Abstract
Objective
Fixed orthodontic appliances impair oral hygiene increasing the risk of non-cavitated lesions (NCLs) and tooth decay. The aim of this study was to compare the outcomes of fluoride and xylitol varnishes in preventing NCLs during comprehensive orthodontic treatment.
Materials and methods
The sample comprised 55 volunteers from 15 to 20 years of age under orthodontic treatment that were randomly divided into three groups: Fluoride Group (FG; n=17), Xylitol Group (XG; n=19), and Placebo Group (PG; n=19). The patients in each group received two applications of the following varnishes: DuraphatTM (5% NaF), 20% xylitol, and placebo (no F/Xylitol) in the three groups, respectively. The varnishes were applied in the first appointment (T0) and 3 months later (T1). Clinical examinations were carried out at T0 and 6 months after (T2) using the ICDAS index and the QLF system (fluorescence difference). The intergroup comparisons were performed by ANOVA/Tukey’s or Kruskal-Wallis/Dunn’s tests (P<0.05).
Results
There was no significant intergroup difference regarding ICDAS index changes from T0 to T2. Fluoride varnish produced significantly greater increase in fluorescence of NCLs (mean change of −0.65 +0.78 and −0.56 +0.83, for maxilla and mandible, respectively) in comparison to the other groups. The majority of non-cavitated lesions improved in the fluoride and xylitol varnish groups.
Conclusions
Fluoride varnish produced significantly greater increase in enamel fluorescence compared to xylitol and placebo varnishes. In short term, both fluoride and xylitol varnishes produced remineralization of NCLs in orthodontic patients.
Clinical relevance
Non-cavitated lesions can be effectively controlled in high-risk orthodontic patients by means of fluoride varnishes.
Clinical trial registration
ReBEC Identifier: RBR-6mdxfq; Date of Register: March 19th, 2020. Retrospectively Registered
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The Global Burden of Disease Study, in 2016, estimated that half of the world’s population have already been affected by an oral disease, and dental caries in permanent teeth was the most prevalent problem [1]. Non-cavitated lesions (NCLs) are associated with a subsuperficial enamel demineralization and represent the first visible stage of dental caries [2, 3]. Factors as oral hygiene routine, dietary habits, fluoride daily exposure, and levels of cariogenic bacteria can have direct effect in caries formation [4]. Recently, Aura-Tormos et al. reported that “Demineralization: prevention and materials” was the 6th most searched topic in Orthodontics [5].
The incidence and prevalence of NCLs in orthodontic patients range from 26 to 97% depending on the diagnostic method [6, 7]. Orthodontic appliances immediately increase biofilm formation and Streptococcus mutans and lactobacilli levels, which has a direct effect on caries formation [8,9,10]. The risk factors for NCLs formation rapidly increase after appliances installation, having a clinical evolution up to 6 times faster than in patients who do not use braces [6, 11,12,13,14,15]. Additionally, fixed appliances make oral hygiene more difficult [6, 8,9,10,11,12,13,14, 16,17,18]. Previous studies in orthodontic patients showed that preventive strategies can lead to a significant NCLs decrease of 50% in 6 months [19].
The association of different methods, such as water fluoridation, incorporation of fluoride in toothpastes, application of sealants, topical application of varnishes, and oral hygiene guidance with personal responsibility of the patients or their legal guardians, is the key for dental caries prevention [20,21,22]. An important part of dental practice is to implement strategies according to the patient’s individual risk of developing dental caries. The most well-known strategies are constant hygiene orientation and supervision, mouthwash and special toothpaste prescription, and topical application of dental varnish [23].
Fluoride is a gold standard in carious lesion prevention [23,24,25,26]. Ten Cate and Buzalaf reported that fluoride in water, toothpastes, and other products are effective [27]. The use of fluoride in the composition of a varnish represent a noncompliance option [20, 28,29,30,31]. The American Dental Association (ADA) centre for evidence-based dentistry (2019) recommends the use of 5% sodium fluoride (NaF) varnish applied every 3 to 6 months for treatment of non-cavitated carious lesions. This protocol was not individualized for orthodontic treatment.
Previous studies evaluated xylitol varnish effectiveness as prevention agent [30, 32, 33]. Varnish with 20% xylitol showed relative decrease in S. mutans and S. sobrinus in the oral biofilm of children when compared to placebo varnish [34]. Recent in vitro and in situ studies revealed that xylitol varnishes were effective in reducing demineralization and accelerating the remineralization of dental enamel [35,36,37].
Even though promising, xylitol varnish has not been studied neither in vivo nor in orthodontic patients. The aim of this clinical study was to compare xylitol and fluoride varnishes in the prevention/remineralization of NCLs in orthodontic patients. The null hypothesis is that there is no difference in the effectiveness of the two types of varnishes.
Methods
This study was approved by the Ethics in Research Committee of Bauru Dental School, University of São Paulo, Brazil (protocol CAAE – 71639316.0.0000.5417). Written informed consent form was obtained from all volunteers/legal guardians.
This double-blinded randomized clinical trial (RCT) with three-parallel arms was registered in the Clinical Trials Registry (ReBEC) under the identifier #RBR-6mdxfq and followed the Consolidated Standards of Reporting Trials (CONSORT) [38].
The study was conducted from August 2017 to June 2018, and the recruitment occurred at the clinic of Orthodontics at Bauru Dental School, University of São Paulo, Brazil. The inclusion criteria were patients undergoing comprehensive orthodontic, in the level and alignment phase, with pre-adjusted metal brackets (Morelli, Sorocaba, Brazil) treatment 1 to 6 months before study commencement, with 15 to 20 years of age, from both sexes, and with complete permanent dentition. The exclusion criteria were patients with cavitated dental caries, developmental enamel alterations (enamel hypoplasia and fluorosis), and use of antibiotics during the follow-up period.
Outcomes (primary and secondary)
The primary outcomes of this study were the changes in the ICDAS scores in enamel fluorescence (ΔF, in %) assessed with the QLF system. The second outcome is prevalence of new NCLs during the treatment and the percentage of regression in NCLs already stablished.
Sample size calculation
The sample size calculation was performed considering a statistical power of 80%, an α error of 5%, a standard deviation of 0.11 [39], and a minimum difference to be detected in the ICDAS index of 0.5.
Groups and procedures
A randomization was performed by sequenced allocation into 3 groups: Fluoride Group (FG; gold standard, 5% NaF, pH 5.0, Duraphat®, Colgate Palmolive), Xylitol Group (XG; 20% Xylitol, pH 5.0, FGM®), and Placebo Group (PG; synthetic resin base, pH5.0, FGM®). Patients were randomly ordered and sequentially assigned to one intervention group, and the allocation was performed following the order: FG, XG, and PG. The randomization process ensured patients allocation in one of the three groups in a 1:1:1 ratio.
Dental prophylaxis procedure was performed using Robinson brush and Herjos-F toothpaste (412.3ppm of fluoride, Vigodent S/A Rio de Janeiro, Brazil) in all patients at baseline. All patients were submitted to two varnish applications at baseline (T0) and after 3 months (T1). Prior to topical application of the products, the dental surface was air-dried and prepared with relative isolation. A thin layer of the varnish was applied to the dental surface around each bracket with a microbrush. Patients were oriented to avoid drinking or eating up to 2 h after the procedure. All patients at T0 received a toothbrush, fluoridated toothpaste (COLGATE®, 1,500 ppm of fluoride, Colgate-Palmolive, São Paulo, Brazil), and guidance on oral hygiene. Patients were blinded regarding the type of varnish.
Caries and fluorescence analysis
The variables were assessed at baseline (T0) and 6 months after the first varnish application (T2), as shown in Fig. 1.
Clinical assessment of the buccal surfaces was performed by one trained examiner using the International Caries Detection and Assessment System (ICDAS) [40]. After professional prophylaxis and adequate conditions, the dental surfaces were classified with scores from 0 to 5, in which 0, no visual evidence of NCLs; 1, initial stage of NCLs; 2, distinct visual change in enamel; 3, localized enamel breakdown due to caries without dentine exposure; 4, underlying dark shadow from dentine; and 5, distinct cavity with exposed dentine. Only maxillary and mandibular canines of the skilful side of the patient were used [41].
Quantitative Light-Induced Fluorescence (QLF) images of the buccal surfaces of all premolars and canines of the skilful side of the patient were obtained at T0 and T2 using the Inspektor Pro QLF camera system (Inspektor BV, Amsterdam, The Netherlands). QLF images of T0 and T2 were stored, and each image was independently and blindly analysed by a single examiner using the QLF software (Inspektor Pro 2.0.0.39, Inspektor Research System BV, Amsterdam, The Netherlands). The images in T0 and T2 were adjusted in the same position before calculating the surface fluorescence (ΔF, in %, Fig. 2) and caries lesion volume (ΔQ, in % mm2).
ICDAS and QLF assessments examiner was unaware of the patient’s group.
Error study
The measurements were repeated by the first author using 30% of the QLF images with an interval of at least 1 month. Reproducibility of the ICDAS scores was evaluated using Kappa index after re-evaluation of 30% of the sample after 30 days. The intra-rater reliability regarding surface fluorescence was assessed using intraclass correlation coefficient (ICC).
Statistical analysis
Data normality and homogeneity were respectively assessed by Kolmogorov-Smirnov and Bartlett’s tests. Intergroup comparability regarding initial age and sex distribution were evaluated with ANOVA and Chi-square tests, respectively (Table 1). Baseline intergroup comparison was analysed using ANOVA and Kruskal-Wallis tests. Intergroup differences for changes in caries index and enamel fluorescence were evaluated using ANOVA/Tukey’s or Kruskal-Wallis/Dunn’s tests for variables with normal or non-normal distributions, respectively. The statistical analyses were performed using Statistica software (Statistica for Windows version 11.0; StatSoft, Tulsa, Okla) with a significance level of 5%.
Results
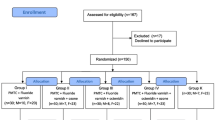
During the study period, 70 patients were examined. Sixty volunteers were enrolled according to the eligibility criteria and randomized in a 1:1:1 ratio to the three study groups (FG= 20, XG=20, and PG=20). Five patients were lost during follow-up, 3 in the FG (15%), 1 in the XG (5%), and 1 in the PG (5%). The excluded patients had their orthodontic fixed appliances removed before T2 analyses or did not attend the appointments. Fifty-five patients were properly analysed. Therefore, since the ICDAS analysed only the canines of the skilful side of the patients, 55 teeth were analysed. Because the QLF analysed canines and premolars of the skilful side, 110 teeth were analysed. Figure 3 shows the participants flow chart. No difference was found in the baseline comparisons for all variables, except for the F mandible, that presented a difference between GF and GP (Table 2).
The intra-examiner Kappa index for the ICDAS scores was strong (≥ 0.9). The intra-examiner reliability for ΔF was strong with the ICC ranging from 0.997 to 0.999.
The study groups were similar regarding age and sex distribution at baseline (Table 1).
No significant intergroup differences were observed in the ICDAS index and ΔQ (lesion volume) changes (Table 3). The fluorescence assessment indicated an improvement in the dental surface mineralization in all study groups. The fluoride varnish (FG) showed a greater increase of enamel mineralization than xylitol and placebo varnish, respectively, for the maxillary and mandibular teeth.
Only 19% of the 110 analysed teeth had non-cavitated lesions. The FG had 9 teeth with NCLs, the XG had 7, and the PG had 5. In the FG group, 6 (67%) of the teeth with NCLs regressed, but another tooth showed a NCLs at the end. In the XG, 7 (100%) of the teeth with NCLs regressed, but another tooth showed a NCLs at the end. In the PG, none of the lesions were regressed (Table 4).
Discussion
This is the first clinical study comparing xylitol and fluoride varnishes in orthodontic patients. The Kappa index for ICDAS was adequate, and the surface fluorescence variables presented excellent intra-examiner agreement. Previous studies also demonstrated adequate reproducibility for the ICDAS with Kappa index varying from 0.59 to 0.82 [33, 36, 40, 42,43,44]. The QLF system consists of an image analyses which can calculate the percentage of fluorescence loss of the selected enamel area based on the amount of mineral loss during the analysed period. Benson et al. (2003) also showed a strong reproducibility of the method and validated the QLF system [45, 46].
Among the different available exams for caries detection, both methods used in this study were proven to have similar performance compared to histological gold standard scores for caries detection [47, 48]. The QLF system was chosen due to its sensitivity and efficiency [6, 49, 50]. This exam is capable of recording a minor area of demineralization during orthodontic treatment with a 5% fluorescence loss detection, value that is not possible to be detected in a visual and clinical examination [6]. The clinical exam, ICDAS, was developed to analyse changes in the enamel surface related to the potential histological status of the lesion [43]. This visual exam depends on a previous examiner calibration, and it is popularly used due its excellent sensitivity, accessibility, and practical use. ICDAS index showed good accuracy, especially in lesions located in the superficial layers of the enamel [51]. Both technique limitations are that they can be affected by inadequate prophylaxis, illumination, and dryness of the examined surface, as well as resin excess and inflammatory and bleeding status of the gingiva.
Orthodontic patients have a high risk of caries formation, and its incidence is higher in canines and premolars, having a clinical evolution 6 times faster than in non-orthodontic patients [40, 41]. Safety, efficacy, simple application, frequency, and patient acceptance are all factors that can affect the election of the preventive strategy. Individual compliance ensuring adequate oral hygiene is still a challenge for orthodontic patients, which lead clinical orthodontists to use associated methods, as the topical application of varnishes.
In the present study, we enrolled 55 15–20-year-old volunteers under orthodontic treatment that were randomly assigned into 3 different groups, according to the varnishes that were applied on their teeth. No difference was found in the baseline comparisons for the variables evaluated, except for the F mandible. In this case, GF presented a higher value than GP, which denotes a higher degree of demineralization.
There were no significant differences on the enamel surface changes from T0 to T2 using the ICDAS index among the three groups (Table 3). This result corroborates with a previous study [52]. Both study and control groups presented low frequency of non-cavitated lesions in T0 and T2, probably due to the presence of fluoride in the toothpaste, water distribution, and constant hygiene stimulation during the orthodontic appointments [42].
On the other hand, fluorescence assessment (QLF) of the enamel indicated that 6 months was enough to obtain improvement of the dental surface mineralization (Table 3). Gokce et al. showed in an in vitro study that only 2 weeks was enough to observe statistical differences in the QLF analyses [53]. Fluoride varnish (FG) showed greater increases of enamel mineralization compared to xylitol and placebo varnishes, in the maxillary and mandibular teeth, respectively. The fluorescence difference between FG and PG in the mandible might be explained by the presence of fluoride in the FG group. This is not surprising, since the pooled D(M)FS prevented fraction estimate comparing fluoride varnish with placebo is estimated to be 43% [32]. It is important to highlight that the FG presented a significantly higher degree of fluorescence (F) loss at baseline as compared with PG, which means that the degree of remineralization was higher than the value expressed by the ΔF.
At T2, the FG group had lesion regression in 67% of the teeth that initially presented NCLs, the XG had lesion regression in 100%, and the PG had no teeth with regression. Considering the regression of the lesions in each group, fluoride and xylitol varnishes were both able to mineralize non-cavitated lesions. Consequently, xylitol varnishes seem to be an alternative to fluoride varnishes in NCLs prevention and remineralization during orthodontic treatment. However, future clinical studies with a longer observation period should be performed. A limitation of the present study was the short evaluation period of 6 months. Future studies should compare fluoride and xylitol varnishes for longer periods of at least 1-year period.
Conclusions
-
Fluoride varnish produced significantly greater increase in enamel fluorescence compared to xylitol and placebo varnishes;
-
In the short term, both fluoride and xylitol varnishes produced remineralization of non-cavitated lesions in orthodontic patients.
References
Vos T, Allen C, Arora M, Barber RM, Bhutta ZA, Brown A, Carter A, Casey DC, Charlson FJ, Chen AZ, Coggeshall M, Cornaby L, Dandona L, Dicker DJ, Dilegge T, Erskine HE, Ferrari AJ, Fitzmaurice C, Fleming T, Forouzanfar MH, Fullman N, Gething PW, Goldberg EM, Graetz N, Haagsma JA, Hay SI, Johnson CO, Kassebaum NJ, Kawashima T, Kemmer L, Khalil IA, Kinfu Y, Kyu HH, Leung J, Liang X, Lim SS, Lopez AD, Lozano R, Marczak L, Mensah GA, Mokdad AH, Naghavi M, Nguyen G, Nsoesie E, Olsen H, Pigott DM, Pinho C, Rankin Z, Reinig N, Salomon JA, Sandar L, Smith A, Stanaway J, Steiner C, Teeple S, Thomas BA, Troeger C, Wagner JA, Wang H, Wanga V, Whiteford HA, Zoeckler L, Abajobir AA, Abate KH, Abbafati C, Abbas KM, Abd-Allah F, Abraham B, Abubakar I, Abu-Raddad LJ, Abu-Rmeileh NME, Ackerman IN, Adebiyi AO, Ademi Z, Adou AK, Afanvi KA, Agardh EE, Agarwal A, Kiadaliri AA, Ahmadieh H, Ajala ON, Akinyemi RO, Akseer N, al-Aly Z, Alam K, Alam NKM, Aldhahri SF, Alegretti MA, Alemu ZA, Alexander LT, Alhabib S, Ali R, Alkerwi A', Alla F, Allebeck P, al-Raddadi R, Alsharif U, Altirkawi KA, Alvis-Guzman N, Amare AT, Amberbir A, Amini H, Ammar W, Amrock SM, Andersen HH, Anderson GM, Anderson BO, Antonio CAT, Aregay AF, Ärnlöv J, Artaman A, Asayesh H, Assadi R, Atique S, Avokpaho EFGA, Awasthi A, Quintanilla BPA, Azzopardi P, Bacha U, Badawi A, Balakrishnan K, Banerjee A, Barac A, Barker-Collo SL, Bärnighausen T, Barregard L, Barrero LH, Basu A, Bazargan-Hejazi S, Beghi E, Bell B, Bell ML, Bennett DA, Bensenor IM, Benzian H, Berhane A, Bernabé E, Betsu BD, Beyene AS, Bhala N, Bhatt S, Biadgilign S, Bienhoff K, Bikbov B, Biryukov S, Bisanzio D, Bjertness E, Blore J, Borschmann R, Boufous S, Brainin M, Brazinova A, Breitborde NJK, Brown J, Buchbinder R, Buckle GC, Butt ZA, Calabria B, Campos-Nonato IR, Campuzano JC, Carabin H, Cárdenas R, Carpenter DO, Carrero JJ, Castañeda-Orjuela CA, Rivas JC, Catalá-López F, Chang JC, Chiang PPC, Chibueze CE, Chisumpa VH, Choi JYJ, Chowdhury R, Christensen H, Christopher DJ, Ciobanu LG, Cirillo M, Coates MM, Colquhoun SM, Cooper C, Cortinovis M, Crump JA, Damtew SA, Dandona R, Daoud F, Dargan PI, das Neves J, Davey G, Davis AC, Leo DD, Degenhardt L, Gobbo LCD, Dellavalle RP, Deribe K, Deribew A, Derrett S, Jarlais DCD, Dharmaratne SD, Dhillon PK, Diaz-Torné C, Ding EL, Driscoll TR, Duan L, Dubey M, Duncan BB, Ebrahimi H, Ellenbogen RG, Elyazar I, Endres M, Endries AY, Ermakov SP, Eshrati B, Estep K, Farid TA, Farinha CSS, Faro A, Farvid MS, Farzadfar F, Feigin VL, Felson DT, Fereshtehnejad SM, Fernandes JG, Fernandes JC, Fischer F, Fitchett JRA, Foreman K, Fowkes FGR, Fox J, Franklin RC, Friedman J, Frostad J, Fürst T, Futran ND, Gabbe B, Ganguly P, Gankpé FG, Gebre T, Gebrehiwot TT, Gebremedhin AT, Geleijnse JM, Gessner BD, Gibney KB, Ginawi IAM, Giref AZ, Giroud M, Gishu MD, Giussani G, Glaser E, Godwin WW, Gomez-Dantes H, Gona P, Goodridge A, Gopalani SV, Gotay CC, Goto A, Gouda HN, Grainger R, Greaves F, Guillemin F, Guo Y, Gupta R, Gupta R, Gupta V, Gutiérrez RA, Haile D, Hailu AD, Hailu GB, Halasa YA, Hamadeh RR, Hamidi S, Hammami M, Hancock J, Handal AJ, Hankey GJ, Hao Y, Harb HL, Harikrishnan S, Haro JM, Havmoeller R, Hay RJ, Heredia-Pi IB, Heydarpour P, Hoek HW, Horino M, Horita N, Hosgood HD, Hoy DG, Htet AS, Huang H, Huang JJ, Huynh C, Iannarone M, Iburg KM, Innos K, Inoue M, Iyer VJ, Jacobsen KH, Jahanmehr N, Jakovljevic MB, Javanbakht M, Jayaraman SP, Jayatilleke AU, Jee SH, Jeemon P, Jensen PN, Jiang Y, Jibat T, Jimenez-Corona A, Jin Y, Jonas JB, Kabir Z, Kalkonde Y, Kamal R, Kan H, Karch A, Karema CK, Karimkhani C, Kasaeian A, Kaul A, Kawakami N, Keiyoro PN, Kemp AH, Keren A, Kesavachandran CN, Khader YS, Khan AR, Khan EA, Khang YH, Khera S, Khoja TAM, Khubchandani J, Kieling C, Kim P, Kim CI, Kim D, Kim YJ, Kissoon N, Knibbs LD, Knudsen AK, Kokubo Y, Kolte D, Kopec JA, Kosen S, Kotsakis GA, Koul PA, Koyanagi A, Kravchenko M, Defo BK, Bicer BK, Kudom AA, Kuipers EJ, Kumar GA, Kutz M, Kwan GF, Lal A, Lalloo R, Lallukka T, Lam H, Lam JO, Langan SM, Larsson A, Lavados PM, Leasher JL, Leigh J, Leung R, Levi M, Li Y, Li Y, Liang J, Liu S, Liu Y, Lloyd BK, Lo WD, Logroscino G, Looker KJ, Lotufo PA, Lunevicius R, Lyons RA, Mackay MT, Magdy M, Razek AE, Mahdavi M, Majdan M, Majeed A, Malekzadeh R, Marcenes W, Margolis DJ, Martinez-Raga J, Masiye F, Massano J, McGarvey ST, McGrath JJ, McKee M, McMahon BJ, Meaney PA, Mehari A, Mejia-Rodriguez F, Mekonnen AB, Melaku YA, Memiah P, Memish ZA, Mendoza W, Meretoja A, Meretoja TJ, Mhimbira FA, Millear A, Miller TR, Mills EJ, Mirarefin M, Mitchell PB, Mock CN, Mohammadi A, Mohammed S, Monasta L, Hernandez JCM, Montico M, Mooney MD, Moradi-Lakeh M, Morawska L, Mueller UO, Mullany E, Mumford JE, Murdoch ME, Nachega JB, Nagel G, Naheed A, Naldi L, Nangia V, Newton JN, Ng M, Ngalesoni FN, Nguyen QL, Nisar MI, Pete PMN, Nolla JM, Norheim OF, Norman RE, Norrving B, Nunes BP, Ogbo FA, Oh IH, Ohkubo T, Olivares PR, Olusanya BO, Olusanya JO, Ortiz A, Osman M, Ota E, PA M, Park EK, Parsaeian M, de Azeredo Passos VM, Caicedo AJP, Patten SB, Patton GC, Pereira DM, Perez-Padilla R, Perico N, Pesudovs K, Petzold M, Phillips MR, Piel FB, Pillay JD, Pishgar F, Plass D, Platts-Mills JA, Polinder S, Pond CD, Popova S, Poulton RG, Pourmalek F, Prabhakaran D, Prasad NM, Qorbani M, Rabiee RHS, Radfar A, Rafay A, Rahimi K, Rahimi-Movaghar V, Rahman M, Rahman MHU, Rahman SU, Rai RK, Rajsic S, Ram U, Rao P, Refaat AH, Reitsma MB, Remuzzi G, Resnikoff S, Reynolds A, Ribeiro AL, Blancas MJR, Roba HS, Rojas-Rueda D, Ronfani L, Roshandel G, Roth GA, Rothenbacher D, Roy A, Sagar R, Sahathevan R, Sanabria JR, Sanchez-Niño MD, Santos IS, Santos JV, Sarmiento-Suarez R, Sartorius B, Satpathy M, Savic M, Sawhney M, Schaub MP, Schmidt MI, Schneider IJC, Schöttker B, Schwebel DC, Scott JG, Seedat S, Sepanlou SG, Servan-Mori EE, Shackelford KA, Shaheen A, Shaikh MA, Sharma R, Sharma U, Shen J, Shepard DS, Sheth KN, Shibuya K, Shin MJ, Shiri R, Shiue I, Shrime MG, Sigfusdottir ID, Silva DAS, Silveira DGA, Singh A, Singh JA, Singh OP, Singh PK, Sivonda A, Skirbekk V, Skogen JC, Sligar A, Sliwa K, Soljak M, Søreide K, Sorensen RJD, Soriano JB, Sposato LA, Sreeramareddy CT, Stathopoulou V, Steel N, Stein DJ, Steiner TJ, Steinke S, Stovner L, Stroumpoulis K, Sunguya BF, Sur P, Swaminathan S, Sykes BL, Szoeke CEI, Tabarés-Seisdedos R, Takala JS, Tandon N, Tanne D, Tavakkoli M, Taye B, Taylor HR, Ao BJT, Tedla BA, Terkawi AS, Thomson AJ, Thorne-Lyman AL, Thrift AG, Thurston GD, Tobe-Gai R, Tonelli M, Topor-Madry R, Topouzis F, Tran BX, Truelsen T, Dimbuene ZT, Tsilimbaris M, Tura AK, Tuzcu EM, Tyrovolas S, Ukwaja KN, Undurraga EA, Uneke CJ, Uthman OA, van Gool CH, Varakin YY, Vasankari T, Venketasubramanian N, Verma RK, Violante FS, Vladimirov SK, Vlassov VV, Vollset SE, Wagner GR, Waller SG, Wang L, Watkins DA, Weichenthal S, Weiderpass E, Weintraub RG, Werdecker A, Westerman R, White RA, Williams HC, Wiysonge CS, Wolfe CDA, Won S, Woodbrook R, Wubshet M, Xavier D, Xu G, Yadav AK, Yan LL, Yano Y, Yaseri M, Ye P, Yebyo HG, Yip P, Yonemoto N, Yoon SJ, Younis MZ, Yu C, Zaidi Z, Zaki MES, Zeeb H, Zhou M, Zodpey S, Zuhlke LJ, Murray CJL (2016) Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet 388:1545–1602
Kidd E, Fejerskov O (2004) What constitutes dental caries? Histopathology of carious enamel and dentin related to the action of cariogenic biofilms. J Dent Res 83:35–38
Machiulskiene V, Campus G, Carvalho JC, Dige I, Ekstrand KR, Jablonski-Momeni A, Maltz M, Manton DJ, Martignon S, Martinez-Mier EA, Pitts NB, Schulte AG, Splieth CH, Tenuta LMA, Ferreira Zandona A, Nyvad B (2020) Terminology of dental caries and dental caries management: consensus report of a workshop organized by ORCA and cariology research group of IADR. Caries Res 54:7–14
Leeper DK, Noureldin A, Julien K, Campbell PM, Buschang PH (2019) Risk assessments in orthodontic patients developing white spot lesions. J Investig Clin Dent 10(14):e12470
Aura-Tormos JI, García-Sanz V, Estrela F, Bellot-Arcís C, Paredes-Gallardo V (2019) Current trends in orthodontic journals listed in Journal Citation Reports. A bibliometric study. Am J Orthod Dentofac Orthop 156:663–674 e661
Boersma J, Van der Veen M, Lagerweij M, Bokhout B, Prahl-Andersen B (2005) Caries prevalence measured with QLF after treatment with fixed orthodontic appliances: influencing factors. Caries Res 39:41–47
Buschang PH, Chastain D, Keylor CL, Crosby D, Julien KC (2019) Incidence of white spot lesions among patients treated with clear aligners and traditional braces. Angle Orthod 89:359–364
Gwinnett AJ, Ceen RF (1979) Plaque distribution on bonded brackets: a scanning microscope study. Am J Orthod Dentofac Orthop 75:667–677
Lima KCC, Paschoal MAB, de Araújo GJ, Freitas KMS, Pinzan-Vercelino CRM (2019) Comparative analysis of microorganism adhesion on coated, partially coated, and uncoated orthodontic archwires: a prospective clinical study. Am J Orthod Dentofac Orthop 156:611–616
Reichardt E, Geraci J, Sachse S, Rödel J, Pfister W, Löffler B, Wagner Y, Eigenthaler M, Wolf M (2019) Qualitative and quantitative changes in the oral bacterial flora occur shortly after implementation of fixed orthodontic appliances. Am J Orthod Dentofac Orthop 156:735–744
Mizrahi E (1982) Enamel demineralization following orthodontic treatment. Am J Orthod Dentofac Orthop 82:62–67
Gorelick L, Geiger AM, Gwinnett AJ (1982) Incidence of white spot formation after bonding and banding. Am J Orthod Dentofac Orthop 81:93–98
Øgaard B, Rølla G, Arends J, Ten Cate J (1988) Orthodontic appliances and enamel demineralization Part 2. Prevention and treatment of lesions. Am J Orthod Dentofac Orthop 94:123–128
Mitchell L (1992) Decalcification during orthodontic treatment with fixed appliances—an overview. Br J Orthod 19:199–205
Keyes PH (1969) Present and future measures for dental caries control. J Am Dent Assoc 79:1395–1404
Øgaard B (1989) Prevalence of white spot lesions in 19-near-olds: a study on untreated and orthodontically treated persons 5 years after treatment. Am J Orthod Dentofac Orthop 96:423–427
Scheie AA, Arneberg P, Krogstad O (1984) Effect of orthodontic treatment on prevalence of Streptococcus mutans in plaque and saliva. Eur J Oral Sci 92:211–217
Chatterjee R, Kleinberg I (1979) Effect of orthodontic band placement on the chemical composition of human incisor tooth plaque. Arch Oral Biol 24:97–100
Demito CF, Rodrigues GV, Ramos AL, Bowman SJ (2011) Efficacy of a fluoride varnish in preventing white-spot lesions as measured with laser fluorescence. J Clin Orthod 45:25–29
Brasil. Portaria do Ministério da Saúde n. 635/BSB de 26 de dezembro de 1975. Estabelece normas e padrões sobre a fluoretação das águas dos sistemas públicos de abastecimento destinadas ao consumo humano. Diário Oficial da União. Brazil; 1975
Burt BA, Marthaler TM (1996) Fluoride tablets, salt fluoridation, and milk fluoridation. Fluor Dent:291–310
Reeves TG (1995) Engineering and administrative recommendations for water fluoridation, 1995. Ctr Dis Control Prev 44:1–40
Lapenaite E, Lopatiene K, Ragauskaite A (2016) Prevention and treatment of white spot lesions during and after fixed orthodontic treatment: a systematic. Stomatologija 18:3–8
Beerens MW, Boekitwetan F, Van Der Veen MH, Ten Cate JM (2015) White spot lesions after orthodontic treatment assessed by clinical photographs and by quantitative light-induced fluorescence imaging; a retrospective study. Acta Odontol Scand 73:441–446
Al Mulla AH, Al Kharsa S, Birkhed D (2010) Modified fluoride toothpaste technique reduces caries in orthodontic patients: a longitudinal, randomized clinical trial. Am J Orthod Dentofac Orthop 138:285–291
Farhadian N, Miresmaeili A, Eslami B, Mehrabi S (2008) Effect of fluoride varnish on enamel demineralization around brackets: an in-vivo study. Am J Orthod Dentofac Orthop 133:S95–S98
Ten Cate J, Buzalaf MAR (2019) Fluoride mode of action: once there was an observant dentist. J Dent Res 98:725–730
Saldaña I, Ernesto J (1988) Avaliação comparativa do controle da placa bacteriana e da gengivite em pacientes sob tratamento ortodôntico, sem orientação, e com métodos de higiene supervisionados e de controle profissional. Ortodontia 22:29–39
Marinho VC, Higgins J, Logan S, Sheiham A (2003) Fluoride toothpastes for preventing dental caries in children and adolescents. Cochrane Database Syst Rev
Lopatiene K, Borisovaite M, Lapenaite E (2016) Prevention and treatment of white spot lesions during and after treatment with fixed orthodontic appliances: a systematic literature review. J Oral Maxillofac Res 7:e1
Newbrun E (1983) Cariology (2nd Edition). The Williams and Wilkins, Baltimore
Marinho VC, Worthington HV, Walsh T, Clarkson JE (2013) Fluoride varnishes for preventing dental caries in children and adolescents. Cochrane Database Syst Rev
Pereira AFF, Silva TC, Silva TL, Caldana ML, Bastos JRM, Buzalaf MAR (2012) Xylitol concentrations in artificial saliva after application of different xylitol dental varnishes. J Appl Oral Sci 20:146–150
Bhatti M, MacRobert A, Meghji S, Henderson B, Wilson M (1997) Effect of dosimetric and physiological factors on the lethal photosensitization of Porphyromonas gingivalis in vitro. Photochem Photobiol 65:1026–1031
Takahashi N, Washio J (2011) Metabolomic effects of xylitol and fluoride on plaque biofilm in vivo. J Dent Res 90:1463–1468
Cardoso C, Cassiano L, Costa E, Souza-e-Silva C, Magalhães A, Grizzo L et al (2016) Effect of xylitol varnishes on remineralization of artificial enamel caries lesions in situ. J Dent 50:74–78
Cardoso C, de Castilho ARF, Salomão PMA, Costa E, Magalhaes A, Buzalaf M (2014) Effect of xylitol varnishes on remineralization of artificial enamel caries lesions in vitro. J Dent 42:1495–1501
Schulz KF, Altman DG, Moher D (2010) CONSORT 2010 statement: updated guidelines for reporting parallel group randomized trials. Ann Intern Med 152:726–732
Miller CC, Burnside G, Higham SM, Flannigan NL (2016) Quantitative light-induced fluorescence-digital as an oral hygiene evaluation tool to assess plaque accumulation and enamel demineralization in orthodontics. Angle Orthod 86:991–997
Pitts N, Ekstrand K, Foundation I (2013) International Caries Detection and Assessment System (ICDAS) and its International Caries Classification and Management System (ICCMS)–methods for staging of the caries process and enabling dentists to manage caries. Community Dent Oral Epidemiol 41:e41–e52
Inada E, Saitoh I, Yu Y, Tomiyama D, Murakami D, Takemoto Y, Morizono K, Iwasaki T, Iwase Y, Yamasaki Y (2015) Quantitative evaluation of toothbrush and arm-joint motion during tooth brushing. Clin Oral Investig 19:1451–1462
Ramires I, Buzalaf MAR (2007) A fluoretação da água de abastecimento público e seus benefícios no controle da cárie dentária: cinqüenta anos no Brasil. Cien Saude Colet 12:1057–1065
Ismail AI, Sohn W, Tellez M, Amaya A, Sen A, Hasson H, Pitts NB (2007) The International Caries Detection and Assessment System (ICDAS): an integrated system for measuring dental caries. Community Dent Oral Epidemiol 35:170–178
Gomez J, Pretty I, Santarpia Iii R, Cantore B, Rege A, Petrou I et al (2014) Quantitative light-induced fluorescence to measure enamel remineralization in vitro. J Caries Res 48:223–227
Benson PE, Pender N, Higham SM (2003) Quantifying enamel demineralization from teeth with orthodontic brackets—a comparison of two methods. Part 1: repeatability and agreement. Eur J Orthod 25:149–158
Benson PE, Pender N, Higham SM (2003) Quantifying enamel demineralization from teeth with orthodontic brackets—a comparison of two methods. Part 2: validity. Eur J Orthod 25:159–165
Gomez J, Zakian C, Salsone S, Pinto S, Taylor A, Pretty I et al (2013) In vitro performance of different methods in detecting occlusal caries lesions. J Dent 41:180–186
Carvalho RNd, Letieri AdS, Vieira TI, Santos TMPd, Lopes RT, Neves AdA et al. (2018) Accuracy of visual and image-based ICDAS criteria compared with a micro-CT gold standard for caries detection on occlusal surfaces. J Braz Oral Res 32
Heymann GC, Grauer D (2013) A contemporary review of white spot lesions in orthodontics. J Esthet Restor Dent 25:85–95
Van Der Veen MH, Attin R, Schwestka-Polly R, Wiechmann D (2010) Caries outcomes after orthodontic treatment with fixed appliances: do lingual brackets make a difference? J Eur J Oral Sci 118:298–303
Diniz MB, Lima LM, Eckert G, Zandona AF, Cordeiro RC, Pinto LS (2011) In vitro evaluation of ICDAS and radiographic examination of occlusal surfaces and their association with treatment decisions. J Oper Dent 36:133–142
Elias F, Pinzan A, Bastos JRM (2006) Influence of fluorine-xylitol complex in the dental plaque and gingival bleeding control in herbiatric patients with fixed orthodontic brace. Dent Press J Orthod 11:42–56
Gokce G, Savas S, Kucukyilmaz E, Veli I (2017) Effects of toothpastes on white spot lesions around orthodontic brackets using quantitative light-induced fluorescence (QLF). J Orofac Orthop 78:480–486
Acknowledgements
The authors would like to thank the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior - Brasil (CAPES) - Finance Code 001.
Funding
Coordenação de Aperfeiçoamento de Pessoal de Nível Superior - Brazil (CAPES) - Finance Code 001. This study was funded by FAPESP (grant number 2016/19761-0).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Vinicius Merino da Silva, Camila Massaro, Guilherme Janson, and Daniela Garib. Varnish selection and ICDAS and QLF analyses were performed by Vinicius Merino da Silva, Camila Massaro, Marilia Afonso Rabelo Buzalaf, and Daniela Garib. The first draft of the manuscript was written by Vinicius Merino da Silva, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Silva, V.M., Massaro, C., Buzalaf, M.A.R. et al. Prevention of non-cavitated lesions with fluoride and xylitol varnishes during orthodontic treatment: a randomized clinical trial. Clin Oral Invest 25, 3421–3430 (2021). https://doi.org/10.1007/s00784-021-03930-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-021-03930-8