Abstract
Objectives
The aim of the present study was to assess the cytocompatibility of epoxy resin-based AH Plus Jet (Dentsply De Trey, Konstanz, Germany), Sealer Plus (MK Life, Porto Alegre, Brazil), calcium silicate-based Bio-C Sealer (Angelus, Londrina, PR, Brazil), Sealer Plus BC (MK Life) and AH Plus BC (Dentsply) through a tridimensional (3D) culture model of human osteoblast-like cells.
Methods
Spheroids of MG-63 cells were produced and exposed to fresh root canal sealers extracts by 24 h, and the cytotoxicity was assessed by the Lactate Dehydrogenase assay (LDH). The distribution of dead cells within the microtissue was assessed by fluorescence microscopy, and morphological effects were investigated by histological analysis. The secreted inflammatory mediators were detected in cell supernatants through flow luminometry (XMap Luminex).
Results
Cells incubated with AH Plus Jet, AH Plus BC, Sealer Plus BC and Bio-C Sealer extracts showed high rates of cell viability, while the Sealer Plus induced a significant reduction of cell viability, causing reduction on the spheroid structure. Sealer Plus and Seaker Plus BC caused alterations on 3D microtissue morphology. The AH Plus BC extract was associated with the downregulation of secretion of pro-inflammatory cytokines IL-5, IL-7, IP-10 and RANTES.
Conclusions
The new AH Plus BC calcium silicate-based endodontic sealer did not reduce cell viability in vitro, while led to the downregulation of pro-inflammatory cytokines.
Clinical significance
Choosing the appropriate endodontic sealer is a crucial step. AH Plus BC demonstrated high cell viability and downregulation of pro-inflammatory cytokines, appearing reliable for clinical use, while Sealer Plus presented lower cytocompatibility.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The effectiveness of endodontic treatment relies on various procedures executed with precision. Among these, proper root canal filling stands out as a pivotal step [1]. Leaving empty spaces due to inadequate obturation can jeopardize a positive prognosis, as exudates may migrate to the non-obturated area, perpetuating the inflammatory process [2]. In this context, the role of root canal sealers is to guarantee the proper sealing of gaps between gutta-percha and the walls of the root canal, preventing any potential infiltration of microorganisms.
Endodontic sealers can be categorized based on their chemical composition, being grouped as sealers based on zinc oxide-eugenol, based on calcium hydroxide, based on epoxy resin, and, more recently, calcium silicate-based sealers. Choosing the right endodontic sealer for clinical use is a crucial decision with a profound impact on the treatment’s long-term success.
Cytotoxicity is one of the characteristics of endodontic sealers that can significantly impair the chances of achieving favorable treatment outcomes [3]. Curiously, even AH Plus (Dentsply De Trey, Konstanz, Germany), considered as a gold-standard material for endodontic procedures by many authors, has been reported as presenting cytotoxicity, probably associated with the release of formaldehyde and the degradation of amines, mainly due to its prolonged curing time, necessary to achieve complete polymerization [4,5,6,7]. Cytotoxicity analyses of endodontic sealers often employ traditional two-dimensional (2D) cell culture methods [8]. Nevertheless, the monolayer exposure has intrinsic limitations as it reduces cell-cell and cell-matrix contact, altering the original characteristics of cellular morphology and functionality seen in living tissues [9]. This may be one of the reasons for some discrepancies between clinical and in vitro results [10]. Therefore, alternative methodologies with more proximity to the physiological conditions of exposure are necessary increase the predictivity of in vitro assessments and reduce and the use of experimental animals for research purposes. In this context, three-dimensional (3D) cell culture models represent a promising tool to better emulate in vivo cellular conditions. When cultured in the absence of an attachment surface or scaffold, cell-cell interactions are established through adhesion molecules, following a process called self-assembly. This approach allows for cell growth and cellular functions, including morphogenesis and cellular metabolism [8, 11]. Tridimensional models have been developed from cell cultures of several different cell types and tissue origins, including osteospheres produced from human bone cells [12]. However, these models are not yet fully integrated in the practice of endodontic research.
Therefore, considering the relevance of predictive cytotoxicity assessments in endodontics and the availability of novel in vitro models, this study aimed to: (i) evaluate the cytotoxic effects of different sealers based on epoxy resin (AH Plus Jet and Sealer Plus) or calcium silicate (Bio-C Sealer, Sealer Plus BC and AH Plus BC) and (ii) identify the adequacy of a 3D bone cell culture model to assess different endpoints related to cytocompatibility and its use as a physiologically relevant and predictive in vitro model.
Materials and methods
Cell culture
This study employed human osteoblast-like bone cells from the MG-63 cell line, obtained from the Clinical Research Unit of Antônio Pedro University Hospital, sourced from the Cell Bank of Fluminense Federal University. The cells were cultured in high-glucose DMEM medium (Cultilab, Campinas, SP, Brazil) supplemented with 10% fetal bovine serum (FBS, Gibco-Invitrogen, Grand Island, NY, USA), and two antibiotics, 10,000 IU/mL of penicillin, and 10 mg/mL of streptomycin. Subsequently, the cells were seeded in 96-well culture plates at an initial cell density of 3 × 104 cells per well and incubated at 37 °C under 5% CO2 until reaching 80% of confluence.
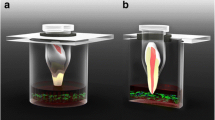
Three-dimensional cell culture
Cellular spheroids were produced as described in Maia-Pinto et al. [13], which involves inhibiting cell adhesion to the plate surface by employing agarose as a non-adherent layer and plate agitation, resulting in a process called self-assembly. Thus, the cells adhere to each other, forming osteospheres. For this, 2 × 104 cells were seeded along with 200 µL of medium in 96-well “v”-bottom microplates coated with 1% agarose (non-adherent) and incubated for 4 days under agitation at 200 rotations per minute in an orbital shaker (Thermo Shaker MS-100, Labgene Scientific SA, Châtel-Saint-Denis, Switzerland) at 37 °C and 5% CO2. The spheroids were evaluated on previous reports concerning sphericity, average size, integrity, and strength [11, 12].
Preparation of extracts from root canal sealers.
The materials, product names, manufacturers and components are listed in Table 1. The endodontic root canal sealers AH Plus Jet (Dentsply), Sealer Plus (MKLife), Bio-C Sealer Sealer (Angelus), Sealer Plus BC (MKLife) and AH Plus BC (Dentsply) were manipulated according to the manufacturers’ instructions, and then test samples were prepared in conditioned media according to ISO 10993-12: 2007 [14]. Briefly, 0.2 g/mL of each root canal sealer and controls was added to serum-free high-glucose DMEM (Cultilab) and incubated for 24 h at 37 °C, 5% CO2 in a humidified chamber. A positive control for maximum release of Lactate Dehydrogenase consisted of 1% Triton, while latex fragments were used as positive control and high-density polystyrene beads as a negative control for cytotoxicity.
Cytotoxicity assay
The enzymatic cytotoxicity test used to indirectly quantify cellular density was based on Lactate Dehydrogenase (LDH) activity. The LDH-P Kit (Wiener Lab, Rosario, Argentina), used in this study, consists of adding the substrates NADH, and pyruvate, which are converted to NAD + and L-lactate, respectively, by LDH. Thus, samples with higher enzymatic activity show lower readings since most of the NADH has been converted to NAD+. For the test, 30 µl of the supernatant from each well was transferred to a flat-bottom 96-well microtiter plate, to which 100 µl of the working solution (single-reagent immediately prepared containing substrates for the LDH enzyme and buffer solution, following Kit protocols) was added per well. The absorbance of the wells was measured at a wavelength of 340 nm on the Microplate Reader (Biotek Inst., Winooski, VT, USA) (after 30 min, with the plate kept at room temperature during these intervals.
Live/dead assay
After the formation of the spheroids, they were exposed to the sealer extracts, as described above, without fetal bovine serum supplementation, for 24 h, and the viability of the spheroids was assessed using the Live and Dead kit (Thermofisher, USA). The spheroids were washed with phosphate buffered saline (PBS) 7.4 at 37ºC and labeled with 40 μm calcein (green, live cells) and 20 μm Ethidium (red, dead), and incubated at 37ºC for 40 min. Images were obtained on a Axio A1 Observer fluorescence microscope (Zeiss, Germany).
Morphological analysis
To evaluate the morphological structure of the spheroids, after exposure for 24 h of the extracts, they were fixed with 3.7% formaldehyde for 1 h. The samples were labeled with eosin and embedded in Tissue-Tek OCT Compound Medium, (Sakura Finetek, USA). After freezing, the samples were sliced in a Leica CM350s cryostat microtome (Leica, USA) with a thickness of 7 μm, and positioned on labeled slides. The samples were then stained with hematoxylin and eosin to evaluate the structural morphology of the cellular spheroids, and observed using Axio A1 Observer microscope (Zeiss, Germany).
Detection of cytokines and growth factors
The determination of the concentration of cytokines and growth factors secreted after incubation with root canal sealers and controls extracts contact was performed through the multiparametric test using magnetic microsphere XMap Luminex. A commercial kit (27 Plex panel, BioRad, California, USA) was employed to quantify interleukin (IL) IL-6, IFN-gamma, IL-1RA, GM-CSF, G-CSF, TNF-alpha, RANTES, Eotaxin, FGF2, VEGF, PDGF, IP-10, MCP-1, MIP-1a, MIP-1b, IL-1beta, IL-2, IL-5, IL-7, IL-8, IL-9, IL-10, IL-15, IL-12 (p70), and IL-17 A. The magnetic beads were quantified using a BioPlex MAGPIX system (BioRad). This pre-selected panel includes representatives of the main categories of inflammatory mediators with impact on the response to biomaterials, including pro- and anti-inflammatory cytokines, chemokines and growth factors. The results were analyzed using Xponent software v. 3.0 (Luminexcorp, USA).
Statistical analysis
The data had their normal distribution assessed by the D`Agostino & Pearson test. For cytotoxicity one-way Analysis of Variance (ANOVA) was employed. To analyze differences between groups on the secretion of cytokines and growth factors, Kruskal-Wallis test and Dunn’s posttest were used. For all analyses, GraphPad Prism 7.0 software (GraphPad Inc, USA) was used and p < 0.05 was considered statistically significant.
Results
Figure 1 shows the results for the cytotoxicity assay of the different tested sealers through the LDH assay. It is possible to observe that the three-dimensional model responded as expected to the negative control (polystyrene beads), which presented no significant difference from the unexposed cells (p > 0.05), and the positive controls (1% Triton and latex), which presented high cytotoxicity. Concerning the tested groups, Sealer Plus was the only endodontic root canal sealer that showed significantly lower cell viability (p > 0.05), with similar values to the positive controls. AH Plus Jet, Bio-C Sealer, Sealer Plus BC, and AH Plus BC did not exhibit significant differences relative to each other nor to the negative control, demonstrating high cell viability.
Cell viability of three-dimensional culture of MG-63 spheroids exposed to the different sealers by 24 h, as measured through the release of lactate dehydrogenase by cells with compromised membranes (LDH assay). Results are represented as mean and Standard deviation of the percentage relative to the unexposed control group. An asterisk indicates significant difference from the other experimental groups (p < 0.05)
A second assessment was performed with a fluorescence-based live and dead assay, aiming to qualitatively observe the distribution of living (green stain) and dead (red stain) cells within the microtissue environment, as shown in Fig. 2. It is possible to confirm the high level of cell survival in the spheroids exposed to biocompatible polystyrene beads (C-, first panel). Exposure to 1% triton X100, as a positive control, confirmed a high level of cell death, with the total predominance of red staining along the hole microtissue. On the other hand, spheroids exposed to extracts of latex presented a reduced size, and were less compact than the negative control, suggesting the loss of integrity and the shedding of cells from the microtissue surface. Regarding the test materials, spheroids exposed to AH Plus and AH Plus BC presented predominantly living cells, although with a less compact appearance. Bio-C Sealer and Sealer Plus BC presented evidence of dead cells only in the spheroid surface. Sealer Plus, however, induced effects visually similar to latex, with reduction on green staining and indications of cell death and shedding from the microtissue (Fig. 2).
Cell viability as revealed by a fluorescent live/dead assay from the 3D model exposed to the different sealers. Cells were stained with calcein (living cells, green) and ethidium (dead cells, red). Extracts of polystyrene beads were used as negative control, while extracts of latex fragments and 1% Triton X100 were employed as positive, cytotoxic controls. The bar indicates 100 micrometers
In order to observe such structural effects on the inner organization of the microtissues after exposure to the sealers, a histological assessment was performed, with results shown in Fig. 3. Exposure to negative control (Fig. 3A) shows, as expected, intact spheroids of around 200 micrometers, with intense cell-cell interaction, the absence of evidence of a necrotic core, and a more compact cell layer on their periphery. Exposure to extracts of latex (Fig. 3B) induced a dramatic reduction in size, with a shape suggesting heavy loss of cells and structural integrity. Even tough with a different pattern, exposure to Triton X100 (Fig. 3C) also presented obvious loss of integrity, with dismantlement of the originally compact microtissue organization. Regarding the tested sealers, spheroids exposed to AH Plus BC (Fig. 3H) presented a rather intact structure, with most characteristics of the control group preserved, while microtissues exposed to AH Plus (Fig. 3D) and Bio-C Sealer (Fig. 3E) presented a loose, less compact organization. MG-63 spheroids exposed to Sealer Plus (Fig. 3F) and Sealer Plus BC (Fig. 3G) presented patterns more similar to the positive controls, with evidence of disaggregation and reduction in size and shape.
Morphological evaluation of the histological structure of spheroids exposed to sealer extracts for 24 h. (A) polystyrene beads (negative control); (B) latex fragments (positive control); (C) 1% Triton X100 (positive control), (D) AH Plus; (E) Bio C Sealer; (F) Sealer Plus (G) Sealer Plus BC; (H) AH Plus BC
To assess the effects of the tested sealers on the release of inflammatory mediator by the MG-63 spheroids, a multiparametric assay was performed investigating the conditioned media of the exposed microtissues during the cytotoxicity tests. Figure 4 shows a heatmap showing the secretion profile of all 27 analytes in all groups tested, relative to the negative control. The secretion of pro-inflammatory interleukins IL-5, IL-7, IP-10 and RANTES was significantly lower for AH Plus BC as compared to the negative control (Fig. 5A-D). IL-1beta secretion was higher after incubation with AH Plus when compared to AH Plus BC extract (Fig. 5E). On the other hand, IL-15 levels were lower after incubation with AH Plus BC extract relative to the positive control (latex) (Fig. 5F). Regarding anti-inflammatory interleukins, IL-1RA secretion was lower in cells incubated with AH Plus BC relative to the negative control (Fig. 5G). Finally, the levels of the growth factor FGF2 was significantly higher after incubation with Sealer Plus relative to Sealer Plus BC (Fig. 5H).
Comparison of inflammatory mediators released by MG-63 spheroids after 24 h exposure to extracts of epoxy resin-based and calcium silicate-based endodontic sealers. The results show mean concentration and standar deviation of the pro-inflammatory interleukins (A) IL-5, (B) IL-7, (C) IP-10, (D) RANTES, (E) IL-1beta and (F) IL-15, as well as the anti-inflammatory interleukins (G) IL-1RA and (H) FGF2. An asterisk indicates significant difference between groups
Discussion
During obturation, sealers may extrude into the periradicular tissues, which can increase the risk of non-healing by 32% [15]. In the search for the best sealer to be used in the final phase of endodontic treatment, this study evaluated AH Plus, Sealer Plus, Bio-C Sealer, Sealer Plus BC and AH Plus BC, regarding different cytocompatibility parameters, including membrane integrity, cell-cell-matrix interactions, and the release of inflammatory mediators. This analysis is justified due to potential cytotoxic effects on human cells, which can compromise membrane integrity based on the chemical composition. Additionally, it may lead to inflammation and DNA damage, resulting in genomic instability and carcinogenic risks [16, 17].
The elutes originating from endodontic sealers could potentially expose periradicular tissues and hinder the process of wound healing [18]. Therefore, the adequate and predictive cytotoxicity analysis of freshly mixed sealers is relevant since the incomplete polymerization stage form in which they are inserted into the root canal system may increase the release of soluble toxicants [19]. In this sense, indirect contact between biomaterials and cells was utilized, following guidance from international standards (ISO 10993-12:2018) [20], to guide the preparation of the biomaterial extracts, aiming to harmonization and reducing experimental errors. This method is employed by most studies examining the cytotoxicity of endodontic sealers, as it simulates the release of soluble toxicants into periapical tissues [10, 21,22,23,24].
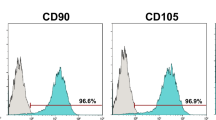
Human bone cells are considered interesting for cytocompatibility assays, as they could play a crucial role in the healing of apical tissues, due direct interaction with biomaterials, including sealers [25, 26]. The present study was conducted employing an in vitro model from human osteoblast-like cells derived from the osteosarcoma MG-63 cell line. These cells are commonly employed as an experimental model for bone cells due to their well-known similarity to primary human osteoblasts. It is important to notice that these are not normal osteoblasts, as these are transformed aneuploid cells from a tumoral origin. However, while they present morphological variations and a shorter duplication time as compared to primary osteoblasts, these cells exhibit the key biological markers of osteoblast behavior, and are regulated by similar differentiation regulatory pathways, and can generate a mineralized matrix when appropriately stimulated, as well as a similar response to endodontic materials, regarding cytotoxicity [27,28,29]. In exchange from the limitations of their origin, the use of cell lines in toxicological studies offers several advantages, as they provide more homogeneous and stable cultures, with consistency of results across different experiments and studies. Their availability (in both quantity and easy obtention from cell banks) allow the cost-effective use in large quantities for long-term studies without the ethical concerns associated with primary cell extraction from living organisms [30].
These cells were used to produce a three-dimensional cell culture model, as proposed previously [11], aiming to improve the exposure to test materials in conditions more similar to the physiological environment, including increased cell-cell-matrix interactions [31]. The structural monolayer format of 2D cell cultures bears little physical resemblance to tissue complexity, potentially leading to increased susceptibility to toxins and inadequate immune reactions. Additionally, higher cytotoxic effects for analyses using 2D cell culture models when compared to 3D are often reported [32, 33]. The osteosphere 3D model has been shown as effective for the evaluation of osteoconductivity and biocompatibility of scaffolds and biomaterials, even though with some limitations in the use of some colorimetric cytotoxicity assays such as MTT, due to the difficulty of dye extraction, while with a good performance with test such as LDH assay [12, 13, 34].
Employing this methodology, the results confirm AH Plus, considered by many authors as a gold-standard material, as presenting a good cytocompatibility. Even though such in vitro biocompatibility would be expected due to its performance by many reports, it also opposes a few in vitro studies identifying toxicity for this epoxy-resin based sealer using conventional 2D cell culture [4,5,6,7]. In fact, tridimensional models have already been used in evaluations including AH Plus, confirming its good performance, even though with models very different from the osteosphere methodology hereby presented, either due to the choice for animal cells, or the use of collagen scaffolds [9]. The present 3D model also allowed to verify that exposure to AH Plus does not affect importantly the morpophology of microtissue organization of these bone cells, resulting from cell-cell interactions.
A significant decrease in cell viability was observed when Sealer Plus, also an epoxy resin-based material, was employed. Despite the addition of calcium hydroxide in an attempt to reduce its cytotoxicity [35], toxic byproducts such as formaldehyde are released during setting, in addition to the presence of phenolic compounds in the paste composition [19], which may possibly explain the decrease in cell viability. The literature employing 2D cell culture presents some controversy regarding the in vitro toxicity of this material, as some authors report cytotoxic effects for this sealer after 24 h of exposure [19], while others identify good cytocompatibility for Sealer Plus [36]. These discrepancies might be a result of methodological differences such as the use of different cell lines, sample configurations. In this sense, the present results provide an insight in the toxical effects of Sealer Plus, as they are confirmed both by the cytotoxicity assessment, and by effects on the organization and integrity of the exposed microtissues in the fluorescence and histological analyses of the human bone cell spheroids.
In contrast, the calcium silicate-based root canal sealers demonstrated a high rate of cell viability in the LDH assay, including Bio-C Sealer, Sealer Plus BC and the new bioceramic AH Plus BC, whose cytocompatibility is reported for the first time using three-dimensional cell culture. This is a very interesting result when compared to findings from randomized clinical trials demonstrating that bioceramic sealers, while presenting lower extrusion than epoxy-resin sealers such as AH Plus, produce similar low post-operative endodontic pain as compared to the gold-standard material [37, 38]. Regarding AH Plus BC, the present study confirms a recent report showing very good responses by both human gingival fibroblasts and macrophages in conventional cell culture, showing the absence of cytotoxicity and genotoxicity for this material [39]. Bioceramic endodontic sealers are expected to exhibit good biological properties, evidenced by the release of calcium and silicate ions that participate in the healing process [40]. Furthermore, they feature calcium phosphate, augmenting their setting characteristics and yielding a substance with a chemical composition and crystalline structure akin to apatite materials found in teeth and bones. This similarity enhances the bonding between the sealer and the root dentin, thereby improving overall dental sealing efficacy [41]. In addition, it also possesses traits that potentialize the repair of periapical tissues when in contact with bacterial toxins [42]. Nevertheless, it is important to notice that the present histological evaluation of the microtissue shows some morphological effects induced by exposure to Sealer Plus BC that should be further investigated in future studies.
It’s noteworthy that both in vitro and in vivo studies have revealed the immunomodulatory impact of various endodontic sealers [43]. Cytokines and growth factors have been recognized as significant contributors to the onset of inflammatory diseases. Additionally, these mediators play a crucial role in promoting tissue regeneration, a process closely associated with wound healing [44]. This study confirmed the secretion of inflammatory mediators by cells exposed to different endodontic sealers, mainly the downregulation of the pro-inflammatory cytokines IL-5, IL-7, IP-10 and RANTES, by AH Plus BC.
IL-5 seems to be linked to eosinophil maturation, activation, and survival associated with the humoral immune response, similar to IL-7 that plays a crucial role in the immune system regulation and in inflammation [45, 46]. While IP-10 and RANTES play a relevant role in the pathogenesis of periapical inflammatory lesions, including in the evolution from granulomas to cysts [47,48,49]. The downregulation of pro-inflammatory cytokines by calcium silicate-based sealers has been show before, corroborating our findings [24]. Additionally, the epoxy resin-based AH Plus Jet upregulated the release of IL-1beta, an important mediator of bone resorption [50], compared with AH Plus BC, another interesting indicator of the upgraded properties of this material.
Among the limitations of the present study, we could point that the proposed model represents only one step towards the approximation with a physiological environment of clinical relevance. Therefore, several variables, such as variations in pH, variations in oxygen levels, or the patients’ immune response, that affect the results observed under clinical conditions, may not be predicted by such an in vitro model [51]. In this sense, future technologies including the combination of multiple microtissues with microfluidic dynamic systems may contribute to increase the predictivity and the role of in vitro tests for initial screening of biomaterials, minimizing the use of animal models [52]. Nevertheless, in the present study, the 3D model presented interesting results in the investigation of cell viability, tissue integrity and cytokine production, and may contribute to a deeper understanding of the biological properties exhibited by the examined sealers, since the clinical characteristics of endodontic sealers may be directly linked to their physicochemical and biological properties [7]. The results demonstrated the biocompatibility of most tested sealers, regardless of their epoxy-resin or ceramic composition, except for Sealer Plus. This finding could be critical considering the potential of a cytotoxic sealer to cause tissue irritation, adverse effects on local repair mechanisms, and possible clinical failure [21]. Conversely, the recently launched AH Plus BC not only exhibited robust biocompatibility but also exhibited a decrease in the production of pro-inflammatory cytokines, a feature that may contribute to mitigate an initial inflammatory response during endodontic procedures.
Conclusions
The epoxy resin-based sealer AH Plus and the calcium silicate sealers AH Plus BC, BioC Sealer and Sealer Plus BC presented good cytocompatibility, as they did not induce considerable cytotoxicity, neither affected negatively cell microtissue morphology or the secretion of inflammatory mediators by human bone cells. Furthermore, the newly developed calcium silicate-based endodontic sealer AH Plus BC promoted lower secretion of pro-inflammatory mediators.
The three-dimensional cell culture model employed in this study presented itself as an interesting tool for the assessment of in vitro biocompatibility of root canal sealers, as it allowed a robust platform for quantitative and qualitative assessments of cytotoxicity, release of inflammatory mediators, besides the distribution of cell death and morphological effects within a microtissue environment with increased cell-cell-matrix interactions.
Data availability
No datasets were generated or analysed during the current study.
References
Nair PN (2006) On the causes of persistent apical periodontitis: a review. Int Endod J. 2006 39(4):249 – 81. https://doi.org/10.1111/j.1365-2591.2006.01099.x
Pinheiro BC, Bramante AS, Hussne RP (2003) Influence of the penetration of instruments, used in the active lateral condensation, in the quality of root canal filling. J Appl Oral Sci 11(3):186–191. https://doi.org/10.1590/s1678-77572003000300006
Komabayashi T, Colmenar D, Cvach N, Bhat A, Primus C, Imai Y (2020) Comprehensive review of current endodontic sealers. Dent Mater J 29(5):703–720. https://doi.org/10.4012/dmj.2019-288
Miletić I, Devcić N, Anić I, Borcić J, Karlović Z, Osmak M (2005) The cytotoxicity of RoekoSeal and AH plus compared during different setting periods. J Endod 31(4):307–309. https://doi.org/10.1097/01.don.0000140570.95688.ee
Silva EJ, Accorsi-Mendonça T, Almeida JF, Ferraz CC, Gomes BP, Zaia AA (2012) Evaluation of cytotoxicity and up-regulation of gelatinases in human fibroblast cells by four root canal sealers. Int Endod J 45(1):49–56. https://doi.org/10.1111/j.1365-2591.2011.01946.x
Jung S, Sielker S, Hanisch MR, Libricht V, Schäfer E, Dammaschke T (2018) Cytotoxic effects of four different root canal sealers on human osteoblasts. PLoS ONE 26(3):e0194467. https://doi.org/10.1371/journal.pone.0194467
Souza LC, Neves GST, Kirkpatrick T, Letra A, Silva R (2023) Physicochemical and Biological properties of AH Plus Bioceramic. J Endod 49(1):69–76. https://doi.org/10.1016/j.joen.2022.10.009
Gaudin A, Tolar M, Peters OA (2020) Cytokine Production and Cytotoxicity of Calcium Silicate-based Sealers in 2- and 3-dimensional Cell Culture Models. J Endod 46(6):818–826. https://doi.org/10.1016/j.joen.2020.03.011. Epub
da Silva EJNL, Zaia AA, Peters OA (2017) Cytocompatibility of calcium silicate-based sealers in a three-dimensional cell culture model. Clin Oral Investig 21(5):1531–1536. https://doi.org/10.1007/s00784-016-1918-9
Scelza MZ, Linhares AB, da Silva LE, Granjeiro JM, Alves GG (2012) A multiparametric assay to compare the cytotoxicity of endodontic sealers with primary human osteoblasts. Int Endod J 45(1):12–18. https://doi.org/10.1111/j.1365-2591.2011.01941.x
Restle L, Costa-Silva D, Lourenço ES, Bachinski RF, Batista AC, Linhares ABR, Alves GG (2015) A 3D osteoblast in vitro model for the evaluation of biomedical materials. Adv Mater Sci Eng. https://doi.org/10.1155/2015/268930
Brochado ACB, Silva DC, Silva JCd, Lowenstein A, Gameiro VS, Mavropoulos E, Mourão CF, Alves GG (2023) Characterization and applicability of a bone spheroid model for the evaluation of cytocompatibility of bone substitutes. Appl Sci 13(3):1602. https://doi.org/10.3390/app13031602
Maia-Pinto MOC, Brochado ACB, Teixeira BN, Sartoretto SC, Uzeda MJ, Alves ATNN, Alves GG, Calasans-Maia MD, Thiré RMSM (2020) Biomimetic mineralization on 3D printed PLA scaffolds: on the response of human primary osteoblasts spheroids and in vivo implantation. Polym (Basel) 13(1):74. https://doi.org/10.3390/polym13010074
ISO International Organization for Standardization (2007) ISO 10993-12:2007 Biological evaluation of Medical Devices—Part 12: Sample Preparation and Reference materials. International Organization for Standardization, Geneva
Aminoshariae A, Kulild JC (2020) The impact of sealer extrusion on endodontic outcome: a systematic review with meta-analysis. Aust Endod J 46(1):123–129. https://doi.org/10.1111/aej.12370
Teixeira ABV, Moreira NCS, Takahashi CS, Schiavon MA, Alves OL, Reis AC (2021) Cytotoxic and genotoxic effects in human gingival fibroblast and ions release of endodontic sealers incorporated with nanostructured silver vanadate. J Biomed Mater Res B Appl Biomater 109(9):1380–1388. https://doi.org/10.1002/jbm.b.34798
Shokrzadeh M, Motafeghi FS, Lotfizadeh A, Ghorbani M, Haddadi Kohsar A (2023) Cytotoxicity and mineralization activity of Calcium Silicate-based Root Canal Sealers compared to Conventional Resin-based Sealer in Human Gingival Fibroblast cells. Int J Dent. https://doi.org/10.1155/2023/4376579. 31;2023:4376579
Brackett MG, Lewis JB, Messer RL, Lei L, Lockwood PE, Wataha JC (2011) Dysregulation of monocytic cytokine secretion by endodontic sealers. J Biomed Mater Res B Appl Biomater 97(1):49–57. https://doi.org/10.1002/jbm.b.31785
Silva EJ, Hecksher F, Vieira VT, Vivan RR, Duarte MA, Brasil SC, Antunes HS (2020) Cytotoxicity, antibacterial and physicochemical properties of a new epoxy resin-based endodontic sealer containing calcium hydroxide. J Clin Exp Dent 1;12(6):e533-e539. https://doi.org/10.4317/jced.56534
ISO International Organization for Standardization (2018) ISO 10993-12:2018 Biological evaluation of Medical Devices—Part 12: Sample Preparation and Reference materials. International Organization for Standardization, Geneva
Vouzara T, Dimosiari G, Koulaouzidou EA, Economides N (2018) Cytotoxicity of a New Calcium Silicate Endodontic Sealer. J Endod 44(5):849–852. https://doi.org/10.1016/j.joen.2018.01.015
Yang X, Zheng T, Yang N, Yin Z, Wang W, Bai Y (2022) A review of the research methods and progress of biocompatibility evaluation of root canal sealers. Aust Endod J 49 Suppl 1508–514. https://doi.org/10.1111/aej.12725
Jung S, Libricht V, Sielker S, Hanisch MR, Schäfer E, Dammaschke T (2019) Evaluation of the biocompatibility of root canal sealers on human periodontal ligament cells ex vivo. Odontology 107(1):54–63. https://doi.org/10.1007/s10266-018-0380-3
Lee BN, Hong JU, Kim SM, Jang JH, Chang HS, Hwang YC, Hwang IN, Oh WM (2019) Anti-inflammatory and Osteogenic Effects of Calcium Silicate-based Root Canal Sealers. J Endod 45(1):73–78. https://doi.org/10.1016/j.joen.2018.09.006
Zhu Q, Haglund R, Safavi KE, Spangberg LS (2000) Adhesion of human osteoblasts on root-end filling materials. J Endod 26(7):404–406. https://doi.org/10.1097/00004770-200007000-00006
Pautke C, Schieker M, Tischer T, Kolk A, Neth P, Mutschler W, Milz S (2004) Characterization of osteosarcoma cell lines MG-63, Saos-2 and U-2 OS in comparison to human osteoblasts. Anticancer Res 24(6):3743–3748
Czekanska EM, Stoddart MJ, Ralphs JR, Richards RG, Hayes JS (2014) A phenotypic comparison of osteoblast cell lines versus human primary osteoblasts for biomaterials testing. J Biomed Mater Res A 102(8):2636–2643. https://doi.org/10.1002/jbm.a.34937
de Lima Barbosa R, Rodrigues Santiago Rocha N, Stellet Lourenço E, de Souza Lima VH, Mavropoulos E, Mello-Machado RC, Spiegel C, Mourão CF, Alves GG (2024) The Association of Nanostructured Carbonated Hydroxyapatite with denatured albumin and platelet-rich fibrin: impacts on growth factors release and osteoblast behavior. J Funct Biomater 5(1):18. https://doi.org/10.3390/jfb15010018
Staehlke S, Rebl H, Finke B, Mueller P, Gruening M, Nebe JB (2018) Enhanced calcium ion mobilization in osteoblasts on amino group containing plasma polymer nanolayer. Cell Biosci 21:8:22. https://doi.org/10.1186/s13578-018-0220-8
Chalak M, Hesaraki M, Mirbahari SN, Yeganeh M, Abdi S, Rajabi S, Hemmatzadeh F (2024) Cell immortality: in Vitro Effective techniques to achieve and investigate its Applications and challenges. Life (Basel) 21(143):417. https://doi.org/10.3390/life14030417
da Silva EJNL, de Carvalho NK, Zaia AA (2016) Cytotoxicity profile of epoxy resin sealer provided by a new experimental 3D cell culture model. ENDO 10(1)
Wataha JC, Nakajima H, Hanks CT, Okabe T (1994) Correlation of cytotoxicity with element release from mercury- and gallium-based dental alloys in vitro. Dent Mater 10(5):298–303. https://doi.org/10.1016/0109-5641(94)90037-x
Silva EJ, Carvalho NK, Ronconi CT, De-Deus G, Zuolo ML, Zaia AA (2016) Cytotoxicity Profile of Endodontic Sealers provided by 3D cell culture experimental model. Braz Dent J 27(6):652–656. https://doi.org/10.1590/0103-6440201600792
Brochado ACB, de Souza VH, Correa J, Dos Anjos SA, de Almeida Barros Mourão CF, Cardarelli A, Montemezzi P, Gameiro VS, Pereira MR, Mavropoulos E, Alves GG (2021) Osteosphere Model to Evaluate Cell-Surface Interactions of Implantable Biomaterials. Materials (Basel) 7;14(19):5858. https://doi.org/10.3390/ma14195858
Piai GG, Duarte MAH, Nascimento ALD, Rosa RAD, Só MVR, Vivan RR (2018) Penetrability of a new endodontic sealer: a confocal laser scanning microscopy evaluation. Microsc Res Tech 81(11):1246–1249. https://doi.org/10.1002/jemt.23129
Cintra LTA, Benetti F, de Azevedo Queiroz ÍO, Ferreira LL, Massunari L, Bueno CRE, de Oliveira SHP, Gomes-Filho JE (2017) Evaluation of the cytotoxicity and biocompatibility of New Resin Epoxy-based Endodontic Sealer Containing Calcium Hydroxide. J Endod 43(12):2088–2092. https://doi.org/10.1016/j.joen.2017.07.016
Seron MA, Nunes GP, Ferrisse TM, Strazzi-Sahyon HB, Victorino FR, Dos Santos PH, Gomes-Filho JE, Cintra LTA, Sivieri-Araujo G (2023) Postoperative pain after root canal filling with bioceramic sealers: a systematic review and meta-analysis of randomized clinical trials. Odontology 111(4):793–812. https://doi.org/10.1007/s10266-023-00830-z
Mendes AT, Weissheimer T, Tietz L, Só BB, Só GB, da Rosa RA, Só MVR (2023) Postoperative pain incidence and intensity following root canal obturation with bioceramic and other sealers: a systematic review with meta-analysis. J Den Res Dentistry 11(2):32–51
Radwanski M, Rozpedek-Kaminska W, Galita G, Siwecka N, Sokolowski J, Majsterek I, Özcan M, Lukomska-Szymanska M (2024) Cytotoxicity and genotoxicity of bioceramic root canal sealers compared to conventional resin-based sealer. Sci Rep 19(1):4124. https://doi.org/10.1038/s41598-024-54726-1
Kwak SW, Koo J, Song M, Jang IH, Gambarini G, Kim HC (2023) Physicochemical Properties and Biocompatibility of various Bioceramic Root Canal Sealers: in Vitro Study. J Endod 49(7):871–879. https://doi.org/10.1016/j.joen.2023.05.013
Khalil I, Naaman A, Camilleri J (2016) Properties of Tricalcium Silicate Sealers. J Endod. 2016;42(10):1529-35. https://doi.org/10.1016/j.joen.2016.06.002
Martorano AS, Messias NS, Bighetti-Trevisan RL, de Oliveira PT, de Castro Raucci LMS, Raucci Neto W (2022) In vitro inflammatory modulation of bioceramic endodontic sealer in macrophages stimulated by bacterial lipopolysaccharide. Int Endod J 56(2):213–226. https://doi.org/10.1111/iej.13858
Guo J, Peters OA (2023) Hosseinpour S. Immunomodulatory Effects of Endodontic Sealers: A Systematic Review. Dent J (Basel). 2023;11(2):54. https://doi.org/10.3390/dj11020054
Tyler LW, Matossian K, Todd R, Gallagher GT, White RR, Wong DT (1999) Eosinophil-derived transforming growth factors (TGF-alpha and TGF-beta 1) in human periradicular lesions. J Endod 25(9):619–624. https://doi.org/10.1016/S0099-2399(99)80322-7
Andreev D, Kachler K, Liu M, Chen Z, Krishnacoumar B, Ringer M, Frey S, Krönke G, Voehringer D, Schett G, Bozec A (2024) Eosinophils preserve bone homeostasis by inhibiting excessive osteoclast formation and activity via eosinophil peroxidase. Nat Commun 15(1):1067. https://doi.org/10.1038/s41467-024-45261-8
Acheampong I, Minadzi D, Adankwah E, Aniagyei W, Vivekanandan MM, Yeboah A, Arthur JF, Lamptey M, Abass MK, Kumbel F, Osei-Yeboah F, Gawusu A, Laing EF, Batsa Debrah L, Owusu DO, Debrah A, Mayatepek E, Seyfarth J, Phillips RO, Jacobsen M (2023) Diminished Interleukin-7 receptor expression on T-cell subsets in tuberculosis patients. Hum Immunol 84(10):543–550. https://doi.org/10.1016/j.humimm.2023.08.141
Kwak HB, Ha H, Kim HN, Lee JH, Kim HS, Lee S, Kim HM, Kim JY, Kim HH, Song YW, Lee ZH (2008) Reciprocal cross-talk between RANKL and interferon-gamma-inducible protein 10 is responsible for bone-erosive experimental arthritis. Arthritis Rheum 58(5):1332–1342. https://doi.org/10.1002/art.23372
Hadziabdic N, Kurtovic-Kozaric A, Frkatovic A, Smajlovic S, Letra A (2019) Quantitative analysis of CCL5 and ep300 in Periapical Inflammatory lesions. Acta Med Acad 48(2):129–139. https://doi.org/10.5644/ama2006-124.251
Silva TA, Garlet GP, Lara VS, Martins W Jr, Silva JS, Cunha FQ (2005) Differential expression of chemokines and chemokine receptors in inflammatory periapical diseases. Oral Microbiol Immunol 20(5):310–316. https://doi.org/10.1111/j.1399-302X.2005.00232.x
Gomes-Filho JE, Watanabe S, Gomes AC, Faria MD, Lodi CS, Penha Oliveira SH (2009) Evaluation of the effects of endodontic materials on fibroblast viability and cytokine production. J Endod 35(11):1577–1579. https://doi.org/10.1016/j.joen.2009.07.022
Sanz JL, Guerrero-Gironés J, Pecci-Lloret MP, Pecci-Lloret MR, Melo M (2021) Biological interactions between calcium silicate-based endodontic biomaterials and periodontal ligament stem cells: a systematic review of in vitro studies. Int Endod J 54(11):2025–2043. https://doi.org/10.1111/iej.13600
Hosseinpour S, Gaudin A, Peters OA (2022) A critical analysis of research methods and experimental models to study biocompatibility of endodontic materials. Int Endod J 55 Suppl 2(Suppl 2):346–369. https://doi.org/10.1111/iej.13701
Funding
This work was supported by the Brazilian agencies CAPES, FAPERJ and CNPq.
Author information
Authors and Affiliations
Contributions
M.F.Z.S. was responsible for Conceptualization, Investigation, Writing - Review & Editing, Supervision and Project administration. S.J.O.T., G.S.R., J.D. and P.E.C.L. participated in the execution of the Methodology, Data Curation and Formal analysis. S.J.O.T. also participated in Investigation and Writing - Original Draft. L.R.L.A. and L.R. captured Resources and did Validation and Visualization. P.S. did Formal analysis, Validation and Visualization. S.C.S. participate in the use of Software, Formal analysis and executed Writing - Review & Editing. G.G.A. did Formal analysis, Validation and Visualization, Revised and supervised the Methodology and executed Writing - Review & Editing.
Corresponding author
Ethics declarations
Conflict of interest
The authors deny any conflicts of interest.
Ethical approval
Not applicable.
Informed consent
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Scelza, M.F., Tavares, S.J., Scelza, P. et al. A three-dimensional cell culture approach to investigate cytotoxic effects and production of inflammatory mediators by epoxy resin-based and calcium silicate-based endodontic sealer. Clin Oral Invest 28, 344 (2024). https://doi.org/10.1007/s00784-024-05743-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00784-024-05743-x