Abstract
Objectives
This in vitro study is aimed at assessing whether implant primary stability is influenced by implant length in artificial bone with varying densities.
Materials and methods
A total of 120 truncated-conical implants (60 long-length: 3p L, 3.8 × 14 mm; 60 short-length: 3p S, 3.8 × 8 mm) were inserted into 20, 30, and 40 pounds per cubic foot (PCF) density polyurethane blocks. The insertion torque (IT), removal torque (RT), and resonance frequency analysis (RFA) values were recorded for each experimental condition.
Results
In 30 and 40 PCF blocks, 3p S implants exhibited significantly higher IT values (90 and 80 Ncm, respectively) than 3p L (85 and 50 Ncm, respectively). Similarly, RT was significantly higher for 3p S implants in 30 and 40 PCF blocks (57 and 90 Ncm, respectively). However, there were no significant differences in RFA values, except for the 20 PCF block, where 3pS implants showed significantly lower values (63 ISQ) than 3p L implants (67 ISQ) in both the distal and mesial directions.
Conclusions
These results demonstrated that the implant’s length mainly influences the IT and RT values in the polyurethane blocks that mimic the mandibular region of the bone, resulting in higher values for the 3p S implants, while the RFA values remained unaffected. However, in the lowest density block simulating the maxillary bone, 3p L implants exhibited significantly higher ISQ values.
Clinical relevance
Therefore, our data offer valuable insights into the biomechanical behavior of these implants, which could be clinically beneficial for enhancing surgical planning.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Primary stability is considered a crucial factor for achieving dental implants osseointegration after their insertion, and it seems to be related to the level of primary bone contact [1]. Moreover, primary stability is known to be influenced by the diameter, length, type of coils, and surface micro-morphology of the implant type, in addition to the volumetric density and/or trabecular connectivity of bone, as well as the thickness and density of the cortical layer [2,3,4,5]. It is also related to the absence of mobility in the axial, lateral, and rotational directions in the surrounding bone immediately after implant placement [6]. Indeed, as an example, in an animal model, it was demonstrated that implants mobile at placement had a 3-year cumulative survival rate of 79.8% compared to 93.4% of implants that were stable at placement [7]. Furthermore, the presence of a high primary stability also allows the immediate loading of implants by reducing the number of surgical interventions and patient discomfort [8].
Primary stability has long been achieved through bicorticalism using implant lengths up to 20 mm. As a matter of fact, increasing the implant length above 10 mm allows to decrease bone stress and increase the stability of implants when inserted into a low-quality bone, such as type IV bone [6, 9]. Some studies documented that short-length implants (<10 mm in length) have a 2.5 times higher risk of failure than long-length implants placed in the posterior jaws with poor bone quality [10, 11].
Nonetheless, conflicting results currently exist, as several studies showed that implant length does not appear to significantly influence the implant survival rate [12,13,14], also proving that short-length (8 mm) cone-blocking implants supporting single crowns could show a 10-year cumulative survival rate of 98.5% in the posterior regions [15, 16]. Moreover, other authors demonstrated that short-length implants could be a viable alternative to sinus floor elevation in the posterior maxilla with severe bone resorption or that they could be used to perform a one-stage maxillary sinus lifting with high survival rates (98.55%) also after 3 years, even in case of a bone height close to 2 mm [17, 18].
A biomechanical parameter that is now spreading in the clinical practice to reveal the implant primary stability indirectly and proportionally is known as the insertion torque (IT) of the implant [19]. A minimum IT value of 20 Ncm and optimal ones around 32 Ncm are routinely used to place implants into healed or fresh extraction sockets prior to immediate loading of implants, being recommended to achieve proper osseointegration. In addition, increased IT values (≥50 Ncm) are able to reduce micromotion without damaging the bone [20, 21]. However, IT values above 80 Ncm have been shown to affect the implant structure regardless of the type of implant connection, encouraging clinical complications [22]. Another clinical measurement used for the prevention, diagnosis, and prediction of implant failures is the resonance frequency analysis (RFA), which is intimately correlated with the bone-to-implant contact (BIC) values, as well as the removal torque (RT), considered the force used for implant removing [23, 24]. In particular, the RFA measurement produces the implant stability quotient (ISQ) value, ranging from 0 to 100 and providing a cutoff value of 47 for good implant stability [20, 23].
Fresh mandibular specimens are widely used for the in vitro biomechanical research, but they possess a variable modulus of elasticity and density depending on the site and orientation of the specimen. Specifically, due to the presence of a cortical bone in the anterior mandibular region, the human mandibular trabecular bone shows a significantly higher modulus of elasticity than in the posterior mandibular region [25]. For this reason, different mathematical and biomechanical models have been developed in substitution of the human bone for in vitro testing the implant-supported prostheses under loading [26, 27]. In this context, polyurethane is an isotropic and homogeneous material, which is considered by the American Society for Testing and Materials (ASTM F-1839-08, “Standard specification for rigid polyurethane foam for use as a standard material for test orthopedic devices for instruments”) a standard prototype for studying force distribution around dental implants at different target anatomical sites [28,29,30,31]. Interestingly, several other authors have recently used this artificial bone to evaluate the primary stability and to perform mechanical tests on dental implants [31, 32]. In fact, synthetic polyurethane foams have a similar cellular structure and biomechanical characteristics consistent with natural bone, being widely used as an alternative material to human cadaver bones and animal bones, which, in addition to the presence of ethical issues, are more difficult to manage [27, 33,34,35].
Low to high-density polyurethane foams are representative of different natural bone densities and, as proposed by Misch [25], they can be classified as follows:
-
D1 bone—40 pounds per cubic foot (PCF): this bone consists almost entirely of a dense cortical. It is found in the anterior mandible
-
D2 bone—30 PCF: this bone consists in porous cortical and coarse trabecular bone. It may have multiple localizations, such as the anterior or posterior mandible but also the anterior maxilla
-
D3 bone—20 PCF: this bone consists of a porous crestal layer of cortical bone and a fine trabecular bone. Tactile analogy can be made to compressed balsa wood. It is commonly found in the anterior and posterior maxilla, but may also be found in the posterior mandible
-
D4 bone—10 PCF: this bone is trabecular without any cortical. It is located in the posterior maxilla
Furthermore, the ease and noninvasive nature of using polyurethane foam blocks make them particularly valuable for predicting and evaluating primary stability and osseointegration of implants compared to other models, such as ex vivo or in vivo [36,37,38].
Based on these grounds, the present in vitro study is aimed at evaluating the IT, RT, and RFA, and therefore, the primary stability of two dental implants with the same shape and diameter but with different lengths through the use of polyurethane foam blocks represents a useful in vitro model able to mimic the density and biomechanical characteristics of natural bone. The null hypothesis, intended to assess statistical differences between the two implants in terms of IT, RT, and RFA values, posits that there are no significant differences when inserting implants into different polyurethane blocks.
Materials and methods
Implants and polyurethane block characteristics
A total number of 120 Cono-In implants (3p Smart Devices, Implafavourite S.r.l, Scalenghe, Italy) with a diameter of 3.8 mm were tested in this study and divided into 2 groups of different lengths: 8 mm (3p S) and 14 mm (3p L). All implants presented a truncated-conical shape in order to satisfy every clinical demand, a trapezoidal double thread of 0.3 mm in depth, which tend to increase the contact with the material, a 1-mm length cervical micro threading to reduce cortical stress and improve cell adhesion, and finally a rounded apex to not insult the tissue. The grade IV titanium im-plants had a 2° Cono-Morse connection of 2.81 mm in diameter and 3.70 mm in length and a micro-rough (Microtek) surface obtained by double acid-etching and plasma finishing, with a mean profile roughness (Ra) of 1.01 ± 0.22 µm, a mean squared profile roughness (Rq) of 1.12 ± 0.39 µm, and a maximum profile roughness height from peak to valley (Rt) of 6.80 ± 0.82 µm. Representative images of both implant designs are reported in Fig. 1.
All tested implants have been inserted in 3 different solid rigid polyurethane foams (Sawbones Europe AB, Malmö, Sweden) with the same size (13 cm × 18 cm × 4 cm) but with different densities. Indeed, the different densities of the blocks used in the present in vitro study were intended to simulate jaw bones of D1, D2, and D3 types, according to Misch’s classification [39], thus imitating a density of 64 kg/m3 (40 PCF density block), 48 kg/m3 (30 PCF density block), and 32.02 kg/m3 (20 PCF density block). For the present investigation, 20 implants per group were placed in each block, for a total of 120 osteotomies. Figure 2 shows the experimental design of this study.
Drilling sequence protocols
Randomization was not applicable in this study model, because of the different preparation protocols and drilling sequences used for implant placement. The osteotomies were prepared following the manufacturer’s recommended protocols. The drilling protocol for 3p S implant insertion involved the use of an initial lanceolate drill at a speed of 1200 rpm, a cylindrical drill of 2 mm in diameter and up to 9 mm in length, a conical drill of 3.8 mm in diameter, and up to 7 mm in length at a speed of 500 rpm for 20 and 30 PCF density blocks; whereas for the 40 PCF density block, it was used the same sequence with an additional cylindrical drill of 3.8 mm in diameter and up to 9 mm in length. The drilling sequence for 3p L implant insertion, instead, required the use of an initial lanceolate drill at a speed of 1200 rpm, a cylindrical drill of 2 mm in diameter, up to 15 mm in length, a conical drill of 3.8 mm in diameter, and up to 7 mm in length at a speed of 500 rpm for the 20 PCF density block. For the 30 and 40 PCF density blocks, it was also used a final cylindrical drill of 3.8 mm in diameter and up to 10 mm and 15 mm in length, respectively. Figure 3 shows the drilling sequences used to perform the osteotomies.
Insertion torque (IT) and removal torque (RT) measurements
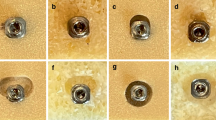
After the final implant insertion using a surgical motor with a 20:1 contra-angle (WS-75 L, W&H Italia S.r.l., Bergamo, Italy) at 600 rpm with a calibrated torque of 40 Ncm, the registration of the IT values was performed in the final 2 mm of insertion with a calibrated torque meter for dynamometric analysis. Then, the maximum RT was assessed by dynamometric analysis of the implant extraction from the block (Fig. 4).
Resonance frequency analysis (RFA) measurements
The RFA was provided registering the ISQ values by a transducer attached to the implant (Smart Peg, W&H Italia S.r.l., Bergamo, Italy) and a frequency response analyzer (Osstell Beacon, W&H Italia S.r.l., Bergamo, Italy) in the mesial and distal directions. The ISQ values ranged from 0 to 100 and provided a classification of the implant stability: values ≤ 60 ISQ indicated low stability, values comprised between 60 and 70 ISQ were indices of medium stability, and values > 70 ISQ indicated high stability [40]. In Fig. 5, an example of the RFA measurements in the mesial and distal directions was reported.
Data analysis
G*Power 3.1.9.7 program (Heinrich-Heine-Universität, Düsseldorf, Germany) was used to perform the power analysis and the a priori sample size planning using the ANOVA: fixed effects, special, main effects, and interactions statistical test (effect size 0.4, α err 0.05; power (1-β) 0.8; numerator df 2; number of groups 6). Thus, the minimum sample size necessary to achieve a statistically significant output was 64 implant sites.
A two-way analysis of variance (ANOVA) with a Tukey’s post hoc test was performed to evaluate the statistical significance of the study variables (IT, RT, and RFA in the mesial and distal directions) when compared all the different bone densities and after assessing the normal distribution of values through Shapiro–Wilk test.
The experimental values were elaborated using the statistical software package GraphPad Prism Software Analysis version 9.0 (San Diego, CA, USA), and the statistical significances were determined for a p < 0.05. Data were expressed as the mean ± standard error of the mean (SEM).
Results
The IT, RT, and RFA mean values were recorded for both the 3p S and 3p L implants after their insertion into the polyurethane blocks of different densities. Table 1 reports the mean and the SEM for each test group and experimental condition.
Regarding the IT values, 3p S implants exhibited significant differences among the tested conditions, resulting significantly higher especially in the 30 and 40 PCF polyurethane densities (p < 0.01 and p < 0.001, respectively) and showing the highest IT value in the 30 PCF density block (90 Ncm), while the lowest value was found in the 20 PCF density block (35 Ncm). On the other hand, the 3p L group showed always significantly lower results than the 3p S one, except for the 20 PCF density block, where it exhibited its highest value (70 Ncm), while in the 40 PCF density block, the absolute lowest value was found (15 Ncm) (Fig. 6). Furthermore, the values expressed by 3p S implants in the 20 PCF density block reported significantly lower values compared to the other blocks (p < 0.0001 and p < 0.01, if compared to 30 and 40 PCF density blocks, respectively), while between 30 and 40 PCF density blocks, no significant differences have been found. Similarly, no significant differences have been reported between IT values of 3p L implants, except when the 20 and 40 PCF density blocks were compared (p < 0.01).
The RT values confirmed the IT results and that is: 3p L implants showed higher values only in the 20 PCF density block (50 Ncm), but not reporting significant differences compared to 3p S implants, while in all the other blocks, 3p S implants revealed always higher results, reporting a significant difference only in the 40 PCF density block (p < 0.01). The lowest RT value has been reported by 3p S implants in the lowest density block (25 Ncm). Comparing all the different densities, other significant differences appeared to be present among the highest RT values expressed by 3p S implants in the 40 PCF density block (90 Ncm) and in the 30 PCF density block (57 Ncm), and the lowest values expressed by the same implant in the 20 PCF density block (25 Ncm) (Fig. 7).
After RFA measurements in the mesial and distal directions, the results showed no significant differences between 3p S and 3p L implants in any artificial bone density, except for the lowest density block, where 3p L implants expressed higher results (67 ISQ compared to 63 ISQ of 3p S implants, with a p < 0.01 in the distal orientation and a p < 0.001 in the mesial orientation). The ISQ values appeared to proportionally increase in respect to the bone density, with significant differences between the 20 PCF density block and all the other blocks for both implants (p < 0.001 for 3p L implants and p < 0.0001 for 3p S implants). However, the highest RFA value has been expressed by 3p L implants in the 40 PCF density block (73 ISQ), whereas the lowest one was shown by 3p S implants in the 20 PCF block (60 ISQ) (Figs. 8 and 9).
Discussion
The achievement of implant primary stability is considered as the absence of implant movement immediately after the implant insertion into the bone, including micromotions [1, 6]. Indeed, several authors have assessed that the BIC is essential for determining implant primary stability [7, 41, 42]. It has been proved that different factors could influence the BIC and implant primary stability, such as the bone quality and the implant length, shape, and diameter [2,3,4,5,6, 41, 43]. Particularly, in some cases, it was demonstrated that implant lengths > 10 mm allow the decrease of bone stress, the increase of primary stability, and a higher implant survival rate than short ones in low-density bones [9,10,11]. However, there are currently differing outcomes that are in opposition to these latter, assessing that the length of dental implants does not influence the survival rate [12,13,14,15,16,17,18]. Indeed, based on the results of this in vitro study, the initial null hypothesis can be rejected, demonstrating that short implants could achieve significantly higher IT and RT values, particularly in high-density artificial bone. Additionally, they exhibited primary stability equal to longer implants, except in low-density bones.
Several authors have chosen the artificial bone in substitution of the human bone to conduct an indirect evaluation of implant primary stability and study the biomechanical behavior of different implants [27,28,29,30,31]. It consists of the use of a solid rigid polyurethane foam, a standard material recognized by the ASTM for studying force distribution around implants and performing mechanical tests on orthopedic and dental devices [30,31,32,33,34,35]. In addition to the employment of different densities of this material, which aimed at representing the natural bone types according to Mish’s classification [25], some clinical parameters could be measured on this in vitro model to indirectly reveal the implant primary stability, such as the IT, RT, and RFA. The IT method suggested a more coherent predictability of osseointegration, and it has been demonstrated to be proportionally correlated to implant primary stability [19], as well as the ISQ quantitative assessment, which is considered, together with the RT methodology, an indirect BIC indicator [20,21,22,23,24]. Basing on this, in the current study, the effect of two implant lengths (8 and 14 mm) on primary stability has been evaluated in D1, D2, and D3 simulated bone types, using 20, 30, and 40 PCF density polyurethane artificial bone blocks. From the results, in low-quality bone (20 PCF in density), a positive correlation between the length of implants and both the IT and RT values could be observed, reporting the highest values of 70 and 50 Ncm, respectively, for 3p L implants (Figs. 6 and 7). The reason beyond this phenomenon could be related to the fact that in this quality of bone, such as D3 bone type, the implant length plays an essential role in decreasing bone stress and enhancing implant stability [6]. As a matter of fact, a study conducted by Trisi et al. [44] demonstrated that implant IT can be increased in order to reduce micromotions between implants and bone, in situations where low-quality bone and high micromotions are present. Consequently, since a correlation between the implant length and a poor quality of bone has been proved, in the present study, it was hypothesized the possible use of implants with higher lengths aims to achieve a higher primary stability. However, when the artificial bone density increased from 20 to 30 and 40 PCF, the 3p S implant showed significantly higher IT than 3p L implants, reaching values of 90 and 80 Ncm in 30 and 40 PCF density blocks, respectively, and an RT of 57 and 90 Ncm in the same foams. Similarly, in a clinical trial conducted by Degidi et al. [45], it was revealed the same IT behavior in different bone densities, demonstrating the close reliance between IT and bone density. Moreover, in the present study, the IT values were higher than the RT ones for all bone densities and implant lengths, as can be also found in literature [46, 47]. Indeed, according to Ahn et al. [48], the difference in IT and RT is due to the restricted viscoelastic properties of the artificial bone surrounding the insertion site, which results in less resistance during removal.
In the RFA measurement technique, the implant’s micro-mobility has been measured, whereas the ISQ is an implant measurement unit based on the frequency movement measured by RFA. Thus, micro-mobility and implant stability can be estimated with this latter value, which normally ranges from 0 to 100 [20]. To this end, ISQ values ≥ 70, ISQ values included between 60 and 69, and ISQ values < 60 are known to represent high, medium, and low stability, respectively [49]. In this work, no statistical differences in the ISQ were noticeable for 3p S and 3p L implants, especially in 30 and 40 PCF density bone blocks (71 and 70 ISQ for 3p S implants in the 30 PCF block and 71 and 72 ISQ for 3p L implants in the same conditions). However, in the lowest density polyurethane bone block, 3p L implants reached significantly higher values in respect to 3p S implants (67 in respect to 63 ISQ for the distal orientation and 67 compared to 63 ISQ for the mesial orientation). In this regard, all RFA values allowed a medium or high implant primary stability in all experimental conditions, since values are included between 60 and 73 ISQ, thus being considered as appropriate values in respect to ranges for clinical applications [50]. In contrast, Barikani et al. [51] reported significantly different ISQ values between the D1 and D3 bone conditions, but similarly to our results, they observed that the implant length did not influence primary stability in high-quality bone. However, some studies showed that in low-quality bone, the ISQ value tended to increase with implant length [51,52,53], demonstrating consistent results with those obtained in this work that reported significantly higher ISQ values for 3p L implants when inserted in the lowest density polyurethane block (67 ISQ in respect to 63 ISQ related to 3p S implants).
Therefore, based on the aforementioned results, the use of shorter implants in the mandibular region, represented by the densities of artificial bone blocks of 30 and 40 PCF, might be conceivable. On the other hand, when the maxillary region is the target, longer implants might result in better primary stability, since in these in vitro conditions, they reported higher IT, RT, and RFA values in low-density bone (20 PCF density block), despite no differences were shown in RFA for both implants in other conditions. Consistently with the previous results, a study conducted by Barikani et al. [41] showed that in parallel implants, the implant stability increased in D3 artificial bone block by increasing the implant length.
Due to the nature of this artificial bone model, all results are obviously not comparable to clinical conditions. Indeed, regarding the limitations of the present study, it is important to recognize that, although polyurethane foam blocks represent a good in vitro model and they are already used in implant research thanks to their consistent and reproducible testing properties and as testing material on alternate cadaver human and animal bones, it is unable to fully replicate the intricate features of real bone. Several factors should be taken into consideration for a more complete discussion of data, such as the absence of individual human variability, natural bone response, and the complex microenvironment of healthy or pathological bone. Additionally, variables related to surgical technique should be considered to better interpret these results. Consequently, the data obtained in this study may not fully reflect the actual in vivo performance of these implants.
However, confirmation of these data through animal and clinical studies is essential for future use and implementation. To strengthen the use of polyurethane blocks as a human bone model for studying implant behavior, biomechanical evaluations using finite element analysis (FEA) studies could also be considered.
Despite the limitations associated with an in vitro study conducted on non-human bone tissue, the authors speculate that these preliminary results may provide useful insights into the biomechanical behavior of these implants, with the goal of enabling clinicians to improve their surgical planning.
Conclusions
In conclusion, our results demonstrate that the implant length mainly influences the IT and RT values in polyurethane blocks mimicking the porous cortical and coarse trabecular bone and the dense cortical bone (30 and 40 PCF in density), resulting in higher values when short implants were used, while the ISQ values appeared to be unaffected. However, in the lowest density block mimicking the fine trabecular bone (20 PCF), the longer dental implant had significantly higher ISQ values.
Overall, although further studies are needed, our data could provide useful information regarding the biomechanical behavior of these implants, with the aim of enabling clinicians to improve their surgical planning on the use of short implants in the mandibular area and long implants in the maxilla.
Data availability
Data is contained within the article and available on request from the corresponding author.
References
Albrektsson T, Albrektsson B (1987) Osseointegration of bone implants: a review of an alternative mode of fixation. Acta Orthop Scand 5:567–577. https://doi.org/10.3109/17453678709146401
Sim CPC, Lang NP (2010) Factors influencing resonance frequency analysis assessed by Osstell Mentor during implant tissue integration: I. Instrument positioning, bone structure, implant length. Clin Oral Implants Res 6:598–604. https://doi.org/10.1111/j.1600-0501.2009.01878.x
Han J, Lulic M, Lang NP (2010) Factors influencing resonance frequency analysis assessed by Osstell Mentor during implant tissue integration: II. Implant surface modifications and implant diameter. Clin Oral Implants Res 6:605–611. https://doi.org/10.1111/j.1600-0501.2009.01909.x
Comuzzi L, Tumedei M, Di Pietro N, Romasco T, Heydari Sheikh Hossein H, Montesani L, Inchingolo F, Piattelli A, Covani U (2023) A comparison of conical and cylindrical implants inserted in an in vitro post-extraction model using low-density polyurethane foam blocks. Materials 14:5064. https://doi.org/10.3390/ma16145064
Fanali S, Tumedei M, Pignatelli P, Inchingolo F, Pennacchietti P, Pace G, Piattelli A (2021) Implant primary stability with an osteocondensation drilling protocol in different density polyurethane blocks. Comput Methods Biomech Biomed Engin 24:14–20. https://doi.org/10.1080/10255842.2020.1806251
Bataineh AB, Al-Dakes AM (2017) The influence of length of implant on primary stability: an in vitro study using resonance frequency analysis. J Clin Exp Dent 1:e1–e6. https://doi.org/10.4317/jced.53302
Orenstein IH, Tarnow DP, Morris HF, Ochi S (2000) Three-year post-placement survival of implants mobile at placement. Ann Periodontol 1:32–41. https://doi.org/10.1902/annals.2000.5.1.32
Del Giudice R, Piattelli A, Grande NM, Cataneo E, Crispino A, Petrini M (2019) Implant insertion torque value in immediate loading: a retrospective study. Med Oral Patol Oral Cir Bucal 3:e398–e403. https://doi.org/10.4317/medoral.22845
Kong L, Sun Y, Hu K, Li D, Hou R, Yang J, Liu B (2008) Bivariate evaluation of cylinder implant diameter and length: a three-dimensional finite element analysis. J Prosthodont 4:286–293. https://doi.org/10.1111/j.1532-849X.2007.00286.x
Abdel-Halim M, Issa D, Chrcanovic BR (2021) The impact of dental implant length on failure rates: a systematic review and meta-analysis. Materials 14:3972. https://doi.org/10.3390/ma14143972
De Santis D, Cucchi A, Longhi C, Vincenzo B (2011) Short threaded implants with an oxidized surface to restore posterior teeth: 1- to 3-year results of a prospective study. Int J Oral Maxillofac Implants 2:393–403
Kotsovilis S, Fourmousis I, Karoussis IK, Bamia C (2009) A systematic review and meta-analysis on the effect of implant length on the survival of rough-surface dental implants. J Periodontol 11:1700–18. https://doi.org/10.1902/jop.2009.090107
Juodzbalys G, Sapragoniene M, Wennerberg A, Baltrukonis T (2007) Titanium dental implant surface micromorphology optimization. J Oral Implantol. 4:177–85. https://doi.org/10.1563/1548-1336(2007)33[177:TDISMO]2.0.CO;2
Malmstrom H, Gupta B, Ghanem A, Cacciato R, Ren Y, Romanos GE (2016) Success rate of short dental implants supporting single crowns and fixed bridges. Clin Oral Implants Res 9:1093–8. https://doi.org/10.1111/clr.12693
Mangano FG, Shibli JA, Sammons RL, Iaculli F, Piattelli A, Mangano C (2014) Short (8-mm) locking-taper implants supporting single crowns in posterior region: a prospective clinical study with 1-to 10-years of follow-up. Clinical oral implants research 25:933–940. https://doi.org/10.1111/clr.12181
Degidi M, Piattelli A, Iezzi G, Carinci F (2007) Immediately loaded short implants: analysis of a case series of 133 implants. Quintessence international 38:193–201
Thoma DS, Zeltner M, Hüsler J, Hämmerle CH, Jung RE (2015) EAO Supplement Working Group 4 - EAO CC 2015 Short implants versus sinus lifting with longer implants to restore the posterior maxilla: a systematic review. Clinical oral implants research 26:154–169. https://doi.org/10.1111/clr.12615
Comuzzi L, Tumedei M, Petrini M, Romasco T, Lorusso F, De Angelis F, Piattelli A, Tatullo M, Di Pietro N (2023) Clinical and radiological evaluation of a self-condensing bone implant in one-stage sinus augmentation: a 3-year follow-up retrospective study. Int J Environ Res Public Health 20:2583. https://doi.org/10.3390/ijerph20032583
do Vale Souza JP, de Moraes Melo Neto CL, Piacenza LT, Freitas da Silva EV, de Melo Moreno AL, Penitente PA, Brunetto JL, Dos Santos DM, Goiato MC (2021) Relation between insertion torque and implant stability quotient: a clinical study. European journal of dentistry 15:618–623. https://doi.org/10.1055/s-0041-1725575
Ottoni JM, Oliveira ZF, Mansini R, Cabral AM (2005) Correlation between placement torque and survival of single-tooth implants. Int J Oral Maxillofacial Implants 20:769–776
Greenstein G, Cavallaro J (2017) Implant insertion torque: its role in achieving primary stability of restorable dental implants. Compend Contin Educ Dent 2:88–95
Gehrke SA, Pereira GMA, Gehrke AF, Junior NDB, Dedavid BA (2021) Effects of insertion torque on the structure of dental implants with different connections: experimental pilot study in vitro. PLoS One 5:e0251904. https://doi.org/10.1371/journal.pone.0251904
Scarano A, Degidi M, Iezzi G, Petrone G, Piattelli A (2006) Correlation between implant stability quotient and bone-implant contact: a retrospective histological and histomorphometrical study of seven titanium implants retrieved from humans. Clin Implant Dent Relat Res 4:218–22. https://doi.org/10.1111/j.1708-8208.2006.00022.x
Simeone SG, Rios M, Simonpietri J (2016) “Reverse torque of 30 Ncm applied to dental implants as test for osseointegration”—a human observational study. Int J Implant Dent 1:26. https://doi.org/10.1186/s40729-016-0060-4
Misch CE, Qu Z, Bidez MW (1999) Mechanical properties of trabecular bone in the human mandible: implications for dental implant treatment planning and surgical placement. J Oral Maxillofac Surg 6:700–6. https://doi.org/10.1016/s0278-2391(99)90437-8
Callea C, Ceddia M, Piattelli A, Specchiulli A, Trentadue B (2023) Finite element analysis (FEA) for a different type of cono-in dental implant. Appl Sci 9:5313. https://doi.org/10.3390/app13095313
Romanos GE, Delgado-Ruiz RA, Sacks D, Calvo-Guirado JL (2018) Influence of the implant diameter and bone quality on the primary stability of porous tantalum trabecular metal dental implants: an in vitro biomechanical study. Clin Oral Implant Res 6:649–655. https://doi.org/10.1111/clr.12792
Comuzzi L, Tumedei M, Covani U, Romasco T, Petrini M, Montesani L, Piattelli A, Di Pietro N (2023) Primary stability assessment of conical implants in under-prepared sites: an in vitro study in low-density polyurethane foams. Appl Sci 10:6041. https://doi.org/10.3390/app13106041
Comuzzi L, Tumedei M, Romasco T, Petrini M, Afrashtehfar KI, Inchingolo F, Piattelli A, Di Pietro N (2023) Insertion torque, removal torque, and resonance frequency analysis values of ultrashort, short, and standard dental implants: an in vitro study on polyurethane foam sheets. J Funct Biomater 1:10. https://doi.org/10.3390/jfb14010010
Di Stefano DA, Arosio P, Gastaldi G, Gherlone E (2018) The insertion torque-depth curve integral as a measure of implant primary stability: an in vitro study on polyurethane foam blocks. J Prosthet Dent 5:706–714. https://doi.org/10.1016/j.prosdent.2017.04.012
Tsolaki IN, Tonsekar PP, Najafi B, Drew HJ, Sullivan AJ, Petrov SD (2016) Comparison of osteotome and conventional drilling techniques for primary implant stability: an in vitro study. J Oral Implant 4:321–5. https://doi.org/10.1563/aaid-joi-D-15-00176
Arosio P, Arosio F, Di Stefano DA (2020) Implant diameter, length, and the insertion torque/depth integral: a study using polyurethane foam blocks. Dent. J 8:56. https://doi.org/10.3390/dj8020056
Calvert KL, Trumble KP, Webster TJ, Kirkpatrick LA (2010) Characterization of commercial rigid polyurethane foams used as bone analogs for implant testing. J Mater Sci Mater Med 21:1453–1461. https://doi.org/10.1007/s10856-010-4024-6
Nagaraja S, Palepu V (2016) Comparisons of anterior plate screw pullout strength between polyurethane foams and thoracolumbar cadaveric vertebrae. J Biomech Eng 138:104505. https://doi.org/10.1115/1.4034427
Gehrke SA, Guirado JLC, Bettach R, Fabbro MD, Martínez CPA, Shibli JA (2018) Evaluation of the insertion torque, implant stability quotient and drilled hole quality for different drill design: an in vitro investigation. Clin Oral Implants Res 29:656–662. https://doi.org/10.1111/clr.12808
Romanos G, Damouras M, Veis AA, Hess P, Schwarz F, Brandt S (2020) Comparison of histomorphometry and microradiography of different implant designs to assess primary implant stability. Clin Implant Dent Relat Res 22:373–379. https://doi.org/10.1111/cid.12915
Mirzaie T, Rouhi G, Mehdi Dehghan M, Farzad-Mohajeri S, Barikani H (2021) Dental implants’ stability dependence on rotational speed and feed-rate of drilling: in-vivo and ex-vivo investigations. J Biomech 127:110696. https://doi.org/10.1016/j.jbiomech.2021.110696
Gehrke SA, Treichel TLE, Pérez-Díaz L, Calvo-Guirado JL, AramburúJúnior J, Mazón P, de Aza PN (2019) Impact of different titanium implant thread designs on bone healing: a biomechanical and histometric study with an animal model. J Clin Med 8:777. https://doi.org/10.3390/jcm8060777
Barikani H, Rashtak S, Akbari S, Fard MK, Rokn A (2014) The effect of shape, length and diameter of implants on primary stability based on resonance frequency analysis. Dent Res J (Isfahan) 1:87–91
Javed F, Romanos GE (2010) The role of primary stability for successful immediate loading of dental implants. A literature review. J Dent 8:612–20. https://doi.org/10.1016/j.jdent.2010.05.013
Ivanova V, Chenchev I, Zlatev S, Mijiritsky E (2021) Correlation between primary, secondary stability, bone density, percentage of vital bone formation and implant size. Int J Environ Res Public Health 13:6994. https://doi.org/10.3390/ijerph18136994
Trisi P, Perfetti G, Baldoni E, Berardi D, Colagiovanni M, Scogna G (2009) Implant micromotion is related to peak insertion torque and bone density. Clin Oral Implants Res 5:467–71. https://doi.org/10.1111/j.1600-0501.2008.01679.x
Degidi M, Daprile G, Piattelli A (2012) Primary stability determination by means of insertion torque and RFA in a sample of 4,135 implants. Clin Implant Dent Relat Res 4:501–7. https://doi.org/10.1111/j.1708-8208.2010.00302.x
Yamaguchi Y, Shiota M, Munakata M, Kasugai S, Ozeki M (2015) Effect of implant design on primary stability using torque-time curves in artificial bone. Int J Implant Dent 1:21. https://doi.org/10.1186/s40729-015-0024-0
Yamaguchi Y, Shiota M, Fujii M, Shimogishi M, Munakata M (2020) Effects of implant thread design on primary stability—a comparison between single-and double-threaded implants in an artificial bone model. Int J Implant Dent 1:42. https://doi.org/10.1186/s40729-020-00239-1
Ahn SJ, Leesungbok R, Lee SW, Heo YK, Kang KL (2012) Differences in implant stability associated with various methods of preparation of the implant bed: an in vitro study. J Prosthet Dent 6:366–72. https://doi.org/10.1016/S0022-3913(12)60092-4
Makary C, Rebaudi A, Sammartino G, Naaman N (2012) Implant primary stability determined by resonance frequency analysis: correlation with insertion torque, histologic bone volume, and torsional stability at 6 weeks. Implant Dent 6:474–80. https://doi.org/10.1097/ID.0b013e31826918f1
Ballo A (2012) Implant dentistry research guide: basic, translational and clinical research. Nova Publishers. ISBN: 978-1-61942-447-0.
Barikani H, Rashtak S, Akbari S, Badri S, Daneshparvar N, Rokn A (2013) The effect of implant length and diameter on the primary stability in different bone types. J Dent 5:449–55
Ustaoğlu G, Paksoy T, GÜMÜŞ K (2020) Evaluating the effect of design and length of implants on primary stability using resonance frequency analysis: an in vitro study. Selcuk Dent J 7:265–272. https://doi.org/10.15311/selcukdentj.538052
Winter W, Möhrle S, Holst S, Karl M (2010) Parameters of implant stability measurements based on resonance frequency and damping capacity: a comparative finite element analysis. Int J Oral Maxillofac Implants 3:532–9
Mish CE (1998) Bone dentistry. A key determinant for clinical success. Contemp Implant Dent 8:109–118
Baltayan S, Pi-Anfruns J, Aghaloo T, Moy PK (2016) The predictive value of resonance frequency analysis measurements in the surgical placement and loading of endosseous implants. J Oral Maxillofac Surg 6:1145–52. https://doi.org/10.1016/j.joms.2016.01.048
Acknowledgements
3p Smart Devices, Implafavourite S.r.l, Scalenghe, Italy, provided the implants at no cost, and this is gratefully acknowledged. Moreover, the authors would like to acknowledge Cruciata Francesco, Rabita Danilo, and Costantino Emanuele for their technical support.
Author information
Authors and Affiliations
Contributions
Conceptualization, N.D.P., A.P., and A.C.; methodology, T.R., M.T., and H.H.S.H.; software, T.R. and H.H.S.H.; validation, F.I., A.P., and N.D.P.; formal analysis and investigation, T.R., N.D.P., and M.T.; resources, A.C.; data curation, T.R. and P.P.; writing—original draft preparation, P.P. and H.H.S.H.; writing—review and editing, N.D.P. and T.R.; visualization, A.P. and F.I.; supervision, A.C.; project administration, N.D.P. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
This is an in vitro study. No ethical approval is required.
Consent
Not applicable.
Competing interests
The authors declare no competing interests.
Conflict of interest
The authors declare no competing interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Romasco, T., Pignatelli, P., Tumedei, M. et al. The influence of truncated-conical implant length on primary stability in maxillary and mandibular regions: an in vitro study using polyurethane blocks. Clin Oral Invest 28, 28 (2024). https://doi.org/10.1007/s00784-023-05444-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00784-023-05444-x