Abstract
Objectives
Evaluate the cytotoxicity and biocompatibility of calcium hydroxide paste [Ca (OH)2] associated with 5% diclofenac sodium, ibuprofen, or amoxicillin.
Materials and methods
Pre-osteoblast-like cells were cultivated and the MTT test was used to determine the cytotoxicity of the paste extracts after time intervals of 24, 48, 72 h, and 7 days. Tubes containing Ca (OH)2 pastes associated with the drugs and empty tubes were implanted in subcutaneous tissue of 30 rats. After 7 and 30 days, the specimens were removed and submitted to histological analysis. The data obtained were submitted to Kruskal-Wallis and Dunn tests (p ≤ 0.05).
Results
All the Ca (OH)2 pastes promoted cell viability after all periods. At 7 days, there was greater inflammatory tissue reaction adjacent to the implants. At 30 days, there was a significant reduction in the number of inflammatory cells, and increase in fibroblasts in all groups. In this period, a lower number of inflammatory cells and a higher number of fibroblasts were observed in the capsules adjacent to the association with diclofenac, when compared with the other mixtures (p ≤ 0.05); the capsule thickness was greater at 7 days than at 30 days.
Conclusions
The Ca (OH)2 pastes associated with the drugs were not cytotoxic and presented biocompatibility after implantation in rat subcutaneous tissues.
Clinical relevance
Ca (OH)2 pastes with anti-inflammatory or antibiotic may be clinical alternatives as intracanal medication to reduce resistant microorganisms in root canal system.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Calcium hydroxide pastes [Ca (OH)2] are widely used in dentistry as intracanal medications, for the purpose of helping to control infection [1]. This medication is known to present innumerable advantages, such as, induction of mineralized tissue [2], antimicrobial activity [3], and inactivation of lipopolysaccharide found in the outer membrane of Gram-negative bacteria [4].
In spite of this, some microorganisms present in endodontic infection are resistant to the action of Ca (OH)2 pastes [5]. Therefore, with the purpose of increasing its antimicrobial spectrum, the association of different substances with Ca (OH)2 has been proposed [6, 7]. Dastidar et al. [8] demonstrated that diclofenac sodium, a non-steroidal anti-inflammatory drug (NSAID), presented antibacterial activity, causing the inhibition of DNA synthesis of Gram-positive and Gram-negative bacteria. Studies have also verified that diclofenac sodium, ibuprofen, and amoxicillin have greater action than Ca (OH)2 paste against Enterococcus faecalis, a resistant microorganism present in endodontic infections [9].
More recently, a study observed that the association of NSAIDs or antibiotics did not interfere in the pH of calcium hydroxide pastes, and significantly increased the antimicrobial activity against the formation of E. faecalis biofilms, with the best results being found in the mixture with diclofenac sodium [7]. Furthermore, according to the authors, the association of NSAIDs with Ca (OH)2 presented the clinical advantage of acting in the control of inflammation, diminishing post-operative pain after endodontic treatment. However, up to now, there are no studies that have evaluated the biological properties of these associations.
Considering that intracanal medications remain in direct contact with the apical and periapical tissues, it is fundamental to evaluate the biocompatibility of these products. Thus, the aim of this study was to evaluate the cytotoxicity and tissue reaction to Ca (OH)2 pastes associated with NSAIDs (diclofenac sodium and ibuprofen) and with amoxicillin after implantation in rat subcutaneous tissues.
Materials and methods
The materials evaluated in the present study were calcium hydroxide paste with propylene glycol, Ca (OH)2, Ca (OH)2 + diclofenac sodium, Ca (OH)2 + ibuprofen, and Ca (OH)2 + amoxicillin. The powders of the drugs (NSAIDs and antibiotic) were added to the calcium hydroxide powder in a proportion of 5% by weight. For manipulating the pastes, 1 g of powder was mixed with 1 mL propylene glycol [7].
Cytotoxicity
For the cell cultivation, MC3T3-E1 (ATCC®) mouse pre-osteoblast cell line cells were used. The cells were cultivated in α-MEM (Alpha Minimum Essential Medium; Gibco®, Gaithersburg, MD, USA), supplemented with 1% of antibiotic (penicillin/streptomycin; Gibco®, Gaithersburg, MD, USA) and 10% SFB (fetal bovine serum; Gibco®, Gaithersburg, MD, USA), and kept in an incubator at 37 °C containing 5% CO2. Then, the cells were subcultivated using the enzyme trypsin, responsible for dissociating the cells from the culture flask (0.25% trypsin, 1 mM EDTA; Sigma-Aldrich®, St Louis, MO, USA); after 5 min in an incubator at 37 °C with 5% CO2, the trypsin was inactivated with α-MEM culture medium with 10% FBS.
The cells were transferred to a 50-ml Falcon tube (Corning®) and centrifuged at 1,200 rpm, at 20 °C for 5 min. After centrifugation, the supernatant was discarded and the cells were resuspended in a new/fresh medium. After this, the cells were counted by means of the Trypan blue protocol. This dye is responsible for staining the non-viable cells. Afterwards, the cells were used for the experimental assays.
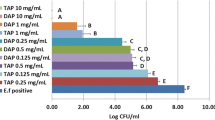
In our experiment, we used different concentrations of the pastes (10%, 1%, 0.1%, and 0.01%), and the control groups: positive (10% FBS) and negative (Milli-Q water). For the experimental groups, from the concentration of 0.1 g/mL (100%) in α-MEM medium, we began serial dilution in the concentrations of 10%, 1%, 0.1%, and 0.01%. The samples were incubated in an oven at 37 °C for 24 h. The experiment was performed as recommended by the ISO standards [10].
For the viability assays, 3 × 103 cells/well were plated in 96-well plates (Corning®). After incubation for 24 h, the culture medium was replaced with α-MEM 10% FBS either conditioned, or not. For each plate, an experimental time interval of 24 h, 48 h, 72 h, and 7 days was evaluated after addition of the medium that was either conditioned, or not. After each experimental period, the culture medium was removed, cells were washed with PBS buffer solution, and then the MTT reduction assay was performed.
Analysis of mitochondrial cell activity was performed by the MTT reduction method (3-[4,5-dimethylthiazol-2-il]-2,5-diphenyl tetrazolium bromide) [11]. This test quantified the conversion of MTT, which is soluble in water, in insoluble formazan. The purple-blue–colored formazan is solubilized; then, its concentration can be determined by optical density in a spectrophotometer. After the experimental time intervals (24, 48, 72 h, and 7 days), the cells were washed with PBS, and then incubated in a solution of 0.5 mg MTT to 1 mL α-MEM without FBS. This solution was filtered through a Millipore (0.22 μm) filter before being added to the plates [12].
After this procedure, the plates remained in an incubator at 37 °C and 5% CO2 for 4 h. Afterwards, the solution was removed; the intercellularly reduced insoluble pigment was extracted in DMSO (dimethyl sulfoxide) and left at ambient temperature for 30 min. Subsequently, the absorbance was measured at 550 nm (Synergy Reader h1 Monochromator-based; BioTek, Winooski, VT, USA) [12].
Tissue reaction
The research protocol in animal experimentation was submitted to and approved by the Ethics Commission on the Use of Animals (CEUA/USC No. 1515200916). Thirty (30) male Holtzman rats (Rattus norvegicus albinus) weighting 250 g were used. Polyethylene tubes (10 mm long and 1.5 mm in diameter), previously sterilized with ethylene oxide, were filled with the different materials (n = 5). After filling, these were immediately implanted in the dorsal subcutaneous tissue. Empty polyethylene tubes were used as control. Two tubes of different experimental groups were implanted in each rat in a rotational system.
The animals were anesthetized by intraperitoneal injection of ketamin (80 mg/of body weight; Virbac do Brasil Indústria e Comércio Ltda, SP, Brazil) associated with xylazine (4 mg/kg of body weight; União Química Farmacêutica Nacional S/A, SP, Brazil). After trichotomy and asepsis with 5% iodine solution in the animals’ dorsal region, a 2-cm incision was made with a scalpel blade. After 7 and 30 days, the tubes were removed with the adjacent connective tissue, and prepared for analysis under a light microscope.
The specimens were fixed in 4% formaldehyde buffered with 0.1 M sodium phosphate and pH 7.2 for 48 h at ambient temperature. Later, the specimens were dehydrated and embedded in paraffin. Longitudinal 6-μm-thick sections were adhered to glass slides and stained with hematoxylin and eosin (HE). Histopathological analysis was performed in accordance with the following parameters: number of inflammatory and fibroblast cells, measurement of capsule thickness, presence of multinucleated giant cells, and areas of necrosis. For this analysis, images were captured with the use of a microscope (BX51, Olympus, Tokyo, Japan).
The number of inflammatory (IC) and fibroblast (Fb) cells in the capsule adjacent to the implants was measured. Three sections from each animal (× 40 magnification) were quantified, maintaining a minimum interval of 100 μm between the sections. Afterwards, an image analysis program (Image-Pro Express 6.0, Olympus – Japan) was used to count the inflammatory and fibroblast cells in each section. A mean value was established for each experimental group according to the experimental time interval and material studied. Furthermore, in three sections, in images captured with a × 20 objective, the thickness of the connective tissue capsule was measured. For these parameters, in accordance with the ISO Standard 7405 [13] and criteria of other studies [14,15,16], scores were established (Table 1) for histopathological analysis.
Statistical analysis
Data were submitted to statistical analysis using GraphPad Prism 5 (GraphPad Software, San Diego, CA, USA) software. The Kruskal-Wallis test followed by the Dunn test was performed, considering the level of significance of 5%.
Results
Cytotoxicity
In the 24-h time interval, we could verify that all the concentrations of calcium hydroxide (H) and amoxicillin (A) were similar to those of the positive control. For ibuprofen (I), the concentrations 1%, 0.1%, and 0.01% demonstrated higher viability values when compared with those of the positive control group (p ≤ 0.05); in diclofenac group (D), the 1% concentration presented higher cell viability values (p < 0.001). After 48 h, all pastes demonstrated cell viability similar to positive control group except for D and A 10% that presented lower values (p < 0.05). At 72 h, H 10%, I 10%, I 1%, and A 10% present cell viability values significantly reduced in comparison to other groups (p ≤ 0.05). In the 7-day period, means of all the concentrations of D and A were similar to positive control. In contrast, Ca (OH)2 with ibuprofen present lower cell viability (p ≤ 0.05). In all the time intervals, the negative control presented significant difference, demonstrating low viability values and even cell death (p < 0.0001), when compared with the positive control group (Table 2).
Tissue reaction
The tissue reaction induced by the different groups may be observed in Fig. 1, and the comparisons among the histological parameters are shown in Table 3. At 7 days, there was a large quantity of IC, particularly neutrophils and multinucleated giant cells in the capsules. After 30 days, a gradual and significant reduction in the inflammatory process was seen, accompanied by an increase in the number of Fb in all the groups (p ≤ 0.05).
Light micrographs of sections showing portions of capsules adjacent to the opening of the tubes implanted (I) in the subcutaneous after 7 (a–e) and 30 (f–j) days of implantation. a–e Capsules show numerous inflammatory cells (arrows) and superficial necrosis (asterisks) adjacent to the calcium hydroxide paste groups (a–d). After 30 days (f–j), typical fibroblasts (Fb) are observed among bundles of collagen fibers (Cf) in the capsules; few inflammatory cells (arrows) are presented. Bv, blood vessels. HE. Bars 40 μm
Comparison among the materials showed that the calcium hydroxide pastes induced a severe inflammatory reaction at 7 days. However, after 30 days, a significantly lower number of IC was shown in the tissue adjacent to the calcium hydroxide paste with diclofenac in comparison with the other medications (p < 0.001). Furthermore, in this group, at 30 days, no statistical differences were observed in the quantity of fibroblasts in comparison with the control (p = 0.08). The pure calcium hydroxide paste, with ibuprofen or amoxicillin, induced a severe inflammatory reaction (score 4) at 7 days and moderate (score 3) after 30 days of implantation in rat subcutaneous tissues.
The capsule thickness was thicker at 7 days while it was classified as thin at 30 days in all the experimental groups. Moreover, superficial necrosis was observed in close contact with the different calcium hydroxide pastes after 7 days (Table 3).
Discussion
The Ca (OH)2 pastes used as intracanal medications remained in direct contact with the apical and periapical tissues, and therefore, must not have been cytotoxic or irritating to these tissues. In vitro cytotoxicity methods, such as those used in the present research, may be influenced by the type of cells and method used [17, 18]. Therefore, complementary analyses are required for studying the biological response of endodontic materials. Implantation in rat subcutaneous tissues is a widely used method for evaluating the type and extension of inflammatory reaction [15, 16]. In this study, the histopathological analysis evaluated the initial inflammatory response, and the capacity for regression of this process induced by the different materials after 30 days.
Our in vitro results showed that all the Ca (OH)2 pastes present low cytotoxicity in all the experimental time intervals and dilutions. Although some concentrations showed decreased cell viability when compared to positive control at 24, 48, and 72 h, after 7 days, the values of all groups were similar. These findings agree with other studies which demonstrated that materials containing Ca (OH)2 are not cytotoxic [1, 2, 19]. So, the use of these pastes has been recommended in regenerative procedures because they increase cell viability in comparison with other medications, such as tri-antibiotic paste, for example [19].
The data obtained by in vivo analysis showed that the calcium hydroxide pastes induced an intense, severe inflammatory reaction at 7 days, with areas of necrosis in close contact with these materials. At 30 days, the inflammatory process regressed, and consequently, the number of fibroblasts and collagen fibers in the capsules increased. Ca (OH)2 has an alkaline pH that promotes the formation of superficial zones of necrosis when in contact with the tissues [20, 21]. The necrotic cells induce migration of neutrophils and multinucleated giant cells to promote phagocytosis initially, enabling tissue repair in longer experimental periods [20, 22, 23]. This mechanism of action could be reinforced by our findings, considering that at 30 days, no zones of necrosis or giant cells were observed in the capsules in contact with the Ca (OH)2 pastes.
Comparison among the materials showed that the drugs associated with Ca (OH)2 paste interfered in the in vivo biological response, because there were statistical differences in the histological parameters evaluated, especially at 30 days. In this period, a reduced number of IC and larger quantity of Fb were observed in the tissue adjacent to the Ca (OH)2 with diclofenac sodium, than those in contact with the mixtures with amoxicillin and ibuprofen. Moreover, the paste with diclofenac sodium induced a less intense inflammatory action than that induced by the pure Ca (OH)2. Furthermore, considering that the association of Ca (OH)2 with diclofenac promoted cell viability, this mixture presented promising biological behavior both in vitro and in vivo. Studies have demonstrated that drugs used in medicine containing diclofenac sodium are not cytotoxic to L929 cell lines and reduce the inflammatory process 30 days after implantation in rats [24].
The Ca (OH)2 pastes with ibuprofen or amoxicillin induced a moderate inflammatory reaction at 30 days, characterized by a higher number of IC and a reduced quantity of Fb in comparison with the paste with diclofenac. However, the severe inflammation at 7 days became moderate at 30 days. Considering that biocompatible materials are those that allowed reduction in the inflammatory process in longer experimental time intervals [25], the mixtures with amoxicillin or ibuprofen presented adequate biological properties. Moreover, these pastes also promoted cell viability in the MTT test, reinforcing their good biological behavior.
Despite our findings indicate promising results related to Ca (OH)2 paste associated with amoxicillin, it is well known that bacteria responsible for endodontic infections develop resistance to the antibiotics. Furthermore, another problem is the risk of provoked allergic reactions to patients previously sensitized or to sensitize patients who had not previously been in contact with that antibiotic [26].
A previous study has demonstrated the anti-biofilm activity of Ca (OH)2 paste associated with different drugs, particularly with diclofenac sodium [7]. Nevertheless, the present research was the first to analyze the cytotoxicity and biocompatibility of these mixtures. Although the results found were promising, the analysis of other physicochemical properties is necessary for indicating their use in clinical practice.
In conclusion, Ca (OH)2 pastes associated with anti-inflammatory or antibiotic are not cytotoxic and present biocompatibility, so, may be clinical alternatives as intracanal medication to reduce the number of microorganisms in root canal system.
References
Desai S, Chandler N (2009) Calcium hydroxide–based root canal sealers: a review. J Endod 35:475–480
Mizuno M, Banzai Y (2008) Calcium ion release from calcium hydroxide stimulated fibronectin gene expression in dental pulp cells and the differentiation of dental pulp cells to mineralized tissue forming cells by fibronectin. Int Endod J 41:933–938
Siqueira JF, Lopes HP (1999) Mechanisms of antimicrobial activity of calcium hydroxide: a critical review. Int Endod J 32:361–369
Tanomaru JM, Leonardo MR, Tanomaru Filho M, Bonetti-Filho I, Silva LA (2003) Effect of different irrigation solutions and calcium hydroxide on bacterial LPS. Int Endod J 36:733–739
Pinheiro ET, Gomes BP, Ferraz CCR, Sousa EL, Teixeira FB, Souza-Filho FJ (2003) Microorganisms from canals of root-filled teeth with periapical lesions. Int Endod J 36:1–11
Valverde ME, Baca P, Ceballos L, Fuentes MV, Ruiz-Linares M, Ferrer-Luque CM (2017) Antibacterial efficacy of several intracanal medicaments for endodontic therapy. Dent Mater J 36:319–324
Freitas RP, Greatti VR, Alcalde MP, Cavenago BC, Vivan RR, Duarte MAH, Weckwerth ACV, Weckwerth PH (2017) Effect of the association of nonsteroidal anti-inflammatory and antibiotic drugs on antibiofilm activity and pH of calcium hydroxide pastes. J Endod 43:131–134
Dastidar SG, Ganguly K, Chaudhuri K, Chakrabarty AN (2000) The anti-bacterial action of diclofenac shown by inhibition of DNA synthesis. Int J Antimicrob Agents 14:249–251
Salem-Milani A, Balaei-Gajan E, Rahimi S, Moosavi Z, Abdollahi A, Zakeri-Milani P, Bolourian M (2013) Antibacterial effect of diclofenac sodium on Enterococcus faecalis. J Dent (Tehran) 10:16–22
ISO-1993-6 (2009) Biological evaluation of medical devices - part 5: tests for in vitro cytotoxicity. International Standards Organization, Switzerland, pp 1–34
Mossman T (1983) Rapid colorimetric assay for cellular growth and survival: application to proliferation and cytotoxicity assays. J Immunol Methods 65:55–63
Oliveira FA, Matos AA, Santesso MR, Tokuhara CK, Leite AL, Bagnato VS, Machado MA, Peres-Buzalaf C, Oliveira RC (2016) Low intensity lasers differently induce primary human osteoblast proliferation and differentiation. J Photochem Photobiol B 163:14–21
ISO-7405 (2008) Evaluation of biocompatibility of medical devices used in dentistry. International Standards Organization, Switzerland, pp 1–34
Stanford JW (1986) Recommendations for determining biocompatibility and safety for the clinical use of metals in dentistry. Int Dent J 36:45–48
Taha NA, Safadi RA, Alwedaie MS (2016) Biocompatibility evaluation of EndoSequence root repair paste in the connective tissue of rats. J Endod 42:1523–1528
Cintra LTA, Benetti F, Queiroz IOA, Ferreira LL, Massunari L, Bueno CRE, de Oliveira SHP, Gomes-Filho JE (2017) Evaluation of the cytotoxicity and biocompatibility of new resin epoxy–based endodontic sealer containing calcium hydroxide. J Endod 43:2088–2092
Tronstad L, Wennberg A (1980) In vitro assessment of the toxicity of filling materials. Int Endod J 13:131–138
Peters OA (2013) Research that matters: biocompatibility and cytotoxicity screening. Int Endod J 46:195–197
Althumairy RI, Teixeira FB, Diogenes A (2014) Effect of dentin conditioning with intracanal medicaments on survival of stem cells of apical papilla. J Endod 40:521–525
Holland R, Pinheiro CE, Mello W, Nery MJ, Souza V (1982) Histochemical analysis of the dogs dental pulp after pulp capping with calcium, barium, and strontium hydroxides. J Endod 8:444–447
Estrela C, Sydney GB, Bammann LL, Felippe-Júnior O (1995) Mechanism of action of calcium and hydroxyl ions of calcium hydroxide on tissue and bacteria. Braz Dent J 6:85–90
Faria G, Celes MRN, Rossi A, Silva LAB, Silva JS, Rossi MA (2007) Evaluation of chlorhexidine toxicity injected in the paw of mice and added to cultured L929 fibroblasts. J Endod 33:715–722
Andolfatto C, da Silva GF, Cornélio AL, Guerreiro-Tanomaru JM, Tanomaru-Filho M, Faria G, Bonetti-Filho I, Cerri PS (2012) Biocompatibility of intracanal medications based on calcium hydroxide. ISRN Dent 2012:904963
Jayant RD, McShane MJ, Srivastava R (2011) In vitro and in vivo evaluation of anti-inflammatory agents using nanoengineered alginate carriers: towards localized implant inflammation suppression. Int J Pharm 403:268275
Silveira CM, Pinto SC, Zedebski Rde A, Santos FA, Pilatti GL (2011) Biocompatibility of four root canal sealers: a histopathological evaluation in rat subcutaneous connective tissue. Braz Dent J 22:21–27
Montero-Miralles P, Martín-González J, Alonso-Ezpeleta O, Jiménez-Sánchez MC, Velasco-Ortega E, Segura-Egea JJ (2018) Effectiveness and clinical implications of the use of topical antibiotics in regenerative endodontic procedures: a review. Int Endod J 51:981–988
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All applicable international, national, and/or institutional guidelines for the care and use of animals were followed.
Informed consent
For this type of study, formal consent is not required.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
da Silva, G.F., Cesário, F., Garcia, A.M.R. et al. Effect of association of non-steroidal anti-inflammatory and antibiotic agents with calcium hydroxide pastes on their cytotoxicity and biocompatibility. Clin Oral Invest 24, 757–763 (2020). https://doi.org/10.1007/s00784-019-02923-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-019-02923-y