Abstract
Children and adolescents with attention-deficit/hyperactivity disorder (ADHD) experience high rates of sleep problems and are also at increased risk for experiencing comorbid mental health problems. This study provides an initial examination of the 1-year prospective association between sleep problems and comorbid symptoms in youth diagnosed with ADHD. Participants were 81 young adolescents (75 % male) carefully diagnosed with ADHD and their parents. Parents completed measures of their child’s sleep problems and ADHD symptoms, oppositional defiant disorder (ODD) symptoms, and general externalizing behavior problems at baseline (M age = 12.2) and externalizing behaviors were assessed again 1 year later. Adolescents completed measures of anxiety and depression at both time-points. Medication use was not associated with sleep problems or comorbid psychopathology symptoms. Regression analyses indicated that, above and beyond demographic characteristics, ADHD symptom severity, and initial levels of comorbidity, sleep problems significantly predicted greater ODD symptoms, general externalizing behavior problems, and depressive symptoms 1 year later. Sleep problems were not concurrently or prospectively associated with anxiety. Although this study precludes making causal inferences, it does nonetheless provide initial evidence of sleep problems predicting later comorbid externalizing behaviors and depression symptoms in youth with ADHD. Additional research is needed with larger samples and multiple time-points to further examine the interrelations of sleep problems and comorbidity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
It is clear that children and adolescents with attention-deficit/hyperactivity disorder (ADHD) experience much higher rates of sleep problems than their peers without ADHD [1, 2]. In a large sample of youth with ADHD, approximately 30 % had mild sleep problems and an additional 45 % had moderate to severe sleep problems [3]. In particular, youth with ADHD have greater bedtime resistance, longer sleep onset latency, poorer sleep quality, and greater daytime sleepiness compared to youth without ADHD [4–7].
In addition to sleep problems, youth with ADHD are also at increased risk for experiencing comorbid mental health problems, including both externalizing (e.g., oppositionality and aggression) and internalizing (e.g., anxiety and depression) symptoms [8, 9]. Across studies, approximately 45–84 % of youth with ADHD meet criteria for comorbid ODD, 25–35 % for an anxiety disorder, and 25–30 % for a depressive disorder [10]. Moreover, up to 67 % of youth with ADHD have at least two comorbid disorders [11]. This is noteworthy because youth with ADHD who have a comorbid condition often experience greater social impairment [8, 12, 13], poorer academic functioning [14, 15], and increased risk for delinquency and substance use [16, 17] in comparison to those without comorbid conditions. In addition, psychiatric comorbidity has been identified as an important predictor of the persistence of ADHD as children and adolescents with ADHD transition to adulthood [18–20]. Despite these findings, remarkably little research attention has been devoted to identifying predictors of comorbidity among youth with ADHD, which is critical to inform prevention and intervention efforts.
Despite the fact that sleep is clearly linked with neurobehavioral functioning [21], perhaps through such mechanisms as executive functions (EF) [22] and affect regulation [23], no study to date has examined whether sleep problems prospectively predict comorbidity among youth diagnosed with ADHD [67]. However, a number of studies have cross-sectionally examined whether psychiatric comorbidity affects or not the sleep patterns of youth with ADHD. For example, Moreau et al. [24] recently found that youth with ADHD and comorbid internalizing or externalizing problems had greater bedtime resistance, shorter sleep duration, more frequent night waking, and greater daytime sleepiness than youth with ADHD alone. In terms of specific comorbidities, several studies have shown that youth with ADHD who have comorbid anxiety or depression have more sleep problems than youth with ADHD alone [25–28]. Evidence to date is more mixed in terms of whether comorbid oppositional defiant disorder (ODD) symptoms or conduct problems are associated with increased sleep problems in youth with ADHD. Specifically, whereas two studies did not report an association between comorbid ODD and increased sleep problems among children with ADHD [28, 29], other studies have found both internalizing and externalizing problems to be associated with overall sleep problems among children with ADHD [30, 31]. Similarly, Ivanenko et al. [27] found sleep duration and sleep latency to be strongly correlated with both externalizing and internalizing problems among 174 children evaluated at a pediatric mental health clinic, 45 % of whom were diagnosed with ADHD. Finally, Lycett and colleagues [32, 33] recently found that among children with ADHD, those who have both internalizing and externalizing comorbidities experience the highest rates of sleep problems.
Taken together, there appears to be a convergence of evidence suggesting that sleep problems are associated with comorbid internalizing problems among youth with ADHD and possibly associated with comorbid externalizing problems as well. However, the extant research is limited in two primary ways. First, with the exception of one study that examined comorbidity as a predictor of sleep problem persistence among youth with ADHD [32], all other studies conducted to date in this area have used a cross-sectional design, leaving it unclear if sleep problems predict increases in comorbid symptoms over time among youth with ADHD. However, research conducted in representative population sample of youth provides evidence of sleep problems longitudinally predicting increases in both internalizing and externalizing problems [34]. A second limitation of research examining sleep and comorbidity among youth with ADHD is the tendency in most studies to combine anxiety and depression [24, 27, 28, 32, 33], thus reducing specificity and possibly clouding differential associations of sleep problems in relation to these two internalizing domains. Indeed, the one study that did distinguish between comorbid anxiety and depression among children with ADHD found that comorbid anxiety was concurrently associated with greater sleep problems whereas comorbid depression was not [25].
In sum, there is a clear need for research that (1) examines whether sleep problems longitudinally predict comorbidity among youth with ADHD, and (2) differentiates between comorbid anxiety, depression, and externalizing symptoms. The present study is an initial step in addressing these two gaps in the literature. Specifically, we examined whether sleep problems would predict later anxiety, depression, or externalizing behaviors over a 1-year period in a sample of 81 young adolescents comprehensively diagnosed with ADHD. In order to determine whether sleep problems actually predicted increases in comorbid symptoms and to bolster confidence in the findings, we controlled for baseline comorbidity as well as demographic characteristics and ADHD symptom severity in our models. Although mixed findings have been reported in the literature, we hypothesized that sleep problems would significantly predict later anxiety, depression, and externalizing behaviors among youth with ADHD.
Methods
Participants
Participants were 81 young adolescents (61 males, 20 females) with ADHD between the ages of 10 and 14 at baseline (M = 12.20, SD = 0.95). Per criteria described below, 42 participants were diagnosed with ADHD predominantly inattentive type (ADHD-I) and 39 participants were diagnosed with ADHD combined type (ADHD-C). Approximately 80 % of the participants were Caucasian (n = 64), with the remaining participants being Black (n = 11), multiracial (n = 5), or Hispanic/Latino (n = 1). Participants’ annual family income ranged from less than $10,000 to over $225,000 (M = $54,248; Median = $37,500). Thirty-three participants (41 %) were taking medication for ADHD at T1, and 38 participants (47 %) were taking medication for ADHD at T2.
Procedures
Data were collected as part of a two-site randomized clinical trial (RCT) examining school-based psychosocial interventions for young adolescents with ADHD. The two time-points examined in the present study, referred to hereafter as T1 and T2, were collected 1 year apart. Participants included in the current set of analyses were included in the community care (i.e., control) condition and, therefore, did not receive any intervention services from study personnel while participating in this study (it is possible that these youth received intervention elsewhere over the course of the study). The study was reviewed and approved by the Institutional Review Board (IRB) and was conducted in accordance with the ethical standards of the 1964 Declaration of Helsinki and its later amendments.
Recruitment was conducted through three primary methods: (1) study announcement letters were mailed to the parents of all students attending identified middle schools at both of the study sites, (2) staff at these schools directly informed parents of some students about the opportunity to participate in this study, and (3) fliers were posted in each participating school. Primary caregivers (hereafter “parents”) who contacted the research staff in response to these recruitment activities were given additional information and were administered a phone screen to assess initial eligibility. On the phone screen, parents had to indicate that their child had a diagnosis of ADHD or had to endorse their child as currently exhibiting at least 4 of 9 Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) [35] symptoms of inattention on a rating scale to be scheduled for an inclusion/exclusion evaluation. The ADHD inattentive symptoms were administered during the phone screen since the study required participating youth to meet criteria for either the ADHD-I or ADHD-C subtypes (and, thus, all eligible youth had to display inattentive symptoms). At the inclusion/exclusion evaluation, all parents signed informed consent and youth provided assent. The inclusionary criteria were (a) meeting full diagnostic criteria for ADHD-I or ADHD-C; (b) an IQ ≥ 80 as estimated using the Wechsler intelligence scale for children, fourth edition (WISC-IV) [36]; and (c) not meeting criteria for a primary diagnosis of a pervasive developmental disorder or meeting diagnostic criteria for any of the following: bipolar disorder, psychosis, substance dependence other than tobacco, or obsessive–compulsive disorder. Of the 326 youth enrolled in the RCT, 104 were randomized to the community care condition and 81 of these had complete data for the current study variables and were used in analyses.
ADHD diagnoses were determined using procedures similar to those used in the Multimodal Treatment Study of ADHD (MTA) [37]. Primarily, the presence of ADHD symptoms was established using the Children's Interview for Psychiatric Syndromes—Parent Version (P-ChIPS) [38, 39], a well-validated structured diagnostic interview that was administered to parents by advanced doctoral students and doctoral-level psychologists. The parent report of ADHD symptoms on the P-ChIPS could be supplemented with the teacher report of ADHD symptoms as reported on the Disruptive Behavior Disorder rating scale (DBD) [40]. The DBD [40] is a well-validated teacher-report measure of DSM-IV ADHD, ODD, and CD symptoms, with items rated on a four-point scale (0 = not at all present, 3 = very much present). If a parent reported at least four symptoms in either ADHD symptom domain on the P-ChIPS, these symptoms could be supplemented with nonoverlapping symptoms (items rated as occurring “pretty much” or “very much”) on the teacher-reported DBD. However, supplementation could only occur if the teacher endorsed at least four symptoms in a domain as occurring “pretty much” or “very much” on the DBD. The same supplementation rules were used to make ADHD subtype determinations. Finally, other criteria for DSM-IV ADHD (i.e., age of onset, pervasiveness, impairment, and ruling out the possibility of other causal disorders) had to be met. The P-ChIPS was also used to assess for the presence of comorbid psychiatric disorders. Using DSM-IV criteria, 54 % of the participants (n = 44) met criteria for comorbid ODD or CD and 33 % of the participants (n = 27) met criteria for a comorbid internalizing disorder (anxiety or depression).
Measures
Sleep problems
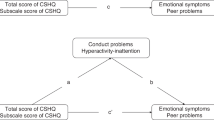
Items from the child behavior checklist for ages 6–18 (CBCL/6–18) [41] were used to measure adolescents’ sleep problems. Although the CBCL does not contain a distinct sleep scale, sleep-specific items are often used by researchers as a measure of sleep problems (e.g., [42–45]). In examining how the CBCL sleep items correlated with daily sleep diaries and objective measures of sleep (i.e., actigraphy, polysomnography), Gregory et al. [46] found the CBCL sleep items to be significantly correlated with several of the other sleep variables. In addition, Becker, Ramsey, and Byars [47] found a composite of the CBCL sleep items to be significantly and strongly correlated with the total score of the well-validated Children's Sleep Habits Questionnaire (CSHQ) [48] in a large sample of children referred to a sleep disorders center. Moreover, Becker et al. found the CBCL sleep composite to evince similar correlations as the CSHQ total score with youths’ social problems and psychopathology symptoms [47]. As further evidence for the predictive validity of the CBCL sleep measure for the current analyses specifically, the CBCL sleep items have been shown to longitudinally predict anxiety/depression and aggression in adolescence [49]. The six CBCL sleep items used in the present study were “nightmares”, “overtired without good reason”, “sleeps less than most kids”, “sleeps more than most kids”, “trouble sleeping”, and “talks or walks in sleep”. A mean score of these items was calculated (Cronbach’s α = 0.61), with higher scores indicating poorer sleep functioning. Each item is rated on a three-point scale (0 = not true, 1 = somewhat or sometimes true, 2 = very true or often true).
ADHD and ODD symptoms
Parents also completed the DBD [40], and sum scale scores were used in the present study as a continuous measure of ADHD inattentive, ADHD hyperactive-impulsive, and ODD symptoms. Baseline ADHD symptom severity was used as a covariate in all analyses, and follow-up ODD symptom severity was used as a primary outcome of interest in the present study.
Externalizing behaviors
The 12-item Externalizing Problems subscale of the parent-completed Social Skills Improvement System (SSIS) [50] was used to measure youths’ general externalizing behavior problems. The externalizing problems subscale was chosen since it includes a range of disruptive behaviors, including items similar to ADHD hyperactive-impulsive symptoms (e.g., “has difficulty waiting for turn”) as well as items assessing oppositional behaviors (e.g., “talks back to adults”) and more severe conduct problem/aggressive behaviors (e.g., “bullies others”, “fights with others”, “forces others to act against their will”). Parents completed this measure at both baseline and follow-up. Items are rated on a four-point scale (0 = never/not true, 3 = almost always/very true). Internal and test–retest reliability of the SSIS are good, and adequate criterion, convergent, and discriminant validity have been established [50].
Depression symptoms
Youth completed the Reynolds Adolescent Depression Scale, Second Edition (RADS-2) [51] at baseline and follow-up as a measure of their own depressive symptoms. The RADS-2 includes 30 items that measure youths’ depressive symptoms (including dysphoric mood, anhedonia/negative affect, negative self-evaluation, and somatic complaints). Each item is rated on a four-point scale (1 = almost never, 4 = most of the time), with some items reverse-coded before summing the items to create subscale and total scores with higher scores indicating greater levels of depressive symptoms. Internal consistency and test–retest reliability across both school-based and clinical samples demonstrated alphas ranging from 0.80 to 0.93 for the subscale and total scores [51]. Content, convergent, and discriminant validity of the RADS-2 has also been established [51]. The participant’s total T-score was used in analyses.
Anxiety symptoms
Youth also completed the Multidimensional Anxiety Scale for Children (MASC) [52, 53] at baseline and follow-up as a measure of their anxiety. The MASC is a 39-item self-report measure of anxiety symptoms in youth (including physical symptoms, harm avoidance, social anxiety, and separation/panic). Item responses range from 0 (never true about me) to 3 (often true about me). Internal consistency for the subscales is adequate (>0.70), and concurrent, convergent, and divergent validity has been established [52–54]. The participant’s total T-score was used in analyses.
Analytic approach
First, preliminary analyses were completed to examine the distribution of the data and the bivariate correlations among the study variables. Next, correlation analyses were conducted to examine whether adolescent demographic characteristics, comorbid psychiatric diagnoses, ADHD symptoms, sleep problems, and externalizing behaviors and internalizing symptoms at the baseline (T1) were bivariately associated with externalizing behaviors and internalizing symptoms 1 year later at follow-up (T2). Finally, hierarchical multiple regression analyses were conducted to examine whether T1 sleep problems predicted T2 externalizing behaviors and internalizing symptoms above and beyond T1 externalizing behaviors/internalizing symptoms, adolescent demographics (i.e., age, sex, race), comorbid psychiatric diagnoses (i.e., having a comorbid ODD/CD or anxiety/depression disorder), and ADHD symptoms. Specifically, demographics, psychiatric comorbidities, ADHD symptoms, and baseline scores on the corresponding outcome of interest were entered on step 1, followed by sleep problems on step 2. For all analyses, statistical significance was set at p < 0.05.
Results
Correlation analyses
Absolute values of skew and kurtosis for all study variables were below 1.5. Bivariate associations of adolescent demographics, presence of a comorbid psychiatric diagnosis, T1 ADHD symptoms, T1 externalizing behaviors/internalizing symptoms, and T1 sleep problems with T2 externalizing behaviors/internalizing symptoms are summarized in Table 1. As shown, having a comorbid ODD/CD diagnosis and ODD symptoms, externalizing problems, inattention, and hyperactivity-impulsivity at T1 were each significantly correlated with T2 ODD symptoms and externalizing problems. Sleep problems were not associated with being on a medication for ADHD at either T1 (r = 0.14, p = 0.23) or T2 (r = 0.02, p = 0.86), nor was T1 or T2 ADHD medication use associated with any of the T2 psychopathology domains. T1 sleep problems were also significantly correlated with both T2 externalizing behavior domains (ps < 0.001). T1 anxiety and depression symptoms were each significantly associated with T2 anxiety and depression symptoms, and although youth characteristics and other T1 psychopathology symptoms were not bivariately associated with T2 anxiety/depression symptoms, these variables were nonetheless controlled for in the subsequent regression models since these variables may still contribute variance in predicting these outcomes. In terms of T1 sleep problems and T2 anxiety/depression symptoms, there was no association between sleep problems and anxiety symptoms at the 1-year follow-up (r = 0.11, p = 0.34), whereas parent-reported sleep problems at T1 were marginally significantly associated with youth-reported depression symptoms 1 year later (r = 0.21, p = 0.06).
Regression analyses predicting externalizing behaviors
Hierarchical regression analyses were conducted to examine whether sleep problems (entered at step 2) predicted adolescents’ externalizing behaviors 1 year later above and beyond demographics, comorbid psychiatric diagnoses, and ADHD symptom severity (entered at step 1). Results are summarized in Table 2. Baseline (T1) externalizing behaviors were also controlled for in each model, and, as expected, T1 externalizing behaviors were a very strong predictor of T2 externalizing behaviors across both the ODD symptom severity and SSIS externalizing problems domains. Thus, these analyses evaluated whether T1 sleep problems would predict T2 externalizing problems after controlling for the expected temporal stability in adolescents’ externalizing behaviors. In the model predicting T2 ODD symptoms (Table 2, top panel), T1 sleep problems were positively associated with greater ODD symptoms (β = 0.26, p = 0.008; ∆R 2 = 0.05) after controlling for T1 ODD symptoms and the other variables included in the model. Similarly, in the model predicting general externalizing problems (Table 2, bottom panel), T1 sleep problems were positively associated with greater externalizing problems (β = 0.26, p = 0.01; ∆R 2 = 0.05) after controlling for T1 externalizing problems and the other variables included in the model.
Regression analyses predicting internalizing symptoms
Similar hierarchical regression analyses were conducted to examine whether sleep problems (entered at step 2) predicted adolescents’ internalizing symptoms 1 year later above and beyond demographics, comorbid psychiatric diagnoses, ADHD symptom severity, and T1 internalizing symptoms (entered at step 1). Results are summarized in Table 3. As expected, T1 internalizing symptoms strongly predicted T2 internalizing symptoms. As shown in Table 3, T1 sleep problems did not significantly predict anxiety (β = 0.13, p = 0.30; ∆R 2 = 0.01) after controlling for T1 anxiety symptoms and the other variables included in the model (Table 3, top panel). However, T1 sleep problems were positively associated with greater depression symptoms (β = 0.23, p = 0.045; ∆R 2 = 0.04) after controlling for T1 depression symptoms and the other variables included in the model.
Discussion
This study examined sleep problems as a predictor of comorbid externalizing behaviors and internalizing symptoms in young adolescents diagnosed with ADHD. Parent-rated sleep problems at baseline predicted parent-rated symptoms of ODD and externalizing problems and youth-rated depressive symptoms 1 year later. Importantly, sleep problems predicted these outcomes after controlling for baseline levels of ODD, externalizing, and depressive symptoms, and also after controlling for demographic characteristics and comorbid diagnostic status (see Tables 2, 3). Specifically, after accounting for youth characteristics and the stability of psychopathology over a 1-year period, sleep problems accounted for an additional 5 % of the variance in predicting youths’ ODD/externalizing behaviors and an additional 4 % of the variance in predicting youths’ depressive symptoms 1 year later. Given the complex processes that likely contribute to the presence of comorbidity among youth with ADHD, these findings are theoretically and clinically important. Together, these findings suggest that sleep problems are not only associated with externalizing and depressive symptoms, but also that sleep problems contribute to the developmental trajectory of externalizing behaviors and depressive symptoms across time. This is especially noteworthy because prior sleep research in ADHD samples has primarily been cross-sectional. Further, these data were collected in a young adolescent sample (M age = 12 at baseline and 13 at follow-up), and adolescence is a high-risk period for the development of antisocial behaviors and depressive disorders [9].
To date, most of the research on the association between sleep and externalizing behaviors in youth with ADHD has been cross-sectional and findings have been mixed, possibly due to the small samples included in these studies (Ns across studies = 27–45) [5, 30, 55]. To the best of our knowledge, the present study is the first to longitudinally evaluate the relation between sleep and externalizing behaviors problems for youth with ADHD. There was a significant association between sleep and externalizing behavior problems broadly and DSM-based ODD symptoms specifically, as rated 1 year post-baseline, even after controlling for comorbid ODD/CD diagnostic status and baseline levels of externalizing and ODD symptom severity. As such, this study provides the strongest evidence to date that sleep problems may contribute to the developmental trajectory of externalizing behaviors in youth with ADHD, exacerbating externalizing behavior problems over time.
The results of the present study also indicated that parent-rated sleep problems significantly predicted youth-rated depressive symptoms even after accounting for baseline levels of depressive symptoms. Our findings suggest that this is an important area for future research since rates of depression increase as children enter adolescence [9] and adolescents with ADHD experience much higher rates of depression and suicidal ideation in comparison to their typically developing peers [56, 57]. In contrast, no association was found between sleep problems and symptoms of anxiety. Although previous cross-sectional studies indicate that youth with comorbid ADHD and anxiety may experience poorer sleep functioning [25, 26], our study suggests that sleep problems do not increase risk for anxiety symptoms over time for young adolescents with ADHD. It is possible that parents are less attuned to certain sleep problems that may be linked to anxiety such as long sleep onset latency or night waking. However, the CBCL measure of sleep functioning used in this study is also limited in its ability to assess for these specific sleep disturbances and the use of longer sleep measures that include items specific to sleep onset, night waking, and sleep-related anxiety (e.g., CSHQ) [48] may yield different findings from those reported in this study. Another intriguing possibility is that the interrelations of sleep and internalizing symptoms are different for anxiety and depression: sleep problems may contribute to increased depression in youth with ADHD whereas anxiety may contribute to increased sleep problems among youth with ADHD. This possibility remains to be empirically tested, and it is likewise clear that the lack of an association between sleep and anxiety in our study will need to be replicated in future studies with larger samples and over a longer developmental period before drawing firm conclusions.
Although sleep problems seem to impact subsequent psychopathology more so than the reverse [58], it is important to point out that the relation between sleep and psychopathology in youth may be bi-directional [58, 59]. For example, Shanahan et al. [34] recently found sleep problems to predict and also be predicted by internalizing and oppositional behaviors in a representative sample of 1,420 youth. Evidence is mixed in terms of whether comorbid oppositional-defiant behaviors exacerbate the sleep problems of youth with ADHD specifically [5, 28, 29], although several studies have found oppositional-defiant behaviors to negatively impact the sleep functioning of youth with ADHD [27, 31]. In terms of sleep problems and depressive symptoms, although the associations between sleep problems and depression may be reciprocal in nature [60], available longitudinal and experimental studies from nonclinical samples indicate that sleep problems more clearly predict depression rather than the reverse [61, 62]. This is especially important to consider since sleep disturbances are part of the diagnostic criteria for depression (as well as for anxiety); it is possible that sleep problems are a useful marker for identifying youth who are at risk for developing depression. Nonetheless, future longitudinal research with additional time points collected over longer periods is needed to evaluate the potential for reciprocal associations between sleep and psychopathology in youth with ADHD specifically [67] (see [58] for an example of this in a community sample). Likewise, it will be important for future research to not only consider sleep problems as identified at a single time point but to also consider the stability of sleep problems over time when examining the long-term effects of sleep problems among youth with ADHD [32, 33].
In addition to examining reciprocal associations, future research should examine mediators that shed light on the processes by which sleep problems contribute to increased ODD/externalizing behaviors and depressive symptoms among youth with ADHD [67]. Sleep problems are associated with a decrement in typically developing youths’ executive functioning as well as increased behavior problems [23, 63, 64]. Since youth with ADHD often experience EF deficits, the added presence of sleep problems may make youth with ADHD especially vulnerable to the negative effects of sleep problems on EF. Deficits in certain aspects of EF such as response inhibition may in turn lead to an increase in behavior problems in youth with ADHD [65]. Another process by which sleep problems may be related to externalizing problems and depressive symptoms is emotion dysregulation. Insufficient or inadequate sleep negatively impacts self-regulation and emotion regulation capabilities [23, 59], which may in turn lead to both externalizing problems and depression [66]. It will be important for future research to extend the findings of the current study by examining mechanisms underlying the link between sleep functioning and comorbid psychopathology in youth with ADHD [67].
Limitations
As noted above, sleep and externalizing behavior problems were both rated by parents and there is potential for within rater bias. Indeed, rater bias likely explains why having a comorbid ODD/CD diagnosis (based on a diagnostic interview conducted with the parent) was associated with T2 ODD symptoms and externalizing problems (based on parent ratings), whereas having a comorbid internalizing diagnosis was not associated with T2 anxiety or depression symptoms (based on youth ratings). It is important to note, however, that youth with ADHD are not considered valid reporters of their own externalizing behaviors and best-practice recommendations are to gather this information from parents and teachers (see [68] for a review). This is in contrast to best-practice assessment recommendations for internalizing symptoms which clearly state that youth self-report is optimal, especially in adolescence [69, 70], which is consistent with the procedures used in this study. In addition, our reliance on the CBCL for measuring youths’ sleep functioning is a limitation and it will be important for future research to include well-validated measures of parent- and youth-reported sleep functioning in tandem with objective measures of youths’ sleep (e.g., polysomnography, actigraphy). Another limitation is the modest sample size (N = 81) and the potential that this limited power to detect effects. However, as noted earlier, the present study’s sample of young adolescents with carefully diagnosed ADHD is actually fairly large in comparison to most of the prior work in the area.
Conclusion
Research on the relation between sleep problems and functioning in youth with ADHD is in the very early stages. Currently, there is not enough longitudinal work completed to draw any firm conclusions about whether sleep problems impact the developmental trajectory of externalizing or internalizing behaviors in youth with ADHD. Research is sorely needed in this area because evidence-based treatments for youth with ADHD do not address sleep in any way. Although best-practice recommendations state that sleep should be assessed as part of an ADHD evaluation to rule-out the possibility that sleep problems are causing inattention [71], only recently have recommendations for treating sleep problems that are comorbid among youth with ADHD begun to be developed [72]. Additional research is needed to guide recommendations on how sleep and ADHD treatments should be optimally sequenced and on the role of ADHD medication [72, 73]. Additional longitudinal work is needed so that evidence-based ADHD interventions can be developed that effectively incorporate sleep as a direct target of treatment.
References
Cortese S, Faraone SV, Konofal E, Lecendreux M (2009) Sleep in children with attention-deficit/hyperactivity disorder: meta-analysis of subjective and objective studies. J Am Acad Child Adolesc Psychiatry 48:894–908
Kirov R, Brand S (2014) Sleep problems and their effect in ADHD. Expert Rev Neurother 14:287–299
Sung V, Hiscock H, Sciberras E, Efron D (2008) Sleep problems in children with attention-deficit/hyperactivity disorder: prevalence and the effect on the child and family. Arch Pediatr Adolesc Med 162:336–342
Corkum P, Moldofsky H, Hogg-Johnson S, Humphries T, Tannock R (1999) Sleep problems in children with attention-deficit/hyperactivity disorder: impact of subtype, comorbidity, and stimulant medication. J Am Acad Child Adolesc Psychiatry 38:1285–1293
Hvolby A, Jorgensen J, Bilenberg N (2009) Parental rating of sleep in children with attention deficit/hyperactivity disorder. Eur Child Adolesc Psychiatry 18:429–438
LeBourgeois MK, Avis K, Mixon M, Olmi J, Harsh J (2004) Snoring, sleep quality, and sleepiness across attention-deficit/hyperactivity disorder subtypes. Sleep 27:520–525
Owens JA, Maxim R, Nobile C, McGuinn M, Msall M (2000) Parental and self-report of sleep in children with attention-deficit/hyperactivity disorder. Arch Pediatr Adolesc Med 154:549–555
Hurtig T, Ebeling H, Taanila A et al (2007) ADHD and comorbid disorders in relation to family environment and symptom severity. Eur Child Adolesc Psychiatry 16:362–369
Merikangas KR, He JP, Burstein M et al (2010) Lifetime prevalence of mental disorders in U.S. adolescents: results from the National Comorbidity Survey Replication-Adolescent Supplement (NCS-A). J Am Acad Child Adolesc Psychiatry 49:980–989
Barkley RA (2006) Attention-deficit hyperactivity disorder: a handbook for diagnosis and treatment, 3rd edn. Guilford, New York
Kadesjo B, Gillberg C (2001) The comorbidity of ADHD in the general population of Swedish school-age children. J Child Psychol Psychiatry 42:487–492
Becker SP, Langberg JM, Vaughn AJ, Epstein JN (2012) Clinical utility of the Vanderbilt ADHD diagnostic parent rating scale comorbidity screening scales. J Dev Behav Pediatr 33:221–228
Booster GD, Dupaul GJ, Eiraldi R, Power TJ (2012) Functional impairments in children with ADHD: unique effects of age and comorbid status. J Atten Disord 16:179–189
Blackman GL, Ostrander R, Herman KC (2005) Children with ADHD and depression: a multisource, multimethod assessment of clinical, social, and academic functioning. J Atten Disord 8:195–207
Hinshaw SP (1992) Academic underachievement, attention deficits, and aggression: comorbidity and implications for intervention. J Consult Clin Psychol 60:893–903
Connor DF, Doerfler LA (2008) ADHD with comorbid oppositional defiant disorder or conduct disorder: discrete or nondistinct disruptive behavior disorders? J Atten Disord 12:126–134
Molina BS, Pelham WE Jr (2003) Childhood predictors of adolescent substance use in a longitudinal study of children with ADHD. J Abnorm Psychol 112:497–507
Biederman J, Petty CR, Clarke A, Lomedico A, Faraone SV (2011) Predictors of persistent ADHD: an 11-year follow-up study. J Psychiatr Res 45:150–155
Lara C, Fayyad J, de Graaf R et al (2009) Childhood predictors of adult attention-deficit/hyperactivity disorder: results from the World Health Organization World Mental Health Survey Initiative. Biol Psychiatry 65:46–54
Mick E, Byrne D, Fried R et al (2011) Predictors of ADHD persistence in girls at 5-year follow-up. J Atten Disord 15:183–192
Beebe DW (2011) Cognitive, behavioral, and functional consequences of inadequate sleep in children and adolescents. Pediatr Clin North Am 58:649–665
Turnbull K, Reid GJ, Morton JB (2013) Behavioral sleep problems and their potential impact on developing executive function in children. Sleep 36:1077–1084
Dahl RE (1996) The impact of inadequate sleep on children’s daytime cognitive function. Semin Pediatr Neurol 3:44–50
Moreau V, Rouleau N, Morin CM (2014) Sleep of children with attention deficit hyperactivity disorder: actigraphic and parental reports. Behav Sleep Med 12:69–83
Accardo JA, Marcus CL, Leonard MB et al (2012) Associations between psychiatric comorbidities and sleep disturbances in children with attention-deficit/hyperactivity disorder. J Dev Behav Pediatr 33:97–105
Hansen BH, Skirbekk B, Oerbeck B, Richter J, Kristensen H (2011) Comparison of sleep problems in children with anxiety and attention deficit/hyperactivity disorders. Eur Child Adolesc Psychiatry 20:321–330
Ivanenko A, Crabtree VM, Obrien LM, Gozal D (2006) Sleep complaints and psychiatric symptoms in children evaluated at a pediatric mental health clinic. J Clin Sleep Med 2:42–48
Mayes SD, Calhoun SL, Bixler EO et al (2009) ADHD subtypes and comorbid anxiety, depression, and oppositional-defiant disorder: differences in sleep problems. J Pediatr Psychol 34:328–337
Hvolby A, Jorgensen J, Bilenberg N (2008) Actigraphic and parental reports of sleep difficulties in children with attention-deficit/hyperactivity disorder. Arch Pediatr Adolesc Med 162:323–329
Choi J, Yoon IY, Kim HW, Chung S, Yoo HJ (2010) Differences between objective and subjective sleep measures in children with attention deficit hyperactivity disorder. J Clin Sleep Med 6:589–595
Noble GS, O’Laughlin L, Brubaker B (2012) Attention deficit hyperactivity disorder and sleep disturbances: consideration of parental influence. Behav Sleep Med 10:41–53
Lycett K, Mensah F, Hiscock H, Sciberras E (2014) A prospective study of sleep problems in children with ADHD. Sleep Med. doi:10.1016/j.sleep.2014.06.004
Lycett K, Sciberras E, Mensah FK, Hiscock H (2014) Behavioral sleep problems and internalizing and externalizing comorbidities in children with attention-deficit/hyperactivity disorder. Eur Child Adolesc Psychiatry
Shanahan L, Copeland WE, Angold A, Bondy CL, Costello EJ (2014) Sleep problems predict and are predicted by generalized anxiety/depression and oppositional defiant disorder. J Am Acad Child Adolesc Psychiatry 53:550–558
American Psychiatric Association (1994) Diagnostic and statistical manual of mental disorders: Fouth edition, 4th edn. American Psychiatric Association, Washington, DC
Wechsler D (2003) Wechsler Intelligence Scale for Children - Fourth Edition (WISC-IV), 4th edn. Psychological Corporation, San Antonio, TX
MTA Cooperative Group (1999) A 14-month randomized clinical trial of treatment strategies for attention-deficit/hyperactivity disorder. The MTA Cooperative Group. Multimodal Treatment Study of Children with ADHD. Arch Gen Psychiatry 56:1073–1086
Fristad MA, Teare M, Weller EB, Weller RA, Salmon P (1998) Study III: development and concurrent validity of the Children’s Interview for Psychiatric Syndromes–parent version (P-ChIPS). J Child Adolesc Psychopharmacol. 8:221–226
Weller EB, Weller R, Rooney MT, Fristad MA (1999) Children’s Interview for Psychiatric Syndromes (ChIPS). American Psychiatric Association, Washington, DC
Pelham WE Jr, Gnagy EM, Greenslade KE, Milich R (1992) Teacher ratings of DSM-III-R symptoms for the disruptive behavior disorders. J Am Acad Child Adolesc Psychiatry 31:210–218
Achenbach TM, Rescorla LA (2001) Manual for the ASEBA school-age forms and profiles. University of Vermont, Research Center for Children, Youth, and Families, Burlington, VT
Alfano CA, Beidel DC, Turner SM, Lewin DS (2006) Preliminary evidence for sleep complaints among children referred for anxiety. Sleep Med 7:467–473
Gregory AM, Van der Ende J, Willis TA, Verhulst FC (2008) Parent-reported sleep problems during development and self-reported anxiety/depression, attention problems, and aggressive behavior later in life. Arch Pediatr Adolesc Med 162:330–335
Stoleru S, Nottelmann ED, Belmont B, Ronsaville D (1997) Sleep problems in children of affectively ill mothers. J Child Psychol Psychiatry 38:831–841
Moore M, Slane J, Mindell JA, Burt SA, Klump KL (2011) Genetic and environmental influences on sleep problems: a study of preadolescent and adolescent twins. Child Care Health Dev 37:638–641
Gregory AM, Cousins JC, Forbes EE et al (2011) Sleep items in the child behavior checklist: a comparison with sleep diaries, actigraphy, and polysomnography. J Am Acad Child Adolesc Psychiatry 50:499–507
Becker SP, Ramsey RR, Byars KC (2014) Convergent validity of the child behavior checklist sleep items with validated sleep measures and sleep disorder diagnoses in children and adolescents referred to a sleep disorders center. Sleep Med. doi:10.1016/j.sleep.2014.09.008
Owens JA, Spirito A, McGuinn M (2000) The children’s sleep habits questionnaire (CSHQ): psychometric properties of a survey instrument for school-aged children. Sleep 23:1043–1051
Gregory AM, O’Connor TG (2002) Sleep problems in childhood: a longitudinal study of developmental change and association with behavioral problems. J Am Acad Child Adolesc Psychiatry 41:964–971
Gresham FM, Elliott SN (2008) Social skills improvement system—rating scales. Pearson, Minneapolis, MN
Reynolds WM (2002) Reynolds adolescent depression scale: RADS-2: professional manual. Psychological Assessment Resources, Odessa
March JS (1997) Multidimensional anxiety scale for children. Multi-Health Systems, North Tonawanda
March JS, Parker JD, Sullivan K, Stallings P, Conners CK (1997) The multidimensional anxiety scale for children (MASC): factor structure, reliability, and validity. J Am Acad Child Adolesc Psychiatry 36:554–565
Baldwin JS, Dadds MR (2007) Reliability and validity of parent and child versions of the multidimensional anxiety scale for children in community samples. J Am Acad Child Adolesc Psychiatry 46:252–260
Hansen BH, Skirbekk B, Oerbeck B, Wentzel-Larsen T, Kristensen H (2014) Associations between sleep problems and attentional and behavioral functioning in children with anxiety disorders and ADHD. Behav Sleep Med 12:53–68
Biederman J, Ball SW, Monuteaux MC et al (2008) New insights into the comorbidity between ADHD and major depression in adolescent and young adult females. J Am Acad Child Adolesc Psychiatry 47:426–434
Chronis-Tuscano A, Molina BS, Pelham WE et al (2010) Very early predictors of adolescent depression and suicide attempts in children with attention-deficit/hyperactivity disorder. Arch Gen Psychiatry 67:1044–1051
Kelly RJ, El-Sheikh M (2014) Reciprocal relations between children’s sleep and their adjustment over time. Dev Psychol 50:1137–1147
Gregory AM, Sadeh A (2012) Sleep, emotional and behavioral difficulties in children and adolescents. Sleep Med Rev 16:129–136
Roberts RE, Duong HT (2014) The prospective association between sleep deprivation and depression among adolescents. Sleep 37:239–244
Dewald-Kaufmann JF, Oort FJ, Meijer AM (2014) The effects of sleep extension and sleep hygiene advice on sleep and depressive symptoms in adolescents: a randomized controlled trial. J Child Psychol Psychiatry 55:273–283
Gregory AM, Rijsdijk FV, Lau JY, Dahl RE, Eley TC (2009) The direction of longitudinal associations between sleep problems and depression symptoms: a study of twins aged 8 and 10 years. Sleep 32:189–199
Sadeh A, Gruber R, Raviv A (2002) Sleep, neurobehavioral functioning, and behavior problems in school-age children. Child Dev 73:405–417
Steenari MR, Vuontela V, Paavonen EJ et al (2003) Working memory and sleep in 6- to 13-year-old schoolchildren. J Am Acad Child Adolesc Psychiatry 42:85–92
Young SE, Friedman NP, Miyake A et al (2009) Behavioral disinhibition: liability for externalizing spectrum disorders and its genetic and environmental relation to response inhibition across adolescence. J Abnorm Psychol 118:117–130
Silk JS, Steinberg L, Morris AS (2003) Adolescents’ emotion regulation in daily life: links to depressive symptoms and problem behavior. Child Dev 74:1869–1880
Becker SP, Langberg JM, Byars KC (in press) Advancing a biopsychosocial and contextual model of sleep in adolescence. J Youth Adolesc
Pelham WE, Fabiano GA, Massetti GM (2005) Evidence-based assessment of attention deficit hyperactivity disorder in children and adolescents. J Clin Child Adolesc Psychol 34:449–476
Klein DN, Dougherty LR, Olino TM (2005) Toward guidelines for evidence-based assessment of depression in children and adolescents. J Clin Child Adolesc Psychol 34:412–432
Silverman WK, Ollendick TH (2005) Evidence-based assessment of anxiety and its disorders in children and adolescents. J Clin Child Adolesc Psychol 34:380–411
Owens JA (2009) A clinical overview of sleep and attention-deficit/hyperactivity disorder in children and adolescents. J Can Acad Child Adolesc Psychiatry 18:92–102
Cortese S, Brown TE, Corkum P et al (2013) Assessment and management of sleep problems in youths with attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry 52:784–796
Stein MA, Weiss M, Hlavaty L (2012) ADHD treatments, sleep, and sleep problems: complex associations. Neurotherapeutics 9:509–517
Acknowledgments
This research was supported by a grant to the second and third authors from the United States National Institute of Mental Health (NIMH; R01MH082865). The contents of this manuscript do not necessarily represent the views of the National Institutes of Health and do not imply endorsement by the Federal Government.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Becker, S.P., Langberg, J.M. & Evans, S.W. Sleep problems predict comorbid externalizing behaviors and depression in young adolescents with attention-deficit/hyperactivity disorder. Eur Child Adolesc Psychiatry 24, 897–907 (2015). https://doi.org/10.1007/s00787-014-0636-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00787-014-0636-6