Abstract
Objective
This retrospective study aimed to compare the occlusal and dentoskeletal initial features of patients treated with four first premolar extractions in the 1970s and after 2000.
Materials and methods
Group 70′ was composed by 30 subjects with Class I malocclusion (mean age of 12.8 years, 10 male, 20 female) treated in the 1970s with four first premolar extractions and comprehensive orthodontic treatment. Group NM comprised 30 subjects with Class I malocclusion (mean age of 13.4 years, 13 male, 17 female) treated in the new millennium, similarly to Group 70′. Initial dental models and lateral cephalograms were digitized and measured using OrthoAnalyzerTM 3D software and Dolphin Imaging 11.0 software, respectively. Initial occlusal and dentoskeletal features were analyzed and compared. Intergroup comparison was performed using t tests (p < 0.05). Holm-Bonferroni correction for multiple comparison was applied.
Results
Group NM showed significantly greater maxillary and mandibular effective lengths and greater maxillary and mandibular incisor protrusion in comparison with Group 70′. Group NM presented a significantly greater lower anterior facial height. Group NM also showed significantly smaller nasolabial angle and protruded inferior lip.
Conclusion
Patients with Class I malocclusion treated with four first premolar extractions in the new millennium present a greater degree of dental and labial protrusion, increased lower anterior facial height, and more acute nasolabial angle compared with patients treated similarly in the 1970s. Greater dental and labial protrusion determines first premolar extractions in the new millennium.
Clinical relevance
Despite the decrease of tooth extraction frequency, four first premolar extractions may be justified in cases with severe dental and skeletal protrusions.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Orthodontics has confronted an extraction vs nonextraction debate in the last hundred years [1,2,3,4,5,6], which is still ongoing in the twenty-first century [6]. In the beginning of the XX century, Angle proposed nonextraction orthodontic interventions, which were accepted and almost not questioned for over 30 years [5]. However, concerns regarding treatment stability [4] and dental protrusion associated with unsatisfactory facial esthetics [1, 2] reintroduced tooth extraction in the orthodontic field. Extraction treatment had such a great impact in the 1960s, 1970s, and 1980s that more than half of patients presented some tooth removed for orthodontic purposes [7, 8]. Nevertheless, a decrease in tooth extraction frequency was observed subsequently, especially in the new millennium [7,8,9].
The decrease of tooth extraction frequency had multifactorial reasons. Excessive incisor uprighting showed a detrimental effect on facial esthetics, leading to a more flattened profile [10,11,12,13]. In the second half of the XX century, changes in the perception of an ideal facial esthetics were observed toward a fuller and more protruded dentofacial profile [14, 15]. Additionally, extraction cases showed similar treatment stability compared with nonextraction treatments [16, 17]. The development of orthopedic treatments [18, 19], two-phase interventions [20, 21], interproximal tooth reduction [22, 23], and concerns with temporomandibular disorders [24, 25] also had an influence in the frequency decrease of tooth extraction. Complexity of orthodontic mechanics [26], prolonged treatment time [27], space reopening [28], and an increased degree of external root resorption [29] were also concerns in extraction treatments.
In Class I malocclusion patients, extractions are frequently used in cases with dentoalveolar protrusion and moderate-to-severe crowding [27, 30]. Facial esthetics, labial protrusion, overjet, and overbite are also considered [9, 27, 30]. In the 1970s, the frequency of four first premolar extraction cases started to decrease [7, 8]. At the 1990s, the frequency of extractions was approximately 10%. In the new millennium, frequency of first premolar extraction ranges from 9 to 16% [8, 9].
No previous study has directly compared facial and occlusal initial morphology of Class I patients treated with premolar extractions in the past and currently. Understanding trend changes overtime might support treatment plan decisions and professional confidence. Therefore, the purpose of this study was to compare the initial dentoskeletal features of patients treated with four first premolar extractions in the 1970s and in the New Millennium. The null hypothesis is that subjects treated with extraction in the 1970s and in the new millennium have similar initial features.
Materials and methods
This retrospective study was approved by the institutional Research Ethics Committee of Bauru Dental School, University of São Paulo (process #71638417.9.0000.5417). The primary outcome was dental crowding. Sample size calculation was based on a standard deviation for maxillary irregularity index of 2.6 [31], a minimum intergroup difference of 2 mm, an alpha value of 5%, and a statistical power of 80%. The sample size for each group was 28 subjects.
The sample was selected from the orthodontic records of patients treated between 1973 to 1979 and 2000 to 2013 in the Orthodontic Department of Bauru Dental School, University of São Paulo. Patients’ records were organized in a crescent order according to the initial exam date. The inclusion criteria were (1) Class I malocclusion treated with four first premolar extractions, (2) complete and adequate initial records, (3) permanent dentition, and (4) absence of tooth agenesis. Exclusion criteria were (1) patients with history of previous orthodontic treatment and (2) craniofacial anomalies. In the 1970s decade, the frequency of extraction was 54.29%. After the year 2000, the frequency of extractions was 7.47%. In order to address potential bias, Group 70′ selection was performed following this order, evaluating the records from the first case treated in 1973 until the 30th case that met the inclusion criteria. Group NM was selected following the same order, starting with the first patient treated in 2000 until the 30th case that met the inclusion criteria.
Group 70′ was composed by 30 patients (10 male; 20 female) with an initial mean age of 12.8 years (SD = 1.17) treated between 1973 and 1979. In the ages 70′, the decision for extraction was driven predominantly by dental models and cephalometric analysis. Group NM comprised 30 patients (13 male; 17 female) with an initial mean age of 13.4 years (SD = 1.33) treated between 2000 and 2013. After 2000, the decision for extraction was driven by dental models and facial analysis, using the cephalometric analysis as a complementary diagnostic method.
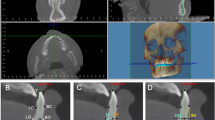
Dental models and lateral cephalograms were used, and all dental models and cephalometric analysis were performed in random order within the same group, so risk of bias was reduced. Initial dental models were digitized using 3D 3Shape R700 scanner (3Shape A/S, Copenhagen, Denmark) and analyzed with OrthoAnalyzerTM 3D software (3Shape A/S, Copenhagen, Denmark). The initial lateral cephalograms were digitized using the Microtek ScanMaker i800 scanner (Santa Fe Springs, CA, USA) and analyzed with Dolphin® 11.5 imaging software (Chatsworth, CA, USA). Magnification factors were corrected according to the cephalostat used in each period, with 6% and 9% (for Group 70′ and NM, respectively). The evaluated cephalometric variables are shown in Figs. 1 and 2.
Both maxillary and mandibular digital dental models were initially oriented with the occlusal plane parallel to the horizontal plane (Fig. 3). The maxillary occlusal plane passed through the mesiopalatal cusp tip of the permanent first molars, bilaterally, and through the mesio-incisal angle of the right central incisor (Fig. 3a). The mandibular occlusal plane passed through the distobuccal cusp tip of the permanent first molars, bilaterally, and through the mesio-incisal angle of the right central incisor (Fig. 3b). The incisor irregularity index [32] was measured on the occlusal view of the digital dental models. The PAR index [33] was evaluated using the physical dental models of each patient.
Error study
All dental model and cephalometric variables were measured twice in 50% of the sample randomly selected after a minimum 30-day interval by one examiner (RN). The intraexaminer reliability was assessed using intraclass correlation coefficient (ICC) [34]; random errors were estimated using Dahlberg’s formula [35] while the systematic errors were calculated with dependent t tests, at P < 0.05.
Statistical analyses
The variables distribution was verified by the Kolmogorov-Smirnov test. Intergroup comparisons were performed with t tests for normally distributed variables and with Mann-Whitney tests for not normally distributed variables, at P < 0.05. Holm-Bonferroni correction for multiple comparison was applied. Statistical analyses were performed using Statistica software (Statistica for Windows version 11.0; StatSoft Inc., Tulsa, OK).
Results
The ICC values varied from 0.849 to 0.989, showing excellent measurement reproducibility. The random errors ranged from 0.47 to 2.20 (maxillary irregularity index and PAR Index, respectively) for the dental model variables (Table 1). The random errors ranged from 0.35 mm to 1.34 mm (molar relationship and Co-A, respectively) for cephalometric linear variables and from 0.54 to 2.88 (ANB and nasolabial angle, respectively) for the angular measurements. No significant systematic errors were found.
The groups were comparable regarding initial age and sex distribution (Table 2).
The dental model analysis showed similar dental crowding and similar initial occlusal malocclusion severity in both groups (Table 3).
Group NM presented significantly greater maxillary and mandibular effective lengths and labial tipping and protrusion of the maxillary and mandibular incisors than Group 70′ (Table 3). Group NM presented significantly greater lower anterior facial height in comparison with Group 70′.
Group NM also displayed significantly smaller nasolabial angle and more protruded lower lip than Group 70′ (Table 3).
Discussion
Accuracy and reproducibility of cephalometric and digital dental model analysis are well documented [36]. Digital lateral cephalograms and dental models have been widely used in orthodontic research [36,37,38]. Our study showed adequate reproducibility within acceptable limits, corroborating previous studies [30, 39,40,41] (Table 1).
Class I malocclusion associated with dental crowding is commonly seen in the orthodontic practice [42], and crowding severity is considered a determinant factor in extraction decision [30]. Previous studies reported low self-esteem associated with severe crowding [43]. In this study, no intergroup differences were found for the initial amount of maxillary and mandibular crowding (Table 3). Both groups showed moderate-to-severe initial dental crowding. Initial occlusal malocclusion severity can also determine the need for tooth extraction. The greater the occlusal malocclusion severity, the greater the probability that tooth extraction will be needed [44]. In this study, both groups presented similar initial occlusal malocclusion severities. Therefore, over the last 30 years, no differences were found for severity of both anterior dental crowding and initial occlusal malocclusion severity in patients treated with four premolar extractions.
Greater maxillary and mandibular effective lengths and dental protrusion was found in patients treated with extractions in the new millennium in comparison with patients treated in the past (Table 3, Figs. 4 and 5). These results corroborate previous studies that indicated four first premolar extractions when an important biprotrusion was present, reporting straightening and improvement of the facial profile [10, 11, 27, 45]. Esthetic evaluation associated low self-esteem with severe protrusion [43] and showed that straight profiles have been considered the most attractive [46,47,48]. Despite the modern esthetic trend toward a fuller and protrusive profile [14, 15], severe biprotrusion and excessive convex profiles are considered to impair facial esthetics [47, 48]. In other words, in the new millennium four premolar extractions were performed in more biprotrusive patients. Conversely, in the 1970s decade, four premolar extractions were performed even when a slight degree of incisor protrusion was present, probably, more often leading to a flattened facial profile. Development of skeletal anchorage devices facilitated treatment of patients with straight profiles indicated to four first premolar extractions, allowing anchorage loss in order to maintain an esthetic facial profile [49, 50].
No intergroup differences in facial growth pattern were found (Table 3). Both groups showed a predominant hyperdivergent growth pattern. These findings were expected considering that previous studies have indicated four first premolar extractions in patients with hyperdivergent pattern [51,52,53]. Control of the vertical dimension was thought to occur by counterclockwise rotation of the mandible, through forward movement of the posterior teeth [51,52,53]. Greater increase in LAFH has been observed after nonextraction than in extraction treatment [51, 54, 55]. Our results are in accordance with indication of four first premolar extractions predominantly in a hyperdivergent pattern, both in the 1970s and in the new millennium. Group NM showed increased LAFH compared with Group 70′ (Table 3). This may be explained by the greater effective maxillary and mandibular lengths observed in group NM.
The soft tissue evaluation showed more acute nasolabial angle and more protruded lower lip in Group NM compared with Group 70′ (Table 3, Figs. 4 and 5). These differences reflect the abovementioned greater dental protrusion in group NM. Soft tissue features have been considered a determinant factor for extraction decision [27, 30, 45]. Recent studies have indicated four first premolar extractions in patients with increased lip prominence [27, 30]. Premolar extractions, followed by anterior retraction, lead to more pleasing profiles in patients with protruded lips [30, 56]. Lip response to anterior teeth retraction shows great variance and depends on inherent characteristics of each individual as ethnic background, lip thickness and quality of the lip musculature [52, 56]. On other hand, in borderline patients, premolar extractions have not compromised the facial profile [57]. Lip retraction is expected in borderline patients after extraction; however, these changes are small and considered clinically irrelevant [57]. Despite the variance of lip-to-incisor-retraction correlation [56], improvement of the facial profile in biprotrusive patients is expected after four first premolar extractions [27, 56].
In summary, four premolar extractions are currently indicated in cases coupling severe dental crowding, significant incisor/lip protrusion, and predominant vertical growth pattern. In the past, a great number of extractions were performed in cases with mild degrees of mandibular incisor protrusion, just to fit a given cephalometric pattern [2, 58,59,60]. These evolutional trends are in consonance with the facial profile preferences and the decrease of tooth extractions over the last decades [7,8,9, 12,13,14,15, 27].
Limitations
Because of the limitations of having a sample composed by patients treated in a single center, future studies should consider multicenter patients in order to confirm these tendencies.
Conclusions
The null hypothesis was rejected because patients with Class I malocclusion treated with four first premolar extractions in the new millennium present the following:
-
A significantly greater dental and labial protrusion
-
A significantly greater lower anterior facial height and smaller nasolabial angle compared with patients treated in the 1970s
References
Tweed CH (1944) Indications for the extraction of teeth in orthodontic procedure. Am J Orthodont Oral Surg 30(8):405–428
Tweed CH (1945) A philosophy of orthodontic treatment. Am J Orthodont Oral Surg 31(2):74–103
Weintraub JA, Vig PS, Brown C, Kowalski CJ (1989) The prevalence of orthodontic extractions. Am J Orthodont Dentofac Orthop 96(6):462–466
Lundström AF (1925) Malocclusion of the teeth regarded as a problem in connection with the apical base. Int J Orthodont Oral Surg Radiogr 11(12):1109–1133
Angle EH (1907) Treatment of malocclusion of the teeth: Angle's system. White Dental Manufacturing Company
Peck S (2017) Extractions, retention and stability: the search for orthodontic truth. Eur J Orthod 39(2):109–115. https://doi.org/10.1093/ejo/cjx004
Proffit WR (1994) Forty-year review of extraction frequencies at a university orthodontic clinic. Angle Orthodont 64(6):407–414. https://doi.org/10.1043/0003-3219(1994)064<0407:FROEFA>2.0.CO;2
Janson G, Maria FR, Bombonatti R (2014) Frequency evaluation of different extraction protocols in orthodontic treatment during 35 years. Prog Orthod 15:51. https://doi.org/10.1186/s40510-014-0051-z
Jackson TH, Guez C, Lin FC, Proffit WR, Ko CC (2017) Extraction frequencies at a university orthodontic clinic in the 21st century: demographic and diagnostic factors affecting the likelihood of extraction. Am J Orthodont Dentofac Orthop 151(3):456–462. https://doi.org/10.1016/j.ajodo.2016.08.021
Drobocky OB, Smith RJ (1989) Changes in facial profile during orthodontic treatment with extraction of four first premolars. Am J Orthodont Dentofac Orthop 95(3):220–230
Bravo LA (1994) Soft tissue facial profile changes after orthodontic treatment with four premolars extracted. Angle Orthodont 64(1):31–42. https://doi.org/10.1043/0003-3219(1994)064<0031:STFPCA>2.0.CO;2
Holdaway RA (1983) A soft-tissue cephalometric analysis and its use in orthodontic treatment planning. Part I. Am J Orthodont 84(1):1–28
Holdaway RA (1984) A soft-tissue cephalometric analysis and its use in orthodontic treatment planning. Part II. Am J Orthodont 85(4):279–293
Peck H, Peck S (1970) A concept of facial esthetics. Angle Orthodont 40(4):284–318. https://doi.org/10.1043/0003-3219(1970)040<0284:ACOFE>2.0.CO;2
Auger TA, Turley PK (1999) The female soft tissue profile as presented in fashion magazines during the 1900s: a photographic analysis. Int J Adult Orthodont Orthogn Surg 14(1):7–18
Little RM (1990) Stability and relapse of dental arch alignment. Br J Orthod 17(3):235–241
Little RM, Wallen TR, Riedel RA (1981) Stability and relapse of mandibular anterior alignment-first premolar extraction cases treated by traditional edgewise orthodontics. Am J Orthod 80(4):349–365
Frankel R (1974) Decrowding during eruption under the screening influence of vestibular shields. Am J Orthod 65(4):372–406
Haas AJ (1970) Palatal expansion: just the beginning of dentofacial orthopedics. Am J Orthod 57(3):219–255
Cancado RH, Pinzan A, Janson G, Henriques JF, Neves LS, Canuto CE (2008) Occlusal outcomes and efficiency of 1- and 2-phase protocols in the treatment of class II division 1 malocclusion. Am J Orthodont Dentofac Orthop 133(2):245–253; quiz 328 e241-242. https://doi.org/10.1016/j.ajodo.2006.03.042
O'Brien K, Wright J, Conboy F, Sanjie Y, Mandall N, Chadwick S, Connolly I, Cook P, Birnie D, Hammond M, Harradine N, Lewis D, McDade C, Mitchell L, Murray A, O'Neill J, Read M, Robinson S, Roberts-Harry D, Sandler J, Shaw I (2003) Effectiveness of early orthodontic treatment with the twin-block appliance: a multicenter, randomized, controlled trial. Part 1: dental and skeletal effects. Am J Orthodont Dentofac Orthop 124(3):234–243; quiz 339. https://doi.org/10.1016/S0889540603003524
Sheridan JJ (1987) Air-rotor stripping update. J Clin Orthodont 21(11):781–788
Sheridan JJ, Hastings J (1992) Air-rotor stripping and lower incisor extraction treatment. J Clin Orthodont 26(1):18–22
Luecke PE 3rd, Johnston LE Jr (1992) The effect of maxillary first premolar extraction and incisor retraction on mandibular position: testing the central dogma of “functional orthodontics”. Am J Orthodont Dentofac Orthop 101(1):4–12. https://doi.org/10.1016/0889-5406(92)70075-L
McLaughlin RP, Bennett JC (1995) The extraction-nonextraction dilemma as it relates to TMD. Angle Orthodont 65(3):175–186. https://doi.org/10.1043/0003-3219(1995)065<0175:TEDAIR>2.0.CO;2
Alexander RG, Sinclair PM, Goates LJ (1986) Differential diagnosis and treatment planning for the adult nonsurgical orthodontic patient. Am J Orthod 89(2):95–112
Iared W, Koga da Silva EM, Iared W, Rufino Macedo C (2017) Esthetic perception of changes in facial profile resulting from orthodontic treatment with extraction of premolars: a systematic review. J Am Dent Assoc 148(1):9–16. https://doi.org/10.1016/j.adaj.2016.09.004
Garib DG, Bressane LB, Janson G, Gribel BF (2016) Stability of extraction space closure. Am J Orthodont Dentofac Orthop 149(1):24–30. https://doi.org/10.1016/j.ajodo.2015.06.019
Sameshima GT, Sinclair PM (2001) Predicting and preventing root resorption: part II. Treatment factors. Am J Orthodont Dentofac Orthop 119(5):511–515. https://doi.org/10.1067/mod.2001.113410
Konstantonis D, Anthopoulou C, Makou M (2013) Extraction decision and identification of treatment predictors in class I malocclusions. Prog Orthod 14:47. https://doi.org/10.1186/2196-1042-14-47
Guirro WJ, Freitas KM, Janson G, de Freitas MR, Quaglio CL (2016) Maxillary anterior alignment stability in class I and class II malocclusions treated with or without extraction. Angle Orthodont 86(1):3–9. https://doi.org/10.2319/112614-847.1
Little RM (1975) The irregularity index: a quantitative score of mandibular anterior alignment. Am J Orthod 68(5):554–563
Richmond S, Shaw WC, O'Brien KD, Buchanan IB, Jones R, Stephens CD, Roberts CT, Andrews M (1992) The development of the PAR index (peer assessment rating): reliability and validity. Eur J Orthod 14(2):125–139
Shrout PE, Fleiss JL (1979) Intraclass correlations: uses in assessing rater reliability. Psychol Bull 86(2):420–428. https://doi.org/10.1037//0033-2909.86.2.420
Dahlberg G (1949) Standard error and medicine. Acta Genet Stat Med 1(4):313–321
Saleh WK, Ariffin E, Sherriff M, Bister D (2015) Accuracy and reproducibility of linear measurements of resin, plaster, digital and printed study-models. J Orthod 42(4):301–306. https://doi.org/10.1179/1465313315Y.0000000016
Farooq MU, Khan MA, Imran S, Sameera A, Qureshi A, Ahmed SA, Kumar S, Rahman MA (2016) Assessing the reliability of digitalized cephalometric analysis in comparison with manual cephalometric analysis. J Clin Diagn Res 10(10):ZC20–ZC23. https://doi.org/10.7860/JCDR/2016/17735.8636
Mayers M, Firestone AR, Rashid R, Vig KW (2005) Comparison of peer assessment rating (PAR) index scores of plaster and computer-based digital models. Am J Orthodont Dentofac Orthop 128(4):431–434. https://doi.org/10.1016/j.ajodo.2004.04.035
Zablocki HL, McNamara JA Jr, Franchi L, Baccetti T (2008) Effect of the transpalatal arch during extraction treatment. Am J Orthodont Dentofac Orthop 133(6):852–860. https://doi.org/10.1016/j.ajodo.2006.07.031
Anthopoulou C, Konstantonis D, Makou M (2014) Treatment outcomes after extraction and nonextraction treatment evaluated with the American Board of Orthodontics objective grading system. Am J Orthodont Dentofac Orthop 146(6):717–723. https://doi.org/10.1016/j.ajodo.2014.07.025
Freitas KM, Freitas DS, Valarelli FP, Freitas MR, Janson G (2008) PAR evaluation of treated class I extraction patients. Angle Orthodont 78(2):270–274. https://doi.org/10.2319/042307-206.1
Sayin MO, Turkkahraman H (2004) Malocclusion and crowding in an orthodontically referred Turkish population. Angle Orthodont 74(5):635–639. https://doi.org/10.1043/0003-3219(2004)074<0635:MACIAO>2.0.CO;2
Jung MH (2015) An evaluation of self-esteem and quality of life in orthodontic patients: effects of crowding and protrusion. Angle Orthodont 85(5):812–819. https://doi.org/10.2319/091814.1
Kamal AT, Shaikh A, Fida M (2016) Occlusal outcome of non-extraction and all first premolars extraction treatment in patients with class-I malocclusion. J Ayub Med Coll Abbottabad 28(4):664–668
Bowman SJ, Johnston LE Jr (2000) The esthetic impact of extraction and nonextraction treatments on Caucasian patients. Angle Orthodont 70(1):3–10. https://doi.org/10.1043/0003-3219(2000)070<0003:TEIOEA>2.0.CO;2
Czarnecki ST, Nanda RS, Currier GF (1993) Perceptions of a balanced facial profile. Am J Orthodont Dentofac Orthop 104(2):180–187. https://doi.org/10.1016/S0889-5406(05)81008-X
Mees S, Jimenez Bellinga R, Mommaerts MY, De Pauw GA (2013) Preferences of AP position of the straight Caucasian facial profile. J Craniomaxillofac Surg 41(8):755–763. https://doi.org/10.1016/j.jcms.2013.01.014
Moresca R (2014) Class I malocclusion with severe double protrusion treated with first premolars extraction. Dent Press J Orthodont 19(3):127–138
Gollner N, Winkler J, Gollner P, Gkantidis N (2019) Effect of mandibular first molar mesialization on alveolar bone height: a split mouth study. Prog Orthod 20(1):22. https://doi.org/10.1186/s40510-019-0275-z
Marusamy KO, Ramasamy S, Wali O (2018) Molar protraction using miniscrews (temporary anchorage device) with simultaneous correction of lateral crossbite: an orthodontic case report. J Int Soc Prevent Commun Dent 8(3):271–276. https://doi.org/10.4103/jispcd.JISPCD_447_17
Beit P, Konstantonis D, Papagiannis A, Eliades T (2017) Vertical skeletal changes after extraction and non-extraction treatment in matched class I patients identified by a discriminant analysis: cephalometric appraisal and Procrustes superimposition. Prog Orthod 18(1):44. https://doi.org/10.1186/s40510-017-0198-5
Bills DA, Handelman CS, BeGole EA (2005) Bimaxillary dentoalveolar protrusion: traits and orthodontic correction. Angle Orthodont 75(3):333–339. https://doi.org/10.1043/0003-3219(2005)75[333:BDPTAO]2.0.CO;2
Pearson LE (1978) Vertical control in treatment of patients having backward-rotational growth tendencies. Angle Orthodont 48(2):132–140. https://doi.org/10.1043/0003-3219(1978)048<0132:VCITOP>2.0.CO;2
Kocadereli I (1999) The effect of first premolar extraction on vertical dimension. Am J Orthodont Dentofac Orthop 116(1):41–45
Kumari M, Fida M (2010) Vertical facial and dental arch dimensional changes in extraction vs. non-extraction orthodontic treatment. J Coll Phys Surg--Pakista 20(1):17–21. https://doi.org/10.2010/JCPSP.1721
Sundareswaran S, Vijayan R (2017) Profile changes following orthodontic treatment of class I bimaxillary protrusion in adult patients of Dravidian ethnicity: a prospective study. Indian J Dent Res 28(5):530–537. https://doi.org/10.4103/ijdr.IJDR_549_15
Kirschneck C, Proff P, Reicheneder C, Lippold C (2016) Short-term effects of systematic premolar extraction on lip profile, vertical dimension and cephalometric parameters in borderline patients for extraction therapy--a retrospective cohort study. Clin Oral Investig 20(4):865–874. https://doi.org/10.1007/s00784-015-1574-5
Steiner CC (1960) The use of cephalometrics as an aid to planning and assessing orthodontic treatment: report of a case. Am J Orthod Dentofac Orthop 46(10):721–735
Tweed CH (1946) The Frankfort-mandibular plane angle in orthodontic diagnosis, classification, treatment planning, and prognosis. Am J Orthodont Oral Surg 32(4):175–230
Wahl N (2006) Orthodontics in 3 millennia. Chapter 8: the cephalometer takes its place in the orthodontic armamentarium. Am J Orthodont Dentofac Orthop 129(4):574–580. https://doi.org/10.1016/j.ajodo.2006.01.013
Acknowledgments
The authors would like to thank the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior - Brasil (CAPES) - Finance Code 001.
Funding
This study was financially supported by the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior - (CAPES) - Finance Code 001.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
In this article, all procedures involving human participants were in accordance with the ethical standards of the Research Ethics Committee of Bauru Dental Scooll, University of São Paulo (#71638417.9.0000.5417).
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is based on research submitted by Dr. Rodrigo Naveda in partial fulfillment of the requirements for the M.Sc. degree in Orthodontics at Bauru Dental School, University of São Paulo.
Rights and permissions
About this article
Cite this article
Naveda, R., Janson, G., Natsumeda, G.M. et al. Pretreatment dentoskeletal comparison between individuals treated with extractions in the 1970s and in the new millennium. Clin Oral Invest 25, 1997–2005 (2021). https://doi.org/10.1007/s00784-020-03508-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-020-03508-w