Abstract
Deficits in emotion regulation (ER) are an important factor in maintaining social anxiety disorder (SAD) in adults. As SAD and ER problems typically develop during childhood and adolescence, and are maintained dynamically within the parent–child dyad, research on families can help to reveal the role ER plays in the early development of SAD. The current study assessed self-reported habitual ER in dyads of children with SAD (n = 31), children with mixed anxiety disorders (MAD; n = 41) and healthy control children (HC; n = 36), and their parents. Results indicate a transdiagnostic quality of ER in that, children with SAD and children with MAD similarly reported less adaptive and more maladaptive ER strategies than HC children, whereas no group differences in parental ER strategies emerged. Furthermore, children’s ER strategies aggressive action, withdrawal and self-devaluation and the parental ER strategy reappraisal were associated with social anxiety symptoms. These results suggest that there may be deficits in ER which generalize across childhood anxiety disorders. Our results are discussed in relation to current theories and their implications for treatment of childhood SAD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Social anxiety disorder (SAD) is one of the most common mental disorders in children and adolescents, and is associated with significant psychosocial impairments [7]. In considering the prevalence of SAD, effective treatment programs for children with SAD are highly relevant. Current treatment programs for SAD could be improved by better understanding the mechanisms involved in the development and maintenance of childhood SAD. Emotion regulation (ER) is one mechanism found to play a role in the development and maintenance of anxiety disorders in children [43]. However, little is known specifically about how children with SAD regulate their emotions or if they differ from children with other anxiety disorders. Another important question that should be addressed, when examining ER in children, is how their parents regulate their emotions, since ER in children and parents is closely related [22]. Focusing on these research questions, the current study assessed ER in children with SAD and their parents, in comparison to both a healthy control group (HC) and a clinical control group with mixed anxiety disorders (MAD).
ER in children’s social anxiety
ER has been defined in many different ways, making comparisons between different studies challenging [16]. In our study, we use a rather broad definition of ER by Gross [25]: ER is defined as a set of behavioral and cognitive strategies influencing “which emotions one has, when one has them, and how one experiences or expresses these emotions” [25]. The ability to regulate emotions starts in infancy and develops continuously throughout the lifespan [16]. Infants’ and young children’s ER is considerably influenced by direct family (e.g. a parent soothing their child [44], while older children rely less on their parents and more on peer influences [44]). When children enter elementary school, children’s ER becomes more differentiated and children develop better skills for using particularly cognitive ER strategies [36, 44].
While numerous studies have investigated ER and its association with psychopathology in adults (see [3] for a meta-analytic review), research on ER in childhood SAD is scarce. The few existing studies on clinical or subclinical samples have found that, compared to low socially anxious children, socially anxious children report more frequent use of maladaptive ER strategies (e.g. rumination) and less frequent use of adaptive ER strategies (e.g. acceptance [4, 27, 30, 39,40,41]). Consequently, researchers have proposed that maladaptive ER in children may be an important maintaining factor in childhood SAD [4]. Interestingly, ER deficits do not seem to be a unique characteristic of childhood SAD. In fact, ER deficits in children have been found not only in SAD, but also in other anxiety disorders such as generalized anxiety disorder or separation anxiety disorder [43]. This has led to the idea that ER deficits represent a transdiagnostic phenomenon cutting across multiple anxiety disorders.
The transdiagnostic quality of maladaptive ER
Anxiety disorders are highly comorbid among children [8] and symptoms overlap considerably. Researchers have proposed that this might be explained by shared biological, genetic and psychosocial factors which are also influencing children’s ER [37]. Surprisingly, there are only a few theoretical models explaining how ER is involved in the aetiology and maintenance of childhood anxiety (e.g. [12, 46]). For example, Weems [46] suggested a transdiagnostic view, with dysregulated anxiety as a core primary feature of childhood anxiety disorders.
On the empirical side, to date, only a few studies have investigated the transdiagnostic quality of ER in childhood anxiety, but the corresponding findings have been rather inconsistent: for example, adolescents aged 12–16 years with SAD reported less frequent use of rumination compared to adolescents with generalized anxiety disorder [32]. In contrast to this finding, no differences could be found in ER strategy use between different anxiety disorders in a younger sample of children aged 9–11 years [31]. Hence, from the existing studies, it remains unclear as to which ER deficits are disorder-specific to childhood SAD and which represent a transdiagnostic phenomenon of childhood anxiety in general.
The role of parental ER
Theoretical models propose that both anxiety symptoms and maladaptive ER strategies typically co-occur and are maintained dynamically in parents and children (e.g. [22]. These models describe the complex interaction of different familial and child factors as having reciprocal influences, meaning that parent’s maladaptive ER may negatively affect children’s anxiety symptoms and vice versa. While these associations have been outlined theoretically, only a few studies have examined the relationship between parental and child ER in childhood internalizing problems like anxiety and depression (Buckholdt et al. [10]). Specific research on childhood SAD is even more scarce: Asbrand et al. [4] found that both children with SAD and their mothers reported more maladaptive ER strategies than healthy control (HC) children and their mothers. Furthermore, maladaptive maternal ER was associated with adaptive child ER moderated by children’s age: in younger children, more maternal maladaptive ER was related to more child adaptive ER, whereas in older children, an inverse relationship was found. However, as the authors stated, they did not use a validated instrument for maternal ER and included no clinical control group. Therefore, the validity and specificity of this result for childhood SAD are uncertain.
The present study
In sum, only a few studies have investigated ER in childhood SAD, and have provided mixed results. Further, the existing studies suffer from several limitations, making specific conclusions about ER in childhood SAD difficult. First, only a few studies have investigated children with a clinical diagnosis of SAD; rather, they have frequently employed subclinical samples [27, 40, 41], and it remains uncertain if these findings apply to clinical groups. Second, some studies [4, 30] did not include a clinical control group, and therefore, the specificity of the results for SAD is uncertain. Also, only one study [4] has assessed primary caregivers and their ER in a clinical sample. Therefore, important information about interrelations between child and parental ER and the dynamics of ER deficits in families of children with SAD is lacking.
Taking previous findings as a starting point and addressing these limitations, the current study aimed to investigate ER in a sample of children with SAD, a clinical control group with MAD (separation anxiety disorder, general anxiety disorder, specific phobia), and healthy controls (HC). Further, we assessed parents’ habitual ER and its relationship with children’s social anxiety and mixed anxiety symptoms. We hypothesized: (a) children with SAD and MAD and their parents would report more maladaptive and fewer adaptive ER strategies than HC children and their parents [4], and (b) both child and parental self-reported ER strategies would relate to children’s social anxiety and mixed anxiety symptoms [22]. As previous research has provided mixed results in terms of differences and similarities in ER in children with SAD and children with MAD [31, 32], no specific hypotheses were proposed regarding group differences between the two clinical groups.
Method
Recruitment and procedure
Diagnostic status of eligible children aged 10–13 years was assessed by trained PhD or graduate students using a modified version of the Anxiety Disorders Interview Schedule for Children (Kinder-DIPS [42]). This measure is intended to assess both the parent’s and the child’s point of view in separate interviews. Reliability and validity were confirmed [38]. All diagnostic sessions were videotaped and supervised by a licensed clinical psychologist. Ethical approval for this study was obtained from the local ethics committee. Inclusion criterion for the SAD group was SAD as a primary diagnosis (n = 31), whereas the HC children (n = 36) did not meet criteria for any lifetime mental disorder. Children in the MAD clinical control group met DSM-5 criteria for separation anxiety disorder (n = 8), specific phobia (n = 15) or generalized anxiety disorder (n = 18) as a primary diagnosis. Exclusion criteria were either current or past psychotic episodes, severe major depression or pervasive developmental disorders.
Sample characteristics are presented in Table 1.
Instruments and materials
ER child and mother
The German questionnaire Fragebogen zur Erhebung der Emotions regulation bei Kindern und Jugendlichen (FEEL-KJ [24]) was used for children and the corresponding adult version, the Fragebogen zur Erhebung der Emotions regulation bei Erwachsenen (FEEL-E [23]), was used for parents. These self-report questionnaires measure ER strategies in response to anxiety, sadness, and anger. Each strategy was assessed by two items, while frequency of strategy’s habitual use was rated on a 1 (almost never) to 5 (almost always) scale. In the current study, only the anxiety scale was used. Items were grouped into child adaptive (problem-oriented action, cheering up, distraction, acceptance, cognitive problem solving, forgetting, reappraisal), child maladaptive (withdrawal, self-degradation, resigning, perseveration, aggression), parent adaptive (problem-oriented action, cheering up, acceptance, cognitive problem solving, forgetting, reappraisal) and parent maladaptive strategies (withdrawal, self-degradation, resigning, rumination, catastrophizing, assignment of guilt to others). Both parent and child versions show acceptable psychometric properties (α = 0.61–0.91) and good retest reliability (after 8 months: 0.61 ≤ rtt ≤ 0.78 [23]; after 6 weeks: 0.62 ≤ rtt ≤ 0.81 [24]). Internal consistencies of the individual subscales range from α = 0.69 to 0.88, for the child version, and from α = 0.73 to 0.89, for the parent version.
Social anxiety child
Social anxiety symptoms were assessed using the German version of the Social Anxiety Scale for Children-Revised (SASC-RD [35]). Children responded to all items on a 1 (not at all) to 5 (all of the time) scale. Items were grouped in two subscales: Fear of Negative Evaluation subscale (FNE; 8 items) and Social Avoidance and Distress (SAD; 10 items).The German version of the SASC-R shows satisfactory retest reliability (after 2 weeks: 0.74 ≤ rtt ≤ 0.84) and internal consistency (α = 0.63–0.83 [35]). Internal consistency for the entire scale in the present sample was excellent (α = 0.93).
Mixed anxiety symptoms child
Mixed anxiety symptoms were assessed using the German version of the revised Fear Survey Schedule for Children (FSSCR [17]), which measures phobic fears in children. The questionnaire consists of 98 items grouped into seven scales (social fears, fear of school, fear of animals, fear of separation, medical fears, fear of danger and death, fear of scary things). Children were required to rate their level of fear regarding 96 situations or objects on a 0 (not at all) to 2 (often) scale. The FSSCR has been shown to have good validity and reliability [17] and showed excellent internal consistency in the current sample (α = 0.96).
Overall psychopathology child
The German version of the Child Behavior Checklist (CBCL [18]) was administered to parents to measure emotional and behavioral problems in children and adolescents, in both internalizing and externalizing domains. The inventory consists of 100 items asking parents to rate the frequency of each child behavior on a three-point scale (0 = not true to 2 = very true or often true). The CBCL has shown good levels of internal consistency, test–retest reliability and acceptable convergent validity (e.g., [1]). Internal consistency in the current sample was excellent (α = 0.94–0.89).
Overall psychopathology parent
The Brief Symptom Inventory (BSI [20]) is a self-report screening questionnaire to measure psychopathology in adults. The inventory consists of 53 items which measure nine symptom dimensions (somatization, depression, anxiety, etc.). Parents endorse the relevance of each item to their experience in the past 7 days on a 5-point scale, from 0 (not at all) to 4 (extremely). In addition to the nine symptom dimensions, the Global Severity Index (GSI), an indicator of the current overall level of distress, was assessed. Internal consistency in the current sample was excellent at α = 0.93.
Statistical analyses
To avoid spurious findings as a result of multiple testing and to reduce the risk of alpha inflation, the following statistical approach was used. First, to assess group differences in single ER strategies, two separate MANOVAs with group (HC, MAD, SAD) as the independent variable and single ER strategies as dependent variables were conducted for children and parents. Post hoc Tukey tests, which are robust to alpha inflation [34], were used for pairwise comparisons between the groups.
Second, to assess associations between parental and child use of ER strategies and childhood social and mixed anxiety symptoms, we correlated single parental and child ER strategies with social and mixed anxiety symptoms scores to identify relevant factors for the regression analysis. Then, two multiple hierarchical regression analyses were run using either child social anxiety (SASC-RD score) or child mixed anxiety symptoms (FSSCR score) as criteria. According to Morris et al. [37], both parent and child characteristics (such as age or gender) are important influences on children’s adjustment and socio-emotional variables. We, therefore, controlled for such possible influences in the first regression step by including children’s age [46], gender [47] and parent’s psychopathology [33]. At the next step, children’s habitual ER was entered as a factor since research indicates that child ER plays an important role in childhood anxiety disorders (e.g. [4, 43]). Finally, we added parental habitual ER because previous studies and theoretical models suggest associations between parental ER and children’s anxieties (e.g. [4, 22]). To avoid overfitting, we included only those ER strategies correlating with children’s anxiety.
Measures of effect size for MANOVAs are expressed as Cohen’s d (small = 0.2, medium = 0.5 and large = 0.8), for correlations as r (small = 0.1, medium = 0.3 and large = 0.5) and for multiple regression analysis as adjusted R 2 [13, 14].
Results
Group differences in children’s ER strategies
A MANOVA comprising all three groups with child single ER strategies as dependent variables revealed a significant main effect of Group, Wilks’ λ = 0.64, F (24, 188) = 1.96, p < 0.01, \( \eta_{\text{p}}^{ 2} \) = 0.20. Post hoc Tukey tests revealed higher scores for the maladaptive ER strategies withdrawal, rumination and giving up, and less frequent use of the adaptive ER strategies acceptance and forgetting in children with SAD when compared to the HC group (see Table 2). Compared to HC children, children with MAD reported using the adaptive strategies distraction and forgetting significantly less frequently, while using the maladaptive strategies giving up and rumination more frequently. Effect sizes varied between 0.46 and 0.80 with partially large confidence intervals ranging between 0.00 and 1.29; thus, while effects were found, no clear conclusions about the real effect sizes can be drawn. No significant differences were found between the SAD and the MAD group. For exploratory analysis, we separated out MAD and analyzed group differences between the single anxiety disorders [separation anxiety disorder (n = 8), specific phobia (n = 15) or generalized anxiety disorder (n = 18)]. Results revealed no significant group differences.
No group differences in parental ER strategies
A MANOVA on Group (SAD, MAD, HC) with parental single ER strategies as dependent variables revealed no significant main effect of group, Wilks’ λ = 0.73, F (24, 19) = 1.33, n.s.; \( \eta_{\text{p}}^{ 2} \) = 0.15. Exploratory post hoc Tukey tests showed no significant differences on any ER strategy between the groups.
Statistical regression of children’s social anxiety and mixed anxiety symptoms
We found significant Pearson correlations between children’s social anxiety and the following single child ER strategies: problem-oriented action (r = −0.25, p = 0.015), distraction (r = −0.21, p = 0.039), cheering up (r = −0.23, p = 0.026), giving up (r = 0.47, p < 0.001), aggressive behavior (r = 0.33, p = 0.001), withdrawal (r = 0.51, p < 0.001), self-devaluation (r = 0.38, p < 0.001) and rumination (r = 0.29, p = 0.005). For the single parental ER strategies, only reappraisal correlated significantly with children’s social anxiety (r = −0.19, p = 0.045). With regard to children’s mixed anxiety symptoms, analysis revealed significant correlations with the following single child ER strategies: problem-oriented action (r = −0.20, p = 0.046), reappraisal (r = −0.24, p = 0.018), giving up (r = 0.32, p = 0.001), aggressive behavior (r = 0.24, p = 0.019), withdrawal (r = 0.30, p = 0.003) and rumination (r = 0.26, p = 0.012). For the single parental ER strategies, only cheering up correlated significantly with children’s mixed anxiety symptoms (r = −0.23, p = 0.017).
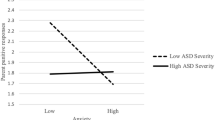
Hierarchical multiple regression analyses were then performed with children’s social anxiety (as measured by SASC-RD score) and mixed anxiety symptoms (as measured by FSSCR score) as criteria. Control variables were entered at step one; children’s and parent’s ER strategies were entered at the second and third steps. Variance inflation factors were always below 10.0. Regarding social anxiety (Table 3), the overall regression model significantly explained 46.2% of the variance in children’s trait social anxiety, F (12, 95) = 8.65, p < 0.001. Gender was significant at the first step. Further, children’s maladaptive ER strategies aggressive behavior, withdrawal and self-devaluation were significantly associated with social anxiety. At the last step, parental reappraisal was significant.
Regarding mixed anxiety symptoms (Table 4), the overall regression model explained 25.8% of the variance in children’s trait anxiety, F (10, 97) = 4.72, p < 0.001. Again, gender was significant at the first step. Children’s reappraisal, aggressive behavior and rumination were significantly associated with children’s mixed anxiety symptoms. At the last step, parental cheering up was significant.
Discussion
To our knowledge, this is the first study investigating maladaptive and adaptive ER strategies in a sample of children with SAD and their parents, including both a clinical control group with mixed anxiety disorders (MAD) and a healthy control (HC) group. Our study partially replicates and importantly extends previous research findings [4, 30]. As hypothesized, SAD and MAD children reported significantly fewer adaptive and more maladaptive ER strategies when compared to HC children. Supporting the idea that ER deficits may exist across different diagnoses of childhood anxiety, children with MAD and SAD did not differ in the frequency of self-reported habitual ER strategies. Further, in our cross-sectional design, both children’s and parent’s single ER strategies were significantly associated with children’s social anxiety symptoms and children’s mixed anxiety symptoms when controlling for age, gender and parent’s psychopathology. This suggests an important role of specific ER strategies in the maintenance of social anxiety and mixed anxiety symptoms. However, when comparing the regression models at a descriptive level, parental and child ER explained almost twice the amount of variance in social anxiety as for mixed anxiety symptoms, implying a particularly strong relationship between ER and social anxiety.
Contrary to our hypothesis, parents of HC children and children with MAD and SAD did not differ in their habitual ER strategy use. However, in our regression models, parental single ER strategies had a statistically significant impact on children’s social and mixed anxiety symptoms.
ER deficits in children with SAD
In accordance with previous research [39,40,41], children with SAD reported more frequent use of rumination when compared to HC children. Furthermore, children with SAD reported fewer ER strategies such as acceptance and forgetting. Also, they seem to give up more easily, in accordance with previous findings for SAD in children [4, 30] and adults [29]. In addition, compared to HC children, children with SAD reported more withdrawal, indicating problems with interpersonal ER. It is possible that children with SAD withdraw when feeling anxious to avoid feared negative evaluations [45]. Our results suggest that these strategies should be targeted in the treatment of childhood SAD.
Transdiagnostic ER deficits in children with SAD and MAD
The finding of similar ER impairments in children with SAD and MAD extends recent research findings on childhood SAD [4, 30]. Our results imply that deficits in ER may exist across different diagnostic domains of clinical anxiety in general and, therefore, may not be specific to SAD. With a closer look, we found some specific associations in our regression analyses: child ER strategies aggressive action, withdrawal and self-devaluation and the parental ER strategy reappraisal were significantly associated with social anxiety in children. Compared to this, child ER strategies reappraisal, aggressive action and rumination and the parental ER strategy cheering up were significantly related to mixed anxiety symptoms. These significant relationships between specific ER strategies and different forms of anxiety in the absence of differences across diagnostic groups may suggest that differences in ER mainly emerge in the subclinical level of childhood anxiety.
Importantly, our results show that our findings have synergized with recent empirical and theoretical work, emphasizing: (a) the association of maladaptive ER with SAD [29]; and (b) that ER deficits cut across different anxiety disorders [19]. If deficits in ER are, in fact, present across different anxiety disorders in childhood, there could be important implications for future research and clinical practice. First, etiological models should consider deficits in ER to be a common symptom in different forms of anxiety by taking into account transdiagnostic processes underlying various forms of psychopathology. This transdiagnostic approach to ER would fit well with the recently proposed research domain criteria perspective [28], which tries to identify similar dimensional constructs, such as ER, that may span across multiple disorders. Furthermore, treatment programs may improve from transdiagnostic findings, in the sense that similar ER training may be offered for children with different anxiety disorders. In fact, several transdiagnostic anxiety programs are available for children with different anxiety disorders, and specific ER strategies are already incorporated in some (e.g. FRIENDS [6]). Of all ER strategies assessed in this study, reappraisal seems to be particularly important: in our study, less reappraisal in children was associated with children’s social anxiety symptoms and less reappraisal in parents was associated with children’s mixed anxiety symptoms. Enhancing reappraisal in both children and parents could, therefore, be a module existing across treatment programs for childhood anxiety disorders. Children could learn to use reappraisal as an alternative for other maladaptive ER strategies they would usually employ like rumination, which was related to children’s mixed anxiety symptoms in our study.
Relations between child and parental ER in childhood anxiety disorders
This study extends findings of previous studies that have assessed ER in different childhood anxiety disorders [31, 32] by examining primary caregivers’ ER and the relationship to both childhood SAD and MAD. First, our results revealed no differences between parents of children with anxiety disorders (including SAD) and parents of HC children, which contradicts theories assuming an accumulation of ER deficits within families [5]. One possible explanation of our finding is that parents only differ in their habitual ER strategy use when they themselves suffer from psychopathology. Congruent with this idea, researchers have argued that parents with mental disorders may show difficulties regulating their emotions and, therefore, lack the skills necessary to model adaptive ER to their children [15, 22]. In our sample, however, parents of both anxiety groups did not differ from control parents in their self-reported psychopathology. In looking further at potential relationships between child and parental ER and children’s symptoms of social anxiety and mixed anxiety, the parental ER strategies reappraisal (social anxiety) and cheering up (mixed anxiety) explained some of the variance in children’s anxiety symptoms. This suggests that some parental ER strategies play an important role at a dimensional level. This finding harmonizes both with previous study results and theoretical work, suggesting a relationship between parental and child ER and children’s anxiety [4, 22, 26].
Limitations and future directions
The following limitations apply: first, while both parental and child ER were assessed, the cross-sectional data did not allow conclusions about causal effects. Therefore, it could not be ruled out that influences of parental ER may appear over time and be a causal factor in childhood anxiety. Second, due to the small sample size, comparisons between the single different anxiety disorders (e.g. SAD vs. specific phobia) are not reliable based on our data. Hence, future research should use larger sample sizes to compare SAD to several individual anxiety disorders.
Third, ER was measured using trait questionnaires, which assess general ER strategies such as rumination, but it is possible that subgroups of children with clinical fears differ in the specific content of these ER strategies, such as the specific ruminative quality (e.g. “I embarrassed myself” vs, “I will get lost”). Also, we only examined ER in the context of fear, and we cannot draw conclusions about how children regulate other emotions such as anger or happiness. Previous research suggests that the dysregulation not only of fear, but also of other emotions (both positive and negative) could play an important role in anxiety disorders [21]. Hence, the measurement of ER focusing on a variety of different emotions should be part of future research.
Fourth, while measuring children’s psychopathology with clinical interviews and multiple informants, we were only able to assess ER via self-reports. The use of self-reports provides insight into children’s regulatory activities, but they need to be validated using multiple measures and methods such as psychophysiology ([40, 41, 48].
Finally, it is important to emphasize that the functionality of ER strategies must be considered within the context and goal(s) of a given situation [9]. Possibly, when examining ER within the situational context, we might find differences between the individual anxiety disorders (e.g. examining ER in a social evaluation context vs. in a separation context). Also, the effectiveness of a given ER strategy may be influenced by other ER strategies, and it is difficult to determine the order in which the person engages in such strategies. Research indicates that children with anxiety disorders report using a number of different ER strategies [11] and we still know very little about how the combination of different ER strategies as well as how the changes between them influence emotional outcomes in a given situation [25]. To elucidate these effects, experience sampling methodologies are urgently needed. A final suggestion for future research would be to explore the most suitable strategies for a child’s age and cognitive development in a given situational context.
Still, information about habitual use of ER strategies in children with SAD and MAD can inform us about possible rigid and inflexible responses that are assumed to be associated with psychopathology [2]. In this way, the current study points to the importance of ER deficits in childhood SAD as well as MAD suggesting that intervention and prevention programs should address these ER difficulties transdiagnostically.
References
Achenbach TM (1991) Manual for the Child Behavior Checklist/4-18 and 1991 Profile. University of Vermont Department of Psychiatry, Burlington, VT
Aldao A (2013) The future of emotion regulation research: capturing context. Perspect Psychol Sci 8(2):155–172. doi:10.1177/1745691612459518
Aldao A, Nolen-Hoeksema S, Schweizer S (2010) Emotion-regulation strategies across psychopathology: a meta-analytic review. Clin Psychol Rev 30(2):217–237. http://www.redi-bw.de/db/ebsco.php/search.ebscohost.com/login.aspx%3fdirect%3dtrue%26db%3dpsyh%26AN%3d2010-01495-006%26site%3dehost-live
Asbrand J, Svaldi J, Krämer M, Breuninger C, Tuschen-Caffier B (2016) Familial accumulation of social anxiety symptoms and maladaptive emotion regulation. PLoS One 11(4):e0153153. doi:10.1371/journal.pone.0153153
Bariola E, Gullone E, Hughes EK (2011) Child and adolescent emotion regulation: the role of parental emotion regulation and expression. Clin Child Fam Psychol Rev 14(2):198–212. doi:10.1007/s10567-011-0092-5
Barrett P, Turner C, Lowry-Webster H (2000) Friends for children group leader’s manual. Australian Academic Press
Beesdo K, Knappe S, Pine DS (2009) Anxiety and anxiety disorders in children and adolescents: developmental issues and implications for DSM-V. Psychiatr Clin N Am 32(3):483–524. doi:10.1016/j.psc.2009.06.002
Beidel DC, Turner SM, Morris TL (1999) Psychopathology of childhood social phobia. J Am Acad Child Adolesc Psychiatry 38(6):643–650
Bonanno GA, Burton CL (2013) Regulatory flexibility: an individual differences perspective on coping and emotion regulation. Perspect Psychol Sci 8(6):591–612. doi:10.1177/1745691613504116
Buckholdt KE, Parra GR, Jobe-Shields L (2014) Intergenerational transmission of emotion dysregulation through parental invalidation of emotions: implications for adolescent internalizing and externalizing behaviors. J Child Fam Stud 23(2):324–332. doi:10.1007/s10826-013-9768-4
Carthy T, Horesh N, Apter A, Gross JJ (2010) Patterns of emotional reactivity and regulation in children with anxiety disorders. J Psychopathol Behav Assess 32(1):23–36. doi:10.1007/s10862-009-9167-8
Cisler JM, Olatunji BO, Feldner MT, Forsyth JP (2010) Emotion regulation and the anxiety disorders: an integrative review. J Psychopathol Behav Assess 32(1):68–82. doi:10.1007/s10862-009-9161-1
Cohen J (1988) Statistical power analysis for the behavioral sciences, 2nd edn. Lawrence Erlbaum Associates, Hillsdale
Cohen J (1992) A power primer. Psychol Bull 112(1):155
Cole PM, Michel MK, Teti LO (1994) The development of emotion regulation and dysregulation: a clinical perspective. Monogr Soc Res Child Dev 59(2–3):73–102
Cole PM, Martin SE, Dennis TA (2004) Emotion regulation as a scientific construct: methodological challenges and directions for child development research. Child Dev 75(2):317–333. doi:10.1111/j.1467-8624.2004.00673.x
Döpfner M, Schnabel M, Goletz H, Ollendick TH (2006) PHOKI: Phobiefragebogen für Kinder und Jugendliche. Hogrefe, Göttingen
Döpfner M, Berner W, Schmeck K (2003) Elternfragebogen über das Verhalten von Kindern und Jugendlichen (CBCL/4-18). Arbeitsgruppe Kinder-, Jugend-und Familiendiagnostik
Fernandez KC, Jazaieri H, Gross JJ (2016) Emotion regulation: a transdiagnostic perspective on a new RDoC domain. Cognit Therapy Res. doi:10.1007/s10608-016-9772-2
Franke GH, Derogatis LR (2000) BSI: brief symptom inventory von LR Derogatis: (Kurzform der SCL-90-R): deutsche version: Testmappe: Beltz test
Gilbert KE (2012) The neglected role of positive emotion in adolescent psychopathology. Clin Psychol Rev 32(6):467–481. doi:10.1016/j.cpr.2012.05.005
Ginsburg GS, Siqueland L, Masia-Warner C, Hedtke K (2004) Anxiety disorders in children: family matters. Cognit Behav Pract 11:28–43
Grob A, Horowitz D (2014) Fragebogen zur Erhebung der Emotions regulation bei Erwachsenen (FEEL-E). Huber, Bern
Grob A, Smolenski C (2005) Fragebogen zur Erhebung der Emotions regulation bei Kindern und Jugendlichen: (FEEL-KJ). Verlag Hans Huber, Bern
Gross JJ (2015) Emotion regulation: current status and future prospects. Psychol Inq 26(1):1–26. doi:10.1080/1047840X.2014.940781
Han ZR, Shaffer A (2013) The relation of parental emotion dysregulation to children’s psychopathology symptoms: the moderating role of child emotion dysregulation. Child Psychiatry Hum Dev 44(5):591–601. doi:10.1007/s10578-012-0353-7
Hodson KJ, McManus FV, Clark DM, Doll H (2008) Can Clark and Wells’ (1995) cognitive model of social phobia be applied to young people? Behav Cognit Psychother. doi:10.1017/S1352465808004487
Insel T, Cuthbert B, Garvey M, Heinssen R, Pine DS, Quinn K, Wang P (2010) Research domain criteria (RDoC): toward a new classification framework for research on mental disorders. Am J Psychiatry 167(7):748–751
Jazaieri H, Morrison AS, Goldin PR, Gross JJ (2015) The role of emotion and emotion regulation in social anxiety disorder. Curr Psychiatry Rep. doi:10.1007/s11920-014-0531-3
Lange S, Tröster H (2014) Strategien der Emotions regulation bei sozial ängstlichen Kindern und Jugendlichen. Z Klin Psychol Psychother 43(1):35–42. doi:10.1026/1616-3443/a000246
Legerstee JS, Garnefski N, Jellesma FC, Verhulst FC, Utens EM (2010) Cognitive coping and childhood anxiety disorders. Eur Child Adolesc Psychiatry 19(2):143–150. doi:10.1007/s00787-009-0051-6
Legerstee JS, Garnefski N, Verhulst FC, Utens EM (2011) Cognitive coping in anxiety-disordered adolescents. J Adolesc 34(2):319–326. doi:10.1016/j.adolescence.2010.04.008
Lieb R, Wittchen H, Höfler M, Fuetsch M, Stein MB, Merikangas KR (2000) Parental psychopathology, parenting styles, and the risk of social phobia in offspring: a prospective-longitudinal community study. Arch Gen Psychiatry 57(9):859–866. doi:10.1001/archpsyc.57.9.859
McHugh ML (2011) Multiple comparison analysis testing in ANOVA. Biochem Med. doi:10.11613/BM.2011.029
Melfsen S, Florin I (1997) Ein Fragebogen zur Erfassung sozialer Angst bei Kindern (SASC-RD). Kindh Entwick 6(4):224–229
Morris AS, Silk JS, Morris MDS, Steinberg L, Aucoin KJ, Keyes AW (2011) The influence of mother-child emotion regulation strategies on children’s expression of anger and sadness. Dev Psychol 47(1):213–225. doi:10.1037/a0021021
Morris AS, Silk JS, Steinberg L, Myers SS, Robinson LR (2007) The role of the family context in the development of emotion regulation. Soc Dev 16(2):361–388. doi:10.1111/j.1467-9507.2007.00389.x
Neuschwander M, In-Albon T, Adornetto C, Roth B, Schneider S (2013) Interrater-Reliabilität des Diagnostischen Interviews bei psychischen Störungen im Kindes-und Jugendalter (Kinder-DIPS). Z Kinder Jugendpsychiatrie Psychother 41:319–334
Schmitz J, Krämer M, Blechert J, Tuschen-Caffier B (2010) Post-event processing in children with social phobia. J Abnorm Child Psychol 38(7):911–919. doi:10.1007/s10802-010-9421-2
Schmitz J, Krämer M, Tuschen-Caffier B (2011) Negative post-event processing and decreased self-appraisals of performance following social stress in childhood social anxiety: an experimental study. Behav Res Ther 49(11):789–795
Schmitz J, Krämer M, Tuschen-Caffier B, Heinrichs N, Blechert J (2011) Restricted autonomic flexibility in children with social phobia. J Child Psychol Psychiatry 52(11):1203–1211. doi:10.1111/j.1469-7610.2011.02417.x
Schneider S, Margraf J (2011) DIPS: Diagnostisches Interview bei psychischen Störungen (4., überarbeitete Auflage). Springer, Berlin. doi:10.1007/978-3-642-15529-1
Suveg C, Zeman J (2004) Emotion regulation in children with anxiety disorders. J Clin Child Adolesc Psychol 33(4):750–759. doi:10.1207/s15374424jccp3304_10
Thompson RA (1994) Emotion regulation: a theme in search of definition. Monogr Soc Res Child Dev 59(2–3):25–52
Weeks JW, Rodebaugh TL, Heimberg RG, Norton PJ, Jakatdar TA (2009) “To avoid evaluation, withdraw”: fears of evaluation and depressive cognitions lead to social anxiety and submissive withdrawal. Cognit Therapy Res 33(4):375–389. doi:10.1007/s10608-008-9203-0
Weems C (2008) Developmental trajectories of childhood anxiety: identifying continuity and change in anxious emotion. Dev Rev 28(4):488–502. doi:10.1016/j.dr.2008.01.001
Wittchen H-U, Stein MB, Kessler RC (1999) Social fears and social phobia in a community sample of adolescents and young adults: prevalence, risk factors and co-morbidity. Psychol Med 29(02):309–323
Zeman J, Klimes-Dougan B, Cassano M (2007) Measurement issues in emotion research with children and adolescents. Clin Psychol Sci Pract 14(4):377–401
Acknowledgements
The authors would like to thank the participating children and parents, as well as members of the research project team who facilitated the completion of the study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Funding
This work was supported by the German Research Foundation (DFG; TU 78/8-1 and SCHM 3056/2-1).
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Keil, V., Asbrand, J., Tuschen-Caffier, B. et al. Children with social anxiety and other anxiety disorders show similar deficits in habitual emotional regulation: evidence for a transdiagnostic phenomenon. Eur Child Adolesc Psychiatry 26, 749–757 (2017). https://doi.org/10.1007/s00787-017-0942-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00787-017-0942-x