Abstract
Objective
To carry out molecular characterization and determine the antibacterial activity of oral antibiotics and copper nanoparticles (Cu-NPs) against endodontic strains isolated from persistent infections.
Materials and methods
Root canal samples from 24 teeth in different patients with persistent endodontic infections were obtained. The isolated strains were identified by biochemical tests and 16S rDNA sequencing. Genotyping was achieved by molecular methods. The antibacterial activity of antibiotics and copper nanostructures was determined by using minimum inhibitory concentration (MIC) and minimum bactericidal concentration (MBC) values. Furthermore, a time-kill kinetics assay was evaluated. Nonparametric tests (Kruskal-Wallis ANOVA) were performed (p value <0.05).
Results
Twenty-one isolated strains were identified. Six isolates of Enterococcus faecalis were grouped into two clusters of three isolates each, two of which were clones. All were clarithromycin-resistant and erythromycin. Eight Pseudomonas putida presented two clusters, two Pseudomonas spp. were not clonal, and all were resistant to the tested antibiotics except tetracycline. Two of five strains of Cutibacterium acnes were clonal, and all were resistant only to metronidazole. The lowest MIC and MBC values were obtained with Cu-NPs. Time-kill kinetics using Cu-NPs showed a significant decrease in all tested species within 4 h and reached 100% in 2 h for C. acnes.
Conclusion
In this study, in relation to health care-associated infections, endodontic strains of each species isolated at least in one patient were polyclonal. In Pseudomonas spp., at least one clone was shared between patients. E. faecalis and C. acnes strains were susceptible to low Cu-NP concentrations, while Pseudomonas spp. strains were resistant.
Clinical relevance
Assessing and keeping track of the susceptibility of clinical strains to antimicrobial compounds is important for the clinical outcome. Based on our results, Cu-NPs could be an alternative for endodontic treatment, in order to avoid selection of resistant strains.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Recently, there has been an increase in the number of multiple drug-resistant microorganisms, and the field of oral microbiology has also been affected by this phenomenon [1]. In this context, persistent endodontic infections can be caused by microorganisms that are involved in primary infection, which can somehow able to resist endodontic disinfection procedures and subsequent lack of nutrients [2]. Enterococcus faecalis has been considered for many years, the main species responsible for endodontic treatment failures [3, 4]. However, some current studies report that other species may be predominant pathogens that are associated with secondary endodontic infections [5,6,7,8,9]. In some of them, persistent endodontic infections are considered as polymicrobial infections that involve fewer species than primary infections. The assertion may be open to debate because the diversity of persistent infections may be associated with a combination of factors that include differences in inclusion/exclusion criteria, dental treatments, or methodologies used to sample or analyze the microbiota, among others [5,6,7,8,9,10,11]. A high prevalence of Pseudomonas spp. has been observed, and their presence is associated with contamination by filtration from saliva to the root canal [9,10,11]. Additionally, Cutibacterium (formerly Propionibacterium) acnes [12] that are isolated from refractory endodontic lesions are considered opportunistic pathogens acquired during endodontic treatment and induce health care-associated infections (HCAI) [13]. Endodontic nosocomial infections, more accurately endodontic HCAI, that are derived from commonly used consumables such as gutta-percha tips, gloves, and rubber dams, as well as avoiding the use of these, can impact on the results of endodontic treatments [14]. Moreover, differences have been reported regarding their genotypes and profiles of sensitivity to antibiotics. These differences have been associated with geographical origin, where Latin American countries have shown lower susceptibility to antibiotics that are commonly used in dentistry [15]. For those strains of endodontic origin, a sustained increase in the antimicrobial resistance of anaerobes isolated from primary endodontic infections over a period of time has been observed [16]. The selection of resistant strains due to the use and abuse of antimicrobial agents has currently generated public health concerns in many countries [17, 18], and the oral microbiome could act as a reservoir for the genes involved in antibiotic resistance [19, 20]. The possible genetic relationships of endodontic isolates and their correlations with their antimicrobial susceptibility have not yet been described.
Currently, there is growing interest in the use of metallic nanoparticles as antimicrobials to control various infections, including those affecting the oral cavity, since, on the one hand, they possess biocidal properties and anti-adhesive capabilities against biofilms, and, on the other, they could also be used as alternatives to prevent superbacteria emergence due to antibiotic resistance [21, 22].
The antimicrobial mechanism of metal nanoparticles is not completely clear yet. It acts on multiple targets. The size and release of ions play a primary role in the antimicrobial effect of metal nanoparticles, considered a reservoir for controlled ion release [21,22,23]. Among metal and metallic nanoparticles, silver nanoparticles are most tested as a possible treatment for microbial infections. Nevertheless, other metallic nanoparticles, such as zinc oxide, gold, and copper, are being studied for antibacterial treatment too [23, 24].
Regarding endodontic treatments, bacteria establish and form biofilms in the small dentinal tubules. Here, copper nanostructures can play a role as antibacterial agents able to reach locations where other antimicrobials cannot [21, 24]. Recent findings show the ability of copper nanoparticles to penetrate the cytoplasm of microbes leaving the cell wall intact and, on the other hand, formed spectacular hierarchical metal oxide marigold-like nanostructures with sharp petals that could cause cellular death, suggesting a dual antimicrobial mechanism [25]. Copper possesses contact antibacterial properties; its application time could be reduced to the minimum time required to avoid selecting resistant pathogenic microbes [18, 22, 25].
The purpose of this study was to determine the antibacterial activity of antibiotics that are commonly used in dentistry and of copper nanoparticles (Cu-NPs) against molecularly characterized endodontic strains related with health care-associated infections.
Materials and methods
Isolation and identification of strains
This study was conducted according to the protocol approved by the Ethics Committee of the School of Dentistry. All subjects agreed to participate in the study by signing an informed consent form (C.I.Y.B. No. 04/15). Bacteriological samples were collected from 24 teeth in different patients who had been diagnosed with previously treated, apical periodontitis, with strict asepsis by a single trained operator. Clinical conditions and methodological details were previously described by Sánchez-Sanhueza et al. regarding metagenomic approach complementary to this study [9]. From each tooth, 2 samples in equal conditions were taken, one for next-generation sequencing [9] and one for bacterial cultures for this study. Briefly, three sterile paper tips were placed at the working length to obtain samples from the root canals. The paper tips were transferred to 1.5-mL cryotubes containing 0.75 mL of reduced transport fluid broth (RTF) and were processed within 3 h. All samples were seeded under aerobic and anaerobic conditions, and up to five dilutions were made to obtain isolated colonies. Under aerobic conditions, each sample was seeded on BHI agar (Oxoid Ltd., Basingstoke, UK) for 48 h at 37°C. From each bacterial plate, different representative pure colonies were isolated according to their macroscopic differences (e.g., shape, color, appearance, and elevation). Each colony was initially characterized microscopically according to its Gram stain, shape, and group. In addition, the production of catalase and oxidase was tested. Under anaerobic conditions, each sample was cultivated as described by Gomes et al. [16]. Plates were incubated at 37°C under anaerobic conditions in a 2.5-L GENbox anaerobic jar (Biomerieux, Marcy-l’Etoile, France) with a GENbox anaerobiosis sachet generator (Biomerieux, Marcy-l’Etoile, France) for 7 days. Different representative pure colonies were isolated from each bacterial plate according to their macroscopic differences, as described above, and were incubated in anaerobic basal broth (Oxoid Ltd., Basingstoke, UK). These strains were then grown in an aerobic environment to separate strict anaerobes from facultative anaerobes. Strict and facultative aerobic strains of Enterobacteriaceae and other nonfermenting gram-negative bacilli were initially identified using a biochemical scale. Identification was then corroborated by the use of an API 20E biochemical identification kit (BioMerieux, Marcy-l’Etoile, France). Strict and facultative aerobic strains and gram-positive coccus strains were further characterized according to their ability to grow in NaCl and perform hemolysis. Strains that were presumed to be strict anaerobes were subjected to identification using the Rapid ID 32A biochemical identification kit (BioMerieux, Marcy-l’Etoile, France). Finally, species identification was corroborated by 16S rRNA sequencing [26].
Molecular typing of isolates
Six E. faecalis isolates from different samples that were obtained from root canals were genotyped by genome macrorestriction followed by pulsed field gel electrophoresis using phage lambda as a control (BioLabs, New England) according to a previously described protocol [27, 28]. Briefly, plugs of each E. faecalis strain were digested with SmaI (1000 U) and incubated for 4 h at 25°C. Then, genomic DNA restriction fragments were separated by 1.8% agarose gel electrophoresis and run for 19 h at 14°C in a contour-clamped homogenous electric field machine (Enduro Power Supplies 250 V; Labnet International, NJ, USA). The gel was added to 5 μL of SafeView (Applied Biological Materials Inc.) for later viewing under ultraviolet light (Uvitec, Cambridge). On the other hand, ten Pseudomonas spp. isolates from different samples were genotyped by random amplification of polymorphic DNA (RAPD), according to Aslam M and Service C [29], with some modifications to determine the clonal relationships of strains [13, 30]. The DNA of Pseudomonas spp. was extracted using InstaGene Matrix (Bio-Rad Laboratories, USA), and a 20-μL PCR mixture consisting of 1 μL of DNA, 1x Master mix of GoTaq Green (Promega, USA), and 0.5 μM oligonucleotide (5′-AGCGGGCCAA-3′) was used. PCR amplification was performed in a thermocycler (MiniAmp Plus, Applied Biosystems by Thermo Fisher Scientific, USA) according to the following protocol: 1 cycle, 5 min each at 94°C, 40°C, and 72°C; 30 cycles, 1 min at 94°C, 1 min at 36°C, and 2 min at 72°C; 1 cycle, 5 min at 94°C, 1 min at 50°C, and 2 min at 72°C; and a final extension for 7 min at 72°C. The amplified DNA fragments were separated on 1.8% agarose gel in an electrophoresis chamber (Enduro Power Supplies 250 V; Labnet International, NJ, USA) at 70 V for 1.5 h. A MassRuler DNA mixing scale (Thermo Fisher Scientific Inc, USA) was included as a size marker.
Phylogenetic analysis of five C. acnes strains was performed by partial sequencing of recA gene. C. acnes recA gene was amplified using the primers PAR-1 and PAR-2 [31], which generated a 1201-bp amplicon. The reaction mixture consisted of 0.5 μL of PAR-1 (concentration, 10 pmol/μL; Sigma); 0.5 μL of PAR-2 concentration, 10 pmol/μL; Sigma); 23 μL of Reddymix (Thermo Scientific); and 1 μL of DNA in a final volume of 25 μL. Thermal cycling conditions included an initial denaturation at 95°C for 3 min, denaturation at 95°C for 1 min, annealing at 55°C for 30 s, and extension at 72°C for 90 s, which were repeated for 35 cycles, and a final extension at 72°C for 10 min. The amplified products were temporarily stored at 4°C. The amplified products were processed on 0.5% agarose gel and visualized under UV transillumination and were subsequently shipped to Macrogen (Seoul, Korea) for Sanger sequencing.
Synthesis and characterization of Cu-NP
Cu-NPs were synthesized using the controlled atmosphere arc discharge method (DARC-AC). DARC-AC is a continuous physical vapor deposition technique, in which a thin wire is used as a metallic precursor and is vaporized by a strong electric arc discharge. In the process, the metallic wire is fed to the system at a constant rate. Due to the high current that passes through the wire, a continuous arc is produced. As a result, the metallic precursor is transformed into a superheated vapor cloud, which expands, collides with atmospheric molecules, and cools down to produce homogeneous nucleations of nanoparticles. The protocol of Jaramillo [32] was used for the synthesis process to produce the nanoparticles. Commercial high-purity 2-mm diameter Cu wire (99.99%) (Sulzer, Winterthur, Switzerland) was used as the metallic precursor, and argon was used as a gaseous precursor with a flow of 500 sccm. The operating voltage and current were 25 V and 30 A, respectively. The arc inclination angle was 40° with an electrode distance of 0.5 cm. The reaction was conducted at 1 atm, and both the reaction and accumulation chambers were enriched with argon before discharge. Cu-NPs of approximately 4.6 mm in size were used. High-resolution transmission electron microscopy (HRTEM) was performed in a JEM-ARM200F (JEOL, USA) probe aberration corrected analytical microscope with a resolution of 0.08 nm. Selected area electron diffraction was performed in a JEOL 2010F operating at 200 kV (point resolution of 0.19 nm). TEM Digital Micrograph™ 3.7.0 software by Gatan (Pleasanton, CA, USA) was used for TEM image processing. Measurements of particle size population diameters were randomly chosen, and the obtained data were represented by a histogram. Therefore, the mean particle size was fitted with a normal distribution.
Antimicrobial susceptibility testing
For the antibiotics that are commonly used in dentistry, tests were performed based on the recommendations given by Kuriyama et al. according to the Clinical and Laboratory Standard Institute (CLSI/M100-S27) [26, 33]. For the nanoparticle tests, the CLSI recommendations were used as a reference, and modifications were made as described by Vargas-Reus et al. Copper nanowires (Cu-NW) and zinc oxide nanoparticles (ZnO-NP) were used as controls [34]. Amoxicillin (AMX), amoxicillin/clavulanate (AMC), tetracycline (TET), clarithromycin (CLR), erythromycin (ERY), and metronidazole (MTZ) were tested [15]. MIC were determined for all strains by the E-test technique (Biomerieux, Marcy-l’Etoile, France) [10]. The breakpoints to antibiotics were determined by CLSI, 2017. For infrequent bacteria, the CLSI document M45-Methods for Antimicrobial Dilution and Disk Susceptibility Testing of Infrequently Isolated or Fastidious Bacteria [26] was consulted to assess the Cu-NPs effect,;antimicrobial activity of nanoparticles against oral strains previously reported was consulted, to compare CMI and CMB values [34].
Determination of time-kill kinetics with Cu-NPs
Time-killing kinetics were determined for a representative strain of each species using the plate count technique. Dilutions of 2500; 1000; 500; 250; and 100 μg/mL Cu-NPs were tested. Sampling times for performing bacterial counts were 0, 1, 2, 3, and 4 h. Three repeated experiments were performed at three different times. To assess the Cu-NP effect of time-kill kinetics assays, antimicrobial activity of nanoparticles against medical clinical strains was compared to those previously reported [35].
Statistical and bioinformatic analysis
For genotypic comparisons, E. faecalis PFGE gels were analyzed with BioNumerics software, version 6.3 (Applied Maths, Inc., Austin, TX, USA). Normalization was performed according to the three control lanes with lambda phage on the gel. The bands used for analysis were manually assigned according to the densitometric curves and gel images. The criterion used for constructing the PFGE clusters was a Dice coefficient with a tolerance level of 1.5–2%. Finally, a dendrogram of clusters was constructed using the UPGMA computational method, and 85% was established as the cutoff for classifying a closely related group [36].
RAPD fingerprints of P. putida were analyzed with GelJ software, version 2.0. Similarities between Pseudomonas spp. DNA patterns based on band positions were determined using the Dice similarity coefficient. Finally, a dendrogram of the clusters was constructed using the UPGMA computational method, and 85% was established as the cutoff for classifying closely related groups [37].
For phylogenetic C. acnes comparisons, recA sequences were submitted for closest matches to the NCBI nucleotide database using the Basic Local Alignment Search Tool (http://0-www.ncbi. nlm.nih.gov.ilsprod.ilb.neu.edu/BLAST/). Additionally, representative recA nucleotide sequences from types IA, IB, II, and III were retrieved from GenBank. The sequences were analyzed, aligned, and trimmed, and a phylogenetic tree was constructed using Geneious® 9.1.8 software [38]. Acidipropionibacterium jensenii was used as an outgroup to root the tree. We employed the neighbor-joining method and the Jukes-Cantor genetic distance model, with 9999 bootstrap resampling replicates.
Data from antibacterial activity were entered into Microsoft Excel spreadsheets for analysis. Nonparametric tests (Kruskal-Wallis ANOVA) were performed. A p value <0.05 was considered a significant difference. SPSS software (SPSS, Chicago, USA, version 23) was used.
Results
Isolation and identification of species
A total of 13 bacterial colonies were selected from aerobic cultures according to their macroscopic differences (e.g., shape, color, and appearance). Initially, according to microscopic and biochemical analyses, ten isolates were classified as Pseudomonas spp. and the other three isolates were classified as cocci or coccobacillary; all were Gram-positive and were presumably of the genus Enterococcus spp. Under anaerobic conditions, eight colonies were isolated, which corresponded to gram-positive bacteria. Five strains that were identified using the Rapid ID 32A identification kit (BioMerieux, Marcy-l’Etoile, France) were classified as strict anaerobes. According to the microscopic and biochemical analyses, three facultative anaerobic strains were classified mainly as cocci or coccobacillary-shaped, all were Gram-positive and were presumably of the genus Enterococcus spp. All strains were sequenced over 1000 base pairs (bp). Good sequencing quality was obtained, and separate peaks were observed with Signal G values above 200. Most bacteria showed similarities of 98–99% with each other; consequently, they were considered part of the same species. The lower percentages found ranged from 95 to 97%; bacteria in this range were considered to belong to the same genus. Summaries with percentages of similarity and accession numbers were registered. Isolation and identification are summarized in Table 1.
Molecular typing of isolates
PFGE analysis of E. faecalis isolates showed two clades with genetic relatedness < 85% (72.3%), each of which formed three strains. Strains 11.2 and 11.3 as well as strains E1 and E2 were indistinguishable among them and corresponded to clonal strains. Strains 11.1 and C1 are not genetically related. The C1 strain is closely related to the E1 and E2 strains, just as the 11.1 strain is closely related to the 11.3 and 11.2 strains (Fig. 1).
RAPD fingerprint analysis with GelJ software, version 2.0, showed two band patterns for P. putida isolates: two clusters were observed according to the band patterns; strains 15.1, 15.2, 13.2, 14.1, and 9.3 were clonal, while strains 6.1, 6.2, and 9.1 were clonal among them. Strains 15.1 and 15.2 demonstrated monoclonality in the same patient, whereas strains 9.3 and 9.1 demonstrated polyclonal monoclonality in the same patient.
The genetic relationship between strains 14.3 and 14.1, which corresponded to Pseudomonas spp., indicates that they correspond to two pulsotypes with a relationship between them <85% (Fig. 2).
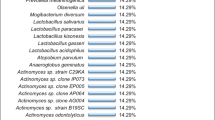
Regarding C. acnes, based on sequence alignment, A1 and A2 had 100% recA sequence similarity and were closely related to strains G1 and E3. In addition, the phylogenetic tree indicates that isolate B1 diverges significantly from the other four isolates of C. acnes that were analyzed in this study, as supported by the 100% bootstrap value. Strains A1 and A2 with isolates G1 and E3 are more closely related to the representative from type IB than to the other types. As expected, the IA representative clustered with IB, while types II and III make up their own branches, with good support from the model. Isolate B1 is located in its own branch away from all other C. acnes representatives. It is worth noting that the recA nucleotide sequence of isolate B1 differs significantly from those of the other isolates, with less than 90% similarity with the other recA sequences. While all other isolates (e.g., A1, A2, E3, and G1) and reference strains (e.g., types IA, IB, II, and III) analyzed share at least 98% similarity among themselves. Of note, the nearest hit for isolate B1 in the NCBI nucleotide database is for an isolate of a proposed new species, Propionibacterium namnetense sp. nov. (accession number KU847778.1), which was isolated from human bone infection. Isolate B1 shares 99.23% recA identity with this strain (sequence coverage 98% E-value 0.0), while it shares only 91% identity with the nearest hit of C. acnes recA. All other isolates of C. acnes in this study share at least 99% identity with C. acnes recA in the database (Fig. 3).
Phylogenetic tree of Cutibacterium acnes isolates based on recA nucleotide sequences; branch node labels show consensus support (%) out of 9999 bootstrap resampling replicates; Acidipropionibacterium jensenii was used as an outgroup to root the tree. A1 and A2 have 100% sequence similarity; bootstrap support percentages are indicated on the nodes. Scale bar = substitutions per site. Sequences retrieved from GenBank: type IA accession number AY642055.1, type IB accession number EU687255.1, type II accession number AY642061, and type III accession number DQ672252
The sequences from the 5 Cutibacterium spp. strains are available at the NCBI Sequence Read Archive under the accession numbers MW455340 (A1); MW455341 (A2); MW455342 (B2); MW455343 (E3); and MW455344 (G1).
Characterization of Cu nanoparticles
Figure 4 shows the characterization of nanoparticles used in this study. The micrograph in Fig. 4a shows that the Cu-NPs are not agglomerated, and they preferably have a spherical morphology. Figure 4b shows an image at higher magnification, where the morphology of the Cu-NPs can be seen in greater detail. Crystalline planes are observed (Fig. 4c) that have an interplanar distance of 0.21 nm, which corresponds to the plane (111) FCC metallic copper. Figure 4d shows an image of the electron diffraction pattern of the nanoparticles. This shows that the nanoparticles are polycrystalline and present crystalline planes (200), (111), and (220), which correspond to metallic copper and are in agreement with the results obtained in the high-resolution microscopy images (Fig. 4c). The average size of the nanoparticles is 4.56 nm, with dispersion ranges of 2.34 and 8.7 nm (Fig. 4e).
Antimicrobial susceptibility testing
A summary of the MIC results for the more common antibiotics used in endodontics obtained by the E-test (Biomerieux, Marcy-l’Etoile, France) is presented in Table 2. Six isolates of E. faecalis were resistant to clarithromycin and erythromycin. Eight isolates of Pseudomonas spp. and two P. putida were resistant to all antibiotics tested except tetracycline. All C. acnes were resistant only to metronidazole.
The lowest MIC and MBC values were obtained with Cu-NPs (Table 3). Cu-NP MIC and MBC values were in the ranges of 130 to >2000 μg/mL and 300 to >2.500 μg/mL, respectively.
Time-kill kinetics with Cu-NPs
The E. faecalis strains were selected according to their molecular profile, with all selected strains having less than 85% similarity between them. In the case of C. acnes, the three most distant strains were selected. Pseudomonas spp. was not tested due to the high MIC and CMB values reported in the previous assay. Six strains tested with Cu-NPs for a period of 4 h showed a very fast concentration-dependent bactericidal effect. Bacterial reductions were significant and reached 100% in several cases: 1 h for C. acnes A1 (Fig. 5a), within 2 h for C. acnes E3 (Fig. 5b), and within 3 h for C. acnes G1 (Fig. 5c). All species responded to the tested concentrations, and in the case of C. acnes A1 and C. acnes E3, statistical analysis indicated that there were significant differences in the antimicrobial activity of the five concentrations of nanoparticles tested (P <0.05) when comparing the higher dose of 2500 μg/mL with the dose of 100 μg/mL. However, for the other four strains evaluated, significant differences were also found between the tested concentrations (P<0.05). C. acnes A1 was the most sensitive strain after 1 h of exposure to 100 μg/mL, followed by C. acnes G1. Only in the latter was there a reduction of three logarithms in that period of time. E. faecalis C1 (Fig. 5d) was the least susceptible strain in the 4-h exposure to 2500 μg/mL, followed by E. faecalis 11.3 and 11.1 (Fig. 5e–5f). Both strains showed a reduction of three logarithms at 3 h.
Discussion
Recent metagenomic studies of persistent endodontic infections have reported only a moderate presence of E. faecalis and contradict what was indicated years ago as the most prevalent species in this pathology and report the presence of other prevalent genera including Pseudomonas spp. and Cutibacterium spp. [5, 9, 11].
C. acnes is the most prevalent specie in primary endodontic infections with a history of or clinical evidence of communication with the oral environment, while it is absent in lesions without communication with the oral environment [13]. In addition, there is evidence that the C. acnes isolates of refractory endodontic infections, with or without periapical abscesses, are probably HCAIs that occur during root canal treatment [37]. It has been reported that endodontic C. acnes strains are predominantly phylotype I, which is consistent with our report [13]. The B1 strain could be part of the polymorphism that this species can present. In this study, this strain is genetically distant from the remaining strains and genetically coincides with the C. namnetense that was isolated from human bone infection [38]. The recombination rates within C. acnes are lower than those found in other species but show plasticity that is evidenced in genetic analysis that reveals mosaics within the same population, which may explain the opportunistic role of C. acnes.
Pseudomonas spp. has been reported as a prevalent genus in the microbiota of persistent endodontic lesions, and its presence is associated with contamination by filtration from saliva to the root canal. This may suggest occurrence of secondary infections in some cases with adequate filled root canals and adequate restorations without any further contamination from the oral environment, probably as a consequence of a breach in the asepsis technique during treatment [7,8,9]; however, there are no reports yet regarding the molecular typing of endodontic isolates. The eight strains of Pseudomonas putida and two Pseudomonas spp. strains that were isolated in this report are considered strict aerobes; however, their oxygen requirements can change under anaerobic conditions by using an alternative electron acceptor, such as nitrate. The anoxic environment generated after canal filling and crown sealing could favor emergence of this bacterium, as it can use the available oxygen, which creates favorable conditions for facultative and strict anaerobic species. The components of the sealing materials could provide the necessary nitrogen source and favor the persistence of these bacteria inside the canals [39, 40]. The clonality of P. putida strains from different patients shows the probable presence of similar circulating clinical strains that reach the root canal system during or after endodontic treatment. There is evidence of a direct relationship with health care-associated infections [41].
The multidrug resistance of Pseudomonas spp. is due to numerous intrinsic or acquired mechanisms, such as a decrease in the permeability of the outer membrane, production of beta-lactamases, and presence of multidrug efflux pumps. Pseudomonas spp. has been reported to be resistant to sulfamethoxazole, erythromycin, amoxicillin, ampicillin, chloramphenicol, trimethoprim, rifampicin, and ceftazidime, as well as colistin and tetracycline. Resistance to multiple drugs, which involved up to 13 antibiotics (65% of Pseudomonas spp. are resistant to between 8 and 13 antibiotics), was found, which was produced by practically all known mechanisms of antimicrobial resistance [39]. Our results show high levels of resistance to the most commonly used antibiotics for treating of odontogenic infections. There are no reports of antimicrobial susceptibility of Pseudomonas spp. that are isolated from endodontic pathologies.
The genotypic similarity of E. faecalis in different patients, as occurs between certain strains in the present study, is not completely clarified. In the study by Vidana et al. [42], intrapatient and interpatient strains that were obtained from root canals were clonal, and it can be established that there is a possible connection among the strains circulating in the clinical environment [27].
Regarding the sensitivity profiles of antibiotics of dental clinical importance in E. faecalis, our report demonstrated differences despite the close genetic relationship. In six E. faecalis strains, with an MIC50 of 0.25 μg/mL AMX, a strain with a 48-μg/mL MIC was isolated for AMX. All E. faecalis strains were susceptible to AMC and TET, and there were no strains that were susceptible to CLR and ERY. A study conducted in a Brazilian population agrees with our findings regarding the percentage of susceptibility [26]. Research on a German population indicates that among six E. faecalis strains, only one was resistant to AMX, and two were resistant to TET. Studies have further concluded that facultative anaerobic bacterial species were resistant to a series of clinically relevant antibiotics [43]. A study conducted in a Polish population showed a low percentage of E. faecalis strains that were susceptible to ERY [31]. Cutibacterium spp. is susceptible to most antibiotics used in dental treatments; however, it is highly resistant to MTZ [27, 31, 40], which agrees with the findings of our report. This is worrying because MTZ is one of the few options for treating infections that are caused by anaerobes. Presence of the ermC, tetM, and tetW genes has been reported in 6, 10, and 7 of 24 cases of asymptomatic apical periodontitis, respectively, which explains the low levels of susceptibility to these antibiotic groups, which is why researching the presence and expression of these and other resistance genes is suggested in future studies.
The microbiota associated with endodontic infections can survive in difficult environmental conditions, organized in a mature biofilm, and make root canal disinfection a challenge. Searching therapeutic options for adequate infection control becomes clinically relevant, combining culture-depend assays with molecular biology to understand the relationship between the microorganisms present and their behavior toward potential new antimicrobial molecules [18, 31].
The antimicrobial activity of the three types of nanoparticles tested against the 21 species of bacteria associated with persistent endodontic infections varied, with Cu-NPs showing the highest levels of activity, followed by Cu-NWs and ZnO-NPs. Regarding susceptibility of Gram-negative strains exposed to Cu-NPs, a very high MIC50 value was observed in comparison to previous reports, for which the values of 312 μg/mL and 325 μg/mL were 4 to 5 times lower. However, the differences lie mainly in the fact that our report included clinical aerobic strains and Cu was used in its pure state and not in an oxidative state, such as CuO or Cu2O. Previous research was conducted with anaerobic and American Type Control Culture (ATCC) strains, which are usually susceptible to antimicrobial tests [22]. Regarding the susceptibility of Gram-positive strains exposed to Cu-NPs, we observed an MIC50 of 100 μg/mL and MBC50 of 500 μg/mL. There are no previous reports of MIC/MBC of Cu-NPs on aerobic strains of oral origin. In reports on clinical strains that were isolated from other human pathologies, MBC values above 500 μg/mL have been observed [44].
The bactericidal effect of Cu-NPs on all species studied in this research suggests that Cu-NPs would induce death by contact, which implies that the release of ions in the local environment is necessary for optimal antimicrobial activity [22, 44]. Cu-NPs that cause death by contact are potentially useful for tackling the emerging resistance to conventional antimicrobial agents since in a short time, the action of simultaneous antimicrobial mechanisms makes the development of resistance to these nanoparticles unlikely [45]. The phenomenon of drug resistance is currently a global public health concern [12] due to the emergence of resistant strains due to the use and abuse of antimicrobial agents. These new strains have gained control of an ecological niche that was previously occupied by sensitive niches. This is precisely what happens during treating chronic infections, which will eventually leave clinicians without effective antimicrobial agents [13].
In the present study, differences in the reduction of biofilm bacteria by Cu-NPs compared to ZnO-NPs could be due to the higher production of ROS by dissolution of Cu-NPs, which were able to spread in the biofilm structure [24]. The ion release essay is not trivial and requires a challenge and equipment. To proceed, nanoparticles are needed that are so narrow in size that they are considered monodisperse. Then, promote oxidation that depends on the medium where the particles are to be tested. The amount of ions that are released would be difficult to measure before the hierarchical copper structures are formed [25]. The ion release (dissolution) needs to be studied and linked to the antibiofilm activity.
One of the limitations of the study is related to the methodological approach due the differences between planktonic monospecies and biofilm multispecies models. Recently a study using a combined approach showed strain-dependent antibacterial activity of ZnO-NPs and Cu-NPs and multispecies antibiofilm activity, after 10 min of exposure [46]. Those results were possibly due to using strains from culture banks, which are more susceptible to antimicrobial agents than clinical strains [18]. The present study used clinical strain culture methods and a monospecies approach, which could affect the time of action of copper nanoparticles due the resistant phenotype of the clinical strains used [18]. However, it is also important to highlight that under this laboratory conditions, there was bactericidal activity against C. acnes; that is, the CFU decreased 3 logarithms from the initial inoculum, at 1h of exposure to the two lowest concentrations of nanoparticles. Between 3 and 4 h were needed to achieve the same result for E. faecalis. The copper nanoparticles showed at least a bacteriostatic action; that is, the CFU decreased 3 logarithms from the initial inoculum, for all strains tested at the two lowest concentrations. In the present study, we test a type of nanoparticles in a rough presentation, a product from DARC technique synthesis, that could influence their antimicrobial activity in time-kill kinetics assays, especially due the early oxidation of the nanoparticles [25, 46]. An electrochemical combined synthesis method for nanoparticles allows obtaining kinetics and small ranges of nanoparticle size distribution [47]. With these nanoparticles, it is possible to synthesize nanostructured polymeric systems with functional properties from the use of surfactants and stabilizers with easily polymerizable functional groups, known as “surfmers.” An excellent candidate for a surfmer is polyvinyl alcohol (PVA), since it is a hydrophilic synthetic polymer, non-toxic, soluble in water, biodegradable, biocompatible, with good mechanical properties, and stable for long periods under different conditions, temperature, and pH. Hydrogels can be obtained from PVA by physical or chemical crosslinking, to enhance the antibacterial action of nanoparticles and reducing their toxicity by lowering the concentration and time of exposure to the minimum possible that could be applied in the endodontic field as an intracanal medicament in clinical conditions [47, 48].
Finally, we cannot fail to consider the potential toxicity of Cu-NPs. An in vitro study suggests that to perform toxicity testing of metallic nanoparticles, the administered dose (i.e., mass of sedimented nanoparticles per volume of suspension) should be considered rather than taking into account the dose administered alone (initial mass concentration of nanoparticles). From this, it was concluded that in vitro dose-response results depend on complex toxicodynamic reactions, which include nanoparticle/cell association-relation, activation of the response pathways of cells involved in the uptake of nanoparticles, and multiple physical-chemical parameters that influence the sedimentation and internalization of these [49]. Cu-NPs and ZnO-NPs are biocompatible at low antibacterial effective doses with human gingival fibroblasts (HGFs) and show a cytotoxic effect after more than 6 h of exposure [46]. It is suggested that more studies be conducted to evaluate the barrier capacity of apical constriction, in an ex vivo or in vivo model, in relation to the cytotoxicity of CuNPs on the periapical tissues.
In conclusion, it is necessary to continuously monitor the susceptibility of bacteria isolated from the oral environment to antibiotics, to determine their genetic relationships in order to understand their dissemination behavior, and to seek strategies to avoid the selection of antibiotic resistance, including the use of alternative antimicrobial agents, such as Cu-NPs. The results of this study show that genetically related bacterial strains isolated from persistent endodontic infections had low levels of susceptibility to antibiotics commonly used in dentistry. Also, we demonstrate that copper nanoparticles may be a viable alternative for disinfection in the treatment of endodontic infections.
References
Prestinaci F, Pezzotti P, Pantosti A (2015) Antimicrobial resistance: a global multifaceted phenomenon. Pathog Glob Health 109(7):309–318. https://doi.org/10.1179/2047773215Y.0000000030
Aw V (2016) Discuss the role of microorganisms in the aetiology and pathogenesis of periapical disease. Aust Endod J 42:53–59. https://doi.org/10.1111/aej.12159
Zhang C, Du J, Peng Z (2015) Correlation between Enterococcus faecalis and persistent intraradicular infection compared with primary intraradicular infection: a systematic review. J Endod 41(8):1207–1213. https://doi.org/10.1016/j.joen.2015.04.008
Borzini L, Condò R, De Dominicis P, Casaglia A, Cerroni L (2016) Root canal irrigation: chemical agents and plant extracts against Enterococcus faecalis. Open Dent J 10:692–703. https://doi.org/10.2174/1874210601610010692
Hong BY, Lee TK, Lim SM, Chang SW, Park J, Han SH, Zhu Q, Safavi KE, Fouad AF, Kum KY (2013) Microbial analysis in primary and persistent endodontic infections by using pyrosequencing. J Endod 39(9):1136–1140. https://doi.org/10.1016/j.joen.2013.05.001
Anderson AC, Al-Ahmad A, Elamin F, Jonas D, Mirghani Y, Schilhabel M et al (2013) Comparison of the bacterial composition and structure in symptomatic and asymptomatic endodontic infections associated with root-filled teeth using pyrosequencing. PLoS One 8(12):1–13. https://doi.org/10.1371/journal.pone.0084960
Tzanetakis GN, Azcarate-Peril AM, Zachaki SZ, Panopoulos P, Kontakiotis EG, Madianos PN et al (2015) Comparison of bacterial community composition of primary and persistent endodontic infections using pyrosequencing Giorgos. J Endod 41(8):1226–1233. https://doi.org/10.1016/j.joen.2015.03.010
Siqueira JFJ, Antunes HS, Rôças IN, Rachid CTCC, Alves FRF (2016) Microbiome in the apical root canal system of teeth with post-treatment apical periodontitis. PLoS One 11(9):1–14. https://doi.org/10.1371/journal.pone.0162887
Sánchez-Sanhueza G, Bello-Toledo H, González-Rocha G, Gonçalves AT, Valenzuela V, Gallardo-Escárate C (2018) Metagenomic study of bacterial microbiota in persistent endodontic infections using Next-generation sequencing. Int Endod J 51(12):1336–1348. https://doi.org/10.1111/iej.12953
Diaz PI, Dupuy AK, Abusleme L, Reese B, Obergfell C, Choquette L, Dongari-Bagtzoglou A, Peterson DE, Terzi E, Strausbaugh LD (2012) Using high throughput sequencing to explore the biodiversity in oral bacterial communities. Mol Oral Microbiol 27(3):182–201. https://doi.org/10.1111/j.2041-1014.2012.00642.x
Siqueira JFJ, Rôças IN (2014) Present status and future directions in endodontic. Endod Top 30:3–22. https://doi.org/10.1111/etp.12060
Scholz CFP, Kilian M (2016) The natural history of cutaneous propionibacteria, and reclassification of selected species within the genus Propionibacterium to the proposed novel genera Acidipropionibacterium gen. Nov., Cutibacterium gen. nov. and Pseudopropionibacterium gen. nov. Int J Syst Evol Microbiol 66(11):4422–4432. https://doi.org/10.1099/ijsem.0.001367
Niazi SA, Al Kharusi HS, Patel S, Bruce K, Beighton D, Foschi F, Mannocci F (2016) Isolation of Propionibacterium acnes among the microbiota of primary endodontic infections with and without intraoral communication. Clin Oral Investig 20(8):2149–2160. https://doi.org/10.1007/s00784-016-1739-x
Saeed M, Koller G, Niazi S, Patel S, Mannocci F, Bruce K, Foschi F (2017) Bacterial contamination of endodontic materials before and after clinical storage. J Endod 43(11):1852–1856. https://doi.org/10.1016/j.joen.2017.06.036
Veloo ACM, Seme K, Raangs E, Rurenga P, Singadji Z, Wekema-Mulder G, van Winkelhoff AJ (2012) Antibiotic susceptibility profiles of oral pathogens. Int J Antimicrob Agents 40(5):450–454. https://doi.org/10.1016/j.ijantimicag.2012.07.004
Gomes BPFA, Jacinto RC, Montagner F, Sousa ELR, Ferraz CCR (2011) Analysis of the antimicrobial susceptibility of anaerobic bacteria isolated from endodontic infections in brazil during a period of nine years. J Endod 37(8):1058–1062. https://doi.org/10.1016/j.joen.2011.05.015
Draft political declaration of the high-level meeting of the General Assembly on antimicrobial resistance. New York: United Nations. 2016. Available from: http://www.un.org/pga/71/wp-content/uploads/sites/40/2016/09/DGACM_GAEAD_ESCAB-AMR-Draft-Political-Declaration-1616108E.pdf
Lewis K (2010) Persister cells. Annu Rev Microbiol 64:357–372. https://doi.org/10.1146/annurev.micro.112408.134306
Kumiyama EY, Lepesqueur LSS, Yassuda CG, Samaranayake LP, Parahitiyawa NB, Balducci I et al (2016) Enterococcus species in the oral cavity: prevalence, virulence factors and antimicrobial susceptibility. PLoS One 11(9):1–11. https://doi.org/10.1371/journal.pone.0163001
Palma TH, Harth-Chú EN, Scott J, Stipp RN, Boisvert H, Salomão MF, Theobaldo JD, Possobon RF, Nascimento LC, McCafferty JW, Faller L, Duncan MJ, Mattos-Graner RO (2016) Oral cavities of healthy infants harbour high proportions of Streptococcus salivarius strains with phenotypic and genotypic resistance to multiple classes of antibiotics. J Med Microbiol 65(12):1456–1464. https://doi.org/10.1099/jmm.0.000377
Song W, Ge S (2019) Application of antimicrobial nanoparticles in dentistry. Molecules 15;24(6):1033. https://doi.org/10.3390/molecules24061033
Rudramurthy GR, Swamy MK, Sinniah UR, Ghasemzadeh A (2016) Nanoparticles: alternatives against drug-resistant pathogenic microbes. Molecules 21(7):1–30. https://doi.org/10.3390/molecules21070836
Vallet-Regí M, González B, Izquierdo-Barba I (2019) Nanomaterials as promising alternative in the infection treatment. Int J Mol Sci 4;20(15):3806. https://doi.org/10.3390/ijms20153806
Shrestha A, Kishen A (2016) Antibacterial nanoparticles in endodontics: a review. J Endod 42(10):1417–1426. https://doi.org/10.1016/j.joen.2016.05.021
Martínez A, Apip C, Meléndrez MF, Domínguez M, Sánchez-Sanhueza G, Marzialetti T, Catalán A (2020) Dual antifungal activity against Candida albicans of copper metallic nanostructures and hierarchical copper oxide marigold-like nanostructures grown in situ in the culture medium. J Appl Microbiol. https://doi.org/10.1111/jam.14859
Institute C and LS. Methods for dilution antimicrobial susceptibility tests for bacteria that grow aerobically; approved standard CLSI document M100-S27S27. Pennsylvania: Clinical and Laboratory Standards Institute. 2017. Available from: https://clsi.org/standards/products/microbiology/documents/m100/
Sánchez-Sanhueza G, M VC, Ulloa I, Pineda C, González-Rocha G et al (2018) Molecular typing of Enterococcus faecalis from persistent endodontic infections. Int J Odontostomat 12(1):113–119. https://doi.org/10.4067/S0718-381X2018000100113
Sedgley CM, Lennan SL, Clewell DB (2004) Prevalence, phenotype and genotype of oral enterococci. Oral Microbiol Immunol 19(2):95–101. https://doi.org/10.1111/j.0902-0055.2004.00122.x
Aslam M, Service C (2008) Genetic characterization of spoilage pseudomonads isolated from retail-displayed beef. Lett Appl Microbiol 47:153–157. https://doi.org/10.1111/j.1472-765X.2008.02411.x
Jungermann GB, Burns K, Nandakumar R, Tolba M, Venezia RA (2011) Fouad AF (2011) Antibiotic resistance in primary and persistent endodontic infections. J Endod 37(10):1337–1344. https://doi.org/10.1016/j.joen.2011.06.028
Rôças IN, Siqueira JFJ (2012) Characterization of microbiota of root canal-treated teeth with. J Clin Microbiol 50(5):1721–1724. https://doi.org/10.1128/JCM.00531-12
Jaramillo AF, Baez-Cruz R, Montoya LF, Medinam C, Pérez-Tijerina E, Salazar F, Rojas D, Melendrez MF (2017) Estimation of the surface interaction mechanism of ZnO nanoparticles modified with organosilane groups by Raman Spectroscopy. Ceram Int 43(15):11838–11847. https://doi.org/10.1016/j.ceramint.2017.06.027
Kuriyama T, Williams DW, Yanagisawa M, Iwahara K, Shimizu C, Nakagawa K, Yamamoto E, Karasawa T (2007) Antimicrobial susceptibility of 800 anaerobic isolates from patients with dentoalveolar infection to 13 oral antibiotics. Oral Microbiol Immunol 22(4):285–288. https://doi.org/10.1111/j.1399-302X.2007.00365.x
Vargas-Reus MA, Memarzadeh K, Huang J, Ren GG, Allaker RP (2012) Antimicrobial activity of nanoparticulate metal oxides against peri-implantitis pathogens. Int J Antimicrob Agents 40(2):135–139. https://doi.org/10.1016/j.ijantimicag.2012.04.012
Ren G, Hu D, Cheng EW, Vargas-Reus MA, Reip P, Allaker RP (2009) Characterisation of copper oxide nanoparticles for antimicrobial applications. Int J Antimicrob Agents 33(6):587–590. https://doi.org/10.1016/j.ijantimicag.2008.12.004
Větrovský T, Baldrian P (2013) The variability of the 16S rRNA gene in bacterial genomes and its consequences for bacterial community analyses. PLoS One 8(2):1–10. https://doi.org/10.1371/journal.pone.0057923
Downes J, Wade WG (2009) Propionibacterium acidifaciens sp. nov., isolated from the human mouth. Int J Syst Evol Microbiol 59(11):2778–2781. https://doi.org/10.1099/ijs.0.010470-0
Aubin G, Bémer P, Kambarev S, Patel N, Lemenand O, Caillon J (2016) Propionibacterium namnetense sp. nov., isolated from a human bone infection. Int J Syst Evol Microbiol 66(9):3393–3399. https://doi.org/10.1099/ijsem.0.001204
Lavilla L, Benomar N, Del C CM, Gálvez A, Abriouel H (2014) Antibiotic multiresistance analysis of mesophilic and psychrotrophic Pseudomonas spp. isolated from goat and lamb slaughterhouse surfaces throughout the meat production process. Appl Environ Microbiol 80:6792–6806. https://doi.org/10.1128/AEM.01998-14
Al-Ahmad A, Ameen H, Pelz K et al (2014) Antibiotic recistance and capacity for biofilm formation of different bacteria isolated from endodontic infection associated with root-filled teeth. J Endod 40:223–230. https://doi.org/10.1016/j.joen.2013.07.023
Fernández M, Porcel M, de la Torre J, Molina-Henares MA, Daddaoua A, Llamas MA, Roca A, Carriel V, Garzón I, Ramos JL, Alaminos M, Duque E (2015) Analysis of the pathogenic potential of nosocomial Pseudomonas putida strains. Front Microbiol 6:1–11. https://doi.org/10.3389/fmicb.2015.00871
Vidana R, Sullivan Å, Billstro H, Ahlquist M, Lund B (2010) Enterococcus faecalis infection in root canals – host-derived or exogenous source ? Lett Appl Microbiol 52:109–115. https://doi.org/10.1111/j.1472-765X.2010.02972.x
Rôҫas IN, Siqueira JF Jr (2013) Detection of antibiotic resistance genes in samples from acute and chronic endodontic infections and after treatment. Arch Oral Biol 58:1123–1128. https://doi.org/10.1016/j.archoralbio.2013.03.010
Ren G, Hu D, Cheng EW, Vargas-Reus MA, Reip P, Allaker RP (2009) Characterization of copper oxide nanoparticles for antimicrobial applications. Int J Antimicrob Agents 33:587–590. https://doi.org/10.1016/j.ijantimicag.2008.12.004
Pelgrift RY, Friedman AJ (2013) Nanotechnology as a therapeutic tool to combat microbial resistance. Adv Drug Deliv Rev 65:1803–1815. https://doi.org/10.1016/j.addr.2013.07.011
Vergara-Llanos D, Koning T, Pavicic MF, Bello-Toledo H, Díaz-Gómez A, Jaramillo A, Melendrez-Castro M, Ehrenfeld P, Sánchez-Sanhueza G (2021) Antibacterial and cytotoxic evaluation of copper and zinc oxide nanoparticles as a potential disinfectant material of connections in implant provisional abutments: An in-vitro study. Arch Oral Biol 122:105031. https://doi.org/10.1016/j.archoralbio.2020.105031
Hashemipour H, Zadeh ME, Pourakbari R, Rahimi P (2011) Investigation on synthesis and size control of copper nanoparticle via chemical reduction method. Int J Phys Sci 6:4331–4336. https://doi.org/10.5897/IJPS10.204
Rodríguez Y, Castro R, Arenas F, López-Cabaña Z, Carreño G, Carrasco-Sánchez V et al (2019) Preparation of hydrogel/silver nanohybrids mediated by tunable-size silver nanoparticles for potential antibacterial applications. Polymers (Basel) 11(4):716. https://doi.org/10.3390/polym11040716
Liu R, Liu HH, Ji Z, Chang CH, Xia T, Nel AE et al (2015) Evaluation of toxicity ranking for metal oxide nanoparticles via an in vitro dosimetry model. ACS Nano 22;9(9):9303–9313. https://doi.org/10.1021/acsnano.5b04420
Funding
The work was supported by the Agencia Nacional de Investigación Y Tecnología ANID, Chile. Award Number: 21130022.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
was obtained from all individual participants included in the study.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sacoto-Figueroa, F.K., Bello-Toledo, H.M., González-Rocha, G.E. et al. Molecular characterization and antibacterial activity of oral antibiotics and copper nanoparticles against endodontic pathogens commonly related to health care-associated infections. Clin Oral Invest 25, 6729–6741 (2021). https://doi.org/10.1007/s00784-021-03959-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-021-03959-9