 8:Cd007813. https://doi.org/10.1002/14651858.CD007813.pub3
Curatolo P, Paloscia C, D'Agati E, Moavero R, Pasini A (2009) The neurobiology of attention deficit/hyperactivity disorder. Eur J Paediatr Neurol 13:299–304. https://doi.org/10.1016/j.ejpn.2008.06.003
Sharma A, Couture J (2014) A review of the pathophysiology, etiology, and treatment of attention-deficit hyperactivity disorder (ADHD). Ann Pharmacother 48:209–225. https://doi.org/10.1177/1060028013510699
Steele M, Jensen PS, Quinn DM (2006) Remission versus response as the goal of therapy in ADHD: a new standard for the field? Clin Ther 28:1892–1908. https://doi.org/10.1016/j.clinthera.2006.11.006
Ghajar A, Aghajan-Nashtaei F, Afarideh M, Mohammadi MR, Akhondzadeh S (2018) l-Carnosine as adjunctive therapy in children and adolescents with attention-deficit/hyperactivity disorder: a randomized, double-blind, placebo-controlled clinical trial. J Child Adolesc Psychopharmacol 28:331–338. https://doi.org/10.1089/cap.2017.0157
Liu DY, Shen XM, Yuan FF, Guo OY, Zhong Y, Chen JG, Zhu LQ, Wu J (2015) The physiology of BDNF and its relationship with ADHD. Mol Neurobiol 52:1467–1476. https://doi.org/10.1007/s12035-014-8956-6
Lopresti AL (2015) Oxidative and nitrosative stress in ADHD: possible causes and the potential of antioxidant-targeted therapies. Atten Defic Hyperact Disord 7:237–247. https://doi.org/10.1007/s12402-015-0170-5
Ikonomidou C, Kaindl AM (2011) Neuronal death and oxidative stress in the developing brain. Antioxid Redox Signal 14:1535–1550. https://doi.org/10.1089/ars.2010.3581
Salehi B, Mishra AP, Nigam M, Sener B, Kilic M, Sharifi-Rad M, Fokou PVT, Martins N, Sharifi-Rad J (2018) Resveratrol: a double-edged sword in health benefits. Biomedicines 6:91. https://doi.org/10.3390/biomedicines6030091
Kanthasamy K, Gordon R, Jin H, Anantharam V, Ali S, Kanthasamy AG, Kanthasamy A (2011) Neuroprotective effect of resveratrol against methamphetamine-induced dopaminergic apoptotic cell death in a cell culture model of neurotoxicity. Curr Neuropharmacol 9:49–53. https://doi.org/10.2174/157015911795017353
Pacheco M, Frozza R, Bernardi A (2018) Anti-inflammatory effects of resveratrol: mechanistic insights. Int J Mol Sci 2018:19
Bastianetto S, Ménard C, Quirion R (2015) Neuroprotective action of resveratrol. Biochim Biophys Acta (BBA) Mol Basis Dis 1852:1195–1201. https://doi.org/10.1016/j.bbadis.2014.09.011
Pasinetti GM, Wang J, Ho L, Zhao W, Dubner L (2015) Roles of resveratrol and other grape-derived polyphenols in Alzheimer's disease prevention and treatment. Biochem Biophys Acta 1852:1202–1208. https://doi.org/10.1016/j.bbadis.2014.10.006
Rege SD, Kumar S, Wilson DN, Tamura L, Geetha T, Mathews ST, Huggins KW, Broderick TL, Babu JR (2013) Resveratrol protects the brain of obese mice from oxidative damage. Oxid Med Cell Longev 2013:419092. https://doi.org/10.1155/2013/419092
Pasinetti GM, Wang J, Ho L, Zhao W, Dubner L (2015) Roles of resveratrol and other grape-derived polyphenols in Alzheimer's disease prevention and treatment. Biochim Biophys Acta 1852:1202–1208. https://doi.org/10.1016/j.bbadis.2014.10.006
Moore A, Beidler J, Hong MY (2018) Resveratrol and depression in animal models: a systematic review of the biological mechanisms. Molecules. https://doi.org/10.3390/molecules23092197
Wightman EL, Haskell-Ramsay CF, Reay JL, Williamson G, Dew T, Zhang W, Kennedy DO (2015) The effects of chronic trans-resveratrol supplementation on aspects of cognitive function, mood, sleep, health and cerebral blood flow in healthy, young humans. Br J Nutr 114:1427–1437. https://doi.org/10.1017/s0007114515003037
Ge JF, Xu YY, Qin G, Cheng JQ, Chen FH (2016) Resveratrol ameliorates the anxiety- and depression-like behavior of subclinical hypothyroidism rat: possible involvement of the HPT axis, HPA axis, and Wnt/beta-catenin pathway. Front Endocrinol (Lausanne) 7:44. https://doi.org/10.3389/fendo.2016.00044
Ghanizadeh A, Mohammadi MR, Yazdanshenas A (2006) Psychometric properties of the Farsi translation of the kiddie schedule for affective disorders and schizophrenia-present and lifetime version. BMC Psychiatry 6:10. https://doi.org/10.1186/1471-244x-6-10
Akhondzadeh S, Mohammadi MR, Khademi M (2004) Zinc sulfate as an adjunct to methylphenidate for the treatment of attention deficit hyperactivity disorder in children: a double blind and randomized trial [ISRCTN64132371]. BMC Psychiatry 4:9. https://doi.org/10.1186/1471-244x-4-9
Farokhnia M, Shafiee Sabet M, Iranpour N, Gougol A, Yekehtaz H, Alimardani R, Farsad F, Kamalipour M, Akhondzadeh S (2014) Comparing the efficacy and safety of Crocus sativus L. with memantine in patients with moderate to severe Alzheimer's disease: a double-blind randomized clinical trial. Hum Psychopharmacol 29(4):351–359. https://doi.org/10.1002/hup.2412
Kashani L, Omidvar T, Farazmand B, Modabbernia A, Ramzanzadeh F, Tehraninejad ES, Ashrafi M, Tabrizi M, Akhondzadeh S (2013) Does pioglitazone improve depression through insulin-sensitization? Results of a randomized double-blind metformin-controlled trial in patients with polycystic ovarian syndrome and comorbid depression. Psychoneuroendocrinology 38(6):767–776. https://doi.org/10.1016/j.psyneuen.2012.08.010
Malek M, Ashraf-Ganjouei A, Moradi K, Bagheri S, Mohammadi M-R, Akhondzadeh S (2020) Prednisolone as adjunctive treatment to risperidone in children with regressive type of autism spectrum disorder: a randomized, placebo-controlled trial. Clin Neuropharmacol 43:39–45
Seidman LJ, Valera EM, Makris N (2005) Structural brain imaging of attention-deficit/hyperactivity disorder. Biol Psychiat 57:1263–1272
Castle L, Aubert RE, Verbrugge RR, Khalid M, Epstein RS (2007) Trends in medication treatment for ADHD. J Attent Disord 10:335–342
Huang Y-S, Tsai M-H (2011) Long-term outcomes with medications for attention-deficit hyperactivity disorder. CNS Drugs 25:539–554
Santosh PJ, Sattar S, Canagaratnam M (2011) Efficacy and tolerability of pharmacotherapies for attention-deficit hyperactivity disorder in adults. CNS Drugs 25:737–763
Palta P, Samuel LJ, Miller ER III, Szanton SL (2014) Depression and oxidative stress: results from a meta-analysis of observational studies. Psychosom Med 76:12
Brown NC, Andreazza AC, Young LT (2014) An updated meta-analysis of oxidative stress markers in bipolar disorder. Psychiatry Res 218:61–68
Joseph N, Zhang-James Y, Perl A, Faraone SV (2015) Oxidative stress and ADHD: a meta-analysis. J Attent Disord 19:915–924
Hawkey E, Nigg JT (2014) Omega-3 fatty acid and ADHD: Blood level analysis and meta-analytic extension of supplementation trials. Clin Psychol Rev 34:496–505
Frémont L (2000) Biological effects of resveratrol. Life Sci 66:663–673
Dasgupta B, Milbrandt J (2007) Resveratrol stimulates AMP kinase activity in neurons. Proc Natl Acad Sci 104:7217–7222
Chung S, Yao H, Caito S, Hwang J-w, Arunachalam G, Rahman I (2010) Regulation of SIRT1 in cellular functions: role of polyphenols. Arch Biochem Biophys 501:79–90
Pasinetti GM, Wang J, Ho L, Zhao W, Dubner L (2015) Roles of resveratrol and other grape-derived polyphenols in Alzheimer's disease prevention and treatment. Biochim Biophys Acta (BBA)-Mol Basis Dis 1852:1202–1208
Turner RS, Thomas RG, Craft S, van Dyck CH, Mintzer J, Reynolds BA, Brewer JB, Rissman RA, Raman R, Aisen PS (2015) A randomized, double-blind, placebo-controlled trial of resveratrol for Alzheimer disease. Neurology 85:1383–1391
Kou X, Chen N (2017) Resveratrol as a natural autophagy regulator for prevention and treatment of Alzheimer’s disease. Nutrients 9:927
Leal G, Afonso PM, Salazar IL, Duarte CB (2015) Regulation of hippocampal synaptic plasticity by BDNF. Brain Res 1621:82–101
Jain S, Banerjee BD, Ahmed RS, Arora VK, Mediratta PK (2013) Possible role of oxidative stress and brain derived neurotrophic factor in triazophos induced cognitive impairment in rats. Neurochem Res 38:2136–2147
Wang X, Xie Y, Zhang T, Bo S, Bai X, Liu H, Li T, Liu S, Zhou Y, Cong X (2016) Resveratrol reverses chronic restraint stress-induced depression-like behaviour: involvement of BDNF level, ERK phosphorylation and expression of Bcl-2 and Bax in rats. Brain Res Bull 125:134–143
Swanson JM, Flodman P, Kennedy J, Spence MA, Moyzis R, Schuck S, Murias M, Moriarity J, Barr C, Smith M (2000) Dopamine genes and ADHD. Neurosci Biobehav Rev 24:21–25
Avshalumov MV, Chen BT, Koós T, Tepper JM, Rice ME (2005) Endogenous hydrogen peroxide regulates the excitability of midbrain dopamine neurons via ATP-sensitive potassium channels. J Neurosci 25:4222–4231
Tsang AH, Chung KK (2009) Oxidative and nitrosative stress in Parkinson's disease. Biochim Biophysica Acta (BBA)-Mol Basis Dis 1792:643–650
Sankhwar ML, Yadav RS, Shukla RK, Singh D, Ansari RW, Pant AB, Parmar D, Khanna VK (2016) Monocrotophos induced oxidative stress and alterations in brain dopamine and serotonin receptors in young rats. Toxicol Ind Health 32:422–436
Acknowledgements
This study was the postgraduate thesis of Dr Maryam Rafeiy-Torghabeh under the supervision of Prof. Shahin Akhondzadeh for the Iranian Board of Psychiatry. This study was supported by a grant from Tehran University of Medical Sciences to Prof. Shahin Akhondzadeh (Grant no. 38897). The funding organization had no role in the design and conduct of the study; in the collection, analysis, and interpretation of the data; or in the preparation, review, or approval of the article and the decision to submit the article for publication.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflict of interest to disclose.
Rights and permissions
About this article
Cite this article
Rafeiy-Torghabeh, M., Ashraf-Ganjouei, A., Moradi, K. et al. Resveratrol adjunct to methylphenidate improves symptoms of attention-deficit/hyperactivity disorder: a randomized, double-blinded, placebo-controlled clinical trial. Eur Child Adolesc Psychiatry 30, 799–807 (2021). https://doi.org/10.1007/s00787-020-01562-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00787-020-01562-z