Abstract
Objectives
Aberrant growth of the maxillomandibular complex in patients with cleft lip and/or palate (CL/P) can be managed with dentofacial orthopaedics. However, no consensus has been reached regarding timing and evolution of the maturational stages. Therefore, the aim of this study is to determine if patients with CL/P have an increased risk for delayed craniofacial maturation.
Materials and methods
A sample of 246 cleft patients and 210 non-affected individuals was retrospectively compiled. Cephalometric radiographs taken between the ages of 10 and 14 years (girls) and 12 and 16 years (boys) were collected and assessed with the cervical vertebral maturation (CVM) method.
Results
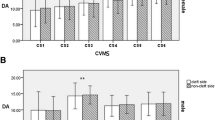
In boys, no significant association between the presence of CL/P and a CVM score of CS3 or higher was observed in any age subsample. This was similar for a CVM score of CS5 or higher. Girls in the CL/P group had a significant lower probability of having a CVM score of at least CS3 in the subsample with age 11 to 12 (p = 0.001) and a borderline non-significant lower probability of having a CVM score of at least CS5 in the subsample with age 12 to 13 (p = 0.055).
Conclusions
The current study demonstrated a discrete delay in skeletal maturation before the pubertal growth spurt of (pre)adolescents with CL/P, especially girls. This delay was less apparent at the end of the pubertal growth spurt.
Clinical relevance
This research suggests that the craniofacial maturational stages relevant for dentofacial orthopaedic treatment in cleft patients, especially girls, occur at higher chronological age. Further research must quantify this delay, investigate its clinical significance, and determine its effect on the timing of dentofacial orthopaedic treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The growth of the maxilla in adolescents with cleft lip and/or palate (CL/P) can be restricted in three dimensions. This can be attributed to the severity of the cleft but also to iatrogenic effects of previous surgeries such as closure of the lip and/or palate. It has been demonstrated that the magnitude of these iatrogenic effects correlates with the experience and case load of the surgeon [1,2,3]. However, basal skeletal characteristics [3], missing lateral incisors as a sign of inherent tissue hypoplasia [3], and altered embryonic development of the pituitary gland resulting in growth hormone deficiency [4, 5] are also considered to be relevant contributing factors.
Abnormal or disturbed growth of the maxillomandibular complex can be approached in two different ways, depending on the maturational status of the patient and the extent of the anomaly. Orthognathic surgery, in combination with pre- and post-orthodontic treatment, allows three-dimensional jaw rehabilitation in a mature patient by one- or two-step procedures. On the other hand, facial growth and development during childhood or early adolescence can be guided by a dentofacial orthopaedic treatment. Transverse, anteroposterior, and to a lesser extent also vertical maxillomandibular discrepancies in CL/P patients can be treated using orthopaedic appliances. This treatment approach primarily includes the use of a (rapid) maxillary expander, face masks, a Fränkel function regulator III (FR-3), and/or bone-anchored maxillary protraction with intermaxillary elastics [6, 7]. The latter is a more recent treatment modality for skeletal class III that has demonstrated satisfying results in CL/P patients [8, 9]. Orthopaedic interventions in the mandible such as functional appliances are less common in cleft patients. However, the mandible in all cleft subtypes has a shorter ramus and body length, and the mandibular position is more retrusive relative to the cranial base than in a non-affected population [10]. In particular cases where the anteroposterior maxillary hypoplasia is less apparent, such as the cleft lip (CL) or cleft palate (CP), a relative skeletal class II relationship can be observed, and therapy with a functional appliance is a valid treatment option [11].
Success in dentofacial orthopaedics is highly dependent on the patient’s maturational stage. Therefore, it is important to determine the period of accelerated growth of the relevant skeletal structure to achieve the most favourable response with the least potential morbidity [12]. In contrast, orthognathic surgery should be delayed until craniofacial maturation is essentially completed [13]. The individual skeletal maturity can be assessed using biological indicators such as increase in body height [14], skeletal maturation of the hand and wrist [15], the third finger middle phalanx maturation (MPM) [16], and the cervical vertebral maturation [12, 17]. The cervical vertebral maturation (CVM) method was introduced by Lamparski and further refined by Baccetti and coworkers [12, 18, 19]. It is a validated method that allows estimation of the skeletal maturation using a cephalometric radiograph. This imaging method is also routinely used for orthodontic purposes, so the radiation dose can be minimized [20, 21].
The aim of this study is to determine if patients with cleft lip and/or palate have an increased risk for delayed skeletal maturation by assessing their cervical vertebral maturation and comparing it with that of a matched, non-affected control group.
Materials and methods
The study was approved by the Ethical Committees of Ghent University Hospital (2019/1064) and University Hospitals Leuven (S63027) and has been performed in accordance with the Declaration of Helsinki.
Sample
The study had a retrospective design and comprised patients with an orofacial cleft treated by the Leuven Cleft Lip and Palate Team and the Centre of Congenital Facial Anomalies of the Ghent University Hospital. The following inclusion criteria were used: uni- or bilateral cleft lip, alveolus, and/or palate, isolated cleft palate, no syndromes, and an age between 10 and 14 (girls) and 12 and 16 (boys). Only subjects with a clearly readable cephalometric radiograph were considered eligible. The age limits were based on the average timing of the peak height velocity, which is at 13.5 years old for boys and 11.5 years old for girls [22]. Syndromic patients were excluded in order to isolate the effect of cleft lip and/or palate on growth. The non-affected control group was compiled at the Department of Orthodontics at the Ghent University Hospital and comprised patients with a clearly readable cephalometric radiograph as part of the diagnostic data prior to an orthodontic treatment. The same age limits as in the study sample were applied for boys and girls in the control group. Only children of European or North African ancestry were considered eligible for inclusion in the cleft or control group. Patients in the study and control group had to be born in the same time span to avoid a historical comparison with bias due to a secular trend of early sexual maturation.
The selected cephalometric radiographs were cropped to an image with only the cervical spine visible. This was performed in order to avoid observer bias such as age estimation based on tooth development or diagnosis of an OFC (Fig. 1). The set of radiographs was randomized and numerically coded to ensure blinding.
Methods
Skeletal maturational status was determined with the cervical vertebral maturation (CVM) method [12]. The CVM method allows classification into six cervical stages (CS1–6) based on a visual appraisal of two morphological characteristics of the cervical vertebrae C2, C3, and C4 (Fig. 2). First, it considers the presence or absence of a concavity at the lower border of the body of C2, C3, and C4. Secondly, the shape of the body of C3 and C4 is assessed. Four basic shapes are considered: trapezoid (the superior border is tapered from posterior to anterior), rectangular horizontal (the heights of the posterior and anterior borders are equal; the superior and inferior borders are longer than the anterior and posterior borders), squared (the posterior, superior, anterior, and inferior borders are equal), and rectangular vertical (the posterior and anterior borders are longer than the superior and inferior borders) [12]. Cervical stages (CS) 1 and 2 are the optimal stages for transverse and anteroposterior orthopaedic interventions in the maxilla. CS 3 and 4 are optimal stages for an anteroposterior orthopaedic intervention in mandible [12].
The complete set of cephalometric radiographs was assessed by one observer (LM). One hundred and seventeen randomly selected radiographs were re-assessed by the same observer on a second occasion and also by a second observer (LT) in order to determine intra- and interobserver agreement. This specific number was determined to be the minimal amount of radiographs needed to show with 80% certainty that the lower limit of the 95% confidence interval for an ICC of 0.80 was not less than 0.70 when having two observers [23]. Before the start of the assessment, the observers were repeatedly trained with radiographs of a smaller patient sample. This training consisted of scoring followed by evaluation and remediation. During the assessment, the observers were provided with multiple reference photographs and written descriptions of the cervical morphology of each single stage as described in Baccetti et al. [12].
Statistical analysis
Analyses were performed in SPSS version 25 (IBM, Armonk, New York, USA). Intra- and interobserver agreement were determined by means of the intraclass correlation coefficient (ICC).All analyses were performed separately for boys and girls. Chi-square tests were used to test if there is an association between presence of a cleft and having a CVM score ≥ CS3 and having a CVM score ≥ CS5. Mann-Whitney U tests were used to test if the mean ranking of the CVM score is different between the cleft group and control group. This test was also used per age category. Logistic regression analysis with age (categorical), presence of a cleft, and their two-way interaction as fixed factors in the model, was used to test if there was an association between the presence of a cleft and having a CVM score ≥ CS3 and ≥ CS5, respectively, according to age category. This regression analysis was also repeated after exclusion of the children with isolated cleft palate (CP) to assess the effect of this cleft type with a different genotype than cleft lip (CL) and cleft lip and palate (CLP).
Results
The application of the in- and exclusion criteria resulted in a study group of 246 patients. The sample characteristics with the distribution according to the age, sex, and cleft type are shown in Table 1. A control group of 210 patients was compiled. Patients in the cleft and control group had a European or North African ancestry and were born between 1989 and 2005 and between 1992 and 2006, respectively. The absolute frequencies of each CVM score according to gender, group, and age can be consulted in Supplementary file 1.
The ICC between the two observers (LM and LT) was 0.907 with a 95% confidence interval of 0.850–0.940. The ICC within one observer (LT) was 0.891 with a 95% confidence interval of 0.840–0.925. There were 2 weeks between the first and second scoring of the radiographs. Both ICCs indicate excellent agreement [24].
For both boys and girls in this sample, there was a significant association between the presence of a cleft and a CVM score of CS3 or higher (p from Chi-square test = 0.033 and 0.031 respectively), with control patients being more likely to have a CVM score of CS3 or higher compared to cleft patients (risk ratio = 76.6/63.6 = 1.20 and 69.0/54.3 = 1.27 respectively). No association between the presence of a cleft and having a CVM score of CS5 or higher was found in any of the two genders (p value from Chi-square test = 0.849 and 0.069 respectively). The corrected coefficients of contingency for the association between cleft and CSV stages are shown in Supplementary file 2.
Boys showed no significant difference in the mean ranking on the CVM score between control and cleft children (p value from Mann-Whitney U test = 0.231). This non-significant association was also detected in each age subsample. In girls, a significant difference in mean ranking on the CVM score between control and cleft children was detected (p value from Mann-Whitney U test = 0.010), with control patients having a higher mean rank than cleft patients. However, this association was only significant for the age subsample 11 to 12 years (p value from Mann-Whitney U test < 0.001).
Logistic regression analysing the association between the presence of a cleft and having a CVM score of CS3 or higher/CS5 or higher according to age category was performed for each sex. The underlying regression function for the model of a CVM score of CS3 or higher in girls is shown as an example in Supplementary file 3. In boys, no association between the presence of a cleft and CVM score of CS3 or higher or a score of CS5 or higher was detected in any age subsample (Figs. 3 and 4). For girls, the subsample with age 11 to 12 showed a significant association between the presence of a cleft and CVM score of CS3 or higher, with the cleft group having 90.0% lower estimated odds of CS3 or higher compared to the control group (95% CI goes from 62.0% to 97.4% lower odds, p value = 0.001) (Fig. 5). Similarly, the subsample with age 12 to 13 showed a borderline non-significant association between the presence of a cleft and CVM score of CS5 or higher, with the cleft group having 75.20% lower estimated odds of CS5 or higher compared to the control group (95% CI goes from 94.0% lower odds to 3.2% higher odds, p value = 0.055) (Fig. 6). The regression analysis after exclusion of the cases with isolated CP showed similar estimated probabilities of CS3 or higher/CS5 or higher, both in boys and girls (Supplementary files 4 and 5).
Discussion
In the sample of the current study, boys and girls with a cleft lip and/or palate were less likely to have a CVM score of CS3 or higher (risk ratio = 0.83 (boys) and 0.79 (girls)) than non-affected individuals. In contrast, there was no significant association between the presence of a cleft and having a CVM score of CS5 or higher. These observations could substantiate the assumption that the growth spurt in cleft patients starts at a later chronological age, is of a shorter duration, and therefore might proceed at a higher velocity. Regrettably, due to the cross-sectional nature of the data, no robust statistical model as a time-to-event analysis could be applied to confirm this hypothesis. However, a logistic regression model could detect that cleft girls have a significantly lower probability of having a CVM score of at least CS3 in the subsample with age 11 to 12 (p = 0.001). Although strictly non-significant (p = 0.055), we also could say that girls showed a (borderline) lower probability of having a CVM score of at least CS5 in the subsample with ages 12 to 13.
Clefts associated with a syndrome were excluded during patient sampling to isolate the effect of the cleft on growth. Nevertheless, inter-subject variability cannot be excluded completely in the study sample. Patients with a cleft lip, cleft lip and alveolus, or cleft lip and palate have a distinct different genotype than patients with an isolated cleft palate. However, it is unknown if the expression of these different genotypes results in differences regarding start, length, and intensity of the pubertal growth spurt.
CVM staging of cleft patients and subsequent comparison with a non-affected control group in a cross-sectional design has been performed previously. Sun and Li calculated odds ratios to test whether cleft patients were more likely not to reach CVM stage 3 or higher. They concluded that Han Chinese cleft boys and girls are at higher risk for a delayed skeletal maturation [25, 26]. Ravi and Ravikala concluded that there is a delay in skeletal maturation at a younger age (10–13 years) but not at an older age (13–15 years) in children with unilateral cleft lip and palate (UCLP) [27]. Although this conclusion has common grounds with the discrete trend observed in the current study, the smaller study sample (60 children with UCLP and 60 non-affected controls) of Ravi and Ravikala might have affected the statistical power. Flieger et al. concluded that cleft patients achieve various CVM scores at later chronological age compared to non-affected patients. However, the absent distinction between boys and girls in both the study and control groups subverts the validity of the results [28]. Cesur et al. also observed a delayed skeletal maturation for boys and girls under the age of 11 in a sample of 85 children with UCLP [29].
Newborn cleft children present impaired craniofacial development before any surgical intervention. Therefore, growth impairment could be classified to some extent as an intrinsic characteristic of the cleft condition. These children present an aberrant genotype, although associated with a highly variable phenotype. It has been observed that sella turcica morphology is deviant in newborn cleft children. This might explain why a subset of this population has occult midline, neural and learning deficiencies, and hypophyseal/endocrine and somatic growth problems [30]. Growth hormone deficiency has also been observed 40 times more often in cleft children than in their non-affected peers [5]. However, nutritional status during early life could also be associated with delayed skeletal maturity. A cleft palate can prevent a newborn cleft child from creating sufficient negative pressure necessary to feed and can limit the normal use of the tongue to compress the nipple [31]. This results in significantly lower weight gain per week in newborns with a cleft [32].
Ethnic background might have been a confounding factor. The sample consisted of individuals with a European or a North African geographic and genetic ancestry. However, in multiethnic cohort studies, both groups are consistently classified in the same ancestry group (European) [33, 34]. Therefore, the confounding effect of ethnicity could be considered of minor importance.
The CVM method is an established procedure to determine the proper timing of dentofacial orthopaedics. Despite its long track record, the method remains a topic for debate. Reliability, repeatability, accuracy, and reproducibility are reported to be highly variable, going from low, moderate, substantial, to high [35,36,37,38,39]. Our results for inter- and intra-observer agreement generally coincide with the reported values between 0.800 and 1 in a 2015 meta-analysis [21]. Perinetti et al. introduced a more extended and objective, morphometric CVM code staging system. They applied this novel method on a cohort of the Oregon Growth Study. It was observed that cases outside the reported norms were not frequent and most of the exceptions were seen in CVM stage 4. Generally, they concluded that the classic CVM method might require more comprehensive staging instructions and that inter-subject variability might be relevant in terms of duration of the single CVM stages [40].
The presence and completeness of a cleft in the alveolus and/or palate might affect the orthopaedic aspect of maxillary expansion in the transverse dimension. In these cases, the increase of the transverse maxillary dimension is to a lesser extent the result of opening of the intermaxillary suture, but mainly the result of opening of the alveolar and/or palatal cleft. A recent study on CBCT observed an average increase of the alveolar cleft volume of 19.6% following rapid maxillary expansion in unilateral clefts [41]. Nevertheless, the intermaxillary suture is not the only determinant of the orthopaedic effect during maxillary expansion. A 2007 study on the biomechanical effects of maxillary expansion on the craniofacial skeleton in a UCLP model using finite element analysis concluded that the fusion or lack thereof between the maxilla and pterygoid plate of the sphenoid bone (pterygomaxillary sutures) was determinative for resistance to expansion forces, regardless of the absence of the midpalate [42]. Notwithstanding the potentially impaired opening of the intermaxillary suture in cleft patients with involvement of the alveolus and/or palate, the orthopaedic effect of a maxillary expander is not solely limited to the transverse correction. It also induces the opening or compression of internasal, nasomaxillary, frontomaxillary, and frontonasal sutures. The stress was induced at these sutures also attributing to a downward and forward displacement of the maxilla [43, 44]. The clinical relevance of the latter in cleft patients and the relationship with the extent and volume of the cleft in the alveolus and palate remain interesting topics for further research.
Clinically, cleft patients present a wide spectrum of transverse, anteroposterior, and vertical deformities of the maxilla and mandible. A substantial part of the malocclusions related to these deformities can be approached in a non-surgical manner if the intervention is well timed. Generally, optimal timing of maxillary expansion is during the CVM stages CS1 and CS2. The current study suggests that these stages might occur at an older chronological age, especially in girls. However, when the cleft is not only limited to the lip or the palate, the timing of maxillary transverse correction is rather also dictated by the dental development than the skeletal age. In the unilateral cleft lip and alveolus (UCLA), unilateral cleft lip and palate (UCLP), and bilateral cleft lip and palate (BCLP), the development of the cleft-adjacent canine(s) dictates the timing of the early secondary bone grafting and subsequently the timing of the preoperative expansion of the maxilla [45]. After all, this expansion is often required to restore the alveolar morphology and to improve access to the receptor site during surgery. Solis et al. concluded that the development of the cleft-adjacent canine in complete UCLP was 1.39 years delayed in comparison to a non-affected population [46].
In a class III relationship due to deficient maxillary growth, maxillary protraction can be performed by means of a face mask or with bone-anchored maxillary protraction (BAMP) and class III intermaxillary elastics. The latter approach has gained remarkable interest and has recently been subject of comprehensive research in UCLP. The three-dimensional assessment of the maxilla, mandible, and the glenoid fossa showed similar effects in patients with and without clefts [9, 47]. The optimal timing of a skeletal class III correction with effect on both the upper and lower jaw is during CVM stages CS1 and CS2. Again, the current study suggests that these stages might occur at an older chronological age, especially in girls.
Therapy for a relative class II jaw relationship (occasionally seen in mild CP and CL cases) can be performed with a functional appliance such as a Herbst appliance or an activator [11]. The optimal timing of a skeletal class II correction is during CVM stages CS3 and CS4. The current study suggests that these stages might occur at a slightly older chronological age in girls.
Conclusions
The current study demonstrated, within its limitations, a discrete delay in skeletal maturation before the pubertal growth spurt of (pre)adolescents with CL/P, especially in girls. Further research must quantify this delay, investigate its clinical significance, and determine its effect on the timing of dentofacial orthopaedic treatment.
References
Ross RB (1987) Treatment variables affecting facial growth in complete unilateral cleft lip and palate. Cleft Palate J 24:5–77
Kapucu MR, Gursu KG, Enacar A, Aras S (1996) The effect of cleft lip repair on maxillary morphology in patients with unilateral complete cleft lip and palate. Plast Reconstr Surg 97:1371–1375 discussion 1376-1378
Meazzini MC, Tortora C, Morabito A, Garattini G, Brusati R (2011) Factors that affect variability in impairment of maxillary growth in patients with cleft lip and palate treated using the same surgical protocol. J Plast Surg Hand Surg 45:188–193. https://doi.org/10.3109/2000656X.2011.583493
Roitman A, Laron Z (1978) Hypothalamo-pituitary hormone insufficiency associated with cleft lip and palate. Arch Dis Child 53:952–955
Rudman D, Davis T, Priest JH, Patterson JH, Kutner MH, Heymsfield SB, Bethel RA (1978) Prevalence of growth hormone deficiency in children with cleft lip or palate. J Pediatr 93:378–382
De Clerck HJ, Proffit WR (2015) Growth modification of the face: a current perspective with emphasis on class III treatment. Am J Orthod Dentofac Orthop 148:37–46. https://doi.org/10.1016/j.ajodo.2015.04.017
Yang X, Li C, Bai D, Su N, Chen T, Xu Y, Han X (2014) Treatment effectiveness of Frankel function regulator on the class III malocclusion: a systematic review and meta-analysis. Am J Orthod Dentofac Orthop 146:143–154. https://doi.org/10.1016/j.ajodo.2014.04.017
Garib D, Yatabe M, de Souza Faco RA, Gregorio L, Cevidanes L, de Clerck H (2018) Bone-anchored maxillary protraction in a patient with complete cleft lip and palate: a case report. Am J Orthod Dentofac Orthop 153:290–297. https://doi.org/10.1016/j.ajodo.2016.10.044
Yatabe M, Garib DG, Faco RAS, de Clerck H, Janson G, Nguyen T, Cevidanes LHS, Ruellas AC (2017) Bone-anchored maxillary protraction therapy in patients with unilateral complete cleft lip and palate: 3-dimensional assessment of maxillary effects. Am J Orthod Dentofac Orthop 152:327–335. https://doi.org/10.1016/j.ajodo.2016.12.024
da Silva Filho OG, Normando AD, Capelozza Filho L (1993) Mandibular growth in patients with cleft lip and/or cleft palate--the influence of cleft type. Am J Orthod Dentofac Orthop 104:269–275. https://doi.org/10.1016/s0889-5406(05)81729-9
Sarnas KV, Rune B, Aberg M (2000) Facial growth in a cleft palate patient treated with the Herbst appliance: a long-term profile roentgenographic and roentgen stereometric analysis of profile changes and displacement of the jaws. Cleft Palate Craniofac J 37:71–77. https://doi.org/10.1597/1545-1569_2000_037_0071_fgiacp_2.3.co_2
Baccetti T, Franchi L, McNamara JJ (2005) The cervical vertebral maturation (CVM) method for the assessment of optimal treatment timing in dentofacial orthopedics. Semin Orthod 11:119–129
Proffit WR, Fields HW, Sarver DM (2014) Contemporary orthodontics - fifth edition. Elsevier Health Sciences, St. Louis
Bjork A (1963) Variations in the growth pattern of the human mandible: longitudinal radiographic study by the implant method. J Dent Res 42(1)Pt 2:400–411. https://doi.org/10.1177/00220345630420014701
Bjork A, Helm S (1967) Prediction of the age of maximum puberal growth in body height. Angle Orthod 37:134–143. https://doi.org/10.1043/0003-3219(1967)037<0134:POTAOM>2.0.CO;2
Perinetti G, Sbardella V, Contardo L (2017) Diagnostic reliability of the third finger middle phalanx maturation (MPM) method in the identification of the mandibular growth peak. Eur J Orthod 39:194–201. https://doi.org/10.1093/ejo/cjw059
O'Reilly MT, Yanniello GJ (1988) Mandibular growth changes and maturation of cervical vertebrae--a longitudinal cephalometric study. Angle Orthod 58:179–184. https://doi.org/10.1043/0003-3219(1988)058<0179:MGCAMO>2.0.CO;2
Baccetti T, Franchi L, McNamara JA Jr (2002) An improved version of the cervical vertebral maturation (CVM) method for the assessment of mandibular growth. Angle Orthod 72:316–323. https://doi.org/10.1043/0003-3219(2002)072<0316:AIVOTC>2.0.CO;2
Lamparski DG (1972) Skeletal age assessment utilizing cervical vertebrae. Am J Orthod Dentofac Orthop 67:458–459
Szemraj A, Wojtaszek-Slominska A, Racka-Pilszak B (2018) Is the cervical vertebral maturation (CVM) method effective enough to replace the hand-wrist maturation (HWM) method in determining skeletal maturation?-a systematic review. Eur J Radiol 102:125–128. https://doi.org/10.1016/j.ejrad.2018.03.012
Cericato GO, Bittencourt MA, Paranhos LR (2015) Validity of the assessment method of skeletal maturation by cervical vertebrae: a systematic review and meta-analysis. Dentomaxillofac Radiol 44:20140270. https://doi.org/10.1259/dmfr.20140270
Cooke DW, Divall SA, Radovick S (2016) Chapter 24 - Normal and aberrant growth in children. In: Melmed S, Polonsky KS, Larsen PR, Kronenberg HM (eds). Williams Textbook of Endocrinology, Philadelphia
Zou GY (2012) Sample size formulas for estimating intraclass correlation coefficients with precision and assurance. Stat Med 31:3972–3981. https://doi.org/10.1002/sim.5466
Altman DG (1991) Practical statistics for medical research. Chapman and Hall, London
Sun L, Li WR (2013) Cervical vertebral maturation of female children with orofacial clefts. Cleft Palate Craniofac J 50:535–541. https://doi.org/10.1597/11-215
Sun L, Li WR (2012) Cervical vertebral maturation of children with orofacial clefts. Cleft Palate Craniofac J 49:683–688. https://doi.org/10.1597/11-006
Ravi M, Ravikala S (2013) Assessment of skeletal age in children with unilateral cleft lip and palate. Int J Clin Pediatr Dent 6:151–155. https://doi.org/10.5005/jp-journals-10005-1209
Flieger R, Kopczynski P, Matthews-Brzozowska T (2015) Analysis of skeletal maturity of children with cleft palate in terms of healthy children by the CVM method. Adv Clin Exp Med 24:99–102. https://doi.org/10.17219/acem/38165
Cesur E, Altug AT, Toygar-Memikoglu U, Gumru-Celikel D, Tagrikulu B, Erbay E (2018) Assessment of sella turcica area and skeletal maturation patterns of children with unilateral cleft lip and palate. Orthod Craniofacial Res 21:78–83. https://doi.org/10.1111/ocr.12219
Nielsen BW, Molsted K, Kjaer I (2005) Maxillary and sella turcica morphology in newborns with cleft lip and palate. Cleft Palate Craniofac J 42:610–617. https://doi.org/10.1597/04-104r.1
Bessell A, Hooper L, Shaw WC, Reilly S, Reid J, Glenny AM (2011) Feeding interventions for growth and development in infants with cleft lip, cleft palate or cleft lip and palate. Cochrane Database Syst Rev CD003315. https://doi.org/10.1002/14651858.CD003315.pub3
Jones WB (1988) Weight gain and feeding in the neonate with cleft: a three-center study. Cleft Palate J 25:379–384
Medina-Gomez C, Heppe DHM, Yin JL, Trajanoska K, Uitterlinden AG, Beck TJ, Jaddoe VWV, Rivadeneira F (2016) Bone mass and strength in school-age children exhibit sexual dimorphism related to differences in lean mass: the generation R study. J Bone Miner Res 31:1099–1106. https://doi.org/10.1002/jbmr.2755
Grgic O, Shevroja E, Dhamo B, Uitterlinden AG, Wolvius EB, Rivadeneira F, Medina-Gomez C (2020) Skeletal maturation in relation to ethnic background in children of school age: the generation R study. Bone 132:115180. https://doi.org/10.1016/j.bone.2019.115180
Santiago RC, de Miranda Costa LF, Vitral RW, Fraga MR, Bolognese AM, Maia LC (2012) Cervical vertebral maturation as a biologic indicator of skeletal maturity. Angle Orthod 82:1123–1131. https://doi.org/10.2319/103111-673.1
Zhao XG, Lin J, Jiang JH, Wang Q, Ng SH (2012) Validity and reliability of a method for assessment of cervical vertebral maturation. Angle Orthod 82:229–234. https://doi.org/10.2319/051511-333.1
Gabriel DB, Southard KA, Qian F, Marshall SD, Franciscus RG, Southard TE (2009) Cervical vertebrae maturation method: poor reproducibility. Am J Orthod Dentofac Orthop 136(478):e471–e477; discussion 478-480. https://doi.org/10.1016/j.ajodo.2007.08.028
Sohrabi A, Babay Ahari S, Moslemzadeh H, Rafighi A, Aghazadeh Z (2016) The reliability of clinical decisions based on the cervical vertebrae maturation staging method. Eur J Orthod 38:8–12. https://doi.org/10.1093/ejo/cjv030
Cunha AC, Cevidanes LH, Sant'Anna EF, Guedes FR, Luiz RR, McNamara JA, Franchi L, Ruellas ACO (2018) Staging hand-wrist and cervical vertebrae images: a comparison of reproducibility. Dentomaxillofac Radiol 47:20170301. https://doi.org/10.1259/dmfr.20170301
Perinetti G, Bianchet A, Franchi L, Contardo L (2017) Cervical vertebral maturation: an objective and transparent code staging system applied to a 6-year longitudinal investigation. Am J Orthod Dentofac Orthop 151:898–906. https://doi.org/10.1016/j.ajodo.2016.09.026
Veloso NC, Mordente CM, de Sousa AA, Palomo JM, Yatabe M, Oliveira DD, Souki BQ, Andrade I Jr (2020) Three-dimensional nasal septum and maxillary changes following rapid maxillary expansion in patients with cleft lip and palate: a case-series analysis. Angle Orthod 90:672–679. https://doi.org/10.2319/090719-583.1
Pan X, Qian Y, Yu J, Wang D, Tang Y, Shen G (2007) Biomechanical effects of rapid palatal expansion on the craniofacial skeleton with cleft palate: a three-dimensional finite element analysis. Cleft Palate Craniofac J 44:149–154. https://doi.org/10.1597/05-161.1
Gautam P, Valiathan A, Adhikari R (2007) Stress and displacement patterns in the craniofacial skeleton with rapid maxillary expansion: a finite element method study. Am J Orthod Dentofac Orthop 132(5):e1–e11. https://doi.org/10.1016/j.ajodo.2006.09.044
Figueiredo DS, Bartolomeo FU, Romualdo CR, Palomo JM, Horta MC, Andrade I Jr, Oliveira DD (2014) Dentoskeletal effects of 3 maxillary expanders in patients with clefts: a cone-beam computed tomography study. Am J Orthod Dentofac Orthop 146:73–81. https://doi.org/10.1016/j.ajodo.2014.04.013
Weissler EH, Paine KM, Ahmed MK, Taub PJ (2016) Alveolar bone grafting and cleft lip and palate: a review. Plast Reconstr Surg 138:1287–1295. https://doi.org/10.1097/PRS.0000000000002778
Solis A, Figueroa AA, Cohen M, Polley JW, Evans CA (1998) Maxillary dental development in complete unilateral alveolar clefts. Cleft Palate Craniofac J 35:320–328. https://doi.org/10.1597/1545-1569_1998_035_0320_mddicu_2.3.co_2
Yatabe M, Garib D, Faco R, de Clerck H, Souki B, Janson G, Nguyen T, Cevidanes L, Ruellas A (2017) Mandibular and glenoid fossa changes after bone-anchored maxillary protraction therapy in patients with UCLP: a 3-D preliminary assessment. Angle Orthod 87:423–431. https://doi.org/10.2319/052516-419.1
Acknowledgements
The authors wish to thank Dr. S. De Buyser for the statistical analyses.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Laurent AM Thierens and Laura Manalili. The first draft of the manuscript was written by Laurent AM Thierens, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee (Ethics Committee Ghent University Hospital with reference 2019/1064; Ethics Committee University Hospitals Leuven with reference S63027) and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
The study was performed anonymized. Therefore, no informed consents were obtained.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
ESM 1
(DOCX 35 kb)
Rights and permissions
About this article
Cite this article
Thierens, L.A.M., Manalili, L., De Roo, N. et al. Assessment of craniofacial maturation in preadolescents with cleft lip and/or palate using the cervical vertebral maturation method. Clin Oral Invest 25, 4851–4859 (2021). https://doi.org/10.1007/s00784-021-03790-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-021-03790-2