Abstract
Objectives
A narrative review on the potential use of low-dose protocols for cone beam computed tomography (CBCT) was conducted to identify indications and their relevance for various dental disciplines.
Materials and methods
Google Scholar was searched using the words “low-dose CBCT”. Reviews, consensus papers, clinical studies, and experimental studies were eligible for the initial screening process, but for data extraction only original articles were selected. Similar search procedures were then performed with the additional search words “pedo,” “ortho,” “endo,” “implant,” “perio,” and “oral surgery.” Furthermore, references of included articles were examined to identify further relevant articles.
Results
After screening, 27 publications remained for the data extraction process. Low-dose protocols have been reported for specialties such as pediatric dentistry (evaluating orofacial clefts, periapical lesions, impacted teeth, and autotransplantation), orthodontics (cephalometric analysis and interim assessment of treatment results), endodontics (detecting root fractures, resorptions and periapical bone loss), implant dentistry (planning implant insertion, evaluating peri-implant fenestration and dehiscence), periodontology (assessing periodontal structures), and oral and maxillofacial surgery (assessing mandibular third molars and TMJs). Nevertheless, most of the literature available is related to non-clinical studies. Furthermore, there is a lack of position statements or guidelines from authoritative bodies regarding the use of low-dose protocols in dental medicine.
Conclusions
Low-dose protocols for CBCT imaging seem to have potential in various disciplines in dental medicine ranging from pediatric dentistry to oral and maxillofacial surgery. Dose reduction is usually achieved by mAs reduction, use of partial rotations, reduced number of projections, and larger voxel sizes, but seldom by kV reduction.
Clinical relevance
Albeit low-dose protocols have potential to result in a reduction of dose exposure for 3D imaging due to dental indications, there is a need to more clearly specify indications and limitations to avoid indiscriminate use of standard and high-dose CBCT scans in the future on the lines of ALARA/ALADA principles.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The initial description and introduction of cone beam computed tomography (CBCT) for use in dental medicine took place over two decades ago by an Italian group from Verona [1]. Since then, CBCT has had a great impact in diagnostic imaging and treatment planning in various dental specialties ranging from oral surgery to orthodontics. CBCT machines and their accompanying software have provided a relatively fast and convenient way to acquire and output three-dimensional (3D) multiplanar images, for which the scans can be taken in a supine, standing or seated position [2, 3]. CBCT imaging has become widely available and easily accessible to a large number of users in universities, dental hospitals, and also in dental practice. Nevertheless, CBCT scans have a significantly higher radiation dose than other conventional two-dimensional (2D) imaging modalities in dental medicine (e.g., intra-oral, panoramic, and cephalometric radiography). Therefore, various authoritative bodies have issued position statements or guidelines that detail the use of CBCT for specific circumstances in numerous dental disciplines, with some of the examples listed below:
-
The European Academy of Dental and Maxillofacial Radiology (EADMFR) [4] and the Swiss Association of Dentomaxillofacial Radiology (SADMFR) [5, 6] regarding the use of CBCT in general.
-
The SEDENTEXCT project which produced the European Commission guidelines that served as a basis for national guidelines worldwide [7];
-
The “Dentomaxillofacial paediatric imaging: an investigation towards low-dose radiation induced risks” (DIMITRA) group regarding paediatric dentistry [8];
-
The American Academy of Oral and Maxillofacial Radiology (AAOMR) regarding orthodontics [9];
-
The European Society of Endodontology (ESE) and the AAOMR/American Association of Endodontists (AAE) regarding endodontology [10, 11];
-
The American Academy of Periodontology (AAP) regarding periodontology [12];
-
The European Association for Osseointegration (EAO), the International Congress of Oral Implantologists (ICOI) and the International Team for Implantology (ITI) regarding implant dentistry [13,14,15]
The 3D visualization of oral and maxillofacial structures by CBCT images provides information for diagnosis, treatment planning, and follow-up. For example for pediatric dentistry, CBCT scans help in evaluating orofacial clefts and in planning autotransplantation procedures [8]. For orthodontics, it is recommended to consider taking CBCT scans to plan orthognathic surgeries and correct jaw asymmetry [9]. For endodontology, a CBCT scan using a limited field-of-view (FOV) is considered an adjunctive imaging modality to diagnose periapical pathology, where periapical radiographs are not conclusive, examine extended dento-alveolar trauma, and assess complex root canal anatomy/calcified canals before commencing endodontic treatment or to plan periradicular surgery [10, 11]. For periodontology, the available literature is limited, but an accepted indication is the assessment of furcation defects to support the selection of an adequate treatment modality [12]. For implant dentistry, CBCT helps in implant treatment planning by evaluating bone dimensions and to assess the need for augmentative procedures (simultaneous or staged), and the health or pathology of the maxillary sinus [13, 14].
With regard to the versatility and increasing popularity of CBCT imaging in dental medicine, evidence is pointing towards indication-oriented and patient-specific imaging [8], and highlights the concept of dose optimization [16], which will be discussed initially in the present review. Then, special emphasis will be given to review the use of novel low-dose protocols with CBCT imaging, and to provide clinical recommendations on the basis of the literature identified and presented.
Radiation dose exposure and aspects of dose protection
Radiation doses are reported to be relatively low for conventional 2D imaging in dentistry, whether they stem from intra- or extraoral methods [17]. Through the increasing popularity of 3D imaging with CBCT exposing patients to higher doses than 2D imaging, radiation dose protection has become more and more relevant and a focus of attention in dental medicine in recent years [5, 6]. One fundamental aspect to radiation dose protection is the implementation of the “as low as reasonably achievable (ALARA)” principle, coined by the International Commission on Radiological Protection (ICRP) in 1977 [18]. In 2014, the National Council on Radiation Protection and Measurements (NCRP) has proposed a shift from ALARA to ALADA (“as low as diagnostically acceptable”), to emphasize the importance of dose optimization in medical diagnostic imaging [16]. Such a shift is also advocated for dental CBCT, as CBCT is recommended as a supplementary imaging technique where conventional 2D dental radiography fails to provide enough diagnostic information, instead of being a tool that simply provides “pretty pictures” [16].
Each CBCT machine has different and device-specific FOVs, which can be roughly divided into large, medium, and small [13, 19]. Ideally, the FOV should be fully adjustable, meaning that the FOV is totally patient-specific and indication-oriented to fulfill the principle of optimization [8]. However, such technology is yet to be commercially available. A large FOV (e.g., diameter × height usually larger than 10 × 10 cm) captures the maxillofacial structures beyond the oral cavity and maxillary sinus floor. Meanwhile, a medium FOV (e.g., between 8 × 5 and 10 × 10 cm) captures dentoalveolar regions including one entire or even both jaws. Finally, a small FOV (e.g., below 8 × 5 cm) captures a localized area of several adjacent teeth with their periapical region [15, 19]. To test the exact effective radiation dose (Sv) of CBCT machines with different devices and imaging protocols, phantom heads have been used to simulate average adult males [19]. Results have shown a wide range of effective doses stemming from CBCT scans: 52–1410 μSv for a large FOV, 18–674 μSv for a medium FOV, 11–252 μSv for a small FOV, and 7–769 μSv for child protocols [15]. When comparing these values to effective doses reported for 2D extra-oral radiography in dentistry, the minimal value for a CBCT (11 μSv) is comparable to 0.2–2.0 times of a dental panoramic view, or 1.0–5.5 times of a cephalometric image [15]. Meanwhile, the range of effective doses for CBCT is usually lower than that of spiral CT in the context of orofacial imaging [20, 21].
Compared to medical radiology, this minimal value of 11 μSv is similar to the average effective dose from a knee radiograph, while the maximal value (1410 μSv) is comparable to a thoracic spine projection including an AP and lateral view [17]. Nevertheless, the maximal value for CBCT scanning is still below the average effective dose for a head CT (2000 μSv) or head angiography (5000 μSv) [17], though certain examinations such as a sinus CT can have a lower effective dose of 200 μSv [22]. Because of this variability in effective doses for a single imaging modality, the basic principles of radiation protection are of paramount importance. Thus, special consideration to justification and dose optimization for each CBCT taken should be given.
Justification is based on the principle that the use of radiation is expected to result in more benefits than harm to the patient [13]. Alternative modalities that involve less or even no radiation exposure (e.g., ultrasonography or magnetic resonance imaging) should also be considered whenever deemed appropriate. Meanwhile, dose optimization can be observed by confirming with the prescribing dentist regarding the FOV and resolution selection whenever in doubt, and monitoring or adapting scanning parameters chosen according to the patient exposed to radiation (for example, child versus adult). In addition, the use of thyroid shielding around the front neck could reduce the effective dose received by the thyroid gland and esophagus to one-third regardless of large, medium, or small FOVs [23].
Certain groups are at a higher risk upon radiation exposure, such as children and the embryo or fetus of pregnant women. Children have a larger lifetime attributable cancer mortality risk per dose unit [24]. Moreover, a recent article has estimated the lifetime attributable risk of radiation-induced cancer due to dental exposures for boys and girls, and concluded that girls generally have a higher risk than boys [25]. Meanwhile, there is always a concern about the radiation risk to the embryo or fetus of pregnant women, with the potential effects being prenatal death, intrauterine growth restriction, reduced head size, mental retardation, organ malformation and cancer [26]. However, consensus is lacking on the issue of radiation protection [27], and thus it is still very important to consider dose reduction whenever applicable. A prospective study using pediatric phantoms has reported that large FOVs would lead to a significantly higher dose for the brain and thyroid [28]. Therefore, one future direction could be the implementation of adaptable FOV for which the size and position are optimized according to the indication and patient [8].
Low-dose protocols can be defined as procedures that lower exposure factors without an unacceptable loss of image quality for diagnostic purposes [29]. Low-dose protocols have also been introduced for dento-maxillofacial imaging using CT scanning [30]. Nevertheless, as CBCT is more easily available and accepted for dental purposes and private practitioners, the present review will focus on CBCT only. After determining an optimized FOV for a particular patient, a CBCT scan can be acquired with even further lower radiation doses, by either using dose reduction settings pre-set by the manufacturers or adjusting imaging parameters for which the CBCT machine allows manually. Generally, so-called low-dose protocols may be achieved by reducing the tube current (mA), scan time (s), resolution (i.e., increasing voxel size), the number of projections, and/or adopting a partial rotation mode (e.g., 180° instead of 360° rotation) [13].
In recent years, several CBCT manufacturers have incorporated features into their machines to accommodate and facilitate image acquisition by low-dose protocols which allow easier dose optimization [31]. For instance, the newer generations of ProMax 3D devices (Planmeca Oy, Helsinki, Finland) have an “ultra low-dose (ULD)” mode that optimizes and reduces the tube current and scan time. The CS 9300 machines (Carestream, New York, USA) have a “low-dose mode” button that serves the same function. Furthermore, Accuitomo and Veraview machines (J. Morita Mfg. Corp., Kyoto, Japan) allow users to choose a 180° instead of a 360° rotation, and to reduce the tube current (ranging from 2 to 10 mA). Through the reduction of FOV height and angle of rotation, the radiation dose including the dose to the eye lens can be significantly reduced [32]. Depending on the machine, it was reported that the doses for the same FOV could have up to 15-fold difference between low-dose and high-resolution protocols [33]. Besides manual reduction of the tube current, tube current modulation is also very efficient in achieving a patient-specific dose optimization via body size estimation with initial scout images [34], which is implemented by VGI evo machines (NewTom, Verona, Italy).
As kV determines the image contrast by relating to the penetrating power of the x-ray beam generated from the CBCT machine, it is said that dose reduction through reducing mA can still retain the image quality [35]. Meanwhile, lowering the resolution (by increasing the voxel size) seems not to have a clear effect on the diagnostic value of CBCT images [36]. In other words, lowering the resolution for CBCT imaging may be an integral part of a low-dose protocols, while keeping the images “diagnostically acceptable” (ALADA). The utilization of low-dose protocols for specific aspects and specialties in dental medicine will be described in the next chapter.
Current use of low-dose protocols for CBCT in various disciplines of dental medicine
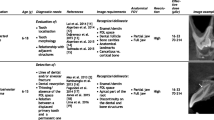
Since the current review has been designed as a narrative review using a standardized approach for gathering the relevant literature and not as a true systematic review, the following search strategy has been applied by the first author. First, Google Scholar was searched using the words “low-dose CBCT” (without quotations, thus not limiting to publications with the exact phrase). Reviews, consensus papers, clinical studies, and experimental (phantom and cadaver) studies were eligible for the initial screening process, but for data extraction only original papers were selected. Similar search procedures were then performed with the additional search words “pedo,” “ortho,” “endo,” “implant,” “perio,” and “oral surgery.” Furthermore, references of included articles were examined to identify further relevant articles. Lastly, the senior authors were consulted for additional references. As a result, approximately 700 publications were initially screened, 100 from the general search, and 100 each per specialty field. After screening, 27 publications remained (details provided in Tables 1, 2, 3, 4, and 5). Of these, 3 publications were related to pediatric dentistry, 4 to orthodontics, 6 to endodontics, 10 to implant dentistry, 1 to periodontology, and 3 to oral and maxillofacial surgery.
For pediatric patients, the Image Gently in Dentistry campaign supported the use of half-scan modes as a general rule for taking CBCT scans for pediatric patients [16]. Table 1 lists the use of low-dose protocols for specific indications in pediatric dentistry. The DIMITRA group has advocated the use of low-dose protocols specifically to evaluate orofacial clefts, inflammatory periapical lesions and dentigerous cysts [8]. Nevertheless, there has been no clinical study on low-dose protocols in pediatric dentistry. Meanwhile, Rivas et al. [29] have recommended reducing the kV and mA, to evaluate impacted maxillary canines. Besides, EzEldeen and co-workers have recommended the use of the ULD mode of the ProMax 3D machine for preoperative and postoperative evaluation of a planned autotransplantation [37].
For orthodontic patients, there is no position statement on the use of low-dose protocols (Table 2). However, Brown et al. [38] (based on experimental data from dry skulls) and Kusnoto et al. [40] (based on clinical CBCT data) recommended reducing the exposure time (and thus reducing the number of projections) when CBCT images are acquired for cephalometric analysis, though it should be noted that 2D, instead of 3D, cephalometric analysis is still the norm. Meanwhile, 3D cephalometrics was also done with images acquired from several CBCT devices using lower resolution and/or lower-dose scan modes [41].
For endodontic patients, there is no position statement or clinical evaluation on the use of low-dose protocols available (Table 3). Results from in vitro studies have shown that for detection of external root resorption, diagnostically acceptable dose reduction can be achieved by using a half-scan [43], and also by applying an increased voxel size [36]. Half-scans can also be used to detect periapical bone loss [45], root fractures [35, 42], and perform endodontic measurements [44].
For implant patients, there is currently no position statement or official guideline on the use of low-dose protocols for treatment planning or follow-up imaging procedures (Table 4). Dawood et al. [47] conducted a retrospective clinical study and concluded that reducing the mA and exposure time and the use of a half-scan can be used for implant planning without any loss in diagnostic value or efficacy for treatment planning purposes. These findings are largely confirmed by multiple studies using skulls or cadavers (Table 4). With regard to the detection of peri-implant bone loss, dose reduction to diagnose fenestration- and dehiscence-type defects can be achieved by using larger voxel sizes, and for fenestrations a half-scan is recommended [48].
Publication on low-dose protocols for periodontology and oral and maxillofacial surgery are still rare (Table 5). To assess periodontal structures, dose reduction can be achieved by reducing the kV and mA [56]. Similarly, mA and exposure time can be reduced for visualizing third molars [57, 58]. A half-scan has been mentioned to be adequate for detecting degenerative changes of the temporomandibular joints (TMJ) [59].
It should be noted that the stated values for kV, mA and other exposure parameters depend on the individual CBCT machine used by the reported studies, and are not directly generalizable to all machines.
Clinical recommendations and conclusions
Most of the publications available supporting the use of low-dose protocols for various indications in dental medicine largely stem from benchmarking studies that involve cadavers, dry skulls, and phantom heads. As a result, most of the existing evidence may not have the highest level of methodological quality or clinical relevance. Notwithstanding, there is a consensus that the FOV size and location are major determinants of the effective dose, and thus the optimization of other imaging parameters should be done on the basis of FOV selection [31].
As the current evidence mainly came from non-clinical data, future research should primarily evaluate the possibilities and limitations of low-dose protocols using CBCT data from a clinical perspective. One future research direction is to produce multiple CBCT data sets, from a single patient scan, to simulate multiple scans of the same patient using different dose reduction settings. By doing so, the ethical issue of scanning a patient multiple times can be circumvented, while clinicians can evaluate the (simulated) effect of low-dose protocols on clinical data instead of data from phantoms or cadavers. This can be achieved by means of altering the reconstruction algorithm, which is similar to the method used by Kusnoto et al. [40]. Another direction is to retrospectively evaluate the diagnostic quality of existing CBCT data sets, such as proposed by Dawood et al. [47]. Moreover, the CBCT machines in the market have different options for users to change the imaging parameters. After basic confirmation of the efficacy or usefulness of low-dose protocols in practice, the applied studies should validate these results using and directly comparing various CBCT devices available on the market, so that users can directly apply these dose optimization protocols to their clinical practice. A recent review has concluded that there are 13 factors that relate to differences in the effective dose emitted by various CBCT scanners, listed as follows: (1) device-based—scan angle, additional copper filter, FOV diameter, FOV height, kV, mA, exposure time, mAs, voxel, and resolution; (2) non-device-based—patient size, region of interest, and use of thyroid shield [60]. As Jacobs et al. [20] have advocated, CBCT protocols should be both “patient-specific” and “indication-oriented,” meaning that the FOV, resolution and radiation dose should depend on patient’s age and anatomy and the diagnostic/therapeutic requirements.
Based on the present review of the available literature, the following statements can be made with regard to the use of low-dose protocols for CBCT in dental medicine:
-
A low-dose protocol should be considered in various disciplines in dental medicine, specifically:
-
Pediatric dentistry (for indications such as evaluation of orofacial clefts, periapical lesions, impacted teeth, and prior to autotransplantation),
-
Orthodontics (cephalometric analysis and interim assessment of treatment results),
-
Endodontics (detecting root fractures, resorptions and periapical bone loss),
-
Implant dentistry (planning implant insertion, evaluating peri-implant bone loss), and
-
Oral and maxillofacial surgery (assessing mandibular third molars and TMJs).
-
-
Dose reduction is usually achieved by mAs reduction, use of partial rotations, reduced number of projections, and larger voxel size, but seldom by kV reduction.
-
Most of the publications on low-dose protocols using CBCT imaging are non-clinical studies.
-
There is a lack of position statements, clinical recommendations, or guidelines from authoritative bodies regarding the use of low-dose protocol in dental medicine.
References
Mozzo P, Procacci C, Tacconi A, Martini PT, Andreis IB (1998) A new volumetric CT machine for dental imaging based on the cone-beam technique: preliminary results. Eur Radiol 8:1558–1564
Scarfe WC, Farman AG, Sukovic P (2006) Clinical applications of cone-beam computed tomography in dental practice. J Can Dent Assoc 72:75–80
Nemtoi A, Czink C, Haba D, Gahleitner A (2013) Cone beam CT: a current overview of devices. Dentomaxillofac Radiol 42:20120443
Horner K, Islam M, Flygare L, Tsiklakis K, Whaites E (2009) Basic principles for use of dental cone beam computed tomography: consensus guidelines of the European Academy of Dental and Maxillofacial Radiology. Dentomaxillofac Radiol 38:187–195
Dula K, Bornstein MM, Buser D, Dagassan-Berndt D, Ettlin DA, Filippi A, Gabioud F, Katsaros C, Krastl G, Lambrecht JT (2014) SADMFR guidelines for the use of cone-beam computed tomography/digital volume tomography. Swiss Dent J 124:1169–1183
Dula K, Benic GI, Bornstein M, Dagassan-Berndt D, Filippi A, Hicklin S, Kissling-Jeger F, Luebbers H-T, Sculean A, Sequeira-Byron P (2015) SADMFR guidelines for the use of cone-beam computed tomography/digital volume tomography. Swiss Dent J 125:945–953
European Commission (2012) Cone beam CT for dental and maxillofacial radiology (evidence-based guidelines). Radiation Protection No 172. https://ec.europa.eu/energy/sites/ener/files/documents/172.pdf. Accessed 8 June 2018
Oenning AC, Jacobs R, Pauwels R, Stratis A, Hedesiu M, Salmon B, Group DR (2018) Cone-beam CT in paediatric dentistry: DIMITRA project position statement. Pediatr Radiol 48:308–316
Evans CA, Scarfe WC, Ahmad M, Cevidanes LH, Ludlow JB, Palomo JM, Simmons KE, White SC (2013) Clinical recommendations regarding use of cone beam computed tomography in orthodontics. Position statement by the American Academy of Oral and Maxillofacial Radiology. Oral Surg Oral Med Oral Pathol Oral Radiol 116:238–257
Patel S, Durack C, Abella F, Roig M, Shemesh H, Lambrechts P, Lemberg K (2014) European Society of Endodontology position statement: the use of CBCT in endodontics. Int Endod J 47:502–504
Fayad MI, Nair M, Levin MD, Benavides E, Rubinstein RA, Barghan S, Hirschberg CS, Ruprecht A (2015) AAE and AAOMR joint position statement: use of cone beam computed tomography in endodontics 2015 update. Oral Surg Oral Med Oral Pathol Oral Radiol 120:508–512
Kim DM, Bassir SH (2017) When is cone-beam computed tomography imaging appropriate for diagnostic inquiry in the management of inflammatory periodontitis? An American Academy of Periodontology best evidence review. J Periodontol 88:978–998
Harris D, Horner K, Gröndahl K, Jacobs R, Helmrot E, Benic GI, Bornstein MM, Dawood A, Quirynen M (2012) E.A.O. guidelines for the use of diagnostic imaging in implant dentistry 2011. A consensus workshop organized by the European Association for Osseointegration at the Medical University of Warsaw. Clin Oral Implants Res 23:1243–1253
Benavides E, Rios HF, Ganz SD, An C-H, Resnik R, Reardon GT, Feldman SJ, Mah JK, Hatcher D, Kim M-J (2012) Use of cone beam computed tomography in implant dentistry: the International Congress of Oral Implantologists consensus report. Implant Dent 21:78–86
Bornstein MM, Scarfe WC, Vaughn VM, Jacobs R (2014) Cone beam computed tomography in implant dentistry: a systematic review focusing on guidelines, indications, and radiation dose risks. Int J Oral Maxillofac Implants 29:55–77
White SC, Scarfe WC, Schulze RK, Lurie AG, Douglass JM, Farman AG, Law CS, Levin MD, Sauer RA, Valachovic RW (2014) The image gently in dentistry campaign: promotion of responsible use of maxillofacial radiology in dentistry for children. Oral Surg Oral Med Oral Pathol Oral Radiol 118:257–261
Mettler FA Jr, Huda W, Yoshizumi TT, Mahesh M (2008) Effective doses in radiology and diagnostic nuclear medicine: a catalog. Radiology 248:254–263
Hendee WR, Edwards FM (1986) ALARA and an integrated approach to radiation protection. Semin Nucl Med 16:142–150
Pauwels R, Beinsberger J, Collaert B, Theodorakou C, Rogers J, Walker A, Cockmartin L, Bosmans H, Jacobs R, Bogaerts R (2012) Effective dose range for dental cone beam computed tomography scanners. Eur J Radiol 81:267–271
Jacobs R, Salmon B, Codari M, Hassan B, Bornstein MM (2018) Cone beam computed tomography in implant dentistry: recommendations for clinical use. BMC Oral Health 18:88
Guerrero ME, Jacobs R, Loubele M, Schutyser F, Suetens P, van Steenberghe D (2006) State-of-the-art on cone beam CT imaging for preoperative planning of implant placement. Clin Oral Investig 10:1–7
Van der Molen A, Schilham A, Stoop P, Prokop M, Geleijns J (2013) A national survey on radiation dose in CT in the Netherlands. Insights Imaging 4:383–390
Qu X, Li G, Zhang Z, Ma X (2012) Thyroid shields for radiation dose reduction during cone beam computed tomography scanning for different oral and maxillofacial regions. Eur J Radiol 81:e376–e380
Brenner DJ, Elliston CD, Hall EJ, Berdon WE (2001) Estimated risks of radiation-induced fatal cancer from pediatric CT. AJR Am J Roentgenol 176:289–296
Jacobs R, Pauwels R, Scarfe WC, De Cock C, Dula K, Willems G, Verdonck A, Politis C (2018) Pediatric cleft palate patients show a 3-to 5-fold increase in cumulative radiation exposure from dental radiology compared with an age-and gender-matched population: a retrospective cohort study. Clin Oral Investig 22:1783–1793
McCollough CH, Schueler BA, Atwell TD, Braun NN, Regner DM, Brown DL, LeRoy AJ (2007) Radiation exposure and pregnancy: when should we be concerned? Radiographics 27:909–917
Kelaranta A, Ekholm M, Toroi P, Kortesniemi M (2015) Radiation exposure to foetus and breasts from dental X-ray examinations: effect of lead shields. Dentomaxillofac Radiol 45:20150095
Marcu M, Hedesiu M, Salmon B, Pauwels R, Stratis A, Oenning ACC, Cohen ME, Jacobs R, Baciut M, Roman R (2018) Estimation of the radiation dose for pediatric CBCT indications: a prospective study on ProMax3D. Int J Paediatr Dent 28:300–309
Hidalgo Rivas JA, Horner K, Thiruvenkatachari B, Davies J, Theodorakou C (2015) Development of a low-dose protocol for cone beam CT examinations of the anterior maxilla in children. Br J Radiol 88:20150559
Widmann G, Bischel A, Stratis A, Bosmans H, Jacobs R, Gassner E-M, Puelacher W, Pauwels R (2017) Spatial and contrast resolution of ultralow dose dentomaxillofacial CT imaging using iterative reconstruction technology. Dentomaxillofac Radiol 46:20160452
McGuigan M, Duncan H, Horner K (2018) An analysis of effective dose optimization and its impact on image quality and diagnostic efficacy relating to dental cone beam computed tomography (CBCT). Swiss Dent J 128:297–316
Pauwels R, Zhang G, Theodorakou C, Walker A, Bosmans H, Jacobs R, Bogaerts R, Horner K, Consortium SP (2014) Effective radiation dose and eye lens dose in dental cone beam CT: effect of field of view and angle of rotation. Br J Radiol 87:20130654
Ludlow J, Timothy R, Walker C, Hunter R, Benavides E, Samuelson D, Scheske M (2015) Effective dose of dental CBCT—a meta analysis of published data and additional data for nine CBCT units. Dentomaxillofac Radiol 44:20140197
Stratis A, Zhang G, Lopez-Rendon X, Politis C, Hermans R, Jacobs R, Bogaerts R, Shaheen E, Bosmans H (2017) Two examples of indication specific radiation dose calculations in dental CBCT and multidetector CT scanners. Phys Med 41:71–77
Jones D, Mannocci F, Andiappan M, Brown J, Patel S (2015) The effect of alteration of the exposure parameters of a cone-beam computed tomographic scan on the diagnosis of simulated horizontal root fractures. J Endod 41:520–525
Neves F, Vasconcelos T, Vaz S, Freitas D, Haiter-Neto F (2012) Evaluation of reconstructed images with different voxel sizes of acquisition in the diagnosis of simulated external root resorption using cone beam computed tomography. Int Endod J 45:234–239
EzEldeen M, Stratis A, Coucke W, Codari M, Politis C, Jacobs R (2017) As low dose as sufficient quality: optimization of cone-beam computed tomographic scanning protocol for tooth autotransplantation planning and follow-up in children. J Endod 43:210–217
Brown AA, Scarfe WC, Scheetz JP, Silveira AM, Farman AG (2009) Linear accuracy of cone beam CT derived 3D images. Angle Orthod 79:150–157
Cook V, Timock A, Crowe J, Wang M, Covell D (2015) Accuracy of alveolar bone measurements from cone beam computed tomography acquired using varying settings. Orthod Craniofacial Res 18:127–136
Kusnoto B, Kaur P, Salem A, Zhang Z, Galang-Boquiren MT, Viana G, Evans CA, Manasse R, Monahan R, BeGole E (2015) Implementation of ultra-low-dose CBCT for routine 2D orthodontic diagnostic radiographs: Cephalometric landmark identification and image quality assessment. Semin Orthod 21:233–247
Ludlow JB, Walker C (2013) Assessment of phantom dosimetry and image quality of i-CAT FLX cone-beam computed tomography. Am J Orthod Dentofac Orthop 144:802–817
Bechara B, McMahan CA, Nasseh I, Geha H, Hayek E, Khawam G, Raad M, Noujeim M (2013) Number of basis images effect on detection of root fractures in endodontically treated teeth using a cone beam computed tomography machine: an in vitro study. Oral Surg Oral Med Oral Pathol Oral Radiol 115:676–681
Durack C, Patel S, Davies J, Wilson R, Mannocci F (2011) Diagnostic accuracy of small volume cone beam computed tomography and intraoral periapical radiography for the detection of simulated external inflammatory root resorption. Int Endod J 44:136–147
Hashem D, Brown JE, Patel S, Mannocci F, Donaldson AN, Watson TF, Banerjee A (2013) An in vitro comparison of the accuracy of measurements obtained from high-and low-resolution cone-beam computed tomography scans. J Endod 39:394–397
Lennon S, Patel S, Foschi F, Wilson R, Davies J, Mannocci F (2011) Diagnostic accuracy of limited-volume cone-beam computed tomography in the detection of periapical bone loss: 360° scans versus 180° scans. Int Endod J 44:1118–1127
Al-Ekrish AA (2012) Effect of exposure time on the accuracy and reliability of cone beam computed tomography in the assessment of dental implant site dimensions in dry skulls. Saudi Dent J 24:127–134
Dawood A, Brown J, Sauret-Jackson V, Purkayastha S (2012) Optimization of cone beam CT exposure for pre-surgical evaluation of the implant site. Dentomaxillofac Radiol 41:70–74
de-Azevedo-Vaz SL, de Faria Vasconcelos K, Neves FS, Melo SLS, Campos PSF, Haiter-Neto F (2013) Detection of periimplant fenestration and dehiscence with the use of two scan modes and the smallest voxel sizes of a cone-beam computed tomography device. Oral Surg Oral Med Oral Pathol Oral Radiol 115:121–127
El Sahili N, David-Tchouda S, Thoret S, Nasseh I, Berberi A, Fortin T (2018) Effect of milliamperage reduction on pre-surgical implant planning using cone beam computed tomography by surgeons of varying experience. J Maxillofac Oral Surg 17:520–530
Liljeholm R, Kadesjö N, Benchimol D, Hellén-Halme K, Shi X-Q (2017) Cone-beam computed tomography with ultra-low dose protocols for pre-implant radiographic assessment: an in vitro study. Eur J Oral Implantol 10:351–359
Neves FS, Vasconcelos TV, Campos PS, Haiter-Neto F, Freitas DQ (2014) Influence of scan mode (180/360) of the cone beam computed tomography for preoperative dental implant measurements. Clin Oral Implants Res 25:e155–e158
Parsa A, Ibrahim N, Hassan B, Motroni A, Van der Stelt P, Wismeijer D (2013) Influence of cone beam CT scanning parameters on grey value measurements at an implant site. Dentomaxillofac Radiol 42:79884780
Sur J, Seki K, Koizumi H, Nakajima K, Okano T (2010) Effects of tube current on cone-beam computerized tomography image quality for presurgical implant planning in vitro. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 110:e29–e33
Vasconcelos TV, Neves FS, de Freitas DQ, Campos PSF, Watanabe PCA (2014) Influence of the milliamperage settings on cone beam computed tomography imaging for implant planning. Int J Oral Maxillofac Implants 29:1364–1368
Waltrick KB, de Abreu Junior MJN, Corrêa M, Zastrow MD, D'Avila Dutra V (2013) Accuracy of linear measurements and visibility of the mandibular canal of cone-beam computed tomography images with different voxel sizes: an in vitro study. J Periodontol 84:68–77
Al-Okshi A, Theodorakou C, Lindh C (2017) Dose optimization for assessment of periodontal structures in cone beam CT examinations. Dentomaxillofac Radiol 46:20160311
de Melo LPL, Oenning ACC, Nadaes MR, Nejaim Y, Neves FS, Oliveira ML, Freitas DQ (2017) Influence of acquisition parameters on the evaluation of mandibular third molars through cone beam computed tomography. Oral Surg Oral Med Oral Pathol Oral Radiol 124:183–190
Neves FS, de Camargo Souza T, de-Azevedo-Vaz SL, Campos PSF, Bóscolo FN (2014) Influence of cone-beam computed tomography milliamperage settings on image quality of the mandibular third molar region. Oral Radiol 30:27–31
Yadav S, Palo L, Mahdian M, Upadhyay M, Tadinada A (2015) Diagnostic accuracy of 2 cone-beam computed tomography protocols for detecting arthritic changes in temporomandibular joints. Am J Orthod Dentofac Orthop 147:339–344
da Silva Moura W, Chiqueto K, Pithon GM, Neves LS, Castro R, Henriques JFC (2018) Factors influencing the effective dose associated with CBCT: a systematic review. Clin Oral Investig 23:1319–1330
Funding
This study has been funded by departmental funds only. No external funding has been received.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
Not applicable.
Informed consent
Not applicable.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Yeung, A.W.K., Jacobs, R. & Bornstein, M.M. Novel low-dose protocols using cone beam computed tomography in dental medicine: a review focusing on indications, limitations, and future possibilities. Clin Oral Invest 23, 2573–2581 (2019). https://doi.org/10.1007/s00784-019-02907-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-019-02907-y