Abstract
Objectives
This study compared the osseointegrative potential of a novel injection molded zirconia dental implant (Neodent Zi ceramic implant, test) and a commercially available titanium implant (Neodent Alvim implant, control) in terms of histomorphometrically derived bone-to-implant contact (BIC), first bone-to-implant contact (fBIC), and the ratio of bone area to total area (BATA) around the implant.
Materials and methods
A total of 36 implants, 18 per individual test device, were implanted in a split-mouth arrangement in either side of the edentulous and fully healed mandible of 6 minipigs. Histomorphometric analysis of BIC, fBIC, and BATA were performed 8 weeks post implantation and subjected to statistical non-inferiority testing. Surface characteristics of both implant types were compared in terms of contact angle, surface topography, and elemental composition.
Results
BIC, fBIC, and coronal BATA values of test and control implants were statistically comparable and non-inferior. BIC values of 77.8 ± 6.9% vs. 80.7 ± 6.9% (p = 0.095) were measured for the test and control groups. fBIC lingual values were − 238 ± 328 μm compared with − 414 ± 511 μm (p = 0.121) while buccal values were − 429 ± 648 μm and − 588 ± 550 μm (p = 0.230) for the test and control devices, respectively. BATA in the apical segment was significantly higher in the test group compared with the control group (67.2 ± 11.8% vs. 59.1 ± 11.4%) (p = 0.0103). Surface topographies of both implant types were comparable. Surface chemical analysis indicated the presence of carbonaceous adsorbates which correlated with a comparable and predominantly hydrophobic character of the implants.
Conclusion
The results demonstrate that the investigated zirconia implants, when compared with a commercially available titanium implant, show equivalent and non-inferior bone integration, bone formation, and alveolar bone level maintenance. This qualifies the investigated zirconia implant as a potential candidate for clinical development.
Clinical relevance
This study investigated the osseointegration of a novel zirconia 2-piece dental implant prototype intended for clinical development. With the aim of translating this prototype into clinical development preclinical models, procedures and materials within this study have been selected as close to clinical practice and human physiological conditions as possible.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Ceramic materials have recently attracted increasing attention as an alternative to titanium for the manufacturing of endosseous dental implants [1]. Driven by its mechanical stability, yttria-stabilized tetragonal zirconia polycrystal (YTZP, short zirconia) has been established as the material of choice for such applications [2]. The mechanical stability of this metastable modification of zirconia is linked to its ability of reducing crack propagation by dissipating the involved energy into the conversion of individual crystallites of the composite into the thermally stable allotrope [3]. The resulting high bending strength and fracture toughness combine with other advantages of this material like a high resistance towards mechanical wear, excellent chemical inertness, high biocompatibility, and a low affinity to bacterial colonization. These properties qualify the material as an excellent candidate for the use as dental implants [4,5,6,7].
Currently, the majority of zirconia implants are still one-piece implants [8]. Although potentially less prone to mechanical failure, one-piece implants bear significant limitations with regard to indications and prosthetic restorations [9]. With increasing experience on their material specific design requirements, 2-piece zirconia implants are now starting to show promising clinical study results and in-field real-world data [10].
Current, state-of-the-art commercially available zirconia implants are produced exclusively by the use of subtractive milling techniques. Surface modifications have shown to potentially increase the osseointegrative properties of zirconia implants. Such modifications, however, represent additional manufacturing steps that significantly increase the manufacturing costs [8, 11, 12]. Further, the mechanical effect/s of such surface modifications must be carefully considered and balanced against the desired positive biological effects [13].
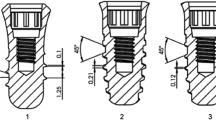
Compared with the current manufacturing techniques, additive manufacturing, and more specifically ceramic injection molding (CIM), represents one of the most promising techniques for mass production of high-quality zirconia implants at significantly reduced costs [14]. The technology is based on plasticity shaping of a zirconia/binder formulation into the form of the implant body (green body). Any organic component is subsequently removed via a carefully controlled process of debinding and sintering under preservation of the overall macroscopic and microscopic shape [15]. Theoretically, one of the great advantages of CIM is the ability to concurrently manufacture and surface engineer a zirconia implant in one single process step by incorporating the desired surface topography directly into the mold [16].
Only a limited number of reports on injection molded zirconia implants are currently available in the literature. These studies mainly address the osseointegrative properties as a function of surface morphology and are based on preclinical prototypes [16,17,18,19]. Considering implant shape, thread design, and drilling protocols have been reported to be equally important design parameters with regard to osseointegration, it is important to isolate as many of these confounding parameters as possible in order to focus on the novelty associated with the test item [20]. Therefore, the aim of this non-randomized, controlled preclinical study was to compare the osseointegrative properties of a novel injection molded 2-piece zirconia implant with those of a commercially available titanium implant, both of which presented the same macro-geometry, dimensions, and consequent drill protocol.
Materials and methods
The primary aim of the study was to test the non-inferiority of the osseointegrative properties of the novel zirconia implant (test device; Neodent Zi ceramic implant) in comparison with the titanium implant (control device; Neodent Alvim with NeoPoros surface) in a mandibular minipig model at 8 weeks after implantation. Test and control implants had identical tapered effect geometries with a diameter of 4.3 mm and a 10 mm length. A total of 18 implants per group were placed with 3 implants per hemi-mandible in a split-mouth design (6 implants per animal). Primary parameters of the study were the histomorphometrically derived percentage of bone-to-implant contact (BIC). Secondary outcomes comprised the first bone-to-implant contact (fBIC) and the ratio of bone area to total area (BATA) as determined in predefined regions of interest around the implant. Furthermore, implant surface characteristics of the two implant types were compared in terms of dynamic contact angle (DCA) measurements, surface roughness measurements (Sa is the average height deviation from the mean plan, Sz is the maximum height differences of the roughness (i.e., differences between the maximum and minimum surface topographical heights), and Ssk is the skewness of the height distribution), X-ray photoelectron spectroscopy (XPS), and scanning electron microscopy (SEM).
This study was conducted at the Biomedical Department of Lund University (Sweden) and approved by the local ethics committee of the university (M-192-14). The study was conducted in accordance with ISO 10993-6 “Biological evaluation of medical devices – Part 6: Tests for local effects after implantation guideline and recommendations.” This study adheres to the ARRIVE guidelines.
Six female Göttingen Minipigs™ (Ellegaard, Denmark) of age between 20 and 24 months at the time of surgery and an average body weight of 40 kg were included in the study. The animals were housed in standard boxes in groups of three starting. Housing started 1 week prior intervention to adapt the animal to experimental conditions. Animals were fed a standard soft food diet (Special Diet Services (SDS), Witham, UK (#801586)). Prior to the surgical procedure, all animals were fasted overnight to prevent vomiting.
Surgical procedure
All surgical procedures were performed under general anesthesia using a combination of dexmedetomidine (25–35 μg/kg i.m., Dexdomitor; Orion Pharma Animal Health) and tiletamine-zolazepam (50–70 mg/kg i.m., Zoletil 100 Vet, Virbac) injected intramuscularly and maintained with intravenous infusion after induction with propofol (PropoVet multidose, Orion Pharma Animal Health) and fentanyl (Fentanyl B. Braun). Carprofen (4 mg/kg, s.i.d., i.m., Rimadyl vet., Orion Pharma Animal Health) was given as a preemptive dose and postsurgically up to 4 days together with buprenorphine (0.03 mg/kg, i.m., Vetergesic vet, Orion Pharma Animal Health). To reduce the dosage of the systemic anesthetic, reduce bleeding during surgery, and alleviate postsurgical pain, local anesthesia was provided intraoperatively by means of an infiltrative injection of 1.8 ml of Xylocaine (Xylocaine, Dental adrenalin, 20 mg/ml and 12.5 μg/ml; Astra AB) per hemi-mandible.
Antibiotic prophylaxis was administered using bensylpenicillinprokain-dihydrostreptomycin (25 mg/kg + 20 mg/kg, s.i.d., i.m., Streptocillin vet., Boehringer Ingelheim Vetmedica). During administration of anesthesia, the animals were intubated and breathing withheld by a ventilator. Vital parameters were monitored continuously (pulse oximetry, rectal temperature, blood pressure, CO2).
Tooth extraction
Both contralateral mandibular premolars (P2–P4) and first mandibular molars (M1) were carefully extracted via a minimally invasive surgical approach, i.e., without raising a flap.
Implant osteotomy and placement
Implant placement was performed 12 weeks post extraction as depicted in Fig. 1. Both sides of the mandibular alveolar ridge were exposed by mid-crestal incision and reflection of a mucoperiosteal flap. The alveolar ridge was carefully flattened using a cylindrical cutting bur.
Depiction of the different steps of the surgical procedure. a Crestal incision. b Mucoperiosteal flap preparation. c Flatting of the alveolar bone crest. d–i Implant bed preparation involving drill sequence using pilot drills with diameters 2.2 mm, 2.8 mm, and 3.5 mm and fine preparation of the implant bad involving coronal profile drilling and threaded implant bed preparation. j–l Implant insertion to prepared implant bed using motorized hand piece. m–o Crestal ridge after placement of implants, healing caps, and primary wound closure with non-resorbable sutures
Implant osteotomy preparation consisted of the following drill sequence: bur diameters of 2.2 mm, 2.8 mm, and 3.5 mm followed by tapping and profiling, as per the manufacturer’s guidelines. Implants were placed at the crestal bone level using a motorized hand piece. Final implant seating was performed using a custom-made torque ratchet (Institut Straumann AG, Switzerland) to measure maximum insertion torques. Implants were subsequently equipped with healing caps (titanium cover screws, 0 mm in height) followed by primary wound closure with resorbable sutures.
Antibiotic cover was administered for 7 days (Streptocillin vet, Boehringer Ingelheim, 3–4 ml/pig i.m.). Further analgesia was delivered if necessary as previously described.
Termination
Termination was performed at 8 weeks post implantation by an intracardiac injection of a 20% solution of pentobarbital (Pentobarbitalnatrium, Apoteket AB; Stockholm, Sweden, 60 mg/ml).
Block sections of the implant sites were extracted using an oscillating autopsy saw under perseveration of the soft tissues. Sections were fixed in formalin (4% solution formaldehyde solution) for at least 2 weeks prior to sending for histological processing.
Histological processing
Block sections were immersed in buffered formalin solution, dehydrated using ascending grades of alcohol and xylene, and subsequently infiltrated and embedded in methyl methacrylate for non-decalcified sectioning. Block sections were next cut in buccolingual direction to sections of 500 μm and grinded to a final thickness of 30–50 μm before staining them with paragon (toluidine blue and basic fuchsin) for microscopic evaluation.
Quantitative histomorphometry
Histomorphometric measurements were performed on central buccolingual sections of the implant (Fig. 2). The distance from the implant shoulder to the fBIC and the percentage of BIC were calculated at the buccal and lingual aspects of the sections. Furthermore, the ratio of section areas containing bone area to the total area as divided into predefined coronal-apical and buccolingual quadrant sections (ROI 1 and ROI 2, Fig. 2) were determined individually and combined for the analysis into coronal and apical segments.
Illustration of measured histomorphometric parameters using histological buccolingual sections. First bone-to-implant contact (fBIC) was measured as the distance from implant shoulder to the apical bone-to-implant contact (red arrow). Bone densities (BATA) were measured in coronal (ROI 1, green area) and apical (ROI 2, blue area) regions of interest. Total bone-to-implant contact (BIC) was measured around the total endosseous circumference of the implant as the percentage the implant surface in contact with bone over the total implant surface
Surface analysis
Surface analysis were carried out directly on the implant surfaces in analogy to previously described methods [21]. In brief, advancing and receding contact angles (DCA) were measured by the dynamic Wilhelmy method on a KRÜSS K100 tensiometer (KRÜSS GmbH, Germany) in deionized water. Only advancing contact angles are reported herein. Surface roughness parameters were determined as triplicates using a μsurf explorer confocal microscope in combination with the μsoftAnalysisXT software (NanoFocus AG, Germany) at × 20 magnification. Surface parameters were evaluated on areas of 798 × 798 μm2 using a Gaussian wavelength cutoff wavelength of 50 × 50 μm2. Surface morphology and EDX measurements were carried on a Zeiss Supra 55 SEM (Carl Zeiss AG, Germany) equipped with an Everhart-Thornley secondary electron detector at an acceleration voltage of 15 kV and 5 kV for the low- and high-resolution voltages. Zirconia implants were sputtered before analysis. X-ray photoelectron spectroscopy was carried out on a PHI 5000 VersaProbe spectrometer (ULVAC-PHI, Inc., USA), and XPS spectra were processed and integrated using CasaXPS following Shirley background subtraction.
Statistical evaluation
Non-inferiority testing was performed on the basis of the following null and alternative hypotheses (H0 and HA):
-
H0: The test device is non-inferior to the control device in terms of BIC, fBIC, or BATA after 8 weeks of healing.
-
HA: BIC, fBIC, or BATA of the test and control devices at 8 weeks of healing is significantly different.
For adjusted comparisons and the non-inferiority tests, a mixed linear regression model was used that adjusted for animal effect, side of the mandible, and position of the test item. The animal effect was introduced in the model as a random effect while all other factors were set as fixed effects. The Dunnett-Hsu adjustment was used to adjust the p values in the case of multiple comparisons. A p value of < 0.05 was considered statistically relevant.
For the hypothesis of non-inferiority of the test device compared with a control device, the average effect and its two-tailed 90% confidence interval was calculated using the above-described regression model. The expected average BIC value was set to 60% with an acceptance range of 15%. These assumptions were based on BIC values reported in the literature on comparable study designs and equivalent healing periods [22,23,24,25]. Ranges of BIC and standard deviations in these studies were from 35.4 to 78.9% and from 9.7 to 22%, respectively. The lower limit of the confidence interval served as the tolerance range for the support of the null hypothesis.
Results
All animals recovered from surgeries in a predictable manner and with uneventful healing. No specific surgical, perioperative, or postoperative complications or signs of inflammation were noted. Test group data of one animal were dropped from histomorphometric evaluation due to the animal chewing on a water pipe during the healing phase, leading to morphological anomalies of formed bone. Removal of these data from the data set was further supported by a statistical analysis for outliers and influencing values (see supplementary information S1). This reduced the number of specimens used for histomorphometry in the test group to 15 compared with 18 specimens in the control group.
Insertion torque
As illustrated by Fig. 3, the insertion torques for implants of the test group were significantly lower compared to the values of the control group. Specifically, average maximum insertion torques and standard deviations were 60.7 ± 14.2 N-cm in the test group compared with 96.7 ± 13.7 N-cm in the control group.
Histologic and histomorphometric analysis
All specimens considered for histomorphometry were well osseointegrated (Fig. 4); 33.3% of test specimens and 16.7% of control specimens, respectively, showed crestal bone overgrowth over the healing cap. The complete set of histological micrographs is included in the supplementary information (Figs. S1 and S2). Tables 1 and 2 show the descriptive statistics for the histomorphometric outcomes and the paired comparisons of both implant types, respectively.
Buccolingual histological sections of test (a) and control (b) implants. The buccal side is oriented to the left for the control specimen (a) and to the right for the test specimen (b). c Comparison of average total bone-to-implant contacts (total BIC) and corresponding standard deviations for test and control specimens (p = 0.095)
Both implant types showed comparable values in terms of overall bone integration, as measured by BIC (Fig. 4). Specifically, mean BIC values of 77.8 ± 6.9% and 80.7 ± 6.9% were measured for the test and control groups, respectively, with the difference of − 3.9 ± 7.4% being non-statistically significant (p value = 0.095).
fBIC as determined for the lingual and buccal aspects showed a trend towards lower values in the control group compared with the test group; however, differences were not statistically significant (Fig. 5). In detail, lingual mean fBIC for the test and control groups was − 238 ± 328 μm and − 414 ± 511 μm, respectively, while buccal values were − 429 ± 648 μm and − 588 ± 550 μm, respectively.
BATA as an indicator for peri-implant bone formation around the implants was analyzed in 4 quadrants around the implant, i.e., differentiated into buccolingual and apicocoronal regions. As illustrated in Fig. 6 c, the total BATA was significantly higher in the test group compared with the control group for the apical section (67.2 ± 11.8% and 59.1 ± 11.4%) (mean difference = 8.0 ± 9.3; p = 0.010) while no difference could be identified in the coronal regions of interest. A subgroup analysis differentiating between lingual and buccal sections (Fig. 6a, b) indicated that this difference was mainly attributed to a difference between groups on the apical side, while corresponding values on the lingual side were comparable between groups (78.7 ± 5.3% for the test group vs. 79.3 ± 4.4% for the control group). Figure 6 also indicates that the values on the coronal aspect of the implants were generally higher compared with the corresponding values on the apical aspect independent of their buccolingual orientation.
Comparison of the ratios between bone areas to total areas (BATAs) as determined for defined apical and coronal regions of interest for lingual (a) and buccal (b) aspects of the implant as well as for the total implant area (BATA total) (c) between test and control implants. Asterisks indicate a significance level of p = 0.01
Statistical adjustment of histomorphometric parameters and non-inferiority testing
In order to test the null hypothesis of the study, i.e., non-inferiority of the test device compared with the control device, mean values of the histomorphometric parameters were statistically adjusted. Table 3 shows the multivariable association between histomorphometric parameters and study devices as well as the test parameters used for the non-inferiority testing, i.e., the average effects of the factor implant type compared to the 90% confidence intervals of the individual factors. The full set of results of the statistical analysis is provided in the supplementary part (Table S1). As evidenced by the comparisons in Table 3, all average effects were well within the confidence intervals, indicating that none of the tested parameters of the test device resulted to be non-inferior to the control device. Therefore, the null hypothesis could be accepted for all histomorphometric parameters tested within this study.
Surface morphological and chemical analysis
The results of the surface morphological and chemical analysis are summarized in Table 4 and Fig. 7, respectively. Specifically, as evidenced by the contact angles of 96.9 ± 5.9° and 95.3 ± 4.7° for test and control implants, the wettability of both implant types was comparable and moderately hydrophobic.
Surface topographical scanning electron micrographs at progressing magnifications of Ti implants (control) (a) and zirconia implants (test) (b). Images in corresponding columns were taken at progressing magnification with the lowest and highest magnifications in the top and bottom rows, respectively
SEM analysis further indicated that both titanium and zirconia implants exhibited characteristic combinations of macro-roughness and micro-roughness with associated macro-cavities with a diameter of 10–50 μm and micro-cavities of 1–2 μm, respectively (Fig. 4). From a qualitative perspective, control implant surfaces appeared to display higher levels of micro-roughness, while zirconia implant surfaces appeared to show more pronounced levels of macro-roughness combined with a granular submicron structure. The higher apparent overall surface roughness of control implant surfaces corroborated with the higher Sa values (test (0.76 ± 0.16 μm) vs. control (1.14 ± 0.18 μm)) while zirconia implant surfaces displayed higher Sz values and hence more pronounced differences between maximum and minimum surface topographical heights (test (10.15 ± 6.68) vs. control (7.2 ± 0.83)). Interestingly, test and control implant surfaces displayed Ssk values with opposite signs (test (− 0.01 ± 0.3) vs. control (0.18 ± 0.16)), indicating that control surfaces were characterized mainly by distinct peaks while zirconia test implant surfaces were mainly characterized by distinct valleys.
Elemental surface compositions as derived by the integrated XPS spectra were in agreement with theoretical chemical compositions, i.e., Y-stabilized ZrO2 for the test and TiO2 for control implants, respectively (Table 4). Surfaces of both the implant types further showed relatively high amounts of carbon (43.9% for test implants and 22.6% for control implants). Further trace amounts of Si (0.2%), N (0.5%), and Na (0.4%) were detected on test substrates while control implants displayed traces of N (0.5%).
Discussion
This non-randomized, controlled split-mouth preclinical minipig study has assessed the osseointegrative capacity of a novel injection molded 2-piece zirconia implant in comparison to a commercially available tapered effect titanium implant of equivalent form and dimensions at 8 weeks after mandibular implantation and submerged healing. The comparison was specifically performed as a non-inferiority test. The choice of implant design and animal models was based with the aim of rendering the study as clinically meaningful as possible, yet also challenging the novel implant design to a worst-case scenario in terms of high bone density and reduced healing potential (the animal model used manifested a type I bone with a thick cortical layer of roughly 4 mm). Specifically, the porcine animal model has been described as very similar to humans with regard to both physiology and bone metabolism. Further, the model itself is well established for investigations of osseointegration of dental implants as a function of material and surface characteristics [26]. From the comparison of the test and control devices, five main observations were obtained: (1) Insertion torques were significantly lower for the test device; (2) BIC values of test and control devices were highly comparable; (3) lingual and buccal fBIC values were comparable for both devices, with a non-significant trend towards higher fBIC values for the test device; (4) coronal total BATA values were comparable, while apical total values were lower for the test device, which could be attributed to a difference in the bucco-apical segments. Non-inferiority of the test device compared with the control device was statistically confirmed for all histomorphometric parameters. (5) Implant surfaces displayed similar overall morphological characteristics of combined macro-porosity and micro-porosity, comparable wettability, and surface elemental compositions that corresponded to their elemental compositions and that were superimposed by varying levels of carbon and trace elements.
The difference of the insertion torques measured for the test and control devices represents valuable information that needs to be considered for any interpretation and validation of the histological results generated within this study. Average insertion torques for positioning of the implant at the crestal bone level in this study ranged between 50 and 100 N-cm for both the test and control devices and can be considered as high but still comparable to clinical settings [27]. Indeed, the control device is considered an implant for immediate placement situations and is marketed as a high primary stability implant. At recorded values, it can be assumed that all implants had good primary stability and a high level of initial bone contact. The effect of insertion torque on osseointegration and marginal bone loss is still controversially discussed. While meta-analysis failed to show any overall effect of the insertion torque on bone formation and resorption around implants, selected systematic preclinical studies seem to indicate a distinct effect [27, 28]. Trisi et al. [28] have specifically reported that high insertion torques, for example, favor higher BIC values as well as faster cortical bone remodeling compared with lower insertion torques. Interestingly, the higher insertion torques of the control implants in this study coincided with a trend towards lower fBIC and lower frequencies of bone overgrowth over the healing cap of the corresponding implants. This supports the general notion that marginal bone level changes have a tendency of being more pronounced in implants, which were placed with high levels of torque [29]. Finally, it should be noted that the observed differences between the test and control groups are not fully understood at this time. Considering the outer geometry and osteotomy preparations were identical, insertion torques were expected to show no differences. Preclinical in vivo and laboratory studies suggest that the observed differences in insertion torque may at least be partly attributed to differences in surface roughness of the implants. Specifically, although early comparisons of insertion torque values between implants with machined and sandblasted acid-etched surfaces seemed to suggest only little influence of surface topography on insertion torque values, more recent studies under defined conditions indicate a clear and strong influence of surface morphology and roughness on frictional forces between implant surfaces and osteotomy bone and hence on insertion torque values [30,31,32].
The osseointegration of zirconia implants and the influence of material and surface properties have been extensively studied. Manzano et al. [33] have recently systematically reviewed the literature comparing the osseointegrative potential of zirconia and titanium implants. From this review, the authors concluded an equivalent performance of both implant materials in terms of osseointegration. Furthermore, the authors attributed differences in osseous integration between individual zirconia implants mainly to differences in surface treatment of the zirconia implants rather than to differences in the implant material itself. The findings in our study are well in line with this general conclusion of equivalency of both material types. Furthermore, the equivalency between titanium and zirconia in terms of osseointegrative potential in this study is consistent with results of previous reports that compared CIM-manufactured zirconia and titanium implants [19]. With regard to this comparison, previous studies indicate that the CIM process itself might also contribute to the osseointegrative potential of the implant surface. Specifically, Kim et al., for example, have compared the osseointegration of CIM-manufactured to machined zirconia implants and have reported on a significantly improved osseointegration of the former implant types. Aboushelib et al. [18] have further shown that the osseointegrative potential of CIM-produced implants can be even improved above the level of titanium implants by surface roughening. However, considering the general notion that surface properties have a greater impact on osseointegration than the base material itself, it is yet impossible to determine if any one of the above materials is generally more or less efficient towards osseointegration compared to the devices used within study (no standardized surface was used across the above studies) [33].
The effect of surface structure and wettability on the osseointegrative potential of endosseous implants is well established and has been thoroughly researched [34, 35]. The chemical and surface morphological characterization reported herein demonstrated that the surfaces of both implant types displayed a comparable wettability and predominately hydrophobic character. Furthermore, both implant surfaces displayed similar overall morphology with a combined micro-roughness and macro-roughness that is typical for implants treated by a combination of sandblasting and acid etching [36]. With regard to both characterizations, i.e., the analysis of surface topography as well as to the histomorphometric analysis of osseointegration, the results reported herein are consistent with results of similar studies that have compared sandblasted and acid-etched zirconia and titanium implants [37]. Besides the discussed similarities in surface topography, this study also revealed relatively high levels of carbon and low levels of other trace elements on both implant types. The tendency of titanium surfaces to rapidly absorb hydrocarbons from air atmosphere has been well described in the literature and has been shown to render such substrates repellent to water or tissue fluids [38]. Hydrocarbon surface deposits and wettability have shown to alter the osseointegrative potential of Ti implants [39]. Since both implant surfaces studied herein displayed relatively high levels of carbonaceous species along with comparable levels of hydrophobicity, these observations corroborate well with the comparable osseointegration and bone formation around the implants. Likewise, the characterized surface properties may also imply the possibility for future chemical surface modification to potentially further improve their osseointegrative potentials.
This study further revealed a trend towards higher values in fBIC for the test device both on the lingual and on the buccal aspects. Trisi et al. [28] have shown that implants that were placed with higher insertion torque showed higher crestal bone remodeling compared with implants that were inserted at lower torque. Therefore, the relatively high insertion torque of the control implants might be a possible explanation for the observed difference in fBIC. A direct proof for this assumption would however require further investigation.
With regard to BATA, a significantly higher value was observed in the test group when compared with the control group. This difference could be attributed to differences in the apical aspect and specifically the bucco-apical aspect of the implants while the corresponding value of the coronal segment was highly comparable for both implants. From the overview of histological sections in Figs. S1 and S2, it becomes evident that some of the specimens protruded into the medullary cavity, resulting in very little to no apical bone contact at the time of placement. With regard to these histological observations, any conclusions from the observed difference in apical BATA might therefore be only considered very carefully. The coronal BATA values were highly comparable for both groups and therefore much more consistent with regard to the absence of any difference in other parameters investigated in this study and in the literature [33].
Conclusions
Within this non-randomized, controlled preclinical study, we have compared the osseointegrative potential of a new tapered effect injection molded 2-piece zirconia implant with a conventional commercially available titanium implant of the same geometry and dimensions. Our results indicate that the new zirconia-type implant performs equivalent and non-inferior with regard to osseointegration, bone formation around the implant, and maintenance of alveolar bone height. Observed differences with regard to apical bone formation between the two implant types could not be clearly attributed to the implants itself. Further studies addressing the mechanical stability and long-term reliability of this promising new implant candidate will help to translate this implant into clinic practice.
References
Pieralli S, Kohal RJ, Jung RE, Vach K, Spies BC (2017) Clinical outcomes of zirconia dental implants: a systematic review. J Dent Res 96:38–46. https://doi.org/10.1177/0022034516664043
Andreiotelli M, Wenz HJ, Kohal R-J (2009) Are ceramic implants a viable alternative to titanium implants? A systematic literature review. Clin Oral Implants Res 20:32–47. https://doi.org/10.1111/j.1600-0501.2009.01785.x
Garvie RC, Hannink RH, Pascoe RT (1975) Ceramic steel? Nature 258:703–704. https://doi.org/10.1038/258703a0
Kohal R-J, Finke HC, Klaus G (2009) Stability of prototype two-piece zirconia and titanium implants after artificial aging: an in vitro pilot study. Clin Implant Dent Relat Res 11:323–329. https://doi.org/10.1111/j.1708-8208.2008.00116.x
Piconi C, Maccauro G (1999) Zirconia as a ceramic biomaterial. Biomaterials 20:1–25. https://doi.org/10.1016/S0142-9612(98)00010-6
Rimondini L, Cerroni L, Carrassi A, Torricelli P (2002) Bacterial colonization of zirconia ceramic surfaces: an in vitro and in vivo study. Int J Oral Maxillofac Implants 17:793–798
Kohal RJ, Knauf M, Larsson B, Sahlin H, Butz F (2012) One-piece zirconia oral implants: one-year results from a prospective cohort study. 1. Single tooth replacement. J Clin Periodontol 39:590–597. https://doi.org/10.1111/j.1600-051X.2012.01876.x
Oliva J, Oliva X, Oliva JD (2010) Five-year success rate of 831 consecutively placed zirconia dental implants in humans: a comparison of three different rough surfaces. Int J Oral Maxillofac Implants 25:336–344
Cionca N, Hashim D (2000) Mombelli A (2017) Zirconia dental implants: where are we now, and where are we heading? Periodontol 73:241–258. https://doi.org/10.1111/prd.12180
Jank S, Hochgatterer G (2016) Success rate of two-piece zirconia implants: a retrospective statistical analysis. Implant Dent 25:193–198. https://doi.org/10.1097/ID.0000000000000365
Schünemann FH, Galárraga-Vinueza ME, Magini R, Fredel M, Silva F, Souza JCM, Zhang Y, Henriques B (2019) Zirconia surface modifications for implant dentistry. Mater Sci Eng C Mater Biol Appl 98:1294–1305. https://doi.org/10.1016/j.msec.2019.01.062
Hafezeqoran A, Koodaryan R (2017) Effect of zirconia dental implant surfaces on bone integration: a systematic review and meta-analysis. Biomed Res Int 2017:1–12. https://doi.org/10.1155/2017/9246721
Moritz T, Lenk R (2009) Ceramic injection moulding: a review of developments in production technology, materials and applications. Powder Inject Mould Int 3:23–34
Yang YS, Yen Chen C (2016) Effect of injection molding and sintering behaviors on Y-TZP dental implants. J Phys Chem Biophys 6. https://doi.org/10.4172/2161-0398.1000220
Kim H-K, Woo KM, Shon W-J et al (2015) Comparison of peri-implant bone formation around injection-molded and machined surface zirconia implants in rabbit tibiae. Dent Mater J 34:508–515. https://doi.org/10.4012/dmj.2015-024
Park Y-S, Chung S-H, Shon W-J (2013) Peri-implant bone formation and surface characteristics of rough surface zirconia implants manufactured by powder injection molding technique in rabbit tibiae. Clin Oral Impl Res 24:586–591. https://doi.org/10.1111/j.1600-0501.2012.02468.x
Gahlert M, Röhling S, Wieland M, Sprecher CM, Kniha H, Milz S (2009) Osseointegration of zirconia and titanium dental implants: a histological and histomorphometrical study in the maxilla of pigs. Clin Oral Implants Res 20:1247–1253. https://doi.org/10.1111/j.1600-0501.2009.01734.x
Aboushelib MN, Salem NA, Taleb ALA, El Moniem NMA (2013) Influence of surface nano-roughness on osseointegration of zirconia implants in rabbit femur heads using selective infiltration etching technique. J Oral Implantol 39:583–590. https://doi.org/10.1563/AAID-JOI-D-11-00075
Chung SH, Kim H-K, Shon W-J, Park Y-S (2013) Peri-implant bone formations around (Ti,Zr)O2-coated zirconia implants with different surface roughness. J Clin Periodontol 40:404–411. https://doi.org/10.1111/jcpe.12073
Wilson TG, Miller RJ, Trushkowsky R, Dard M (2016) Tapered implants in dentistry: revitalizing concepts with technology: a review. Adv Dent Res 28:4–9. https://doi.org/10.1177/0022034516628868
Pippenger BE, Rottmar M, Kopf BS, Stübinger S, Dalla Torre FH, Berner S, Maniura-Weber K (2019) Surface modification of ultrafine-grained titanium: influence on mechanical properties, cytocompatibility, and osseointegration potential. Clin Oral Impl Res 30:99–110. https://doi.org/10.1111/clr.13396
Benlidayi ME, Gaggl A, Bürger H, Brandner C, Kurkcu M, Ünlügenç H (2011) Comparative study of the osseointegration of dental implants after different bone augmentation techniques: vascularized femur flap, non-vascularized femur graft and mandibular bone graft. Clin Oral Implants Res 22:594–599. https://doi.org/10.1111/j.1600-0501.2010.02013.x
Fuerst G, Gruber R, Tangl S et al (2003) Enhanced bone-to-implant contact by platelet-released growth factors in mandibular cortical bone: a histomorphometric study in minipigs. Int J Oral Maxillofac Implants 18:685–690
Kwon Y-S, Namgoong H, Kim J-H, Cho IH, Kim MD, Eom TG, Koo KT (2013) Effect of microthreads on removal torque and bone-to-implant contact: an experimental study in miniature pigs. J Periodontal Implant Sci 43:41–46. https://doi.org/10.5051/jpis.2013.43.1.41
Meng H-W, Chien EY, Chien H-H (2016) Dental implant bioactive surface modifications and their effects on osseointegration: a review. Biomark Res 4:24. https://doi.org/10.1186/s40364-016-0078-z
Mardas N, Dereka X, Donos N, Dard M (2014) Experimental model for bone regeneration in oral and cranio-maxillo-facial surgery. J Investig Surg 27:32–49. https://doi.org/10.3109/08941939.2013.817628
Berardini M, Trisi P, Sinjari B, Rutjes AWS, Caputi S (2016) The effects of high insertion torque versus low insertion torque on marginal bone resorption and implant failure rates: a systematic review with meta-analyses. Implant Dent 25:532–540. https://doi.org/10.1097/ID.0000000000000422
Trisi P, Todisco M, Consolo U, Travaglini D (2011) High versus low implant insertion torque: a histologic, histomorphometric, and biomechanical study in the sheep mandible. Int J Oral Maxillofac Implants 26:837–849
Ikar M, Grobecker-Karl T, Karl M, Steiner C (2020) Mechanical stress during implant surgery and its effects on marginal bone: a literature review. Quintessence Int 51(2):142–150.
Buser D, Nydegger T, Oxland T, Cochran DL, Schenk RK, Hirt HP, Snétivy D, Nolte LP (1999) Interface shear strength of titanium implants with a sandblasted and acid-etched surface: a biomechanical study in the maxilla of miniature pigs. J Biomed Mater Res 45(2):75–83
dos Santos MV, Elias CN, Cavalcanti Lima JH (2011) The effects of superficial roughness and design on the primary stability of dental implants: primary stability of dental implant. Clin Implant Dent Relat Res 13:215–223. https://doi.org/10.1111/j.1708-8208.2009.00202.x
Tabassum A, Meijer GJ, Wolke JGC, Jansen JA (2009) Influence of the surgical technique and surface roughness on the primary stability of an implant in artificial bone with a density equivalent to maxillary bone: a laboratory study. Clin Oral Implants Res 20:327–332. https://doi.org/10.1111/j.1600-0501.2008.01692.x
Manzano G, Herrero LR, Montero J (2014) Comparison of clinical performance of zirconia implants and titanium implants in animal models: a systematic review. Int J Oral Maxillofac Implants 29:311–320. https://doi.org/10.11607/jomi.2817
Wennerberg A, Albrektsson T, Andersson B, Krol JJ (1995) A histomorphometric and removal torque study of screw-shaped titanium implants with three different surface topographies. Clin Oral Implants Res 6:24–30. https://doi.org/10.1034/j.1600-0501.1995.060103.x
Palmquist A, Omar OM, Esposito M, Lausmaa J, Thomsen P (2010) Titanium oral implants: surface characteristics, interface biology and clinical outcome. J R Soc Interface 7. https://doi.org/10.1098/rsif.2010.0118.focus
Roehling S, Astasov-Frauenhoffer M, Hauser-Gerspach I, Braissant O, Woelfler H, Waltimo T, Kniha H, Gahlert M (2017) In vitro biofilm formation on titanium and zirconia implant surfaces. J Periodontol 88:298–307. https://doi.org/10.1902/jop.2016.160245
Gahlert M, Roehling S, Sprecher CM, Kniha H, Milz S, Bormann K (2012) In vivo performance of zirconia and titanium implants: a histomorphometric study in mini pig maxillae: in vivo performance of zirconia and titanium implants. Clin Oral Impl Res 23:281–286. https://doi.org/10.1111/j.1600-0501.2011.02157.x
Rupp F, Scheideler L, Olshanska N, de Wild M, Wieland M, Geis-Gerstorfer J (2006) Enhancing surface free energy and hydrophilicity through chemical modification of microstructured titanium implant surfaces. J Biomed Mater Res A 76:323–334. https://doi.org/10.1002/jbm.a.30518
Buser D, Broggini N, Wieland M, Schenk RK, Denzer AJ, Cochran DL, Hoffmann B, Lussi A, Steinemann SG (2004) Enhanced bone apposition to a chemically modified SLA titanium surface. J Dent Res 83:529–533. https://doi.org/10.1177/154405910408300704
Acknowledgments
The authors would like to thank Letitia Grace from the Swiss Tropical Institute (Basel) for the support of the statistical analysis and Novonexile AG (Switzerland) for the writing assistance and editorial support in the preparation of the manuscript.
Funding
This research was financially supported by Neodent and Straumann. Neodent is a daughter company of Straumann. This work may potentially lead to the development of products, in which Neodent and Straumann may have a business and/or financial interest. Neodent and Straumann therefore may be affected by the research reported in the enclosed paper.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr. Geninho Thomé declares that he is an employee of Neodent. Mrs. Rebecca Sandgren declares that she has no conflict of interest. Dr. Sergio Bernardes declares that he is an employee of Neodent. Dr. Larissa Trojan declares that she is an employee of Neodent. Dr. Nils Warfving declares that he has no conflict of interest. Dr. Benjamin Pippenger declares that he is an employee of Straumann. Mr. Benjamin Bellón declares that he is an employee of Straumann.
Ethical approval
This article does not contain any studies with human participants performed by any of the authors. Ethical standards related to the research of human subjects are not applicable. All applicable international, national, and/or institutional guidelines for the care and use of animals were followed. This study was conducted at the Biomedical Department of Lund University (Sweden) and approved by the local ethics committee of the university (M-192-14). The study was conducted in accordance with ISO 10993-6 “Biological evaluation of medical devices – Part 6 Tests for local effects after implantation guideline and recommendations.” This study adheres to the ARRIVE guidelines.
Informed consent
For this type of study, formal consent is not required.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 3470 kb)
Rights and permissions
About this article
Cite this article
Thomé, G., Sandgren, R., Bernardes, S. et al. Osseointegration of a novel injection molded 2-piece ceramic dental implant: a study in minipigs. Clin Oral Invest 25, 603–615 (2021). https://doi.org/10.1007/s00784-020-03513-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-020-03513-z