Abstract
Objectives
The aim of the study was to identify predictors of the masticatory muscle activity during chewing (MMA) of the masseter and temporalis anterior (TA) muscles in patients with unilateral myogenous temporomandibular disorder (mTMD).
Materials and methods
This observational and cross-sectional study included 109 patients diagnosed with unilateral mTMD. Surface electromyography was used to separately evaluate the MMA of the masseter and TA on the affected and unaffected sides. Also, pain intensity (with a visual analog scale), pressure pain threshold (with an algometer), active pain-free maximum mouth opening and temporomandibular joint lateral movements (with a ruler), cervical range of motions (with a goniometer), and TMD severity (with a Fonseca Anamnestic Index) were assessed. Various statistical methods were used to predict the MMA of the masseter and TA, including standard, forward, and best subsets multiple regression models.
Results
While there were significant correlations between the MMA of the masseter and TA and pain intensity, pressure pain threshold values, and TMD severity, they were not found with other variables. These parameters were also predictive factors for MMA of both muscles (p < 0.05).
Conclusions
According to the present study, pain intensity, muscle and joint tenderness, and the severity of the disorder are predictive factors for MMA of the masseter and TA muscles in patients with mTMD. It is recommended that these parameters be considered when establishing clinical evaluation and treatment programs focusing on MMA in patients with mTMD.
Clinical relevance
The pain intensity, masticatory muscles and TMJ tenderness, and disorder severity are predictors for MMA of the masseter and TA in patients with mTMD. Pain intensity has the most significant importance.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Temporomandibular disorders (TMDs) are defined as a group of neuromuscular and musculoskeletal disorders that may affect the masticatory muscles, temporomandibular joint (TMJ), and related structures [1]. Signs and symptoms of TMD include masticatory muscles and/or TMJ pain (at rest and/or during chewing), limited jaw movement, joint sounds (crepitus and clicking), the tenderness of the TMJ and/or masticatory muscles, chewing difficulty, and headache [2]. Myogenous TMD (mTMD), characterized by myofascial pain syndrome in the masticatory muscles, is the most common type of TMD [3]. TMD signs and symptoms can negatively affect patients’ quality of life and daily activities such as chewing, speaking, eating, and social participation resulting in physical disability and psychosocial dysfunction. It has been reported that TMD is most common in adults aged 18 to 45, with prevalence rates of up to 25% [4]. In a systematic review and meta-analysis study conducted by Valesan et al. [5], the prevalence of TMD was found to be 31% for adults and the elderly. Physical trauma, occlusal factors, emotional stress, parafunction, and deep pain input were defined as etiological factors associated with TMD [1].
Pain, the primary symptom of patients with TMD, can affect the TMJ and/or the masticatory muscles. Pain may be accompanied by tenderness in the TMJ and/or masticatory muscles and limitation in jaw movement. TMD pain can cause adaptations in masticatory muscle activities to prevent possible traumas to the masticatory system. As a result of these protective adaptations, changes in electromyographic activity during muscle contraction can occur [5, 6].
Lund et al. [7] stated that chronic musculoskeletal pain might cause a decrease in the electrical activities of agonist and synergist muscles and, as a result, a reduction in muscle force production and range of motion of the affected body part. Supporting this, Wang et al. [8] and Gavish et al. [9] reported that pain in TMD inhibits motor unit firing in masticatory muscles, resulting in decreased muscle activation and strength. These authors added that depending on the decrease in muscle strength, the bite force decreased, and the chewing difficulty appeared.
Surface electromyography (sEMG) has been described as a reliable method for assessing masticatory muscle function and activity through the detection of electrical potentials of the muscles in patients with TMD [10, 11]. sEMG, a non-invasive and safe method, has been used to evaluate muscle activity during functions such as chewing and maximum voluntary contraction in patients with TMD [6, 12]. However, various educational and technical barriers have been reported to the use sEMG in the clinical setting. Many clinicians have limited knowledge of sEMG and its neuromuscular basis. Analysis of performance indicators, such as sEMG amplitude normalization, requires special training and attention [13]. Despite providing valuable data, user dependency, the relatively high cost of sEMG devices, and the long time required for sEMG analysis of muscles and interpretation of the results limit the clinical use of this method [13, 14].
To the best of the authors’ knowledge, no research has been found in the literature that has examined the predictive factors affecting the masticatory muscle activity during chewing (MMA) in patients with TMD. Knowing the independent predictors that affect the MMA is significant for the clinician to assess and monitor masticatory muscle function and dysfunction in patients with TMD. Therefore, the present study aimed to identify predictors of MMA of the masseter and TA muscles in patients with unilateral mTMD.
Materials and methods
Study design and ethical aspects
The present study, which was designed as observational and cross-sectional research, was approved by the Karamanoğlu Mehmetbey University Faculty of Medicine Clinical Research Ethics Committee (Decision no: 06–2022/12). Written informed consent was obtained from all patients who were given detailed information about the study. The study was conducted in accordance with the principles of the Declaration of Helsinki.
Participants
The study population consisted of 109 patients diagnosed with unilateral mTMD out of 164 who applied to Karamanoğlu Mehmetbey University Faculty of Dentistry with TMD complaints. The clinical and radiological examinations of the patients were performed by a specialist dentist (experience in TMD), and the patients were diagnosed with mTMD according to the first axis of the Diagnostic Criteria for TMD [15]. The inclusion criteria for the TMD patients were age 18–50 years, diagnosis of unilateral mTMD, pain and/or fatigue in the masticatory muscles during functional activities for at least 6 months on the affected side, not receiving treatment for TMD in the past 3 months, not using splints, dental braces, and/or analgesic drugs, and body mass index (BMI) between 19 and 25 kg/m2. The exclusion criteria were the following: history of surgery or trauma involving the TMJ, face or neck, tooth loss, history of subluxation or dislocation of the TMJ, BMI greater than 25 kg/m2, systemic or psychiatric disease (such as diabetes, rheumatoid arthritis or depression), current treatment involving muscle relaxants/analgesics or orthodontic treatment, and history of pregnancy. The demographic and clinical characteristics of the patients were recorded who volunteered to participate in the study and met the inclusion criteria. Other assessments made are listed below.
Assessment of pain ıntensity
Pain intensity during jaw functions such as biting and chewing was evaluated by a visual analog scale (VAS) for affected and unaffected sides separately. The VAS consisted of a 10-cm line labeled “no pain” at one end and “the most severe pain” at the other. The value marked by the patient on the line and indicating pain intensity was recorded in cm (VAScm) [16].
Assessment of the pressure pain threshold
Pressure pain threshold (PPT) was measured with a digital pressure algometer with a 1 cm2 probe (JTech Commander Algometer, JTech Medical, Salt Lake City, UT, USA) at the lateral pole of the TMJ, the masseter muscle belly, and the temporalis anterior (TA) muscle on the affected and unaffected sides separately. During the measurements, the patients were asked to say “yes” when they experienced pain. The amount of pressure causing pain was recorded as Newton(N)/cm2. Three measurements were made from each of the three points with 30-s rest intervals, and the average of these measurements was recorded separately for use in the analysis [17].
Assessment of active pain-free maximum mouth opening and temporomandibular joint lateral movements
Active pain-free maximum mouth opening (MMO) and TMJ lateral movements were measured with a ruler in millimeters (mm). The distance between the upper and lower central incisors was measured in millimeters for MMO measurement. While measuring the lateral movement of the TMJ, the lateral distance between the midpoints of the upper and lower central incisors was measured in mm, separately for the right and left sides. The average of the values of the right and left sides was used in the analysis [16].
Assessment of cervical range of motions
Active neck flexion, extension, and left and right lateral flexion, which are cervical spine movements, were measured with a cervical range of motion goniometer (CROM) (CROM Basic, Performance Attainment Associates, St. Paul, MN, USA) in degrees. While neck flexion and extension values were recorded separately, left and right lateral flexion values were averaged for lateral flexion value. The CROM device is valid and reliable for measuring cervical spine movements [18].
Assessment of temporomandibular disorder severity
To assess the severity of TMD based on the patient’s signs and symptoms, the Turkish version of the Fonseca Anamnestic Index (FAI) was used [19]. The FAI is a 10‐item tool that evaluates pain frequency, jaw function limitation, parafunctional behaviors, and psychological distress related to TMD. Items in the index are answered with “yes” (10 points), “sometimes” (5 points), or “no” (0 points). The total Index score is obtained by adding the scores of the answers given to the items and varies between 0 and 100 points. A higher index score indicates that TMD is more severe [19].
Surface electromyography measurement procedures
In order to obtain MMA of the masseter and TA muscles, electromyographic activities of the masseter and TA muscles were evaluated separately on the affected and unaffected sides with a wireless sEMG device (Delsys Trigno Wireless System, Delsys Inc., Natick, MA, USA). Measurements were performed in an isolated, quiet room with a room temperature of 25 °C by a clinician trained and experienced in sEMG. The patients were seated upright on the chair with their heads unsupported and were asked to maintain their natural upright position. In order to reduce the skin impedance, the skin areas to be measured were carefully cleaned with an alcohol solution before electrode placement [20]. Wireless surface electrodes were placed with double-sided tape on the muscle bellies parallel to the muscle fibers unilaterally (on the affected and unaffected sides), as described in the study by Ferrario et al. [20] After electrode placement, sEMG measurements were performed in two protocols, separately on the affected and unaffected sides. sEMG measurement protocols were first performed on the unaffected side. After an adequate resting time to avoid fatigue from affecting the measurements, sEMG measurements for the affected side were then carried out.
Protocol I: mastication: unilateral gum chewing
Patients were asked to chew a standard pre-softened sugarless gum on the posterior teeth on the affected or unaffected side for 15 s at their habitual frequency. EMG activity was recorded during unilateral chewing of gum. The protocol was performed three times with 3-min rest intervals, and the task with the best EMG recording achieved was used for further analysis [21].
Protocol II: maximum voluntary clenching on a cotton roll
A 10-mm thick cotton roll was positioned on the mandibular second premolar/first molars of the affected or unaffected side. The patient was invited to clench his/her teeth with a maximum force as hard as possible and maintain the same contraction level for 5 s [20]. This equipment’s specific software program (EMGworks® Acquisition) was used for the acquisition and storage of digitized signals.
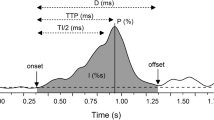
Surface electromyography data analysis
Raw EMG signals of both muscles were analyzed separately with this equipment’s special software program (EMGworks® Analysis). First, the raw signals were filtered to remove any possible noise (Filter class: Butterworth, Order: 4, Response: Band Pass, Corner Frequency 1: 20 Hz, Corner Frequency 2: 500 Hz). Then, the Root Mean Square filter was applied to the filtered maximum voluntary clenching (MVC) signals (Window Length: 0.025 ms, Window Overlap: 0.0125 ms). It has been reported that a relative value of MMA can be obtained by dividing the EMG value calculated during chewing by the activity produced during maximum voluntary contraction [7]. In the current study, this method was used through the device’s proprietary software (EMGworks® Analysis) to obtain the relative value of muscle activity during chewing. Normalization was achieved by dividing the filtered version of the highest EMG value calculated during chewing by the MVC value passed through the Root Mean Square filter. As a result, the percentage of maximum voluntary contraction (%MVC) values was obtained for both muscles separately on affected and unaffected sides. In simplest terms, %MVC is the ratio of muscle activity produced during chewing to muscle activity produced during MVC. In the present study, a high %MVC value was interpreted as a high MMA value [7, 21].
Statistical methods
While mean and standard deviation values were given for the quantitative variables that were found to be normally distributed, qualitative variables were given as numbers and percentages. The independent sample t-test was used to compare the quantitative measurement data from the affected and unaffected sides. In the data analysis process, various statistical methods were used to predict the MMA values of the masseter and TA muscles. Standard (classical), forward, and best subsets multiple regression methods have been considered in this study. All models have been applied to the data set, and different regression results have been obtained corresponding to each target variable. The experimental settings can be summarized as follows:
-
The statistical assumptions, including outliers, normality, linearity, independency, homoscedasticity, and multicollinearity were checked via various analytical and visual approaches and given in the results section in detail.
-
The descriptive statistics, including frequencies, central tendency, and dispersion measures, were obtained.
-
Classic multiple regression model and its stepwise alternatives, including forward and best subsets regression were run to predict the target variables and determine the most predictive factors. The MMA values of the masseter and TA muscles were considered dependent variables.
-
In order to measure the performance of the regression models, the root mean square error (RMSE), adjusted Akaike information criterion (AAIC), and r-squared (R2) values were calculated and reported.
-
To assess the variable importance of each variable on the regression models, the relative contribution to the increase in r-squared value was calculated and reported as visually.
Statistical analysis was carried out via Statistical Package for Social Sciences 24.0 (SPSS. Inc., Chicago, IL, USA), Minitab (State College, PA: Minitab, Inc.), and R-software (R Core Team, 2022). A p-value < 0.05 was considered significant.
Results
The assumptions required for reliable regression results were examined carefully. The outliers were examined using z-scores with [− 3,3] range and box plots. As a result of the analysis, sixteen observations found to be outliers were excluded from the study. The assumption of normality was met as assessed by using both the Kolmogrov-Smirnov test and the Q-Q plot. The linearity was evaluated using the studentized residuals against the predicted values corresponding to each dependent variable and found no violation. The independence of residuals was checked via Durbin-Watson statistics and found independent. The homoscedasticity assumption was examined by observing the plot of studentized residuals versus predicted values for each dependent variable and found no violation. The variance inflation factor values were calculated to determine whether there is a multicollinearity problem between variables. The results indicated that there are no variance inflation factor values larger than 10. As a result of overall controls, there were no critical problems in terms of violating the statistical assumptions.
Of the 164 patients who applied to the clinic, 125 who met the inclusion criteria were included in the study. Data from 109 patients who met the necessary statistical assumptions were analyzed. The flow diagram of the study was shown in Fig. 1.
The descriptive statistics, including count and percentages for qualitative variables and mean, standard deviation, and minimum and maximum values for quantitative variables were given in Table 1. There was a significant difference in the pain intensity, PPT values of the TMJ, masseter, and TA muscles, and MMA values of the masseter and TA muscles between the affected side and the unaffected side (p < 0.05). Accordingly, while the severity of pain was higher on the affected side, PPT values of the TMJ, masseter, and TA muscles and MMA values of the masseter and TA muscles were lower (Table 1).
The results based on three different multiple regression models, including standard (classical), forward, and best subsets regression were obtained and presented separately in Tables 2, 3, 4, 5, 6, and 7. Tables 2, 3, and 4 correspond to the masseter %MVC values, and the rest (Tables 5, 6, and 7) belong to the TA %MVC values. Each table includes model coefficients, standard errors, significance values, confidence intervals, relative importance values, and model performance metrics. According to all regression models for both target variables, the overall models were found to be significant (p < 0.05). In each of these models corresponding to the masseter %MVC, while pain intensity, masseter PPT, and TA PPT were found as statistically significant (p < 0.05) (Tables 2, 3, and 4), TMJ PPT, MMO, and FAI scores were included as additional significant variables only for standard and best subsets models (Tables 2 and 4) (Figs. 2, 3, and 4).
The most important features based on the standard regression model for both temporalis anterior and masseter muscle %MVCs. %MVC: Percentage of maximum voluntary contraction; PPT: Pressure pain threshold; TA: Temporalis anterior; TMJ: Temporomandibular joint; FAI: Fonseca anamnestic index; MMO: Active pain-free maximum mouth opening
The most important features based on the best subsets regression model for both temporalis anterior and masseter muscle %MVCs. %MVC: Percentage of maximum voluntary contraction; PPT: Pressure pain threshold; TA: Temporalis anterior; TMJ: Temporomandibular joint; FAI: Fonseca anamnestic index; MMO: Active pain-free maximum mouth opening
On the other side, pain intensity, TA PPT, and masseter PPT stand out as significant variables shared by all three regression models obtained for the TA %MVC variable (Tables 5, 6, and 7). TMJ PPT and FAI scores were additionally included for standard and best subset models (Tables 5 and 7) (Figs. 2, 3, and 4). The coefficients for each regression model represent the change in the dependent variable for a one-unit change in the corresponding independent variable (Tables 2, 3, 4, 5, 6, and 7). As an example of the interpretation of the variables, an increase in pain intensity of one unit is associated with the decrease in masseter %MVC of − 1.97 units when other independent variables are kept constant in the standard model. However, neck flexion does not significantly affect the masseter %MVC value (p = 0.15) (Table 2). The masseter PPT and TA PPT were positively and significantly associated with the masseter %MVC and the TA %MVC (p < 0.05). The increase (or decrease) in these variables was associated with the increase (or decrease) in target variables. Similar interpretations can be made for all possible regression models corresponding to two target variables (Tables 2, 3, 4, 5, 6, and 7).
When comparing the overall performance of each model, three different criteria were taken into account including RMSE, AAIC, and R2. The model with larger R2 but smaller AAIC and RMSE values can be considered the best model. When comparing all three regression models developed based on performance criteria, the best subsets model seems the best for both the masseter %MVC and the TA %MVC estimation due to having larger R2 and smaller AAIC and RMSE.
Discussion
The results of the present study indicated significant correlations (considering the best subsets models) between the %MVC values of the masseter and TA muscles and pain intensity, pressure pain threshold values, and FAI scores in patients with mTMD. In addition, while there was a significant relationship between MMO and masseter %MVC, there was no relationship between TA %MVC. On the other hand, there was no correlation between %MVC values of both muscles, age, TMJ lateral movement, and all cervical range of motion values. Another finding of the study was the difference between the affected side and the unaffected side in terms of pain intensity, PPT values of the TMJ, masseter, and TA muscles, and MMA values of the masseter and TA muscles. These results show that MMA is adversely affected by pain intensity, muscle and joint tenderness, and severity of the disorder in patients with mTMD. Considering these findings, it can be said that pain intensity, muscle and joint tenderness, and severity of the disorder are the predictive factors of MMA of the masticatory muscles in patients with mTMD.
TMD reduces the quality of life of individuals by negatively affecting basic daily living activities such as speaking and chewing [4]. In patients with TMD, biting and chewing difficulties are the most common complaints after pain. Factors contributing to chewing and biting difficulties include pain, limited jaw movements, masticatory muscles, TMJ tenderness, and altered muscle activation patterns. The mTMD can cause essential changes in the electrical activity of the masticatory muscles due to the disorder or the compensatory mechanisms related to the symptoms, as the primary problems in affected patients are of muscular origin [2]. In studies investigating MMA in patients with TMD, it has been found that patients have more asymmetrical and lower muscle potential than healthy individuals [11, 20, 22]. In addition, it has been reported that there is more asymmetry in muscle activities in patients with more severe diseases [21], and there is a negative correlation between the severity of the disease and muscle activity [22]. However, in a comprehensive literature review, no published study investigating the predictive factors of MMA in patients with mTMD was found.
Lund et al. [7] explained the effects of chronic musculoskeletal pain on muscle activity with the Pain Adaptation Model. According to this neurophysiological theory, based on phasic modulation of excitatory and inhibitory interneurons provided by high-threshold sensory afferents, pain originating from the muscle itself or non-muscular sources is effective in decreasing the motor activity of the synergist as well as agonist muscles during function (e.g., masticatory muscle activity during chewing) [7]. There is increasing interest in the relationship between pain and motor function (muscle activity) in studies on TMD. Consistent with the Pain Adaptation Model, these studies reported slower, smaller amplitude movements and lower agonist and synergist muscle EMG activity during pain. In other words, pain in TMD can reduce muscle activation and strength by inhibiting motor unit firing in masticatory muscles [8, 9, 11, 23,24,25]. Similarly, Shimada et al. [26] reported that pain has an inhibitory effect on MMA and reduces bite force. In another study, Goldreich et al. [27] suggested that the pain input may reduce muscle activity by causing protective reflex inhibition in the jaw-closing muscles. In the current study, significant negative correlations were found between pain intensity and EMG activities of both masseter and TA muscles, consistent with the literature. Pain intensity was a significant predictor of MMA. Considering the studies in the literature and the results of the present study, pain intensity is an important predictor of MMA in mTMD patients.
The PPT is very precious for providing a quantitative and objective measurement of tenderness in masticatory muscles and TMJ [28]. Ohrbach and Gale [29], who determined that there were significant negative relationships between PPT values measured from the painful area and pain severity in patients with mTMD, reported that PPT measurements in patients with mTMD provided valid and reliable important data about tenderness. Similarly, in the study of Stuginski-Barbosa et al. [28] in mTMD patients, significant negative correlations were revealed between PPT values measured from TMJ, masseter, and TA muscles and pain intensity. The results of these studies support the negative relationships between PPT and pain intensity in patients with mTMD [28, 29]. In the present study, significant positive correlations were found between PPT values measured from masticatory muscles and TMJ and %MVC values of both muscles. While PPT measured from the masseter muscle had a greater effect on the masseter muscle MVC% value, PPT measured from the TA muscle had a greater effect on the TA muscle %MVC value. These findings imply that tenderness in mTMD patients may be a predictor of MMA, particularly when PPT is measured from the muscle itself. Indirect relationships can be established between pain intensity, tenderness, and muscle activation. It has been reported that with the increase in pain intensity, tenderness may increase due to the sensitization of peripheral nociceptors, and PPT value may decrease [28, 29]. Considering that pain can reduce muscle activity [8, 9, 11, 23,24,25], a decrease in PPT due to pain and, at the same time, a decrease in muscle activity in the presence of pain may be expected. Another interesting result obtained in the current study was that PPTs of TMJ and the other masticatory muscle (e.g., TA muscle) were also influential on the %MVC value of the mentioned masticatory muscle (e.g., masseter muscle). This result implies that there may be close relationships between the masticatory muscles themselves and between the masticatory muscles and the TMJ, which is supported by previous research and the Pain Adaptation Model. In these studies, it has been reported that pain and tenderness arising from the muscle itself or non-muscular sources may be effective in reducing motor activity in synergist muscles as well as painful muscles [7, 23, 24].
In patients with TMD, the functional status of the jaw may worsen due to signs and symptoms such as decreased chewing muscle activity and strength due to pain and restricted jaw movements [24]. TMD severity and its effects on the functional status of the jaw could be evaluated using assessment tools such as FAI. In this study, FAI was used to assess the severity of TMD, and a higher score from the index was interpreted as a higher severity of TMD [19]. Significant negative correlations were found between FAI score and %MVC values of both masseter and TA muscles. These findings can be interpreted as the severity of the disorder may negatively affect MMA. Ardizone et al. [25] evaluated the severity of TMD with the Helkimo Clinical Dysfunction Index and the activities of the masseter and TA muscles during MVC with sEMG in patients with TMD. The authors revealed that as the severity of pain and symptoms increased, MMA decreased. Mapelli et al.21 reported that the masseter muscle activity of the TMD patients with the severe disorder was significantly lower than in the asymptomatic individuals during mastication. In another study conducted by De Felício et al. [22], the masseter and TA muscle activities during MVC were assessed with sEMG, and the severity of TMD signs and symptoms was assessed with the ProTMDmulti-part II Questionnaire in patients with TMD and found that there were significant correlations between sEMG indices and the severity of TMD. Given that the current study’s findings agree with those of previous research, it can be concluded that the severity of TMD is a significant predictive factor of MMA.
Pain and limitation in jaw movements are two significant interrelated symptoms of TMD. The pain input in the orofacial region can stimulate the brainstem centrally, causing dysfunction and protective spasm (increased muscle tension) of the masticatory muscles. As a result, jaw movements can be limited [1, 7, 24]. Fernandez-Carnero et al. [30] reported that in patients with mTMD, dry needling increased MMO by reducing muscle tension of taut bands and pain in the masseter muscle. The results of the study of Fernandez-Carnero et al. [30] support the associations between pain intensity, muscle tension/spasm, and jaw movement limitations in patients with mTMD. The present study found a significant positive relationship between MMO and masseter %MVC but not between TA %MVC. This result shows that there may be indirect relationships between MMO and MMA. MMO may be restricted due to pain-induced spasms in the masticatory muscles. Restricted MMO may imply the presence of spasm and pain in the jaw muscles [1, 24, 30]. Considering the negative associations between pain that triggers muscle spasm and muscle activity [8, 9, 11, 23,24,25,26], it can be said that there may be indirect relationships between MMO and MMA through pain. In this respect, it can be said that MMO is a predictor of MMA, albeit at a low level. However, this suggestion should be investigated in further studies.
The current study found no correlation between %MVC values of both muscles and age, TMJ lateral movement, and all cervical range of motion values. Visser et al. [31] revealed that the EMG activity of the TA during MVC decreased with increasing age in patients with mTMD, but there was no significant age-related change in masseter EMG. Researchers reported that the decrease in the EMG activity of TA with increasing age might be due to muscle atrophy or a decrease in the number of motor units activated during contraction [31]. In the current study, it was thought that the relatively close age range of the study participants was influential in the absence of a relationship between age and MMA. With this, investigating the relationship between MMA and age, TMJ lateral movement, and cervical range of motion parameters in further studies may provide useful information.
In the literature, no studies were found examining the predictors of MMA of the masseter and TA muscles in patients with mTMD. In the present study, pain intensity, muscle and joint tenderness, and severity of the disorder were found to be predictors of MMA in patients with mTMD. In this respect, it is thought that the current study will make important contributions to the literature.
The present study had some limitations. First, only patients diagnosed with unilateral myogenous TMD were included in the study, considering that MMA may be more affected in mTMD. Comparisons between different TMD diagnosis groups could not be made because other diagnostic groups, such as disc displacement were not included. Considering that psychological factors (e.g., depression, anxiety, stress) may affect sEMG recordings [32], another limitation is that psychological factors were not evaluated in the current study. Third, gender comparisons were not made in statistical analyzes, and results were not compared by gender. It is recommended to investigate these limitations in future studies and to confirm the current results.
Conclusions
The present study found that the pain intensity, muscle and joint tenderness, and severity of the disorder may be predictive factors of MMA in patients with mTMD. Given the limited use of sEMG in the clinical setting due to various educational and technical barriers, the present study’s findings may provide important information about the functional status of masticatory muscles in patients with TMD. The authors recommend that these parameters be considered when establishing clinical evaluation and treatment programs focusing on MMA in patients with mTMD.
References
Chung J, Lobbezoo F, van Selms MK et al (2021) Physical, psychological and socio-demographic predictors related to patients’ self-belief of their temporomandibular disorders’ aetiology. J Oral Rehabil 48(2):109–123
Pires PF, Rodrigues-Bigaton D (2018) Evaluation of integral electromyographic values and median power frequency values in women with myogenous temporomandibular disorder and asymptomatic controls. J Bodyw Mov Ther 22(3):720–726
Rammelsberg P, LeResche L, Dworkin S et al (2003) Longitudinal outcome of temporomandibular disorders: a 5-year epidemiologic study of muscle disorders defined by research diagnostic criteria for temporomandibular disorders. J Orofac Pain 17(1):1–12
Marpaung C, van Selms MK, Lobbezoo F (2018) Prevalence and risk indicators of pain-related temporomandibular disorders among Indonesian children and adolescents. Community Dent Oral Epidemiol 46(4):400–406
Valesan LF, Da-Cas CD, Réus JC et al (2021) Prevalence of temporomandibular joint disorders: a systematic review and meta-analysis. Clin Oral Investig 25(2):441–453
Szyszka-Sommerfeld L, Machoy M, Lipski M et al (2019) The diagnostic value of electromyography in identifying patients with pain-related temporomandibular disorders. Front Neurol 10:180
Lund JP, Donga R, Widmer CG et al (1991) The pain-adaptation model: a discussion of the relationship between chronic musculoskeletal pain and motor activity. Can J Physiol Pharmacol 69(5):683–694
Wang K, Arima T, Arendt-Nielsen L et al (2000) EMG-force relationships are influenced by experimental jaw-muscle pain. J Oral Rehabil 27(5):394–402
Gavish A, Winocur E, Astandzelov-Nachmias T et al (2006) Effect of controlled masticatory exercise on pain and muscle performance in myofascial pain patients: a pilot study. Cranio 24(3):184–190
Ferrario VF, Sforza C, D’addona A et al (1991) Reproducibility of electromyographic measures: a statistical analysis. J Oral Rehabil 18(6):513–521
Tartaglia GM, Lodetti G, Paiva G et al (2011) Surface electromyography assessment of patients with long lasting temporomandibular joint disorder pain. J Electromyogr Kinesiol 21:659–664
Suvinen TI, Malmberg J, Forster C et al (2009) Postural and dynamic masseter and anterior temporalis muscle EMG repeatability in serial assessments. J Oral Rehabil 36(11):814–820
Campanini I, Disselhorst-Klug C, Rymer WZ et al (2020) Surface EMG in clinical assessment and neurorehabilitation: barriers limiting its use. Front Neurol 11:934
Prakash A, Sharma S, Sharma N et al (2019) A compact-sized surface EMG sensor for myoelectric hand prosthesis. Biomed Eng Lett 9(4):467–479
Schiffman E, Ohrbach R, Truelove E et al (2014) Diagnostic criteria for temporomandibular disorders (DC/TMD) for clinical and research applications: recommendations of the International RDC/TMD Consortium Network and Orofacial Pain Special Interest Group. J Orofac Pain 28(1):6–27
La Touche R, Fernández-de-Las-Peñas C, Fernández-Carnero J et al (2009) The effects of manual therapy and exercise directed at the cervical spine on pain and pressure pain sensitivity in patients with myofascial temporomandibular disorders. J Orofac Pain 36(9):644–652
Chaves TC, Nagamine HM, de Sousa LM et al (2007) Intra-and interrater agreement of pressure pain threshold for masticatory structures in children reporting orofacial pain related to temporomandibular disorders and symptom-free children. J Orofac Pain 21(2):133–142
Micarelli A, Viziano A, Granito I et al (2022) Temporomandibular disorders and cervicogenic dizziness: relations between cervical range of motion and clinical parameters. Cranio 40(4):348–357
Kaynak BA, Taş S, Salkın Y (2020) The accuracy and reliability of the Turkish version of the Fonseca anamnestic index in temporomandibular disorders. Cranio 41(1):78–83
Ferrario VF, Tartaglia GM, Luraghi FE (2007) The use of surface electromyography as a tool in differentiating temporomandibular disorders from neck disorders. Man Ther 12(4):372–379
Mapelli A, Machado BCZ, Giglio LD et al (2016) Reorganization of muscle activity in patients with chronic temporomandibular disorders. Arch Oral Biol 72:164–171
De Felicio CM, Ferreira CLP, Medeiros APM et al (2012) Electromyographic indices, orofacial myofunctional status and temporomandibular disorders severity: a correlation study. J Electromyogr Kinesiol 22(2):266–272
Svensson P, Houe L, Arendt-Nielsen L (1997) Bilateral experimental muscle pain changes electromyographic activity of human jaw-closing muscles during mastication. Exp Brain Res 116(1):182–185
Peck CC, Murray GM, Gerzina TM et al (2008) How does pain affect jaw muscle activity? The Integrated Pain Adaptation Model. Aust Dent J 53(3):201–207
Ardizone I, Celemin A, Aneiros F et al (2010) Electromyographic study of activity of the masseter and anterior temporalis muscles in patients with temporomandibular joint (TMJ) dysfunction: comparison with the clinical dysfunction index. Med Oral Patol Oral Cir Bucal 15(1):e14-19
Shimada A, Hara S, Svensson P (2013) Effect of experimental jaw muscle pain on EMG activity and bite force distribution at different level of clenching. J Orofac Pain 40(11):826–833
Goldreich H, Gazit E, Lieberman MA et al (1994) The effect of pain from orthodontic arch wire adjustment on masseter muscle electromyographic activity. Am J Orthod Dentofacial Orthop 106(4):365–370
Stuginski-Barbosa J, Silva RS, Cunha CO et al (2015) Pressure pain threshold and pain perception in temporomandibular disorder patients: is there any correlation? Rev Dor 16(1):22–26
Ohrbach R, Gale EN (1989) Pressure pain thresholds, clinical assessment, and differential diagnosis: reliability and validity in patients with myogenic pain. Pain 39(2):157–169
Fernandez-Carnero J, La Touche R, Ortega-Santiago R et al (2010) Short-term effects of dry needling of active myofascial trigger points in the masseter muscle in patients with temporomandibular disorders. J Orofac Pain 24(1):106–112
Visser A, McCarroll RS, Oosting J et al (1994) Masticatory electromyographic activity in healthy young adults and myogenous craniomandibular disorder patients. J Oral Rehabil 21(1):67–76
Klasser GD, Okeson JP (2006) The clinical usefulness of surface electromyography in the diagnosis and treatment of temporomandibular disorders. J Am Dent Assoc 137(6):763–771
Funding
No funding was obtained for this study.
Author information
Authors and Affiliations
Contributions
N.T.Y. and H.K. contributed to data acquisition, conception, design, and data interpretation, and drafted and critically revised the manuscript. H.Y. contributed to the conception, design, and data interpretation, performed the statistical analysis, and, drafted and critically revised the manuscript. All authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
This study was approved by the Karamanoğlu Mehmetbey University Faculty of Medicine Clinical Research Ethics Committee (Decision no: 06–2022/12). Written informed consent was obtained from all patients who were given detailed information about the study. The study was conducted in accordance with the principles of the Declaration of Helsinki.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yıldız, N.T., Kocaman, H. & Yıldırım, H. Predictors of the masticatory muscle activity during chewing in patients with myogenous temporomandibular disorder. Clin Oral Invest 27, 6547–6558 (2023). https://doi.org/10.1007/s00784-023-05260-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-023-05260-3