Abstract
Objectives
To assess the impact of orthodontic treatment combined with piezocision (OT-PC) on root structure and alveolar bone.
Materials and methods
Twelve adults were treated with OT-PC. Pre- and post-treatment CBCT examinations evaluated apical root resorption (ARR) and alveolar bone height and thickness changes. Pre- and post-treatment differences were compared using one-sample t test and Wilcoxon signed-rank test.
Results
ARRs were generalized and significantly more severe in both anterior sextants compared with posterior sextants. Bone thickness decreased significantly in the maxilla at mid-root and apex areas. The majority of mandibular alveolar bone dehiscences occurred on the buccal aspect at the mid-root level, especially where thickness was less than 0.3 mm. Overall bone height decreased twice as much on the buccal aspect (1.43 mm, P < 0.001) compared with the lingual aspect (0.67 mm, P = 0.001), most significantly in the lower incisors, where the average median loss was 2.10 mm (P = 0.003).
Conclusion
OT-PC causes minor negative effects on both alveolar bone and root resorption.
Clinical relevance
Orthodontic treatment combined with piezocision causes minor negative effects on periodontal support. Nevertheless, mild bone height loss on the buccal aspect of the mandibular teeth and root resorption in both anterior sextants have been detected with this new treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Reducing the length of orthodontic treatment has become a key goal for orthodontists, since it would decrease the risk of developing negative side effects, such as caries, decalcifications, gingival recession, root resorption, alveolar bone loss, and discomfort. In addition, patient satisfaction with orthodontic treatment is often correlated with reduced treatment time.
In 2009, Dibart et al. reported on a minimally invasive surgical technique to accelerate orthodontic tooth movement by using piezocision called Piezocision™ [1]. This newer type of corticision consists of creating damage to the alveolar bone by perforating the interproximal cortices with a piezo-electric device. It is considered a minimally invasive technique because it does not require a gingival flap, unlike other surgical approaches such as corticotomy. However, the effectiveness of orthodontic treatment combined with piezocision (OT-PC) has been controversial. Two randomized controlled trials (RCT) demonstrated a twofold decrease in the alignment phase and in the total treatment time with OT-PC, while another did not find any statistically significant difference [2,3,4,5]. Although recent systematic reviews have found no significant periodontal damage following OT-PC, the effects on alveolar bone have not been reported [6, 7]. To date, no studies have attempted to quantify alveolar bone alterations in humans treated with OT-PC. Only a few studies have investigated the effects of conventional orthodontic treatment (COT) on alveolar bone height and thickness, particularly on the anterior teeth [8,9,10]. Due to this lack of evidence, an efficient OT-PC protocol has yet to be standardized. Although some OT-PC protocols recommend an additional bone allograft at the time of the surgery, its use and benefits are still debated [1, 3, 5, 11]. While the effect of OT-PC on apical root resorption (ARR) remains unknown [3, 5, 12], its impact on the periodontal health merits further investigation. Therefore, the aim of this study was to evaluate the effects of OT-PC on alveolar bone height and thickness, as well as on root structure.
Material and methods
This study was approved by the ethics committee of the Université de Montréal (15–002-CERES-P, clinical trial number NCT02359760, Assessment of Piezoelectric Periodontal Surgery Effects on Orthodontic Treatment: a Prospective Pilot Study).
Twelve adult patients interested in undergoing OT-PC were recruited in the graduate orthodontic clinic at the Faculty of Dentistry. It was determined that inclusion of at least 11 subjects was required after sample size calculation in order to achieve a power of 80% at a 5% significance level, based on a mean treatment time of 18 months for OT-PC. This was compared with a treatment time of 24 months using conventional orthodontic therapy, with a standard deviation of 4.6 months and a two-sample t test (PASS version 12). The inclusion criteria are as follows: patients aged 18 to 40; minor skeletal disharmonies; dental malocclusion not requiring tooth extraction or orthognathic surgery; patients without systemic diseases; complete permanent dentition; good oral hygiene; and absence of oral infection or periodontitis. The exclusion criteria are as follows: patients regularly taking analgesics and antidepressants; patients abusing alcohol or drugs or smoking more than 10 cigarettes per day; pregnancy; coagulation disorders or anticoagulant intake; oral or intravenous bisphosphonate intake for more than 4 years; patients requesting early cessation of treatment; and non-compliant patients with more than five missed appointments or bracket failures.
All patients had complete extra- and intra-oral examinations, including photographs, dental cast models, panoramic radiographs, and lateral cephalographs. A calibrated examiner used the discrepancy index (DI) devised by the American Board of Orthodontics (ABO) to rate case degree of difficulty [13]. This method permits a clinical assessment of a patient’s condition by quantifiying and objectively listing the target disorders associated with orthodontic diagnosis. The DI method is based on observations and measurements taken from standard pretreatment orthodontic records, including casts, cephalometric, and panoramic radiographs. Also, Two cone beam computed tomography (CBCT) examinations (NewTom 5G®, Newtom, Verona, Italy) were performed 1 month before initiating treatment and the week after bracket debonding. All acquisitions were carried out using the same CBCT machine with the following settings: 110 kVp, 5.4 s of exposure, 120 × 80 mm field of view, and 0.150 mm voxel size.
The surgical protocol used was that described by Strippoli et al. [14]. Briefly, after local anesthesia was achieved using bupivaine HCL 0.5% with epinephrine 1:200,000 (Vivacaine®, Septodont, Saint-Maur-des-Fossés, France), interradicular piezocisions were performed using a 3-mm-long and 0.35-mm-thick piezoelectric insert (OT7S-3 Piezosurgery®, Mectron, Piezosurgery Inc., Columbus, OH, USA). The piezocisions were carried out from the mesial of the 1st molar to the contralateral tooth in both arches. Mean depth of the 5-mm-long piezocisions were approximatively 2 mm between the anterior teeth and 3 mm in the posterior sextants depending on the interradicular anatomy, i.e., adequate inter-radicular spacing. Neither sutures nor bone and soft tissue grafts were used. Patients were given 500 mg acetaminophen (paracetamol) immediately after surgery and were prescribed the same dosage every 4 h for the first 48 h postoperatively. Orthodontic treatment started on the same day of the surgery. Patients were treated using SPEED™ brackets (Strite Industries Limited, Shepard, ON, Canada), and the archwire sequence was adapted for each patient’s biomechanical needs, except for the first wire where an 0.018″ coaxial superelastic nickel titanium (Supercable™, Strite Industries Limited) was used for 3 weeks.
Data collection
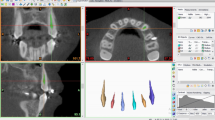
The alveolar bone height and thickness and ARR were measured on pre- and post-treatment CBCT exams using slightly modified methodologies of Garlock et al. [8] and Kook et al. [15]. Reference points, reference lines, and measurements are described in Table 1 and Fig. 1. Measurements were taken from the mesial of the 1st molar to the contralateral tooth in both the maxilla and mandible. One examiner (JS) did all the measurements and was calibrated with a gold standard examiner (MS). The intra-examiner reliability was made by the calibrated examiner (JS) who made all the measurements. For the inter-examiner reliability, the gold standard examiner (MS) made measurements once, and these were compared with the first measurements of the calibrated examiner (JS) involved in the intra-examiner reliability. For each arch, the CBCT slices were oriented along the long axis of the tooth in both mesiodistal and buccolingual orientation. The buccolingual section was used to determine the alveolar bone thickness and crest height. CBCT image analyses were performed using NNT software (Newtom, Verona, Italy) (Fig. 1). All the images were visualized on a high-definition medical monitor (EIZO RadiForce MX215-BK 21.3” LCD monitor, EIZO Co., Hakui, Japan).
Measurements to evaluate alveolar bone thickness and height taken through the CBCT buccolingual section of the tooth. Abbreviations are described in Table 1
Alveolar bone thickness
All measurements were carried out parallel to the cervical reference line (CRL). To measure alveolar bone thickness, post-treatment root length was used as a reference to avoid the influence of the ARR on the measurements. For premolars with two roots, all measurements were assessed parallel to the CRL on both roots. The total thickness of the alveolar bone and the thickness of buccal and lingual cortical bones were measured at the mid-root height and at the apex of the root (Fig. 1). Dehiscences with complete buccal or lingual bone resorption were assessed. In the maxilla, if the root apex was located above the level of the palatal plane, only the buccal cortical thickness was measured.
Alveolar crest height loss
All the measurements were taken perpendicularly to the CRL. Buccal and lingual alveolar crest heights were determined for each tooth pre- and post-treatment (Fig. 1). The loss of the alveolar crest height was assessed by the difference between the values pre- and post-treatment.
Apical root resorption
Quantitative and qualitative analyses were carried out to estimate the ARR. The root length was measured pre- and post-treatment (Fig. 1). As a complementary qualitative assessment, the Levander and Malmgren index [16] was used in order to classify ARR into five stages on the buccolingual and the mesiodistal slices (Table 1).
Statistical analysis
Intra- and inter-examiner reliability scores were determined using intraclass correlation coefficients (ICC). The Dahlberg’s formula was performed to quantify random errors. The P < 0.05 level of significance was chosen. Differences between post- and pre-values were calculated as post-value–pre-value. A Shapiro-Wilk test was used to assess the normality of distributions. Mean ± SD and median ± IQR were used for descriptive statistics. Differences were compared with zero by using one-sample t tests and Wilcoxon signed-rank tests when appropriate. Spearman’s rho correlation was used to determine if the mean DI crowding score was correlated to buccal bone height resorption. All analyses were performed with the SPSS version 24 software (IBM Co., Armonk, NY, USA) and SAS version 9.4 (SAS Institute Inc., Cary, NC, USA).
Results
Reliability of the measurements
Table 1 shows the calibration results. For all measurements, the intra-examiner ICC ranged from 0.845 to 0.986 and the inter-examiner ICC from 0.690 to 0.988, showing moderate to excellent reliability. The inter-examiner ICC for the DI score was 0.980. Random error measurement ranged from 0.089 to 0.248 for the intra-examiner and 0.140 to 0.396 for the inter-examiner calibrations.
Patient and treatment characteristics
Patient and treatment characteristics are described in Table 2. The mean age of participants was 28 ± 6 years and the female to male ratio was 2:1. The mean initial DI score was 16.6 ± 5.7 and the mean treatment time was 14.5 ± 3.1 months.
Alveolar bone thickness and alveolar crest height loss
There were significant pre- vs post-treatment differences in the alveolar bone thickness and height (Fig. 2). While the bone thickness was significantly reduced at the apex level of the maxillary teeth (ATA, LCTA), the anterior region presented a more marked reduction in bone thickness than the posterior teeth. At the mid-root level, all upper teeth showed statistically significant differences in the lingual cortical thickness (LCTM) and alveolar process (ATM). Significant loss of alveolar crest height was observed at the lingual aspect of maxillary anterior teeth (LCH) and on the buccal crest height (BCH) of the upper posterior teeth. However, in the mandible, alveolar crest height loss was statistically significant in all teeth, except at the lingual alveolar crest of the anterior teeth. More precisely, the buccal crest height loss in the lower anterior teeth was double that on the lingual surface. For the posterior teeth, crestal bone height reduction was more than 3 times greater on the buccal surface compared with the lingual surface.
Alveolar bone thickness changes, crest height loss and root resorption following OT-PC assessed from the mesial of the 1st molar to the contralateral tooth in both the maxilla and mandible. Differences between post- and pre-treatment values were calculated in mm; therefore a negative value corresponds to a post-treatment decrease. ‡ data did not follow the normal law therefore a one sample Wilcoxon test was used and the median with inter quartile range (IQR) was expressed. For others variables, a one sample t-test was used and the mean with the standard deviation (SD) was expressed. % = percentage of site with completely alveolar bone dehiscence after OT-PC. * = 0.05 > P > 0.01; ** = 0.01 ≥ P > 0.001; *** = P ≤ 0.001
Location and proportion of sites with alveolar bone dehiscence
Complete alveolar bone dehiscence occurred primarily at the mid-buccal aspect of the roots of the mandibular teeth. The anterior teeth were the most affected comprising 68.8% of dehiscences. In the mandible, 75% of subjects presenting post-treatment dehiscences had a pre-treatment bone thickness ≤ 0.3 mm (Table 3).
Correlation between DI crowding score and lower incisor buccal cortical bone
No statistical correlations were found between the mean of the DI crowding score and the loss of buccal bone height in lower incisors (p = 0.064).
Root resorption
Significant ARR was observed for all teeth, with the anteriors being most affected. The same tendency was demonstrated using the Levander and Malmgren index (LM) (Fig. 2).
Discussion
CBCT is a reliable, reproducible, and accurate modality for quantifying ARR and for measuring alveolar bone thickness and height [17,18,19,20,21,22,23,24,25]. It appears to be more effective in detecting apical root resorption compared with panoramic and periapical radiography [18,19,20,21, 26]. For precise quantification of alveolar bone thickness and height, the voxel size must be less than 0.400 mm, since the measurement accuracy increases with spatial resolution [22,23,24]. The voxel size used in this study was 0.150 mm, allowing for precise measurements with high resolution. Moreover, the intra- and inter-examiner reliability was considered good or excellent for most radiologic measurements.
Alveolar bone height in the maxilla and mandible decreased significantly in both lingual and buccal sites after OT-PC, but the bone loss on the buccal aspect of the mandibular anterior teeth was approximately double that on the lingual aspect. Although this decrease in anterior bone height was twice as much compared with the other sextants, it was still inferior to the amounts described for COT as reported by Garlock et al. (1.33 mm) [8]. However, the amount of alveolar bone height reduction on the buccal aspect of the mandible incisors was higher when compared with COT (1.12 mm) [8]. This difference could be explained by the fact that in our study, the mean age was 28 years old, while in the Garlock et al. study, it was 18.7 years old. Indeed, it was shown that older patients were more susceptible to buccal bone dehiscence after orthodontic therapy [27]. Further controlled clinical trials should be performed in humans, to assess the impact of OT-PC on bone dehiscence compared with conventional therapy and to evaluate the safety of the OT-PC treatment protocol.
The median DI score was 4, corresponding to crowding ranging between 5 and 7 mm. Although it may predispose teeth to procline after alignment and lead to bone lysis, this was not confirmed statistically in our study, probably due to the large interquartile range (IQR) or small sample size. Garlock et al. also found no statistically significant correlation between incisor to mandibular plane angle (IMPA) changes and facial vertical bone loss after COT [8].
The overall alveolar bone thickness (ATA/ATM) and the lingual cortical thickness (LCTA/LCTM) significantly decreased after OT-PC. Changes were particularly significant for the maxillary incisors, where the alveolar ridge was reduced by approximately a millimeter at the root apex level. In the mandible, alveolar bone thickness did not exhibit any significant change, possibly due to its minimal initial thickness. More specifically, if the bone was thin, the amount of resorption could not be easily detected.
Complete alveolar bone dehiscence occurred primarily in the buccal cortical bone at mid-root level of the lower teeth. According to our findings, 75% of subjects presenting post-treatment dehiscences had a pre-treatment mandibular bone thickness ≤ 0.3 mm. This emphasizes the need for bone grafts to prevent bone resorption after OT-PC, as initially proposed by Dibart et al. [1]. To our knowledge, this information has not been previously discussed in the literature. Further studies are necessary to assess the necessity for pre-orthodontic bone grafting procedures, even for COT and to investigate whether these bone dehiscences are caused by PC, by proclination of the anterior mandibular teeth or by both.
In our study, ARR was relatively small with a mean reduction of 0.55 mm. However, it was more significant in both anterior sextants, remaining below a millimeter. This amount of ARR resorption was similar with those reported for COT [26]. Results should be interpreted with caution since the measurement of root length could have been affected by the teeth’s large apical curvatures. This possibility led us to investigate ARR using another objective measure, the Levander and Malmgren index. The overall mean score index of 0.98 is considered as mild root resorption. It was comparable with Charavet et al.’s results showing a mean root resorption score of 0.91 [3]. Randomized controlled trials comparing OT-PC and COT could reveal if PC reduces the risk of ARR, since this question is still debated in the literature [28,29,30,31]. Two studies concluded that there were no significant differences between the two techniques [3, 5], while a recent and controversial trial found that OT-PC increased root resorption [12, 32]. However, we hypothesize that the shorter treatment time with OT-PC should have a lesser impact on ARR than for the COT group [31]. Further studies are necessary to investigate whether the periodontal inflammation caused by PC may have a negative effect on the root structure [33].
Nevertheless, our study presents some limitations. Since CBCT was performed within 1 week after the end of active treatment, newly formed or remodeled bone was possibly present but not detected by radiography [34]. In addition, since very thin bone may not be detected even with high CBCT resolution, alveolar bone dehiscences may have been overestimated [25]. While our sample size was small and consisted of more females than males, previous studies have shown that the impact of gender on root resorption, initial bone volume or defects was not significant [29, 35]. Since this study excluded malocclusions with extractions or major skeletal disharmonies, our findings cannot be extrapolated to all orthodontic populations. The lack of standardization of the arch wire sequence could influence root resorptions but this impact is not clear [36]. Although further studies including a control group are required, our findings highlight the potential effects of OT-PC on the periodontal health. The OT-PC requires appliance activation every 2 weeks, in order to optimize the effect of the regional acceleratory phenomenon and to accelerate the tooth movement. The inclusion of a control group was not considered for this study because this protocol for such frequent application of orthodontic force over shorter time periods could lead to important undesirable side effects to the periodontal support in patients not receiving the piezocision. Nonetheless, our study showed the impact of OT-PC on the root and bone structures, in patients who underwent the procedure.
Conclusion
OT-PC causes minor negative effects on both alveolar bone and root resorption. Nevertheless, CBCT evaluation demonstrated that bone height loss was greater on the buccal aspect of the mandibular teeth and showed that ARR was more significant in both anterior sextants. Moreover, the majority of complete alveolar bone dehiscences occurred on the buccal cortical bone at mid-root level of the lower teeth.
References
Dibart S, Sebaoun JD, Surmenian J (2009) Piezocision: a minimally invasive, periodontally accelerated orthodontic tooth movement procedure. Compend Contin Educ Dent 30:342–344 346, 348–350
Gibreal O, Hajeer MY, Brad B (2018) Efficacy of piezocision-based flapless corticotomy in the orthodontic correction of severely crowded lower anterior teeth: a controlled trial. Eur J Orthod
Charavet C, Lecloux G, Bruwier A, Rompen E, Maes N, Limme M, Lambert F (2016) Localized piezoelectric alveolar decortication for orthodontic treatment in adults: a randomized controlled trial. J Dent Res 95:1003–1009
Uribe F, Davoody L, Mehr R, Jayaratne YS, Almas K, Sobue T et al (2017) Efficiency of piezotome-corticision assisted orthodontics in alleviating mandibular anterior crowding-a randomized clinical trial. Eur J Orthod 39:595–600
Abbas NH, Sabet NE, Hassan IT (2016) Evaluation of corticotomy-facilitated orthodontics and piezocision in rapid canine retraction. Am J Orthod Dentofac Orthop 149:473–480
Yi J, Xiao J, Li Y, Li X, Zhao Z (2017) Efficacy of piezocision on accelerating orthodontic tooth movement: a systematic review. Angle Orthod 87:491–498
Hoffmann S, Papadopoulos N, Visel D, Visel T, Jost-Brinkmann PG, Prager TM (2017) Influence of piezotomy and osteoperforation of the alveolar process on the rate of orthodontic tooth movement: a systematic review. J Orofac Orthop 78:301–311
Garlock DT, Buschang PH, Araujo EA, Behrents RG, Kim KB (2016) Evaluation of marginal alveolar bone in the anterior mandible with pretreatment and posttreatment computed tomography in nonextraction patients. Am J Orthod Dentofac Orthop 149:192–201
Ma ZG, Yang C, Fang B, Xia YH, Mao LX, Feng YM (2015) Three-D imaging of dental alveolar bone change after fixed orthodontic treatment in patients with periodontitis. Int J Clin Exp Med 8:2385–2391
Kennedy DB, Joondeph DR, Osterberg SK, Little RM (1983) The effect of extraction and orthodontic treatment on dentoalveolar support. Am J Orthod 84:183–190
Aksakalli S, Calik B, Kara B (2015) Ezirganhi S. Accelerated tooth movement with piezocision and its periodontal-transversal effects in patients with Class II malocclusion, Angle Orthod
Patterson BM, Dalci O, Papadopoulou AK, Madukuri S, Mahon J, Petocz P, Spahr A, Darendeliler MA (2017) Effect of piezocision on root resorption associated with orthodontic force: a microcomputed tomography study. Am J Orthod Dentofac Orthop 151:53–62
Cangialosi TJ, Riolo ML, Owens SE Jr, Dykhouse VJ, Moffitt AH, Grubb JE, Greco PM, English JD, James RD (2004) The ABO discrepancy index: a measure of case complexity. Am J Orthod Dentofac Orthop 125:270–278
Strippoli JDR, Schmittbuhl M, Voyer R, Rompré P, Nishio C (2017) Pain and quality of life in patients undergoing guided piezocorticision-assisted orthodontic treatment. J Clin Orthod 51:792–799
Kook YA, Kim G, Kim Y (2012) Comparison of alveolar bone loss around incisors in normal occlusion samples and surgical skeletal class III patients. Angle Orthod 82:645–652
Levander E, Malmgren O (1988) Evaluation of the risk of root resorption during orthodontic treatment: a study of upper incisors. Eur J Orthod 10:30–38
Lund H, Grondahl K, Grondahl HG (2010) Cone beam computed tomography for assessment of root length and marginal bone level during orthodontic treatment. Angle Orthod 80:466–473
Dudic A, Giannopoulou C, Leuzinger M, Kiliaridis S (2009) Detection of apical root resorption after orthodontic treatment by using panoramic radiography and cone-beam computed tomography of super-high resolution. Am J Orthod Dentofac Orthop 135:434–437
Sherrard JF, Rossouw PE, Benson BW, Carrillo R, Buschang PH (2010) Accuracy and reliability of tooth and root lengths measured on cone-beam computed tomographs. Am J Orthod Dentofac Orthop 137:S100–S108
Ren H, Chen J, Deng F, Zheng L, Liu X, Dong Y (2013) Comparison of cone-beam computed tomography and periapical radiography for detecting simulated apical root resorption. Angle Orthod 83:189–195
Ponder SN, Benavides E, Kapila S, Hatch NE (2013) Quantification of external root resorption by low- vs high-resolution cone-beam computed tomography and periapical radiography: a volumetric and linear analysis. Am J Orthod Dentofac Orthop 143:77–91
Timock AM, Cook V, McDonald T, Leo MC, Crowe J, Benninger BL, Covell DA Jr (2011) Accuracy and reliability of buccal bone height and thickness measurements from cone-beam computed tomography imaging. Am J Orthod Dentofac Orthop 140:734–744
Leung CC, Palomo L, Griffith R, Hans MG (2010) Accuracy and reliability of cone-beam computed tomography for measuring alveolar bone height and detecting bony dehiscences and fenestrations. Am J Orthod Dentofac Orthop 137:S109–S119
Sun Z, Smith T, Kortam S, Kim DG, Tee BC, Fields H (2011) Effect of bone thickness on alveolar bone-height measurements from cone-beam computed tomography images. Am J Orthod Dentofac Orthop 139:e117–e127
Patcas R, Muller L, Ullrich O, Peltomaki T (2012) Accuracy of cone-beam computed tomography at different resolutions assessed on the bony covering of the mandibular anterior teeth. Am J Orthod Dentofac Orthop 141:41–50
Samandara A, Papageorgiou SN, Ioannidou-Marathiotou I, Kavvadia-Tsatala S, Papadopoulos MA (2018) Evaluation of orthodontically induced external root resorption following orthodontic treatment using cone beam computed tomography (CBCT): a systematic review and meta-analysis. Eur J Orthod
Jäger F, Mah JK, Bumann A (2017) Peridental bone changes after orthodontic tooth movement with fixed appliances: a cone-beam computed tomographic study. Angle Orthod 87(5):672–680
Proffit WRFHJ, Sarver DM (2012) Contemporary orthodontics, 5th edn. Elveseir Mosby, St. Louis
Sameshima GT, Sinclair PM (2001) Predicting and preventing root resorption: part I. Diagnostic factors Am J Orthod Dentofacial Orthop 119:505–510
Kaley J, Phillips C (1991) Factors related to root resorption in edgewise practice. Angle Orthod 61:125–132
Roscoe MG, Meira JB, Cattaneo PM (2015) Association of orthodontic force system and root resorption: a systematic review. Am J Orthod Dentofac Orthop 147:610–626
Khoo E, Alansari S, Nervina J (2017) Piezocision and root resorption: a biased conclusion? Am J Orthod Dentofac Orthop 151:1020–1021
Iglesias-Linares A, Hartsfield JK Jr (2017) Cellular and molecular pathways leading to external root resorption. J Dent Res 96:145–152
Molen AD (2010) Considerations in the use of cone-beam computed tomography for buccal bone measurements. Am J Orthod Dentofac Orthop 137:S130–S135
Qu X, Liu Z, Wang Y, Fang Y, Du M, He H (2017) Dentofacial traits in association with lower incisor alveolar cancellous bone thickness: a multiple regression analysis. Angle Orthod 87:409–415
Mandall NA, Vine S, Hulland R, Worthington HV (2006) The impact of fixed orthodontic appliances on daily life. Community Dent Health 23:69–74
Acknowledgments
This study would not have been possible without financial support from the Associate Dean of Research funds at the Université de Montréal.
Funding statement
This study was financial supported by the Associate Dean of Research Funds, Faculty of Dentistry, Université de Montréal.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The author(s) warrants that this study is original and free of conflict of interest, does not infringe upon any copyright or other proprietary right of any third party, is not under consideration by another journal and has not been published previously.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethics committee of the Université de Montréal (15–002-CERES-P, clinical trial number NCT02359760, Assessment of Piezoelectric Periodontal Surgery Effects on Orthodontic Treatment: a Prospective Pilot Study) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Strippoli, J., Schmittbuhl, M., Durand, R. et al. Impact of piezocision-assisted orthodontics on root resorption and alveolar bone: a prospective observational study. Clin Oral Invest 25, 4341–4348 (2021). https://doi.org/10.1007/s00784-020-03282-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-020-03282-9