Abstract
The following hypotheses were tested in a longitudinal, population-based study: (1) Attention deficit hyperactivity disorder (ADHD) symptoms are associated with peer dislike and victimisation; (2) Peer dislike and victimisation increase the risk for subsequent depression; and (3) The effect of ADHD symptoms on depression is partly mediated through peer dislike and victimisation. Gender differences in mediating pathways through peer dislike and victimisation to depression were additionally explored. The Child Behaviour Checklist (CBCL), Youth Self Report (YSR) and Teacher’s Checklist of Pathology (TCP) assessed ADHD symptoms in 728 adolescents. Peer nominations were used to assess peer dislike and victimisation. The Composite International Diagnostic Interview (CIDI) was used to assess depression. Effects of peer dislike, victimisation, and ADHD symptoms on depression were modelled using Cox regression. ADHD symptoms were associated with peer dislike (rs = 0.17, p < 0.001) and victimisation (rs = 0.11, p = 0.001). Dislike, victimisation, and ADHD symptoms increased risk for depression. Risk for depression associated with victimisation and ADHD symptoms reduced with time. Dislike and victimisation mediated 7 % of the effect of ADHD symptoms on depression. Pathways through dislike and victimisation were present in girls but not in boys. Peer dislike and victimisation explain, to a limited extent, the prospective association between ADHD and depression, particularly in girls.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Attention deficit hyperactivity disorder (ADHD), a common neurodevelopmental disorder [1], is often comorbid with depression [2]. Depression not only leads to morbidity by itself, but when associated with ADHD also increases the severity and duration of ADHD and worsens prognosis [3]. Consequently, it is of importance to prevent the development of depression in ADHD. A better understanding of the comorbid association of ADHD and depression is required as a first step to develop preventive measures and interventions. Since ADHD manifests at an early age [4], while depressive disorders typically have an onset in adolescence and young adulthood [5], it could be said that the onset of depression generally follows the onset of ADHD. Depression may arise in ADHD either directly or through the development of other, intermediate problems. Being disliked and being a victim of bullying by peers may be two such intermediate problems.
Adolescents with ADHD have problems in regulating their behaviours, and exhibiting behaviours deemed aberrant by peers could lead to being disliked [6]. Impairments in the development of age-appropriate social skills in ADHD can further compound the peer dislike [7]. Being disliked may in turn spiral into further difficulties in forming and maintaining relationships with peers [8]. The resulting social disconnection can increase feelings of stress, anxiety, and loneliness, setting the stage for development of depression [8, 9].
Due to difficulties in controlling behaviours, adolescents with ADHD often respond aggressively to bullying, making them not only easy but also attractive victims for bullies [10]. Victimisation involves infliction of purposeful hurtful actions by bullies, which ostracise and demoralise the victims [11]. Being victimised may intensify the spiral of isolation and rejection [12, 13], providing an increased risk for depression.
The above-mentioned influences of dislike and victimisation on the risk for future depression may act differently in adolescent boys and girls with ADHD. Boys with ADHD face greater social impairment at school [14], which in turn may make them more likely to be disliked or victimised. Girls, meanwhile, tend to be more sensitive to peers’ opinions, and thus may be affected more by peer dislike and victimisation [8, 15, 16]. The net outcome of these contrasting predispositions might lead to a roughly similar influence of dislike and victimisation on pathways to depression in the two genders. On the other hand, the higher likelihood of social impairment in boys and the greater sensitivity to peer problems in girls might as well produce unexpected differences in these pathways between boys and girls.
Existing studies on the influences of peer problems in the ADHD-depression relationship have shown mixed results. In a short-term prospective study, Mikami and Hinshaw [17] found peer-nominated rejection measures to be associated with depressed anxious behaviour in girls diagnosed with ADHD. Humphreys et al. [18] in a population-based cohort of individuals followed up from birth to 20 years of age, found that teacher- and, self-reported peer rejection and popularity mediated the pathways from ADHD symptoms to depressive symptoms. In another retrospective study, Humphrey et al. [19], found a correlation between victimisation and depression in children diagnosed with ADHD. Finally, Mrug et al. [20] found no evidence to suggest that peer rejection specifically predicted depression in boys and girls diagnosed with ADHD.
Previously, we demonstrated that not only a full diagnosis of ADHD, but subthreshold ADHD too increased the risk for depression [21]. Relatively mild symptoms of ADHD in adolescents may, therefore, be sufficient to increase the risk for being disliked by peers or being victimised, which in turn could increase the risk for depression. The present study was set up to better understand pathways from ADHD symptoms to depression through peer dislike and victimisation. Using a prospective general population sample of adolescents, we tested the hypotheses that: (1) ADHD symptoms are associated with peer dislike and victimisation; (2) Peer dislike and victimisation increase the risk for subsequent depression; and (3) The effect of ADHD symptoms on depression is partly mediated through peer dislike and victimisation. In addition, we explored gender differences in mediating pathways through peer dislike and victimisation to depression.
Methods
The data were collected as part of the TRacking Adolescents’ Individual Lives Survey (TRAILS), a Dutch prospective cohort study focusing on psychosocial development and mental health of adolescents from the general population. TRAILS involves bi- or triennial measurements from age 11 to at least age 25 [22, 23]. The methodology has been described in detail elsewhere [24] and is summarised briefly below.
Cohort
Children were recruited from five municipalities in the north of The Netherlands, including both urban and rural areas. Primary school participation was a requisite for inclusion. Of the 2,935 children who met these criteria, 2,230 (76.0 %) provided informed consent from both parent and child to participate in the study. Four assessment waves have been completed to date.
The present study used data from the second (T2) and fourth wave (T4) which ran from September 2003 to December 2004 (T2), and October 2008 to September 2010 (T4), respectively. The response rate at T2 was 96.4 % (N = 2,149, mean age 13.6, SD = 0.53, 51.0 % girls) of whom 47 % (N = 1,007) completed the peer assessments. The response rate at T4 was 83.4 % (N = 1,881, mean age 19.1, SD = 0.60, 52.3 % girls), of whom 84.2 % (N = 1,584) completed the below described diagnostic interview. Adolescents without peer nomination data at T2 (N = 827) were excluded. Adolescents who had developed depression before T2 (N = 29) were also excluded, to allow only participants who either did not develop depression, or developed depression between T2 and T4. These led to a total of 728 participants (54 % girls) being included in this study. Figure 1 presents a flowchart of participants included at each wave. The study was approved by the Dutch Central Committee on Research Involving Human Subjects (CCMO). Participants were treated in accordance with the Declaration of Helsinki, and all measurements were carried out with their adequate understanding and written consent.
Measures
Attention deficit hyperactivity disorder symptoms were measured using the Child Behaviour Checklist (CBCL) filled out by parents, the Youth Self Report (YSR) filled out by the children, and the Teacher’s Checklist of Psychopathology (TCP) filled out by teachers in the second measurement wave (T2) [25, 26]. The CBCL and YSR are internationally validated questionnaires for child emotional and behavioural problems at ages 4–18 [27]. We used the attention problem scale, which consists of ten items in the CBCL (M = 0.32, SD = 0.30) and nine items in the YSR (M = 0.55, SD = 0.33). The TCP was developed by the TRAILS team and is a shorter version of the Teacher’s Report Form (TRF) [28]. The TCP requires a shorter time than the TRF to be completed and therefore is easier to use in classrooms with many pupils. It contains nine descriptions of behaviours with response options for these behaviours ranging from 1 = not applicable’ to 5 = very clearly applicable’. Information from teacher-reported attention and hyperactivity/impulsivity problems (corresponding to the CBCL-YSR attention problems scales) were used in this study (M = −0.001, SD = 0.91). Multi-informant scores have been reported to give better estimates for ADHD than single-informant scores [29, 30]. We used mean ADHD symptom scores, calculated from standardised parent, adolescent, and teacher ratings (M = 0.005, SD = 0.14).
Information on peer dislike and victimisation was obtained through peer nominations at the second measurement wave (T2) [31]. Peer nominations were collected in classes with at least 3 TRAILS participants. This led to the inclusion of 3,798 adolescents (54.1 % girls) from 150 classes in 34 schools, of whom 1,078 were TRAILS participants [32]. Participants received a list of all classmates and were asked to indicate, amongst other things, whom in their classroom they disliked and who they bullied. The number of nominations participants could make ranged from none to all classmates. All participants completed the peer nominations independently. Variables used in this study reflect the percentage of classmates nominating the TRAILS participants as being disliked (M = 11, SD = 0.13) and victimised (M = 2, SD = 0.05). Percentage nominations were used to offset differences in the number of participants per classroom.
During the fourth assessment wave, psychiatric disorders were assessed by means of the World Health Organization Composite International Diagnostic Interview (CIDI), version 3.0 (N = 1,584). The CIDI is a structured diagnostic interview, which yields lifetime and current diagnoses according to the definitions and criteria of the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV). The CIDI has been used in a large number of surveys worldwide [33], and has shown to have a good concordance with clinical diagnoses [34, 35]. In addition to the occurrence of psychiatric disorders, the CIDI yields their age of onset. In the present study, data on major depressive episode (MDE) was used and depression was operationalized as MDE, either with or without (hypo)manic symptoms. Age of onset refers to the age depression emerged for the first time.
Participants with and without completed CIDI interviews differed significantly in terms of dislike (t = 2.8, p = 0.005), victimisation (t = 3.2, p = 0.002) and ADHD symptom (t = 4.1, p < 0.001) scores at T2. ADHD symptoms scores differed significantly between (excluded) participants with an MDE prior to T2 (N = 29, M = 0.63, SD = 1.2) and included participants (N = 728, M = −0.02, SD = 1.0) (t = −3.5, p = 0.001). The two groups had comparable dislike (t = −1.6, = 0.11) and victimisation (t = 0.40, p = 0.69) scores.
Statistical analysis
Spearman’s rank correlations were used to estimate associations between ADHD symptoms, and peer dislike and victimisation. ADHD symptom, peer dislike and victimisation variables were non-normally distributed for which Spearman’s correlations are better suited. Cox proportional hazards regression was used to estimate the effects of peer dislike and victimisation on the probability to develop an MDE. Next, the effect of ADHD symptoms on the probability to develop an MDE was examined by means of Cox regression both with and without adjusting for dislike and victimisation. The percentage change (reduction) in the hazard ratio (HR) before and after adjusting for dislike and victimisation was computed to assess mediation by these two variables. Lastly, Cox regression models estimating mediation through dislike and victimisation were stratified by gender to explore gender differences.
Continuous variables (i.e., ADHD symptoms, peer dislike and victimisation) were standardised to mean 0 and SD 1 before analysis to ease interpretation of the regression coefficients. The proportional hazards assumption was tested using Schoenfeld residuals. For significant residuals, time-dependent variables were additionally included in the regression models. Time-dependant variables were computed by multiplying the continuous variables with survival time. Survival time was the number of years between assessment of peer data (T2) and onset of depression. Peer dislike and victimisation were included both separately and simultaneously in the above-described regression models to assess their individual and combined effects. Except for the gender-stratified analysis, all models were adjusted for gender. Analyses were performed using SPSS v. 20.0 (IBM Corp., Armonk, NY). All tests were two-tailed and a p value of <0.05 was considered statistically significant.
Results
In the sample, 12 % (n = 90) of the adolescents eventually developed a depressive episode between T2 and T4, of whom 76 % (n = 68) were girls. While 66 % (n = 483) of the adolescents received one or more nominations for being disliked, only 21 % (n = 149) received at least one nomination for being victimised. Nominations (at least one) for both peer dislike and victimisation were received by 18 % (n = 130) of the adolescents.
Spearman’s rho revealed weak but statistically significant relationships between ADHD symptoms and peer dislike (rs = 0.17, p < 0.001), and between ADHD symptoms and victimisation (rs = 0.11, p = 0.001).
Table 1 presents the effects of peer dislike and victimisation on major depression onset. With each unit rise in the standardised peer dislike score, the risk for depression increased by 1.4 times. Victimisation but not peer dislike was found to have a time-varying effect (Schoenfeld residual = −0.25; p = 0.018), and a time-dependent victimisation variable was additionally included in the model. The initial (i.e., at T2) effect of victimisation was stronger, that is, a 1.6 times increased depression risk per unit change in standardised victimisation score which gradually decreased over time and disappeared after about 2 years. When included simultaneously, the effects of dislike and victimisation were roughly similar to their effects on including them separately in the model, suggesting that the effects were non-overlapping.
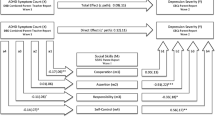
Table 2 presents the effect of ADHD symptoms on major depression onset before and after adjusting for a low peer status and victimisation. ADHD symptoms violated the proportional hazards assumption (Schoenfeld residual = −0.30; p = 0.005), and an additional time-dependent ADHD symptom variable was included in the model. Peer dislike mediated 4 %, while victimisation mediated 3 % of the effect of ADHD symptoms on depression. When included simultaneously, the peer variables explained 7 % of the effect of ADHD symptoms on depression.
The time-varying effect of ADHD symptoms on the risk for depression, before and after adjusting for dislike and victimisation, is illustrated in Table 3. While ADHD symptoms were strongly associated with an increased risk for depression at T2, the estimated risk declined over time and after 6 years, no excess risk remained.
To explore gender differences in pathways from ADHD symptoms to depression, gender-stratified analyses were carried out. Table 4 presents results of these exploratory analyses. In boys, peer dislike and victimisation did not mediate the effect of ADHD symptoms on depression. For girls, peer dislike mediated 7 % and victimisation mediated 3 % of the effect of ADHD symptoms on depression. Please note that the estimated effect of victimisation on depression in girls was not significant when adjusted for ADHD symptoms.
In a previous study, we showed that disruptive behaviours and anxiety problems mediated the pathways from ADHD to depression [21]. We carried out post hoc analyses to assess if effects of peer dislike and victimisation on depression were confounded by disruptive behaviours and anxiety problems. Inclusion of these additional covariates in the models did not change the essence of the results (please see supplementary material), suggesting that effects of peer dislike and victimisation on depression are largely independent of disruptive behaviour and anxiety problems.
Discussion
Through this study, we aimed to further our understanding of the paths to depression in adolescents with symptoms of ADHD. We found that ADHD symptoms were associated with peer dislike and victimisation. Peer dislike, victimisation, and symptoms of ADHD were associated with an increased risk for depressive outcomes. Peer problems of dislike and victimisation mediated to a limited extent the paths to depression. Lastly, exploratory gender analyses showed mediation through peer dislike and victimisation only in girls and not in boys with ADHD symptoms.
Studies on clinical samples have shown a high risk for dislike and victimisation in children with ADHD as compared to other classmates [7, 19]. We found ADHD symptoms to be only weakly associated with dislike and victimisation. These weak associations could be related to the use of a population sample and a continuous measure of ADHD in our study. Moreover, some peers may admire the disruptive and aggressive behaviours of adolescents with ADHD [36, 37], and peer support from a few classmates can protect against dislike and victimisation [38]. Consequently, not all adolescents with ADHD symptoms may be susceptible to face dislike or victimisation, explaining the weak associations of ADHD with these problems.
In accordance with previous literature, we found that peer dislike, victimisation, and ADHD symptoms independently increase the risk for depression [39–42]. In this study, we found that pathways from ADHD symptoms to depression were mediated by peer dislike and victimisation, but to only a limited extent. The limited mediation may be attributable to positive illusory bias [43]. Adolescents with ADHD tend to make inaccurate and overtly positive evaluations of their social skills and classroom peer status [44], which, even though erroneous, may protect against negative outcomes such as depression. Alternatively, the use of a population sample and a continuous measure for ADHD symptoms may have contributed to the lack of substantial mediating effects. It is also possible that peer relationship difficulties indeed play a little role in the development of depression in ADHD, and other factors such as comorbid psychiatric illnesses, poor parental relationships, and traumatic life events mediate these paths to a greater extent [45].
The strength of the association between ADHD symptoms and depression decreased during the course of adolescence. In part, this decrease may be due to transitory state effects at the time ADHD symptoms were assessed. Yet another part may be explained by the fact that adolescents who are most vulnerable to the depressogenic effects of ADHD symptoms are likely to develop a depression first, thereby gradually leaving a more and more resilient group [46, 47]. The reduced risk for depression could also be related to changes in peer perceptions of problem behaviours with age such that, from childhood to adolescence, the symptoms of ADHD become more and more acceptable to peers [37, 48]. Reduction in social impact of ADHD symptoms with age may consequently reduce the risk for depression.
Exploratory analyses of gender differences showed that dislike and victimisation mediated the paths to depression in girls but not in boys. This finding could be explained on the basis of girls’ higher sensitivity to peer opinions [16]. In addition, symptoms and behaviours of ADHD in girls are considered gender inappropriate and are less well tolerated by peers than in boys [14]. This may give rise to more negative appraisals by peers and in turn increase risk for depressive outcomes in girls. Alternatively, the lack of mediation in boys could be related to a lack of power. Since our gender-stratified analyses were conducted in a relatively small sample of boys, our findings have to be corroborated by future research.
The main limitation of our study was that we did not follow up on the peer relationships of the participants. Thus, we could not assess how ADHD symptoms might have affected peer relationships over a period of time, and if this contributed to changes in depressive outcomes. It was also not known whether participants utilised any interventions for their ADHD symptoms. Interventions may lead to cessation of ADHD symptoms, reducing the risk of developing depression. Furthermore, stimulant medications used in the treatment of ADHD may reduce symptoms of depression in ADHD [49]. Treatment can thus alter the occurrence of depression in ADHD and lack of this information may bias interpretations.
The strengths of our study include the use of multi-informant ratings for assessment of ADHD, and peer nominations for assessment of peer relationships. We also used a longitudinal, population-based sample, which allowed us to follow up the effects of ADHD on depression in time. Population-based samples also have the benefit of providing more accurate estimates of prevalences [50], and a balanced representation of genders compared to clinical and referred samples [51]. Lastly, in light of findings suggesting that dimensional approaches depict ADHD more accurately than categorical ones [52, 53], our study, which used ADHD symptom scores, may provide a better picture of this mental health problem than studies based on diagnoses.
Peer problems not only prove to be a possible hindrance to development of adolescents with ADHD but also, as we found in our study, increase the risk for depression. Therefore, interventions aimed at improving peer relationships in ADHD may be of importance. However, such interventions have failed in many instances to modify or improve peer problems [54, 55]. In addition, negative perceptions of peers and teachers may make it difficult for adolescents with ADHD to interact and form friendships [56–58]. This points to the need for developing newer modalities of interventions, which focus on development of a sensitive environment in schools and in the community, responsive to the symptoms of ADHD. Peer problems in ADHD are resistant to change, such that adolescents who cease to show symptoms of ADHD may yet continue to face peer problems [59]. Thus, it is difficult for adolescents to ease into social situations and establish a normal life even with effective treatment and control of ADHD symptoms. In short, interventions aimed at making school and community environments more conducive for adolescents with ADHD may have a better effect in the long term than attempts at ‘integrating’ these adolescents into non-favourable and incompatible environments. A recent study aimed at increasing peers’ social inclusion of children with ADHD has shown promising results in this direction [60].
To conclude, this study elaborates the role of problems in peer relationships as partial mediators of the pathways from ADHD to depression. Though these may not be at work singly and may be complicated by presence of other factors, they provide an insight into the underlying mechanisms leading to depression. Knowledge of the possible precursors to depression in ADHD could help in the development of effective interventions, prevention of depression, and an improvement in the quality of life.
Abbreviations
- ADHD:
-
Attention deficit hyperactivity disorder
- MDE:
-
Major depressive episode
References
American Psychiatric Association (2013) DSM 5. American Psychiatric Association
Connor DF, Edwards G, Fletcher KE, Baird J, Barkley RA, Steingard RJ (2003) Correlates of comorbid psychopathology in children with ADHD. J Am Acad Child Adolesc Psychiatry 42:193–200
Jensen PS, Shervette RE 3rd, Xenakis SN, Richters J (1993) Anxiety and depressive disorders in attention deficit disorder with hyperactivity: new findings. Am J Psychiatry 150:1203–1209
Kessler RC, Amminger GP, Aguilar-Gaxiola S, Alonso J, Lee S, Ustun TB (2007) Age of onset of mental disorders: a review of recent literature. Curr Opin Psychiatry 20:359
Oldehinkel AJ, Wittchen HU, Schuster P (1999) Prevalence, 20-month incidence and outcome of unipolar depressive disorders in a community sample of adolescents. Psychol Med 29:655–668
Diamantopoulou S, Henricsson L, Rydell A (2005) ADHD symptoms and peer relations of children in a community sample: examining associated problems, self-perceptions, and gender differences. Int J Behav Dev 29:388–398
Murray-Close D, Hoza B, Hinshaw SP, Arnold LE, Swanson J, Jensen PS, Hechtman L, Wells K (2010) Developmental processes in peer problems of children with attention-deficit/hyperactivity disorder in the multimodal treatment study of children with ADHD: developmental cascades and vicious cycles. Dev Psychopathol 22:785–802
Oldehinkel AJ, Rosmalen JG, Veenstra R, Dijkstra JK, Ormel J (2007) Being admired or being liked: classroom social status and depressive problems in early adolescent girls and boys. J Abnorm Child Psychol 35:417–427
Lansford JE, Capanna C, Dodge KA, Caprara GV, Bates JE, Pettit GS, Pastorelli C (2007) Peer social preference and depressive symptoms of children in Italy and the United States. Int J Behav Dev 31:274–283
Perry DG, Kusel SJ, Perry LC (1988) Victims of peer aggression. Dev Psychol 24:807
Olweus D (1994) Bullying at school: basic facts and effects of a school based intervention program. J Child Psychol Psychiatry 35:1171–1190
Rigby K, Slee P (1997) What children tell us about bullying in schools. Child Aust 22:28–34
Dake JA, Price JH, Telljohann SK (2003) The nature and extent of bullying at school. J Sch Health 73:173–180
de Boo GM, Prins PJ (2007) Social incompetence in children with ADHD: possible moderators and mediators in social-skills training. Clin Psychol Rev 27:78–97
Oldehinkel AJ, Verhulst FC, Ormel J (2011) Mental health problems during puberty: tanner stage-related differences in specific symptoms. The TRAILS study. J Adolesc 34:73–85
Bakker MP, Ormel J, Verhulst FC, Oldehinkel AJ (2010) Peer stressors and gender differences in adolescents’ mental health: the TRAILS study. J Adolesc Health 46:444–450
Mikami AY, Hinshaw SP (2003) Buffers of peer rejection among girls with and without ADHD: the role of popularity with adults and goal-directed solitary play. J Abnorm Child Psychol 31:381–397
Humphreys KL, Katz SJ, Lee SS, Hammen C, Brennan PA, Najman JM (2013) The association of ADHD and depression: Mediation by peer problems and parent–child difficulties in two complementary samples. J Abnorm Psychol 122:854
Humphrey JL, Storch EA, Geffken GR (2007) Peer victimization in children with attention-deficit hyperactivity disorder. J Child Health Care 11:248–260
Mrug S, Molina BS, Hoza B, Gerdes AC, Hinshaw SP, Hechtman L, Arnold LE (2012) Peer rejection and friendships in children with attention-deficit/hyperactivity disorder: contributions to long-term outcomes. J Abnorm Child Psychol 40:1013–1026
Roy A, Oldehinkel AJ, Verhulst FC, Ormel J, Hartman CA (2014) Anxiety and disruptive behavior mediate pathways from attention-deficit/hyperactivity disorder to depression. J Clin Psychiatry 75:e108–e113
Huisman M, Oldehinkel AJ, de Winter A, Minderaa RB, de Bildt A, Huizink AC, Verhulst FC, Ormel J (2008) Cohort profile: the Dutch ‘TRacking Adolescents’ Individual Lives’ Survey’; TRAILS. Int J Epidemiol 37:1227–1235
de Winter AF, Oldehinkel AJ, Veenstra R, Brunnekreef JA, Verhulst FC, Ormel J (2005) Evaluation of non-response bias in mental health determinants and outcomes in a large sample of pre-adolescents. Eur J Epidemiol 20:173–181
Ormel J, Oldehinkel AJ, Sijtsema J, van Oort F, Raven D, Veenstra R, Vollebergh WA, Verhulst FC (2012) The TRacking Adolescents’ Individual Lives Survey (TRAILS): design, current status, and selected findings. J Am Acad Child Adolesc Psychiatry 51:1020–1036
Achenbach TM (1991) Manual for the Child Behavior Checklist/4-18 and 1991 profile. University of Vermont, Burlington
Achenbach TM (1991) Manual for the Youth Self-Report and 1991 profile. University of Vermont, Burlington
Achenbach TM, Dumenci L, Rescorla LA (2003) DSM-oriented and empirically based approaches to constructing scales from the same item pools. J Clin Child Adolesc Psychol. 32:328–340
Achenbach TM (1991) Manual for the Teacher’s Report Form and 1991 Profile. University of Vermont, Burlington
Loeber R, Green SM, Lahey BB, Stouthamer-Loeber M (1989) Optimal informants on childhood disruptive behaviors. Dev Psychopathol 1:317–337
Tripp G, Schaughency EA, Clarke B (2006) Parent and teacher rating scales in the evaluation of attention-deficit hyperactivity disorder: contribution to diagnosis and differential diagnosis in clinically referred children. J Dev Behav Pediatr 27:209–218
Kupersmidt JB, Coie JD (1990) Preadolescent peer status, aggression, and school adjustment as predictors of externalizing problems in adolescence. Child Dev 61:1350–1362
Dijkstra JK, Cillessen AH, Lindenberg S, Veenstra R (2010) Same-gender and cross-gender likeability: Associations with popularity and status enhancement: The TRAILS study. J Early Adolesc 30:773–802
Kessler RC, Berglund P, Chiu WT, Demler O, Heeringa S, Hiripi E, Jin R, Pennell BE, Walters EE, Zaslavsky A, Zheng H (2004) The US National Comorbidity Survey Replication (NCS-R): design and field procedures. Int J Methods Psychiatr Res 13:69–92
Kessler RC, Avenevoli S, Green J, Gruber MJ, Guyer M, He Y, Jin R, Kaufman J, Sampson NA, Zaslavsky AM (2009) National comorbidity survey replication adolescent supplement (NCS-A): III. Concordance of DSM-IV/CIDI diagnoses with clinical reassessments. J Am Acad Child Adolesc Psychiatry 48:386–399
Haro JM, Arbabzadeh-Bouchez S, Brugha TS, de Girolamo G, Guyer ME, Jin R, Lepine JP, Mazzi F, Reneses B, Vilagut G, Sampson NA, Kessler RC (2006) Concordance of the Composite International Diagnostic Interview Version 3.0 (CIDI 3.0) with standardized clinical assessments in the WHO World Mental Health surveys. Int J Methods Psychiatr Res 15:167–180
Glass K, Flory K, Hankin BL (2012) Symptoms of ADHD and close friendships in adolescence. J Atten Disord 16:406–417
Sandstrom MJ, Coie JD (1999) A developmental perspective on peer rejection: Mechanisms of stability and change. Child Dev 70:955–966
Sainio M, Veenstra R, Huitsing G, Salmivalli C (2011) Victims and their defenders: a dyadic approach. Int J Behav Dev 35:144–151
Bukowski WM, Laursen B, Hoza B (2010) The snowball effect: friendship moderates escalations in depressed affect among avoidant and excluded children. Dev Psychopathol 22:749–757
Kaltiala-Heino R, Rimpela M, Marttunen M, Rimpela A, Rantanen P (1999) Bullying, depression, and suicidal ideation in Finnish adolescents: school survey. BMJ 319:348–351
Rajendran K, O’Neill S, Halperin JM (2013) Inattention symptoms predict level of depression in early childhood. Postgrad Med 125:154–161
Angold A, Costello EJ, Erkanli A (1999) Comorbidity. J Child Psychol Psychiatry 40:57–87
Hoza B, Pelham WE, Milich R, Pillow D, McBride K (1993) The self-perceptions and attributions of attention deficit hyperactivity disordered and nonreferred boys. J Abnorm Child Psychol 21:271–286
Hoza B, Murray-Close D, Arnold LE, Hinshaw SP, Hechtman L (2010) Time-dependent changes in positively biased self-perceptions of children with attention-deficit/hyperactivity disorder: a developmental psychopathology perspective. Dev Psychopathol 22:375–390
Daviss WB, Diler RS, Birmaher B (2009) Associations of lifetime depression with trauma exposure, other environmental adversities, and impairment in adolescents with ADHD. J Abnorm Child Psychol 37:857–871
Hillegers MH, Burger H, Wals M, Reichart CG, Verhulst FC, Nolen WA, Ormel J (2004) Impact of stressful life events, familial loading and their interaction on the onset of mood disorders Study in a high-risk cohort of adolescent offspring of parents with bipolar disorder. Br J Psychiatry 185:97–101
Surtees PG, Wainwright NW (1999) Surviving adversity: event decay, vulnerability and the onset of anxiety and depressive disorder. Eur Arch Psychiatry Clin Neurosci 249:86–95
Moffitt TE (1993) Adolescence-limited and life-course-persistent antisocial behavior: a developmental taxonomy. Psychol Rev 100:674
Gurkan K, Bilgic A, Turkoglu S, Kilic BG, Aysev A, Uslu R (2010) Depression, anxiety and obsessive-compulsive symptoms and quality of life in children with attention-deficit hyperactivity disorder (ADHD) during three-month methylphenidate treatment. J Psychopharmacol 24:1810–1818
Goodman SH, Lahey BB, Fielding B, Dulcan M, Narrow W, Regier D (1997) Representativeness of clinical samples of youths with mental disorders: A preliminary population-based study. J Abnorm Psychol 106:3
Gaub M, Carlson CL (1997) Gender differences in ADHD: a meta-analysis and critical review. J Am Acad Child Adolesc Psychiatry 36:1036–1045
Hyman SE (2010) The diagnosis of mental disorders: the problem of reification. Annu Rev Clin Psychol 6:155–179
Levy F, Hay DA, McStephen M, Wood C, Waldman I (1997) Attention-deficit hyperactivity disorder: a category or a continuum? Genetic analysis of a large-scale twin study. J Am Acad Child Adolesc Psychiatry 36:737–744
McQuade JD, Hoza B (2008) Peer problems in Attention Deficit Hyperactivity Disorder: current status and future directions. Dev Disabil Res Rev 14:320–324
Nijmeijer JS, Minderaa RB, Buitelaar JK, Mulligan A, Hartman CA, Hoekstra PJ (2008) Attention-deficit/hyperactivity disorder and social dysfunctioning. Clin Psychol Rev 28:692–708
Martin JK, Pescosolido BA, Olafsdottir S, McLeod JD (2007) The construction of fear: Americans’ preferences for social distance from children and adolescents with mental health problems. J Health Soc Behav 48:50–67
Atkinson IM, Robinson JA, Shute RH (1997) Between a rock and a hard place: an Australian perspective on education of children with ADHD. Educ Child Psychol 14:21–30
Chi TC, Hinshaw SP (2002) Mother–child relationships of children with ADHD: the role of maternal depressive symptoms and depression-related distortions. J Abnorm Child Psychol 30:387–400
Bagwell CL, Molina BS, Pelham WE Jr, Hoza B (2001) Attention-deficit hyperactivity disorder and problems in peer relations: predictions from childhood to adolescence. J Am Acad Child Adolesc Psychiatry 40:1285–1292
Mikami AY, Griggs MS, Lerner MD, Emeh CC, Reuland MM, Jack A, Anthony MR (2013) A randomized trial of a classroom intervention to increase peers’ social inclusion of children with attention-deficit/hyperactivity disorder. J Consult Clin Psychol 81:100
Acknowledgments
This research is part of the TRacking Adolescents’ Individual Lives Survey (TRAILS), and was made possible by various grants from the Netherlands Organization for Scientific Research NWO (Medical Research Council program grant GB-MW 940-38-011; ZonMW Brainpower grant 100-001-004; Social Sciences Council medium-sized investment grants GB-MaGW 480-01-006 and GB-MaGW 480-07-001; Social Sciences Council project grant GB-MaGW 452-04-314, NWO large-sized investment grant 175.010.2003.005); the Dutch Ministry of Justice (WODC), the European Science Foundation (EuroSTRESS project FP-006), the University Medical Centre and University of Groningen, the Erasmus University Medical Centre Rotterdam, University of Utrecht, Radboud Medical Centre Nijmegen, and Parnassia Bavo group. We are grateful to all participating adolescents and parents and to everyone who worked on this project and made it possible.
Conflict of interest
This research is part of the TRacking Adolescents’ Individual Lives Survey (TRAILS). Participating centers of TRAILS include various departments of the University Medical Center and University of Groningen, the Erasmus University Medical Center Rotterdam, the University of Utrecht, the Radboud Medical Center Nijmegen, and the Parnassia Bavo group, all in the Netherlands. TRAILS has been financially supported by various grants from the Netherlands Organization for Scientific Research NWO (Medical Research Council program grant GB-MW 940-38-011; ZonMW Brainpower grant 100-001-004; ZonMw Risk Behavior and Dependence grants 60-60600-98-018 and 60-60600-97-118; ZonMw Culture and Health grant 261-98-710; Social Sciences Council medium-sized investment grants GB-MaGW 480-01-006 and GB-MaGW 480-07-001; Social Sciences Council project grants GB-MaGW 457-03-018, GB-MaGW 452-04-314, and GB-MaGW 452-06-004; NWO large-sized investment grant 175.010.2003.005; NWO Longitudinal Survey and Panel Funding 481-08-013); the Sophia Foundation for Medical Research (projects 301 and 393), the Dutch Ministry of Justice (WODC), the European Science Foundation (EuroSTRESS project FP-006), and the participating universities. The authors report no biomedical financial interests or potential conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Roy, A., Hartman, C.A., Veenstra, R. et al. Peer dislike and victimisation in pathways from ADHD symptoms to depression. Eur Child Adolesc Psychiatry 24, 887–895 (2015). https://doi.org/10.1007/s00787-014-0633-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00787-014-0633-9