Abstract
Objectives
The aim of this study was to evaluate the accuracy of cone beam computed tomography (CBCT), periapical radiograph, and intrasurgical linear measurements in the assessment of molars with furcation defects.
Materials and methods
This parallel, single-blinded, randomised controlled trial (RCT) consisted of 22 periodontitis patients who had molar with advanced furcation involvement (FI). All patients followed the same inclusion criteria and were treated following the same protocol, except for radiographic evaluation (CBCT vs. periapical). This study proposed and evaluated five parameters that represent the extent and severity of furcation defects in molars teeth, including CEJ-BD (clinical attachment loss), BL-H (depth), BL-V (height), RT (root trunk), and FW (width).
Results
There were no statistically significant differences between CBCT and intrasurgical linear measurements for any clinical parameter (p > 0.05). However, there were statistically significant differences in BL-V measurements (p < 0.05) between periapical and intrasurgical measurements in maxillary molars. Meanwhile, the sensitivity were 62.8% and 56.9% for CBCT and periapical, respectively.
Conclusions
Overall, when compared to the intrasurgical measurements, CBCT provided better diagnostic, sensitivity, and quantitative information on CAL, height, depth, and width of the furcation defects than periapical radiograph.
Clinical relevance
An accurate presurgical furcation diagnostic can guide the clinicians from the stage of diagnosis to definitive management so that unnecessary periodontal surgical interventions can be prevented.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Furcation lesion or defect was defined as ‘the pathologic resorption of bone in the anatomic area of a multirooted tooth where the roots diverge’ [1]. Previous studies have concluded that the diagnosis of furcation involvement (FI) can be assessed based on probing pocket depth (PPD), clinical attachment level (CAL), and furcation entrance (FE) by using periodontal probe and Naber’s probe [2,3,4,5]. However, it may be difficult to accurately assess, diagnose, and treat a molar with furcation defects due to anatomical and morphological variations. Thus, additional diagnostic procedures such as radiographic investigations are necessary to assist clinicians, especially periodontists, in the decision-making process concerning management plan from diagnosis to definitive treatment [6].
Conventionally, the standard diagnostic imaging techniques used to supplement clinical assessment of furcation included periapical radiograph [7,8,9]. In recent studies, it was reported that cone beam computed tomography (CBCT) improved the diagnostic accuracy in detecting molar with FI and measuring the furcation defects. Thus, CBCT has been suggested as an adjunct assessment tool for FI [3, 10, 11].
To date, only few clinical studies have compared the CBCT and intrasurgical measurements in assessing furcation defects [12,13,14]. However, none of these studies had compared the linear measurement of the furcation defects with sample randomisation between periapical and CBCT against the intrasurgical measurements. Instead, the researchers performed two imaging modalities, i.e. periapical and CBCT on the same furcation defects to evaluate the accuracy of each type of radiograph [15, 16]. In this study, linear measurement refers to the measurement of a straight distance between two points or a dimensional reference such as height, width, and depth of furcation defects. Therefore, the aim of this study was to evaluate the accuracy of linear measurements between periapical radiograph, CBCT, and intrasurgical in molars with furcation defects.
Materials and methods
Study population
This parallel, single-blinded, randomised controlled trial (RCT) has received approval from the Ethical Committee of Universiti Teknologi MARA (REC/295/17) and registered with the Identification of Randomised Controlled Clinical Trials worldwide registry (ISRCTN89375372). This study was conducted following the ICH Good Clinical Practice Guidelines, Malaysia Good Clinical Practice Guidelines, and the Declaration of Helsinki and internationally accepted guidelines for RCT, including the CONSORT statement (www.consort-statement.org). This study was performed between September 2017 and June 2019 at the Periodontic Clinic, Faculty of Dentistry, Universiti Teknologi MARA (UiTM) Sungai Buloh Campus, Selangor, Malaysia.
Twenty-two patients (13 men and 9 women) between the ages 29 and 64 were enrolled in the study. At the beginning of the study, all patients were informed in detail about the objectives of the investigation, radiation risks, benefits of the treatment, and the flow of the treatments. All patients who were willing to participate in this study were asked to sign an informed consent form. An impression with alginate was taken for all participated patients to prepare individual custom occlusal stent.
Purposive sampling technique, a type of non-probability sampling, was chosen to select patients who fulfilled all the inclusion and exclusion criteria to participate in the study. The patients must have been diagnosed with periodontitis stage III or IV according to American Academy of Periodontology (AAP) 2017 classification [17] and abled to sit for all required radiographic surveys and periodontal therapies. Non-surgical periodontal therapy included oral hygiene instruction, scaling, and root debridement was performed at least 8 weeks to 3 months prior study inclusion. Re-evaluations of the periodontal conditions were regularly performed. The patients must have at least one identifiable cementoenamel junction (CEJ) of molar with FI Class II or III [18] with probing pocket depth (PPD) of ≥ 6 mm that is indicated for periodontal surgery with full mouth plaque score (FMPS) [19] and full mouth bleeding score (FMBS) ≤ 15% [20].
Patients with uncontrolled systemic disease, smoker, pregnant, and lactating women, molar with FI that is indicated for extraction, or furcation caries, or metal crowns in the furcation area or silver amalgam fillings near the alveolar crest, and third molars, were excluded from the study.
Randomisation, allocation concealment, and blinding
Block randomisation and allocation concealment of patients were performed using sequentially numbered, opaque sealed envelopes (SNOSE) [21]. Three blocks of 4 and two blocks of 6 were used to allocate equal participants to each group. In this single-blind trial, the clinician was blinded to the type of radiographic procedures.
Cone beam computed tomography measurements
Following the randomised group allocation, the CBCT image of the involved tooth was obtained using Carestream Dental® (CS 9000 3D Imaging System, Rochester, NY, USA). Based on the region of interest, field of view (FOV) of 5 × 3 cm, settings in the 78 kV, 10 mA, and voxel size of 0.076 × 0.076 × 0.076 mm were chosen. The slice thickness was standardised at 0.076 mm, and the acquisition time was 10.8 s.
Pre-operative CBCT image acquisition was performed at least 2 weeks prior to periodontal surgery. Subsequently, CBCT images were viewed under dimmed lighting with a ViewSonic 27.0, light-emitting diode, high-definition screen (1080 pixels) monitor and measurements were made to the nearest 0.1 mm using software with a specialised linear measurement tools and a digital magnification lens. The three axes (axial, sagittal, and coronal) of the CBCT images were analysed continuously. The linear measurements of the dimension of bone loss in the horizontal and vertical directions (BL-H, BL-V), clinical attachment level/loss (CAL), root trunk (RT), and furcation width (FW) were assessed with the CS 9000 3D proprietary software (Fig. 1). Table 1 shows the summary of the definition for each measurement.
Periapical radiograph measurements
Following the randomised group allocation, a digital radiograph of the periapical view of the tooth involved was acquired using long-cone paralleling techniques. The CMOS sensor (EzSensor, pixel size 35 μm, Vatech, Hwaseong, Korea) coupled to an intra-oral machine (Satelec X-mind AC/DC, Satelec ACTEON Tuusula, Finland) was used in this study. The obtained periapical radiograph was evaluated and measured on EasyDent V4® viewer software version 4.1.4.5 (Vatech, Hwaseong, Korea) in similar manner as the measurement parameters for CBCT, except for BL-H measurements (horizontal) (Fig. 2). Measurements were made to the nearest point of 0.1 mm with a linear measurement tool and a digital magnification lens with the same monitor used for CBCT measurements. The measurement was performed in a room with subdued lighting to enhance visibility and increase accuracy.
Intrasurgical measurements
The scheduled surgical treatment for the patients could be either an open flap debridement, regenerative procedure, or resection procedure. The decision would be made during the re-evaluation phase following initial periodontal therapy. Prior to surgery, the patient was asked to rinse his or her mouth with chlorhexidine 0.12% for 1 min. Then, local anaesthesia was administered at the selected site. Intrasulcular or paramarginal incision would be made, depending on the amount of keratinised tissue present, and a full-thickness flap would be raised. A thorough debridement with manual Gracey curettes and ultrasonic scaler was carried out. Once the furcation defects were visualised, they would be evaluated by trained calibrated examiners. Each defect was measured using a manual 15-mm periodontal probe (PCPUNC-15; Hu Friedy®). The defects were measured as same per the measurements performed in CBCT (CEJ-BD/CAL, BL-H, BL-V, RT, FW) (Table 1). Figure 3 shows the anatomical landmarks and the measurements used during furcation surgery.
The custom-made occlusal stent was placed prior to defects measurement. Each stent had prefabricated prominent vertical grooves to guide the periodontal probe placement. An endodontic stopper was inserted into the periodontal probe to obtain maximum accuracy in horizontal measurement due to limited access and view. Following the intrasurgical measurements, furcation defects were managed according to the treatment plan. Subsequently, the flap was sutured with 5/0 or 6/0 non-resorbable sutures. The patients were instructed to rinse with 0.12% chlorhexidine mouthwash twice a day for 1 min. The patients were reviewed 1 to 2 weeks after the surgery for post-operative assessment or suture removal, depending on the treatment received. The patients then scheduled for supportive periodontal treatment at 3- to 4-month intervals once the periodontal status was deemed stable.
Clinical and radiographic measurements of the investigators
All the clinical and radiographic parameters were performed by trained calibrated examiners (NAMY and EN for clinical and MYPMY and NHR for radiographic). To ensure inter-examiner reliability, all examiners performed the same steps. The measurements of the examiners were then compared. All examiners were blinded to each other’s measurement values. The intraclass correlation coefficient (ICC) was used to determine inter-examiner reproducibility which resulted as excellent levels of agreement (Table 2) [22].
Sample size determination
The sample size was calculated using the Power and Sample Size Program (PS version 3.1.2). It was calculated based on the mean difference between the 2D and 3D images in comparison with direct surgical measurements for the determination of periodontal bone loss, which derived from another published study [15]. A sample size of at least 10 subjects in each group (n = 10) will give a 90% probability of detecting a mean difference of δ = 0.15 mm between groups at a statistically significant level of alpha significance, α = 0.05. The number of patients in the present study was increased to 12 patients (20%) for each arm considering possible dropouts.
Statistical analysis
All collected data were organised and analysed using IBM SPSS® statistics Version 25. Descriptive statistics were used to describe the demographic data and distribution of molar teeth among the sample population. The primary outcome variables of this study were CEJ-BD, BL-H, BL-V, FW, and RT. As the data were not normally distributed, non-parametric test, Wilcoxon signed-rank test (p < 0.05) was used to analyse the differences of the linear measurements of furcation defects between CBCT/periapical and intrasurgery. The data were presented as medians and interquartile range (IQR). Significance level was set at p < 0.05.
RStudio Inc. Statistical Software version 0.97.551—© 2009–2012 (package ‘pROC’) was used to calculate the sensitivity of the CBCT and periapical radiographs. The CBCT and periapical radiograph were used as a binary response, while measurements comprising the CEJ-BD, BL-V, RT, and FW were used as predictors. The optimal cut-off points corresponding to the maximum combination sensitivity and specificity observed were dichotomised into two cut-offs: 0 = intrasurgical measurement and 1 = CBCT/periapical radiograph measurement.
Results
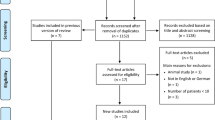
The study sample was initially comprised of 23 patients. However, one patient from the intervention group dropped out of the study because of the hopeless prognosis of the involved molar tooth with FI during the randomised controlled trial. The remaining subjects (n = 22) completed all evaluations, and their data were included in the final analysis (CONSORT flow chart; Fig. 4). Patient in the CBCT group ranged between 29 and 64 years old, with a mean age of 44 years old. The mean age for periapical group was 47.8 years old. Majority of the affected teeth were the first molar. The highest number of furcation defects was found in the buccal site (Table 3).
Tables 4 and 5 show the comparison of variables measured using CBCT and periapical group with intrasurgical methods. In CBCT (3D) group, there was no significant difference between the measurements of all the variables in all molars teeth (CEJ-BD, BL-H, BL-V, RT, and FW) (p > 0.05). In periapical (2D) group, the differences between the periapical and intrasurgical measurements for CEJ-BD, BL-V, RT, and FW were not statistically significant (p > 0.05) in all molars teeth except BL-V parameter in maxillary molars.
The diagnostic characteristics of CBCT and periapical radiograph were evaluated by calculating the sensitivity and specificity. Figure 5 shows the area under the curve (AUC) for both groups. CBCT provided better sensitivity of the furcation defects that periapical radiograph with 62.8%.
Discussion
This study compared the measurements of furcation defects between CBCT (3D), periapical radiograph (2D), and intrasurgical (clinical) methods for the treatment of periodontitis patients who had molar with advanced FI. Among the three methods, the intrasurgical assessment is considered as the ‘gold standard’ for the assessment of furcation defects [4, 12]. Therefore, this gold standard procedure was used as a control in the current study.
To the best of our knowledge, the current study is the first investigation comparing two different radiographic techniques of furcation defects for the treatment of molar with advanced FI in the same population. Previous studies to evaluate the use of CBCT and periapical in furcation bone defects [23], and intrabony bone defects [24] were mostly performed on dry human skull or animals. However, these studies might not be able to simulate the exact in vivo conditions to ensure the diagnostic validity of periodontal osseous defects.
There was a high degree of agreement between CBCT measurements and intrasurgical findings. In the analysis, there were no statistically significant differences between the CBCT and intrasurgical measurements for any clinical parameter (p > 0.05) in all molars teeth. Thus, it may be interpreted that the median values of the two methods were similar, indicating that both methods were able to produce similar measurements for the furcation defects in terms of height (BL-V), width (FW), and depth (BL-H). It also meant that the error between CBCT-based data and intrasurgical measurements of a molar with FI was trivial and could be accepted in the clinical periodontal application. CBCT-based data were able to accurately reflect the real state of furcation defects in molar with FI. In short, both methods were similar in measuring the physical access of the furcation defects. These results are consistent with those of other studies and suggest that CBCT images demonstrated a high accuracy in assessing furcation defects and optimise treatment planning, particularly when involve more invasive treatment approaches [2,3,4, 12].
Coherently, the results from this study indicated that CBCT was highly accurate for the diagnosis of a molar with FI particularly in horizontal bone loss. The assessment of horizontal bone loss cannot be completed comprehensively with a periapical radiograph. This finding was in line with a study by Fiejo et al. that found no statistically significant differences between intrasurgical and CBCT measurements in the measurement of horizontal periodontal bone defects of 72 maxillary molar teeth [25].
The most interesting aspect of the data was in the periapical group. With no statistically significant difference between all the measurement parameters in periapical group, except for the BL-V parameter in maxillary molars, the results suggested that although 2D imaging radiographs have certain limitations and questionable roles for diagnostic purpose, the periapical radiograph is still the most useful imaging technique in periodontal practice [6, 26]. The method was proven to be effective in the assessment of mandibular molars [27, 28]. However, its application is limited in the assessment of maxillary molars due to obstruction by the roots and alveolar bone, particularly at the interradicular area. These results are in agreement with Vasconcelos et al.’s findings, which showed a statistically significant difference in terms of the height but no statistically significant difference in the measurement of the depth and width of the bone defects between CBCT and periapical radiograph [29]. However, the findings of the current study differ from a recent study, which found significant results in all parameters between periapical and intrasurgical methods [16]. A possible explanation of these results may be due to differences in the type of molar and clinical parameters used in the previous study.
Apart from that, recent evidences found that both vertical and horizontal classification seems to be a good predictor of survival of molar with furcation defects [30, 31]. In other words, BL-H (depth) and BL-V (height) are the most important parameters involved during prognosis of molar. Therefore, based on the study results, if the clinician is interested to assess the prognosis of furcation defects, particularly in maxillary molars, CBCT is more superior choice and more versatile in terms of the comprehensive visualisation planes as compared to the periapical views. This is particularly important especially when measuring BL-H (depth) and BL-V (height) in furcation defect measurements where periapical radiograph could not make up for its accuracy.
The findings from this study also suggest that CBCT is still not the first choice in imaging for periodontal bone support. Although CBCT images had a higher agreement with the intrasurgical measurement compared to periapical radiograph in the assessment of molar with furcation defects, CBCT should not routinely replace other intra-oral images. In other words, not all suspected molars with FI are warranted for CBCT imaging.
As such, the decision to select the best imaging modality for diagnostic purposes of furcation defects should be made on a case-by-case basis. It should take into account the expected diagnostic yield expected and follow the ALARA principle. Both CBCT and periapical radiographs have their respective advantages and limitations. However, previous studies, literature, and radiation guidelines have highlighted that CBCT is warranted when a surgical procedure is scheduled for the molar tooth with FI, particularly in maxillary molar, to prevent inappropriate treatment plans and unnecessary radiation exposure [2, 3, 32].
There were certain limitations to this study. Firstly, it is necessary to note that the CEJ point taken in both CBCT and periapical radiographs was in a linear line created by joining the mesial and distal points of CEJ for each tooth. However, during the intrasurgical measurements, the initial point of CEJ in the furcation site that was taken might differ from the point taken during the radiographs. In other words, the radiographic assessment of furcation areas might be less accurate and less reliable in view of the complex anatomy and the overlay of the different anatomic structures.
Secondly, this study was only conducted on the deepest site of a molar with furcation defects. Hence, only one site was chosen for the measurement of the furcation defects in a molar tooth of a single patient. Therefore, the FI of trifurcation or bifurcation had to be matched to the highest degree of FI or furcation defects. While it is possible to discuss the result for prognosis or therapeutic implications on a tooth level, the results may not be valid for the discussion on a site level (each furcation entrance).
Conclusions
Despite these limitations, the study findings added significant contribution to the existing literature on the clinical uses of dental radiographs in periodontal management. The following conclusion can be drawn from this study:
-
i.
CBCT and intrasurgical measurements of a molar with furcation defects were found to be at a substantial level of agreement. CBCT images enable the accurate reproduction of the clinical measurement of clinical attachment loss (CEJ-BD), height (BL-V), width (FW), depth (BL-H), and root trunk (RT) in assessing molars with furcation defects.
-
ii.
The periapical radiograph was found to be less accurate in the clinical measurement of vertical bone loss in assessing maxillary molar with furcation defects.
-
iii.
Overall, when compared to the intrasurgical measurements, CBCT provided better diagnostic, sensitivity, and quantitative information on CAL, height, depth, and width of the furcation defects than periapical radiograph.
References
American Academy of Periodontology (1992) Glossary of periodontal terms, 3rd edn. Illinois, Chicago
Walter C, Kaner D, Berndt DC, Weiger R, Zitzmann NU (2009) Three-dimensional imaging as a pre-operative tool in decision making for furcation surgery. J Clin Periodontol 36:250–257
Walter C, Schmidt JC, Dula K, Sculean A (2016) Cone beam computed tomography (CBCT) for diagnosis and treatment planning in periodontology: a systematic review. Quintessence Int (Berl) 47(1):25–37
Qiao J, Wang S, Duan J, Zhang Y, Qiu Y, Sun C, Liu D (2014) The accuracy of cone-beam computed tomography in assessing maxillary molar furcation involvement. J Clin Periodontol 41:269–274
Darby I, Sanelli M, Shan S, Silver J, Singh A, Soedjono M, Ngo L (2015) Comparison of clinical and cone beam computed tomography measurements to diagnose furcation involvement. Int J Dent Hyg 13(4):241–245
Mol A (2004) Imaging methods in periodontology. Periodontol 34:34–48
Cury PR, de Araújo NS, Bowie J, Sallum EA, Jeffcoat M (2004) The relationship between radiographic and clinical parameters in periodontal maintenance in class II furcation defects. Braz Oral Res 18(2):116–120
Deas DE, Moritz AJ, Mealey BL, McDonnell HT, Powell CA (2006) Clinical reliability of the ‘furcation arrow’ as a diagnostic marker. J Periodontol 77(8):1436–1441
Laky M, Majdalani S, Kapferer I, Frantal S, Gahleitner A, Moritz A, Ulm C Periodontal probing of dental furcations compared with diagnosis by low-dose computed tomography: a case series. J Periodontol 84(12):1740–1746
Cimbaljevic MM, Spin-Neto RR, Miletic VJ, Jankovic SM, Aleksic ZM, Nikolic-Jakoba NS (2015) Clinical and CBCT-based diagnosis of furcation involvement in patients with severe periodontitis. Quintessence Int 46(10):863–870
Yusof NAM, Noor E, Yusof MYPM (2020) The accuracy of linear measurements in cone beam computed tomography for assessing intrabony and furcation defects: a systematic review and meta-analysis. J Oral Res 8(6):527–539
Walter C, Weiger R, Zitzmann NU (2010) Accuracy of three-dimensional imaging in assessing maxillary molar furcation involvement. J Clin Periodontol 37:436–441
Pajnigara N, Kolte A, Kolte R, Pajnigara N, Lathiya V (2016) Diagnostic accuracy of cone beam computed tomography in identification and postoperative evaluation of furcation defects. J Indian Soc Periodontol 20(4):386–390
Padmanabhan S, Dommy A, Guru SR, Joseph A (2017) Comparative evaluation of cone-beam computed tomography versus direct surgical measurements in the diagnosis of mandibular molar furcation involvement. Contemp Clin Dent 8(3):439–445
Pahwa P, Lamba A, Grewal H, Faraz F, Tandon S, Yadav N (2014) Evaluation of two-dimensional and three-dimensional radiography with direct surgical assessment of periodontal osseous defects: a clinical study. Indian J Dent Res 25(6):783–787
Parvez MF, Manjunath N, Kini R (2018) Comparative assesment of accuracy of IOPA and CBCT for maxillary molar furcation involvement: a clinical and radiological study. Int J Res Med Sci 6(5):1765–1769
Tonetti MS, Greenwell H, Kornman KS (2018) Staging and grading of periodontitis: framework and proposal of a new classification and case definition. J Clin Periodontol 89(Suppl 1):S159–S172
Hamp S, Nyman S, Lindhe J (1975) Periodontal treatment of multirooted teeth. Results after 5 years. J Clin Periodontol 2(3):126–135
O’Leary TJ, Drake RB, Naylor JE (1972) The plaque control record. J Periodontol 43:38
Ainamo J, Bay I (1975) Problems and proposals for recording gingivitis and plaque. Int Dent J 25(4):229–235
Doig GS, Simpson F (2005) Randomization and allocation concealment: a practical guide for researchers. J Crit Care 20(2):187–191
Koo TK, Li MY (2016) A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med 15(2):155–163
Salineiro FCS, Gialain IO, Kobayashi-Velasco S, Pannuti CM, and Cavalcanti MGP (2017) Detection of furcation involvement using periapical radiography and 2 cone-beam computed tomography imaging protocols with and without a metallic post: an animal study. Imaging Sci. Dent., vol. 47, no. 1
Mengel R, Candir M, Shiratori K, Flores-de-Jacoby L (2005) Digital volume tomography in the diagnosis of periodontal defects: an in vitro study on native pig and human mandibles. J Periodontol 76(5):665–673
Feijo CV, de Lucena JGF, Kurita LM, da S Pereira SL (2012) Evaluation of cone beam computed tomography in the detection of horizontal periodontal bone defects: an in vivo study. Int J Periodontics Restorative Dent 32(5):e162–e168
Scarfe WC, Azevedo B, Pinheiro LR, Priaminiarti M, Sales MAO (2017) The emerging role of maxillofacial radiology in the diagnosis and management of patients with complex periodontitis. Periodontology 2000 74(1):116–139
Horwitz J, Machtei EE, Reitmeir P, Holle R, Kim TS, Eickholz P (2004) Radiographic parameters as prognostic indicators for healing of class II furcation defects. J Clin Periodontol 31(2):105–111
Jenabian N, Haghanifar S, Maboudi A, Bijani A (2013) Clinical and radiographic evaluation of Bio-Gen with biocollagen compared with Bio-Gen with connective tissue in the treatment of class II furcation defects: a randomized clinical trial. J Appl Oral Sci 21(5):422–429
De Faria VK, Evangelista KM, Rodrigues CD, Estrela C, De Sousa TO, Silva MAG (2012) Detection of periodontal bone loss using cone beam CT and intraoral radiography. Dentomaxillofac Radiol 41(1):64–69
Tonetti MS, Christiansen AL, Cortellini P (2017) Vertical subclassification predicts survival of molars with class II furcation involvement during supportive periodontal care. J Clin Periodontol 44:1140–1144
Nibali L, Sun C, Akcalı A, Yeh YC, Tu YK, Donos N (2018) The effect of horizontal and vertical furcation involvement on molar survival: a retrospective study J. Clin Periodontol 45:373–381
Sedentexct (2012) Radiation protection 172: cone beam CT for dental and maxillofacial radiology—evidence-based guidelines off. Off. Publ. Eur. Communities
Funding
The work was supported by LESTARI Research Grant, Universiti Teknologi MARA, Malaysia (600-IRMI 5/3/LESTARI (011/2019)).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in this study were in accordance with the Ethical Committee of Universiti Teknologi MARA (REC/295/17) and registered with the Identification of Randomised Controlled Clinical Trials worldwide registry (ISRCTN89375372). This study was conducted following the ICH Good Clinical Practice Guidelines, Malaysia Good Clinical Practice Guidelines, and the Declaration of Helsinki.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Yusof, N.A.M., Noor, E., Reduwan, N.H. et al. Diagnostic accuracy of periapical radiograph, cone beam computed tomography, and intrasurgical linear measurement techniques for assessing furcation defects: a longitudinal randomised controlled trial. Clin Oral Invest 25, 923–932 (2021). https://doi.org/10.1007/s00784-020-03380-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-020-03380-8