Abstract
Objectives
The aim of this study was to compare the upper airway space changes after miniscrew-anchored maxillary protraction with hybrid (HH) and conventional hyrax (CH) expanders.
Material and methods
The sample comprised Class III malocclusion growing patients that were randomized into two groups of miniscrew-anchored maxillary protraction. The group HH was treated with a hybrid hyrax appliance in the maxilla and two miniscrews distally to the canines in the mandible. Class III elastics were used from the maxillary first molar to the mandibular miniscrews until anterior crossbite correction. The group CH was treated with a similar protocol except for the conventional hyrax expander in the maxilla. Cone-beam computed tomography was obtained before (T1) and after 12 months of therapy (T2). The shape and size of upper airway were assessed. Intergroup comparisons were performed using Mann-Whitney U test (p < 0.05).
Results
The group HH was composed of 20 patients (8 female, 12 male) with a mean age of 10.76 years. The group CH was composed of 15 patients (6 female, 9 male) with a mean age of 11.52 years. Anteroposterior and transverse increases of the upper airway were found for both groups. The oropharynx and the most constricted area increased similarly in both groups.
Conclusions
No differences in upper airway changes were observed using protraction anchored on hybrid or conventional hyrax expanders.
Clinical relevance
Maxillary protraction anchored on hybrid or conventional hyrax expanders may benefit patients with breathing disorders due to the increase of the upper airway volume and most constricted area. Registration: ClinicalTrials.gov (NCT03712007).
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Skeletal discrepancies and maxillary deficiency can influence the airway space volume and morphology [1]. The airway space is divided into nasopharynx, oropharynx, and hypopharynx, all related to several structures of the face [2]. In Class III growing patients, orthopedic maxillary protraction causes not only skeletal changes but also modifications in the adjacent soft tissue as the airway [2,3,4,5].
Several studies investigated the effects of maxillary protraction on pharyngeal airway dimension and have shown conflicting results [3, 6, 7]. The effects of maxillary protraction using facemask therapy on the upper airway were evaluated using cephalometric radiographs in a sample of Class III malocclusion patients with 10.3 years of age [8]. The results indicated that maxillary protraction increased the naso and oropharynx after treatment [8]. Previous studies using conventional 2D evaluation found that facemask therapy associated with rapid maxillary expansion (RME) caused pharyngeal airway increase [4, 5, 8, 9]. On the other hand, previous studies reported that the nasopharyngeal and oropharyngeal airway dimensions remained unchanged after maxillary protraction [7, 9]. A recent meta-analysis found that facemask therapy associated with RME increases the upper airway space changes in children or young adolescents [4]. However, the authors reported that 2D cephalometric radiographs might not completely reflect the exact changes in the pharyngeal airway space [4].
Most of the previous studies evaluated the changes of the upper airway using lateral headfilms. Two-D cephalometric radiographs may limit the accuracy of the upper airway measurements [10,11,12]. Currently, cone-beam computed tomography (CBCT) has been widely used to assess the upper airway shape and volume [3, 13,14,15]. CBCT offers the advantages of volumetric rather than linear measurements, distortion-free measurements, and measurements that are independent of head positioning [3, 14]. Chen et al. [3] used CBCT in order to evaluate changes of the upper airway after maxillary protraction with facemasks. An increase was found in the volume of the naso and oropharynx of growing patients with Class III malocclusion when compared to untreated Class III patients [3]. Nguyen et al. [14], using CBCT, showed an increase in airway volume and oropharyngeal dimensions in subjects treated with bone-anchored maxillary protraction (BAMP). BAMP is an innovative treatment modality that uses miniplates to anchor Class III elastics and correct the maxillary deficiency [16, 17]. A previous study demonstrated an effective maxillary protraction by using a hybrid hyrax anchoring a facemask in growing Class III malocclusion individuals [18]. The use of a hybrid hyrax and mentoplate combination (modified miniplate) and comparison with the hybrid hyrax-facemask combination were also described in the literature showing effective maxillary advancement in growing subjects [19]. Miniscrew-anchored maxillary protraction (MAMP) is a BAMP-derived therapy that replaces the mandibular miniplates for miniscrew [20]. The MAMP therapy seems to be an effective treatment alternative for Class III malocclusion correction in growing patients. However, no previous studies evaluated the effect of MAMP therapy on the upper airway volume and morphology.
Specific objectives and hypotheses
The aim of this study was to compare the upper airway changes after miniscrew-anchored maxillary protraction with hybrid (HH) and hyrax expanders (CH). The null hypothesis is that miniscrew-anchored maxillary protraction with hybrid and hyrax expanders has similar upper airway changes after treatment.
Methods
Trial design and any changes after trial commencement
This study was a single center randomized controlled trial with two parallel arms and a 1:1 allocation ratio. Changes in participants number were performed after trial commencement and were described below (Fig. 1). The study followed the Consolidated Standards of Reporting Trials guidelines (CONSORT) [21]. This clinical trial was registered under the number NCT03712007 at Clinicaltrials.gov.
The study was approved by the Ethics in Research Committee of BauruDental School, University of São Paulo, Brazil (protocol number 67610717.7.0000.5417) where patients were treated by the same orthodontist (FM). The airway evaluation was performed at the Department of Orthodontics of School of Dental Medicine, Case Western Reserve University, USA. All patients and parents signed the written informed consent before treatment.
Participants, eligibility criteria, and settings
The individuals were recruited at the Orthodontic Clinic of BauruDental School, University of São Paulo, Brazil, from July 2017 to March 2018. The sample consisted of 40 individuals with Class III malocclusion from 9 to 13 years of age. The eligibility criteria were (1) both sexes, (2) late mixed or early permanent dentition, (3) skeletal Class III malocclusion with maxillary deficiency (Wits appraisal of −1 mm or less), (4) anterior crossbite or incisor edge-to-edge relationship. Exclusion criteria were individuals with history of previous orthodontic treatment, non-erupted mandibular permanent canines, and individuals with special needs or syndromes.
Interventions
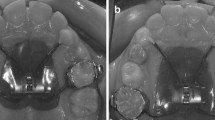
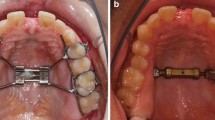
The two treatment groups differed in the maxillary anchorage strategy. The group HH was treated with miniscrew-anchored maxillary protraction therapy anchored in a hybrid expander [20]. A hybrid expander was used in the maxilla (Fig. 2A), and two mandibular miniscrews were positioned distal to the permanent canines, bilaterally (Fig. 2A). Patients were instructed to wear Class III elastics full time, from the maxillary first molar hooks to the mandibular miniscrews (Fig. 2A). The group CH was treated with a similar protocol using a conventional hyrax expander instead of hybrid expanders (Fig. 2B). Parents were oriented to activate the expander screw 1/4 turn twice a day for 14 days, achieving 5.6 mm of expansion. Traction started with a load of 150 g/side in the first month and 250 g/side in the following period. Class III elastics were changed twice a day in the morning and at night [17]. The elastics were used until reaching an overjet correction or until a maximum of 12 months of treatment. After appliance removal, a chin cup was used during the night as active retention.
Cone-beam computed tomography (CBCT) was obtained before (T1) and after treatment (T2), using the i-CAT 3-dimensional system (Imaging Sciences International, Hatfield, PA) with a protocol of 13-cm FOV, 120 kV, 23.87 mA and a voxel size of 0.25 mm. All CBCT data were exported in DICOM format (Digital Imaging and Communications in Medicine) to Dolphin 3D Imaging software (Chatsworth, CA, USA). The head orientation was standardized in the sagittal view, positioning the Frankfort plane parallel to the horizontal plane (considering the right side); in the frontal view, leveling the orbital plane with the horizontal plane; and in the axial view, positioning the midsagittal plane passing through the anterior and posterior nasal spines.
Outcomes
The primary outcomes of this RCT were dentoskeletal changes produced by maxillary protraction that was evaluated in a previous study. Group HH and CH displayed similar Co-A changes of 1.81 and 0.81 (p = 0.082), respectively. The SNA angle changes were 1.40 and 0.81 in group HH and CH (p = 0.283), respectively. The intermolar width demonstrated a 3.5-mm and 3.47-mm increase in group HH and CH after expansion, respectively. The three-dimensional changes were registered as secondary outcomes in the Clinicaltrials.org (NCT03712007).
The outcomes of this study were the shape and volume analysis performed by innovative open source software. Semiautomatic airway segmentations were performed in the ITK-SNAP software (http://www.itksnap.org). The palatal plane was used as the upper limit of the oropharynx (OP, Fig. 3). A parallel line passing in the antero-inferior border of the third cervical vertebrae (C3) was used as the lower limit of the OP (Fig. 3). The upper airway volume was generated after segmentation. To ensure a spherical topology, the constructed airway models were processed to avoid spicules and holes in the model [22]. The epiglotic vallecula was excluded [23]. The shape analysis was performed in the 3D Slicer (www.slicer.org) via the SlicerSALT project (salt.slicer.org, Vicory et al. 2018) [24]. Parametric surface models were created for each segmented airway (Figs. 4 and 5). The mean latitude axis and minimum axial area were found for each model. The minimum axial area (minAx) was considered the most constricted axial area in the oropharynx. Surface superimpositions and color maps were generated to visually compare the changes between T1 and T2 (Figs. 6 and 7).
The volume changes of the oropharynx (OP) and minimum axial area (minAx) were also calculated using Dolphin 3D Imaging software (Chatsworth, CA, USA). The OP volume was defined using the same anatomic boundaries of the shape analysis. The threshold sensitivity was individualized for each scan.
Sample size calculation
The sample size calculation considered the maxillary anteroposterior changes described in a previous study reporting the primary outcomes of this randomized clinical trial. Sample size was calculated in order to provide 80% of test power, at a significance level of 0.05. With a minimum intergroup difference of 2 mm and a standard deviation of 1.4 mm in maxillary length changes (CoA) [16], a minimum sample of nine patients was required for each group. Considering possible losses, twenty patients were selected for each group. A post hoc power analysis was conducted using the G*power software (version 3.1.9, Heinrich-Heine-University, Düsseldorf, Germany)[25].
Interim analyses and stopping guidelines
If any harm or undesirable side-effect occurred, the treatment would be interrupted.
Randomization
Randomization, envelopes concealment, and allocation were performed by different operators. Randomization was performed electronically in the Randomization.com website (http://www.randomization.com). Opaque, sealed, and numbered envelopes containing the group name were made according to the sequence generated by the randomization [26].
The allocation process started after recruitment, and the signed informed consent was obtained. The patients’ name and date of allocation were identified in the external surface of the envelopes. After that, the envelope was opened to verify to which group the patient was allocated. During treatment, undesirable dental effects in the maxillary arch were observed in the group CH. Undesirable dental effects included the mesial migration of posterior teeth, decreases in the maxillary arch perimeter, and maxillary canine crowding. For ethical reasons, the group CH treatment was interrupted after 11 months of treatment and before installation in the last 5 individuals.
Blinding
To avoid bias, all CBCT scans were unidentified before assessment, achieving a simple blinding. Double blinding was not accomplished considering that both operator and patient were aware of the type of treatment performed.
Statistical analysis
Repeated measurements on 30% randomly selected patients were performed after 1 month by the same examiner. The intraclass correlation coefficient (ICC) and Bland-Altman limits of agreement were used to assess the reliability of repeated measures and the correlation between software.
Normal distribution was verified by the Shapiro-Wilk test. Interphase comparisons were performed using the Wilcoxon test. Intergroup comparisons were performed using the Mann-Whitney U test on an intention-to-treat (ITT) basis, using multiple imputation to deal with the missing data of the dropouts. Spearman correlation was performed to analyze the association between skeletal and oropharyngeal effects. A significance level of 5% was regarded for all tests. Statistical analyses were performed with SPSS Statistical Software Package (Version 21.0; SPSS, Chicago, IL).
Results
Participant flow
Forty subjects were selected and agreed to participate in this trial. The final sample in the group HH comprised 20 patients (8 female, 12 male) with a mean age of 10.76 years. After trial commencement, one patient quit and another was excluded due to palatal miniscrew instability. Before CBCT upper airway analysis, five patients had to be excluded due to unsuitability of CBCT scan (teeth were not in occlusion).
Fifteen patients were treated in the group CH. The final sample in the group CH comprised 15 patients (6 female, 9 male) with a mean age of 11.52 years. One patient interrupted treatment, and two were excluded due to unsuitability of CBCT scan (teeth were not in occlusion). Figure 1 shows the complete participant flow chart.
Mean active treatment time was 11.38(SD 3.98) and 11.00 (SD 3.78) months in group HH and CH, respectively (Table 1).
Baseline data
The demographic characteristics of each group are presented in Table 1. Both groups presented similar initial age, sex distribution, and treatment time. Both groups also presented similar initial SNA, SNB, and Wits appraisal (Table 1).
Baseline characteristics are presented in Table 2. Similar upper airway size was observed in both groups.
Number analyzed for each outcome, estimation, and precision, subgroup analyses
In the intraexaminer analysis, the ICC varied from 0.808 to 0.997 showing good to excellent agreement of the measurements. The ICC showed high correlations for the minimum axial area and volume measurements between the 2 software (Table 3).
The post hoc power analysis showed that the sample of this study achieved a power of 7% for the measurements (effect size = 0.14). Both groups demonstrated a similar increase in the SNA and Wits appraisal (Tables 4 and 5). The oropharynx volume and minimum axial area demonstrated a posttreatment increase in the group HH (Table 4). The oropharynx volume showed similar increases in both groups (MD: −138.61; 95% CI: −3078.01, 2800.80). Also, the minimum axial area showed similar increases in both groups (MD: 10.58; 95% CI: −39.14, 60.30). No significant correlation was found between the skeletal and oropharyngeal effects (Table 6). Figure 7 shows individual treatment changes in the upper airway illustrated using color maps. Both transverse and anteroposterior changes were observed in both groups (Fig. 7).
Harms
The frequency of instability of the mandibular miniscrews in the groups HH and CH was 15.7% and 17.8%, respectively. When mandibular miniscrews were unstable before anterior crossbite correction, they were replaced after 2 weeks in the same region with 30° inclination. The instability of palatal miniscrews was 2.6%.
Treatments were performed until anterior crossbite correction or after 12 months of therapy. Patient compliance was very important for successful outcomes. Non-compliant patients presented poor results; however, they were also considered in the final analysis.
Discussion
Main findings in the context of the existing evidence and interpretation
In the past decade, there was a marked increase in volumetric airway analyses and obstructive sleep apnea (OSA) assessment [27]. Previous studies showed that maxillary protraction increased the upper airway volume and most constricted area [3, 4, 9, 14, 28]. The airway volumetric increase after maxillary advancement can benefit the OSA management in growing subjects [29]. This study compared three dimensionally the upper airway space between two different protocols of miniscrew-anchored maxillary protraction in growing Class III malocclusion patients.
Adequate reproducibility was found for all volumetric measurements. These results are in accordance with previous studies demonstrating that CBCT is a reliable tool for measuring the upper airway volume [30, 31]. Threshold sensitivity influences the OP volume [32]. A fixed threshold interval selection produced different segmentation and volume measurements when comparing different software [32]. In this study, the threshold sensitivity was individualized for each scan showing adequate reproducibility for the OP measurements (ICC varying from 0.985 to 0.986). CBCT accuracy and reliability for upper airway analyses showed conflicting results in previous studies [15, 30, 32, 33]. CBCT allows a static rather than dynamic examination of the airway [15]. During the exam, some factors as the respiratory phase, CBCT definition, mandible, and head position need to be controlled [31, 34]. Variability in the dimensions and shape of the airway can occur when the CBCT is acquired with no standardization. On the other hand, CBCT is considered an easy access and low-cost tool to assess the airway volume [31]. CBCT has the possibility to define the boundaries and segment the soft tissue and airway spaces accurately [30, 31].
In this study, two different methods were used to assess the upper airway. The first analysis included the ITK-SNAP software to perform a semi-automatic segmentation and volume assessment followed by the SPHARM-PDM module in the SlicerSalt software that performed an upper airway model shape analysis. Although this first analysis is time consuming, the software choices are open access. The second method of analyzing the upper airways was with Dolphin3D software that present a highly intuitive interface even though consists in a high-cost commercial software. A good correlation was found when comparing the two software (Table 3). A previous study reported good correlation between three different commercial software for upper airway assessments with semi-automatic segmentations (Dolphin3D, InVivoDental and OnDemand3D) [30]. However, the accuracy was considered poor when comparing automatic and manual segmentation software [30]. The ITK-SNAP + SPHARM-PDM and Dolphin3D upper airway analysis were also previously compared [23]. Good reproducibility was reported for both intra and inter examiner correlations [23]. No differences were reported between the three-dimensional volumetric assessments between these software [23].
Miniscrew-anchored maxillary protraction produced similar increases in the upper airway volume after treatment with hybrid and conventional hyrax expanders (Table 5). Anteroposterior increases were observed in the oropharynx after treatment (Fig. 7). One of the possible explanations was the orthopedic maxillary advancement produced by MAMP therapy. The correlation between maxillary protraction and the increase in the upper airway dimension was previously reported [2]. Additionally, significant increases in the pharyngeal airway dimensions were reported after facemask therapy [4, 8, 35]. On the other hand, Baccetti et al. [9] found no changes in the sagittal airway dimension after facemask therapy.
The oropharynx also showed an increase in the transverse dimension after treatment (Fig. 7). The increase in the transverse dimension might be correlated with the maxillary expansion performed before maxillary protraction. Increases in airway dimensions after maxillary expansion were previously reported [4, 36, 37]. Additionally, craniofacial growth might have contributed to sagittal and transverse increase of the upper airways [13, 37,38,39].
The minimum axial area corresponds to the most constricted axial area in the oropharynx, and it is one of the most important changes to be assessed in upper airway studies [29, 40]. Determining the minimum axial area can help to locate the exact location of the airway obstruction, which can benefit the treatment plan of OSA patients [40, 41]. In our study, both groups showed similar increases in the minimum axial area after treatment (Table 5). Maxillary advancement may be the main cause for the change in the airway’s most constricted area. No differences were reported for the minimum axial area after BAMP therapy [14]. Group HH demonstrated a significant increase in upper airway after treatment. Class III patients with small upper airway and signs of oral respiration or sleep apnea might be beneficiated with hybrid hyrax maxillary protraction.
Limitations
Our study main limitation is the absence of an untreated Class III malocclusion control group for growth comparisons. However, maintaining a Class III population without treatment would be unethical. The number of patient exclusions due to CBCT quality decreasing the sample size was also a limitation of this study. Post hoc power analysis demonstrated a test power lower than the ideal; therefore, the outcomes of this study should be interpreted carefully. However, the remained sample size was enough to demonstrate interphase volume and shape changes. Further studies with greater samples should be analyzed. Also, to deal with the missing data of the dropouts, an intention-to-treat analysis was performed.
Conclusions
The null hypothesis was accepted. Both groups showed similar upper airway increases after maxillary protraction. Functional analysis comparison should be further performed to confirm these findings.
References
Nargozian C (2004) The airway in patients with craniofacial abnormalities. Paediatr Anaesth 14(1):53–59. https://doi.org/10.1046/j.1460-9592.2003.01200.x
Lee J-W, Park K-H, Kim S-H, Park Y-G, Kim S-J (2011) Correlation between skeletal changes by maxillary protraction and upper airway dimensions. Angle Orthod 81(3):426–432. https://doi.org/10.2319/082610-499.1
Chen X, Liu D, Liu J, Wu Z, Xie Y, Li L, Liu H, Guo T, Chen C, Zhang S (2015) Three-dimensional evaluation of the upper airway morphological changes in growing patients with skeletal Class III malocclusion treated by protraction headgear and rapid palatal expansion: a comparative research. PLoS One 10(8):e0135273. https://doi.org/10.1371/journal.pone.0135273
Lee WC, Tu YK, Huang CS, Chen R, Fu MW, Fu E (2018) Pharyngeal airway changes following maxillary expansion or protraction: a meta-analysis. Orthod Craniofac Res 21(1):4–11. https://doi.org/10.1111/ocr.12208
Ming Y, Hu Y, Li Y, Yu J, He H, Zheng L (2018) Effects of maxillary protraction appliances on airway dimensions in growing class III maxillary retrognathic patients: a systematic review and meta-analysis. Int J Pediatr Otorhinolaryngol 105:138–145. https://doi.org/10.1016/j.ijporl.2017.12.013
Iwasaki T, Saitoh I, Takemoto Y, Inada E, Kakuno E, Kanomi R, Hayasaki H, Yamasaki Y (2013) Tongue posture improvement and pharyngeal airway enlargement as secondary effects of rapid maxillary expansion: a cone-beam computed tomography study. Am J Orthod Dentofac Orthop 143(2):235–245. https://doi.org/10.1016/j.ajodo.2012.09.014
Mucedero M, Baccetti T, Franchi L, Cozza P (2009) Effects of maxillary protraction with or without expansion on the sagittal pharyngeal dimensions in Class III subjects. Am J Orthod Dentofac Orthop 135(6):777–781. https://doi.org/10.1016/j.ajodo.2008.11.021
Akin M, Ucar FI, Chousein C, Sari Z (2015) Effects of chincup or facemask therapies on the orofacial airway and hyoid position in Class III subjects. J Orofac Orthop 76(6):520–530. https://doi.org/10.1007/s00056-015-0315-3
Baccetti T, Franchi L, Mucedero M, Cozza P (2010) Treatment and post-treatment effects of facemask therapy on the sagittal pharyngeal dimensions in Class III subjects. Eur J Orthod 32(3):346–350. https://doi.org/10.1093/ejo/cjp092
Abe-Nickler MD, Portner S, Sieg P, Hakim SG (2017) No correlation between two-dimensional measurements and three-dimensional configuration of the pharyngeal upper airway space in cone-beam computed tomography. J Craniomaxillofac Surg 45(3):371–376. https://doi.org/10.1016/j.jcms.2017.01.004
Aboudara C, Nielsen I, Huang JC, Maki K, Miller AJ, Hatcher D (2009) Comparison of airway space with conventional lateral headfilms and 3-dimensional reconstruction from cone-beam computed tomography. Am J Orthod Dentofac Orthop 135(4):468–479. https://doi.org/10.1016/j.ajodo.2007.04.043
Burkhard JP, Dietrich AD, Jacobsen C, Roos M, Lubbers HT, Obwegeser JA (2014) Cephalometric and three-dimensional assessment of the posterior airway space and imaging software reliability analysis before and after orthognathic surgery. J Craniomaxillofac Surg 42(7):1428–1436. https://doi.org/10.1016/j.jcms.2014.04.005
El H, Palomo JM (2014) Three-dimensional evaluation of upper airway following rapid maxillary expansion: a CBCT study. Angle Orthod 84(2):265–273. https://doi.org/10.2319/012313-71.1
Nguyen T, De Clerck H, Wilson M, Golden B (2015) Effect of Class III bone anchor treatment on airway. Angle Orthod 85(4):591–596. https://doi.org/10.2319/041614-282.1
Tsolakis IA, Venkat D, Hans MG, Alonso A, Palomo JM (2016) When static meets dynamic: comparing cone-beam computed tomography and acoustic reflection for upper airway analysis. Am J Orthod Dentofac Orthop 150(4):643–650. https://doi.org/10.1016/j.ajodo.2016.03.024
Cevidanes L, Baccetti T, Franchi L, McNamara JA Jr, De Clerck H (2010) Comparison of two protocols for maxillary protraction: bone anchors versus face mask with rapid maxillary expansion. Angle Orthod 80(5):799–806. https://doi.org/10.2319/111709-651.1
De Clerck HJ, Cornelis MA, Cevidanes LH, Heymann GC, Tulloch CJ (2009) Orthopedic traction of the maxilla with miniplates: a new perspective for treatment of midface deficiency. J Oral Maxillofac Surg 67(10):2123–2129. https://doi.org/10.1016/j.joms.2009.03.007
Nienkemper M, Wilmes B, Franchi L, Drescher D (2015) Effectiveness of maxillary protraction using a hybrid hyrax-facemask combination: a controlled clinical study. Angle Orthod 85(5):764–770. https://doi.org/10.2319/071614-497.1
Willmann JH, Nienkemper M, Tarraf NE, Wilmes B, Drescher D (2018) Early Class III treatment with Hybrid-Hyrax-Facemask in comparison to Hybrid-Hyrax-Mentoplate—skeletal and dental outcomes. Prog Orthod 19(1):42. https://doi.org/10.1186/s40510-018-0239-8
Miranda F, Bastos JCC, dos Santos AM, Vieira LS, Aliaga-Del Castillo A, Janson G, Garib D (2020) Miniscrew anchored maxillary protraction in growing Class III patients. J Orthod 47(2):170–180. https://doi.org/10.1177/1465312520910158
Schulz KF, Altman DG, Moher D, Group C (2010) CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. PLoS Med 7(3):e1000251. https://doi.org/10.1371/journal.pmed.1000251
Nguyen T, Phillips C, Paniagua B (2016) The use of SPHARM-PDM and mean latitude axis to evaluate airway changes. Angle Orthod 86(6):943–948. https://doi.org/10.2319/110815-753.1
Pinheiro ML, Yatabe M, Ioshida M, Orlandi L, Dumast P, Trindade-Suedam IK (2018) Volumetric reconstruction and determination of minimum crosssectional area of the pharynx in patients with cleft lip and palate: comparison between two different softwares. J Appl Oral Sci 26:e20170282–e20170282. https://doi.org/10.1590/1678-7757-2017-0282
Vicory J, Pascal L, Hernandez P, Fishbaugh J, Prieto J, Mostapha M, Huang C, Shah H, Hong J, Liu Z, Michoud L, Fillion-Robin JC, Gerig G, Zhu H, Pizer SM, Styner M, Paniagua B (2018) SlicerSALT: Shape AnaLysis Toolbox. Shape Med Imaging 11167:65–72. https://doi.org/10.1007/978-3-030-04747-4_6
Faul F, Erdfelder E, Lang AG, Buchner A (2007) G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods 39(2):175–191. https://doi.org/10.3758/bf03193146
Pandis N (2012) Randomization. Part 3: allocation concealment and randomization implementation. Am J Orthod Dentofac Orthop 141(1):126–128. https://doi.org/10.1016/j.ajodo.2011.09.003
Aura-Tormos JI, Garcia-Sanz V, Estrela F, Bellot-Arcis C, Paredes-Gallardo V (2019) Current trends in orthodontic journals listed in Journal Citation Reports. A bibliometric study. Am J Orthod Dentofac Orthop 156(5):663–674 e661. https://doi.org/10.1016/j.ajodo.2019.01.019
Aloufi F, Preston CB, Zawawi KH (2012) Changes in the upper and lower pharyngeal airway spaces associated with rapid maxillary expansion. ISRN Dent 2012:290964–290965. https://doi.org/10.5402/2012/290964
Behrents RG, Shelgikar AV, Conley RS, Flores-Mir C, Hans M, Levine M, McNamara JA, Palomo JM, Pliska B, Stockstill JW, Wise J, Murphy S, Nagel NJ, Hittner J (2019) Obstructive sleep apnea and orthodontics: an American Association of Orthodontists White Paper. Am J Orthod Dentofac Orthop 156(1):13–28 e11. https://doi.org/10.1016/j.ajodo.2019.04.009
El H, Palomo JM (2010) Measuring the airway in 3 dimensions: a reliability and accuracy study. Am J Orthod Dentofac Orthop 137(4 Suppl):S50 e51–S50 e59. https://doi.org/10.1016/j.ajodo.2010.01.014
Guijarro-Martinez R, Swennen GR (2011) Cone-beam computerized tomography imaging and analysis of the upper airway: a systematic review of the literature. Int J Oral Maxillofac Surg 40(11):1227–1237. https://doi.org/10.1016/j.ijom.2011.06.017
Weissheimer A, Menezes LM, Sameshima GT, Enciso R, Pham J, Grauer D (2012) Imaging software accuracy for 3-dimensional analysis of the upper airway. Am J Orthod Dentofac Orthop 142(6):801–813. https://doi.org/10.1016/j.ajodo.2012.07.015
Zimmerman JN, Vora SR, Pliska BT (2018) Reliability of upper airway assessment using CBCT. Eur J Orthod 41(1):101–108. https://doi.org/10.1093/ejo/cjy058
Bhattacharyya N, Blake SP, Fried MP (2000) Assessment of the airway in obstructive sleep apnea syndrome with 3-dimensional airway computed tomography. Otolaryngol Head Neck Surg 123(4):444–449. https://doi.org/10.1067/mhn.2000.109367
Kilinc AS, Arslan SG, Kama JD, Ozer T, Dari O (2008) Effects on the sagittal pharyngeal dimensions of protraction and rapid palatal expansion in Class III malocclusion subjects. Eur J Orthod 30(1):61–66. https://doi.org/10.1093/ejo/cjm076
Zhao T, Zhang X, Ngan P, Yuan W, Chen X, Hua F, He H (2020) Effects of maxillary skeletal expansion on upper airway airflow: a computational fluid dynamics analysis. J Craniofac Surg 31(1):e6–e10. https://doi.org/10.1097/SCS.0000000000005806
Buck LM, Dalci O, Darendeliler MA, Papageorgiou SN, Papadopoulou AK (2017) Volumetric upper airway changes after rapid maxillary expansion: a systematic review and meta-analysis. Eur J Orthod 39(5):463–473. https://doi.org/10.1093/ejo/cjw048
Oliveira De Felippe NL, Da Silveira AC, Viana G, Kusnoto B, Smith B, Evans CA (2008) Relationship between rapid maxillary expansion and nasal cavity size and airway resistance: short- and long-term effects. Am J Orthod Dentofac Orthop 134(3):370–382. https://doi.org/10.1016/j.ajodo.2006.10.034
Abdalla Y, Brown L, Sonnesen L (2019) Effects of rapid maxillary expansion on upper airway volume: a three-dimensional cone-beam computed tomography study. Angle Orthod 89(6):917–923. https://doi.org/10.2319/101218-738.1
Ogawa T, Enciso R, Shintaku WH, Clark GT (2007) Evaluation of cross-section airway configuration of obstructive sleep apnea. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 103(1):102–108. https://doi.org/10.1016/j.tripleo.2006.06.008
Alwadei AH, Galang-Boquiren MTS, Kusnoto B, Costa Viana MG, Lin EY, Obrez A, Evans CA, Masoud AI (2018) Computerized measurement of the location and value of the minimum sagittal linear dimension of the upper airway on reconstructed lateral cephalograms compared with 3-dimensional values. Am J Orthod Dentofac Orthop 154(6):780–787. https://doi.org/10.1016/j.ajodo.2018.01.022
Acknowledgements
The authors thank PecLab (Belo Horizonte, Brazil) and Morelli (Sorocaba, Brazil) for the support.
Funding
This study was financed in part by the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior—Brasil (CAPES)—Finance Code 001 and by the São Paulo Research Foundation, FAPESP (grants # 2017/04141-9, 2017/24115-2 and 2019/03175-2).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
In this article, all procedures involving human participants were in accordance with the ethical standards of the Research Ethics Committee of Bauru Dental School, University of São Paulo, Brazil (protocol number 67610717.7.0000.5417).
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is based on research submitted by Dr. Felicia Miranda in partial fulfillment of the requirements for the degree of Ph.D. in Orthodontics at Bauru Dental School, University of São Paulo.
Rights and permissions
About this article
Cite this article
Miranda, F., Garib, D., Pugliese, F. et al. Upper airway changes in Class III patients using miniscrew-anchored maxillary protraction with hybrid and hyrax expanders: a randomized controlled trial. Clin Oral Invest 26, 183–195 (2022). https://doi.org/10.1007/s00784-021-03989-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-021-03989-3