Abstract
Objectives
Sialolithiasis is the most common cause of chronic sialadenitis of the submandibular gland (SMG). Symptomatic superficial lobe stones are often treated by submandibulectomy. A gland preserving operation allows for transoral stone removal through endoscopically assisted sialolithotomy. Herein, we provide clinical and sonographical follow-up data in patients who underwent sialolithotomy under general anesthesia.
Materials and methods
Sixty patients treated at the Department of Oral and Maxillofacial Surgery at Düsseldorf University Hospital for superficial lobe sialolithiasis of SMG were included in this study. All received transoral sialolithotomy under general anesthesia. Follow-up was conducted via standardized patient questionnaires, clinical examination, and B-mode and color Doppler sonography.
Results
Mean patient age was 48.9 years. 56.6% of right and 43.4% of left SMG were affected. Mean follow-up was 45 months. Fifty-five of 59 detected stones could be removed. Mean operation time was 71 min. 3.3% of patients reported recurrent episodes of postoperative pain and 10% felt recurrent episodes of gland swelling. Persistent postoperative lingual nerve hypesthesia was described in one patient. No facial nerve damages occurred. Salivary flow rates remained reduced in most of the affected glands upon stone removal. Sonographical follow-up data of the previously affected SMG after intraoral endoscopy-assisted sialolithotomy showed a regular gland size in 70.8% of cases, a parenchyma free of inflammation in 93.8%, and without signs of fibrosis in 72.9% of cases. 68.7% of patients showed a regular structure of Wharton’s duct at time of follow-up. In total, 89.6% of patients were diagnosed stone-free within both glands on follow-up. No case required subsequent submandibulectomy.
Conclusions
Sialolithotomy of Wharton’s duct for removal of stones from the SMG’s superficial lobe is a promising alternative to submandibulectomy.
Clinical relevance
Reduction of postoperative morbidity through endoscopically assisted sialolithotomy for removal of superficial lobe stones from SMG.
Trial registration
Ethics Committee of Heinrich-Heine-University Düsseldorf (no. 5586)
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Obstructive sialadenitis is the most common non-malignant salivary gland pathology with sialolithiasis accounting for the largest part of the pathogenesis of the disease, at around 60% [1, 2]. Salivary stones are caused by the formation of calcified calculi due to successive deposition of calcium salts around an initial organic nidus [3]. These sialoliths maintain an inflammation of the ductal wall and impede salivary outflow of the upstream glandular parenchyma leading to increased backlog of produced saliva [4]. Consequently, the affected gland may suffer from chronic inflammation, pressure atrophy, and fibrosis [5]. Clinical symptoms include pressing pain, visible glandular swelling, and viscous or even purulent discharge from the ductal orifice [6]. Due to the anatomy of its excretory duct and the chemical composition of its saliva, the submandibular gland (SMG) is particularly susceptible to sialolith formation and is affected in 80–90% of cases [7]. Anatomically, the stones of the SMG can be located in the deep lobe (53%), Wharton’s duct (37%), or superficial lobe (10%) [8]; the mean diameter of the stones in this region is about 8.3 mm [8].
B-mode ultrasound represents the gold standard in imaging of salivary gland stones with a reported sensitivity between 75 and 94% and specificity of approximately 95% [9, 10]. With modern high-resolution transducers (up to 18 MHz), a lot of information not only on salivary stones, but also about the ductal system and the glandular parenchyma can be obtained and compared with histological findings.
Whereas stones located in the distal third of Wharton’s duct anterior of the hilar region are easily accessible to ductal incision [11] or 810 nm diode laser therapy [12] under local anesthesia deep and superficial lobe sialoliths cannot be reached by these procedures. Extracorporeal shock wave lithotripsy (ESWL) can be used to treat stones in the hilar or intraglandular region of SMG but with relatively poor success rates of approximately 50% [13]. For a long time, adequate therapy for symptomatic sialoliths located in the hilar region or the superficial lobe consisted of submandibulectomy [14]. However, several years ago, reports on the functional recovery of salivary glands upon removal of the cause of obstruction appeared [15]. Furthermore, a significant percentage of the submandibular glands removed due to salivary stones exhibited normal histologic findings. And there was no correlation in the clinical course of patients with the degree of damage to the glandular parenchyma as determined by histopathology [16]. Therefore, a paradigm shift in the therapy of hilar stones took place in favor of minimally invasive combined endoscopic and surgical techniques with preservation of the respective gland [17]. Compared to submandibulectomy, the procedure of transoral sialolithotomy has been reported to be beneficial for the patients in terms of risks, postoperative pain, hospitalization time, and costs [18]. A success rate (i.e., avoiding submandibulectomy) of about 95% has been reported [19]. However, this procedure only allows extraction of sialoliths up to the hilar region and with only few studies determining long-term success rate to date. Therefore, our study aimed at expanding the indication of the endoscopically assisted sialolithotomy to stones of the superficial lobe of the SMG and at generating data on success rates and long-term follow-up results.
This study, for the first time, provides long-term clinical and sonographical follow-up data on gland preserving removal of superficial lobe stones of the SMG.
Materials and methods
Ethical approval
This combined prospective-retrospective study was carried out under careful consideration of the Declaration of Helsinki for conducting patient studies. Approval of the Ethics Committee of Düsseldorf University Hospital was granted prior to this study (no. 5586). A patient consent form was signed by each patient taking part in the study.
Data collection
Patients were invited per post, email, and/or telephone call to our outpatient clinic for a follow-up examination. At this appointment, the survey of the patient questionnaire, the clinical follow-up, and the ultrasound examination took place.
A total number of 60 patients with sialolithiasis of the SMG that underwent endoscopically assisted transoral superficial lobe stone removal under general anesthesia between the years 2008 and 2018 were comprised in this study. Only patients with superficial lobe stones which could not be removed by sialendoscopy alone due to their size and deep intraglandular position were included. All patients were scheduled for an in-office examination. Follow-up data was evaluated retrospectively. Patients lost to follow-up were excluded from the study. The mean follow-up time after the operation was 45 months. All patients filled out a standardized questionnaire regarding their oral rehabilitation after the intervention (Table 1).
A standardized medical examination form was filled out for each patient at time of follow-up by the same trained examiner (J.L.) over the course of the study (Table 2).
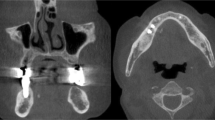
Preparation for the surgical intervention
None of the patients had received any previous treatment for a salivary gland pathology elsewhere or in our institution. Preoperative assessment included patient history collection, clinical examination including assessment of salivary flow and palpation of the floor of the mouth, and a B-mode and color Doppler ultrasound examination of the head and neck including all major salivary glands. Only when needed or in case of ambiguous findings, further investigations as sialo-MR, cone-beam computed tomography (CBCT), or diagnostic sialendoscopy were performed.
Surgical intervention
The intervention was performed under general anesthesia. The maximum muscle relaxation was achieved by intravenous rocuronium (0.6 mg/kg) or cis-atracurium (0.15 mg/kg) injection adapted to patient weight. After thorough oral disinfection with Braunol® (B. Braun, Melsungen, Germany), Wharton’s duct of the affected SMG was dilated at the papillary region with tapered conical tip salivary duct dilators (Karl Storz GmbH, Tuttlingen, Germany) to a size 8 diameter (Fig. 5a). In cases where Wharton’s duct could not be sufficiently probed, a small papillotomy was made with a no. 11 stainless steel scalpel (B. Braun, Melsungen, Germany). After dilation, an Erlangen 1.1 mm or 1.6 mm all-in-one sialendoscope (Karl Storz GmbH, Tuttlingen, Germany) was inserted into the duct depending on the anatomical width of the papilla. Now, the assistant had to vigorously mobilize the gland around the rear edge of the mylohyoid muscle in cranio-ventral direction to enable access to the stone with the endoscope. The position of the sialendoscope directly in front of the stone could intraorally be monitored by inspection of the endoscopic light beam shining through the oral mucosa (Fig. 5b). Superficial lobe stones positioned in a ductal region with a diameter that was smaller than the 1.1 mm of the sialendoscope could not be visualized endoscopically. In these cases, the stone position was located by careful bimanual finger palpation. Now, a small mucosal incision was made directly over the stone position. Bleeding was stopped by careful cauterization avoiding contact with the lingual nerve. The sublingual gland as well as the lingual nerve where bluntly preparated and protected. The glandular parenchyma was pushed bluntly sidewards; the stone was located and removed through a small ductal incision (Fig. 5c, d). After thorough rinsing of the neighboring duct areas, the sialendoscope was further advanced over the site of the sialodochotomy into the proximal glandular structures to check for additional concrements that could be either washed out or removed. Postoperatively, a small arterial polyethylene catheter (18G) (Vygon GmbH & Co., Aachen, Germany) was inserted via a Seldinger technique into the (neo-)ostium for stabilization (Fig. 5e, f). The stent as well as the orifice of the (neo-)ostium were sutured to the surrounding oral epithelium (Fig. 5g). Removal of the stent was intentionally conducted 3 weeks postoperatively. All patients received postoperative intravenous antibiotics (3 g ampicillin/sulbactame 3× per day) as well as 1 g novalgin 3× per day. We conducted postoperative inpatient monitoring for 2 days to allow for sufficient control of patient well-being.
Sonography
For sonography, the ACUSON S2000 HELX Evolution system (Siemens, Munich, Germany) with the linear transducer L5–14 was used. For image acquisition, B-mode and color Doppler mode were utilized using an individually developed preset “submandibular gland.” Sonographical parameters taken into consideration for SMG assessment are shown in Table 3. The applied scoring system is adapted to histopathological findings of resected SMGs due to sialolithiasis described earlier by Marchal et al. (2001) [16]. Sonographical images of each patient were taken without and directly after ingestion of a teaspoon of vitamin C (Caesar and Loretz GmbH, Hilden, Germany).
Measurement of salivary flow
Salivary flow of the SMG on both sides was measured using a modified Schirmer test [20] with Sugi Sponge Points (Kettenbach GmbH, Eschenburg, Germany). Unlike Schirmer’s test, no defined time was given; after that, the wetted distance of the point was measured, but the time was measured until the sponge points were completely soaked which was the case upon outflow of 0.3 ml. The examiner compressed the ductal orifice of the contralateral SMG using a cotton tip. Now, a Sugi Sponge Point was held at the orifice of the uncompressed orifice while an assistant manually massaged the SMG at test. The time (in seconds) was taken until the Sugi Sponge Point’s capacity for saliva uptake was reached which could be identified by the maximum expansion of the Sugi Sponge Point. A time difference of > 5 s between the left and right SMG before the maximum expansion was reached was considered significant.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request
Results
General statistics
Of 72 patients that received endoscopically assisted stone removal from the SMG’s superficial lobe between 2008 and 2018, 60 (83.3%) were available for a follow-up assessment. Of the remaining 12 (16.7%) patients, ten could not be reached via mail or phone or through their general practitioner and two, over time, had passed away due to another illness. However, these patients did not differ significantly in epidemiological or nosological terms from the patients who could be contacted for follow-up. Therefore, 60 patients were comprised in this study. Of these, 48 came in for an in-office appointment at our clinic and 12 merely filled out the questionnaire via mail or phone as they invariably came from distant parts of the country or from abroad, so that they declined to travel for follow-up. The mean patient age was 48.9 years (range 18.1–83.4 years). Of all patients, 35 were male with a mean age of 49.8 years (range 18.1–83.4 years) and 25 were female with a mean age of 47.6 years (range 19.3–69 years). Sialolithiasis affected the right SMG in 34 (56.6%) patients and the left SMG in 26 (43.4%) patients. The mean follow-up time after the operation was 45 months (range 1–117 months). The mean operation time was 71 min. In the 48 patients who were available for an in-office appointment, 59 stones were diagnosed by clinical examination and ultrasound (43 patients presented with one stone, one patient had two, two patients three, and another two patients had four stones). In one patient, the stone was not detectable by ultrasound, and therefore we had to perform a CBCT. Mean diameter of the stones was 10.1 mm (range 3.9–17.9 mm). Overall, 55 (93.2%) stones could successfully be removed. All patients were successfully discharged on the second postoperative day.
Patient perceived oral rehabilitation
From the 60 patients examined 7 (11.7%) reported sensation of pain at some point after the operation. Two (28.6%) of these patients still feel recurrent episodes of dull pressure sensation in the SMG area. Six (10%) patients reported the perception of persistent minimal swelling of the affected gland. Four (6.7%) patients reported concrement discharge after the operation. None of the patients were treated for sialolithiasis at another clinic or practice after the operation or felt a speech impediment. Two (3.3%) patients reported slight difficulty eating after the operation but addressed this was no need for further treatment. One (1.7%) patient mentioned hypesthesia of the lateral border of the tongue on the affected side. None of the patients reported impaired tongue mobility, facial expression, facial appearance, or drier mouth when compared to the preoperative state. No patient perceived a purulent taste after the operation and no medication that reduces salivary flow was taken.
Physician perceived oral rehabilitation of patient
At time of follow-up, four (8.3%) patients presented with facial asymmetry due to visible swelling on the side of the affected SMG. Skin color and texture over the affected SMG area had not changed in any patient. None of the patients had signs of anesthesia, hypesthesia, dysesthesia, hyperalgesia, or allodynia in SMG area. The facial nerve was not damaged in any patient. Cervical palpation revealed a moveable resistance of the affected SMG in 6 (12.5%) patients. Intraorally, scars from papillotomy could be found in 18 (37.5%) patients. One (2.1%) patient described hypesthesia of the lateral border of the tongue on the affected side during the examination. No patient was found to have dysfunctional tongue mobility. A solid palpable resistance of Wharton’s duct was present in 4 (8.3%) patients. Olfactory sensation was normal in all patients.
When assessing salivary flow rates, 22 (45.8%) patients were found to have reduced flow rates of the affected SMG after external SMG massage procedures (Fig. 1a). No salivary flow of the affected SMG was observed in 5 (10.4%) patients (Fig. 1a). Increased salivary flow was seen in 3 (6.3%) patients (Fig. 1a). Regular salivary flow of both SMG was found in 18 (37.5%) patients (Fig. 1a).
Number of patients with a equal (blue), reduced (orange), and no detectable (gray) salivary flow rate of affected compared to unaffected submandibular gland (SMG) after manual extraoral massage. b Equal (blue) and reduced (orange) size of the affected submandibular gland compared to unaffected contralateral side in B-mode sonography images. c No detectable (blue), dilated (orange), widened (gray), or ectasia-like structures of the ductal system of the affected submandibular gland compared to unaffected contralateral side in B-mode sonography images. d Equal (blue), hypodens (orange), and hyperdens (gray) parenchymal structure of the affected submandibular gland compared to unaffected contralateral side in B-mode sonography images
Sonography
In 14 (29.2%) patients, the size of the affected SMG was found to be smaller than on the contralateral side (Fig. 1b). Thirty-four (70.8%) patients presented with equally sized SMG parenchyma on both sides of the mouth (Fig. 1b). Wharton’s duct of the affected SMG was dilated in 5 (10.4%) patients, showed an ampullary widening at the former site of the stone in 7 (14.6%) patients (Fig. 1c), and multiple duct ectasias in 3 (6.3%) patients (Fig. 1c). Thirty-three (68.7%) patients showed a regular duct structure on both sides (Fig. 1c). When looking at parenchymal gland structure, 12 (25%) patients were diagnosed with hypodense parenchyma of the affected gland (Fig. 1d). A hyperdense gland parenchyma was found in the affected SMG of 4 (8.3%) patients (Fig. 1d). Thirty-two (66.7%) patients were found to have a regular parenchyma density on both sides (Fig. 1d). Of all 48 sonographically examined patients, 43 (89.6%) were diagnosed stone-free within both glands at the time of follow-up (Fig. 2a). Of these, 2 (4.3%) patients presented with one sonographically detectable residual stone concrement after the operation (Fig. 2a). In 1 (2.1%) patient, two residual stone concrements were sonographically detected (Fig. 2a). A new stone within the affected SMG was detected in 1 (2.1%) patient (Fig. 2a). Mucus plugs were detected in the formerly affected SMG in 1 (2.1%) patient as well (Fig. 2a). A mild atrophy of the affected SMG was found in 15 (31.6%) patients, whereas a severe atrophy was present in 3 (6.3%) patients (Fig. 2b). No signs of atrophy were found in 30 (62.5%) patients (Fig. 2b). Mild inflammation was seen in 3 (6.3%) patients in the affected SMG (Fig. 2c). Forty-five (93.8%) patients did not show signs of SMG inflammation on either side (Fig. 2c). Eleven (22.9%) patients showed signs of mild fibrosis of the affected SMG and 2 (4.2%) patients were diagnosed with severe fibrosis of the affected SMG (Fig. 2d). Thirty-five (72.9%) patients lacked detectable sonographical signs of gland fibrosis at time of follow-up (Fig. 2d). Occurrence of fibrosis, inflammation, and atrophy was irrespective of the timespan between operation and follow-up appointment but showed a correlation with age. Ninety percent of patients with a reduced SMG size were 60 years and older. 68.8% of patients with sonographical alterations within the glands’ parenchyma as well as 77.8% of patients with signs of gland atrophy were 50 years and older. Of all patients with sonographical appearance of gland fibrosis, 69.2% were 60 years and older. Images of the analyzed sonographical gland pathologies are shown in Figs. 3a–f and 4a–d.
Number of patients with a no (blue), 1 (orange), and 2 (gray) residual concrements of the affected submandibular gland in B-mode sonography images (number of patients with new stone formation (yellow) and mucus plugs (turquoise) are also displayed). b No detectable (blue), mild (orange), and severe (gray) atrophy of the affected submandibular gland compared to unaffected contralateral side in B-mode sonography images. c No detectable (blue) and mild (orange) inflammation of the affected submandibular gland compared to unaffected contralateral side in B-mode sonography images. d No detectable (blue), mild (orange), and severe (gray) fibrosis of the affected submandibular gland compared to unaffected contralateral side in B-mode sonography images
Sonographical findings (a–f) of submandibular gland pathologies related to chronic obstruction; stimulated refers to oral vitamin C application. a The remaining glandular tissue is heavily reduced and indistinguishable from the surrounding connective tissue. This finding was taken as severe atrophy (grade III). b Unaffected contralateral submandibular gland. c The size of the affected right-sided gland is the same as on the healthy opposite side (d), but the parenchyma is clearly rarefied and fibrotically rebuilt. This finding was interpreted as grade III atrophy. e Similar findings as in c and d, but here the parenchyma is more hypodens. The affected gland is characterized by sclerotic and indurated parenchyma; this finding was also interpreted as fibrosis grade III. f The asterisk marks a region of slightly less fibrotic appearance of the parenchyma
Sonographical findings (a–d) of submandibular gland pathologies related to chronic obstruction; stimulated refers to oral vitamin C application. a Persistent mild inflammation with ampullary dilatation of the intraglandular D. Wharton in the former stone area, two small residual calculi, and a sparse periductal inflammatory infiltrate in the glandular parenchyma. b Unaffected contralateral side. c and d Example of a patient with complete recovery of the glandular parenchyma. The formerly affected side can no longer be determined by the ultrasound examination. This finding was interpreted as grade 0 in all three categories (atrophy, fibrosis, and inflammation)
Discussion
Numerous new techniques for diagnosing obstructive salivary gland pathologies have been introduced to the clinic over the past 20 years: high-resolution ultrasound, diagnostic sialendoscopy (dSGE), and Sialo-MR, for instance [21]. But also, the treatment of salivary stones has become more complex through a variety of mostly minimally invasive procedures. In particular, interventional sialendoscopy (iSGE), extracorporeal shock wave lithotripsy (ESWL), and combined endoscopic-surgical procedures should be mentioned [22]. This has led to a diversification of salivary stone therapy and a relatively complicated treatment regimen, where the therapy is guided by several factors, such as the gland involved, the size and number of stones, the location at different sections of the excretory duct, and the relationship to the duct; the aim of the regimen being to find the least invasive approach with the preservation of the affected gland [23]. By consistently following the therapeutic graduated scheme of increasing invasiveness, the rate of removal of the gland due to salivary stones could be reduced to below 5% of cases [23]. Until recently, one of the remaining primary indications for submandibulectomy in our institution has been the intraglandular sialolithiasis of the superficial lobe of the SMG (Fig. 5) [24]. Postoperative complications like facial and lingual nerve deficits, pain, and visible scarring had to be gradually accepted in order to ease symptoms [25, 26]. In clinical trials, the risk for postoperative hematomas and infection was evaluated to reach up to 14% [27]. Xerostomia was observed in up to 31% and alteration of taste in 16.3% of cases [28]. Damage to the facial nerve was as high as 8% and impairment of the lingual nerve had an even higher occurrence with up to 12% [29]. There are many reports about successful transoral stone removal under local anesthesia even for deep hilar stones [19, 30]. In their study, Schapher et al. (2017) report about a mean operation time under local anesthesia of approximately 40 min [19]. We sought to extend the indication for the combined endoscopic-surgical approach to the treatment of stones located in the superficial lobe of the SMG. According to our experience, this requires general anesthesia with complete relaxation of the patient as this enables a better overview and control of the surgical field. Besides this, general anesthesia allows for a longer operation time in cases where sialoliths are more difficult to locate and extract. Successful gland preserving treatment of parotid duct sialolithiasis has been shown before [31, 32]. Here, success rates of about 95% were reached [33]. About the same success rates are described for submandibulotomy [19]. In our study, we had a success rate of 100% (i.e., no subsequent submandibulectomy required), with a critical remark that only 60 cases were investigated since stones in the superficial lobe are a rather rare event [8]. In a histopathological study, the potential of submandibular gland recovery after a profoundly congested duct was shown [15]. Our data support these findings as most glands did not show signs of atrophy, inflammation, or fibrosis in sonographic images, although we cannot provide histopathological data, obviously. Functional recovery of salivary glands upon removal of the cause of obstruction has been shown by several authors [15]. Our ultrasound data are in line with these functional data and are supported by the findings of a regular flow rate on both sides in 37.5% of patients. Noteworthy, 56.3% of patients had a non-stone-related asymptomatic reduced salivary flow rate on the affected side at time of follow-up. 95.8% of patients did not develop new sialoliths during follow-up. Though, it has to be mentioned that in 6.3% of cases, small concrements remained in the ductal system after the operation. None of the patients reported xerostomia. Our study supports the hypothesis that postoperative complications after microsurgical endoscopically assisted interventions are less frequent compared to submandibulectomy [34]. With 11.7% pain was the mostly mentioned complication after the operation. In terms of impaired neurological functions, one patient reported about hypoesthesia in the lingual nerve innervation territory. This has also been stated by McGurk et al. (2004) for sialadenectomy [17] and Kim et al. (2007) for submandibulotomy [35]. Our and other studies demonstrate a successful technique for transoral removal of single as well as multiple sialoliths [36]. This is especially valuable as submandibulectomy was deemed more likely the more sialoliths were located within the ductal system. After the biggest sialolith has been removed, there is a good chance that minor stones will wash out or remain asymptomatic. Whether ductal stent insertion or sialodochoplasty by marsupialization is superior for operational success is still unclear [37, 38]. We preferred stent implantation for a better salivary outflow rate. Regarding inpatient monitoring for two consecutive postoperative days, it should be critically noted that sialolithotomy is generally considered outpatient surgery [19]. Here, we used a more conservative approach because of deep intraglandular stone location and application of general anesthesia. Even though sialodochotomy is promising, additional studies are necessary to foster our understanding of long-term success of transoral removal of intraglandular sialoliths.
Removal of a sialolith from the superficial lobe of the right submandibular gland (SMG) via an intraoral endoscopy-assisted sialolithotomy. a Cannulation of the orifice of dilated right Wharton’s duct with a sialendoscope. b Advancement of the sialendoscope into the ductal system until the stone position is reached after the superficial lobe has been manually pressed around the posterior border of the mylohyoid muscle. The stone position is indicated by the light of the sialendoscope. c Mucosal incision to carefully visualize the stone. d Ductal incision to carefully extract the stone. e Placement of a guidewire before application of the stent into the orifice of Wharton’s duct in Seldinger technique. f Bridging the proximal and distal end of the ductal system by the stent. g Primary wound closure with resorbable sutures and insertion of a stent into the orifice of Wharton’s duct. h Image of the extracted salivary stone
Conclusion
Transoral endoscopically assisted sialodochotomy is a promising new way to cure sialolithiasis and prevent submandibulectomy even in superficial lobe stones of the SMG. With success rates of more than 90% and a good patient tolerability, this technique is suitable to extract ductal as well as intraglandular sialoliths alike. In rare cases where sialolith location is inaccessible by sialendoscopy or palpation submandibulectomy, it still remains the final approach.
Abbreviations
- SMG:
-
Submandibular gland
- CBCT:
-
Cone-beam computed tomography
- dSGE:
-
Diagnostic sialendoscopy
- iSGE:
-
Interventional sialendoscopy
- ESWL:
-
Extracorporeal shock wave lithotripsy
References
Koch M, Zenk J, Iro H (2008) Diagnostic and interventional sialoscopy in obstructive diseases of the salivary glands. Hno 56(2):139–144
Capaccio P, Clemente IA, McGurk M, Bossi A, Pignataro L (2011) Transoral removal of hiloparenchymal submandibular calculi: a long-term clinical experience. Eur Arch Otorhinolaryngol 268(7):1081–1086
Fusconi M, Petrozza V, Schippa S, de Vincentiis M, Familiari G, Pantanella F, Cirenza M, Iebba V, Battaglione E, Greco A, Gallipoli C, Campo F, Gallo A (2016) Bacterial biofilm in salivary gland stones: cause or consequence? Otolaryngol Head Neck Surg 154(3):449–453
Escudier MP, Brown JE, Drage NA, McGurk M (2003) Extracorporeal shockwave lithotripsy in the management of salivary calculi. Br J Surg 90(4):482–485
Farnaud SJ et al (2010) Saliva: physiology and diagnostic potential in health and disease. ScientificWorldJournal 10:434–456
Levy DM, Remine WH, Devine KD (1962) Salivary gland calculi. Pain, swelling associated with eating. Jama 181:1115–1119
Shahoon H, Farhadi S, Hamedi R (2015) Giant sialoliths of Wharton duct: report of two rare cases and review of literature. Dent Res J (Isfahan) 12(5):494–497
Sigismund PE, Zenk J, Koch M, Schapher M, Rudes M, Iro H (2015) Nearly 3,000 salivary stones: some clinical and epidemiologic aspects. Laryngoscope 125(8):1879–1882
Vogl TJ, al-Nawas B, Beutner D, Geisthoff U, Gutinas-Lichius O, Naujoks C, Reich R, Schröder U, Sproll C, Teymoortash A, Ußmüller J, Wittekindt C, Zenk J, Fischer S (2014) Updated S2K AWMF guideline for the diagnosis and follow-up of obstructive sialadenitis--relevance for radiologic imaging. Rofo 186(9):843–846
Terraz S, Poletti PA, Dulguerov P, Dfouni N, Becker CD, Marchal F, Becker M (2013) How reliable is sonography in the assessment of sialolithiasis? AJR Am J Roentgenol 201(1):W104–W109
Nahlieli O, Shacham R, Zagury A, Bar T, Yoffe B (2007) The ductal stretching technique: an endoscopic-assisted technique for removal of submandibular stones. Laryngoscope 117(6):1031–1035
Angiero F, Benedicenti S, Romanos GE, Crippa R (2008) Sialolithiasis of the submandibular salivary gland treated with the 810- to 830-nm diode laser. Photomed Laser Surg 26(6):517–521
Lafont J, Graillon N, Hadj Saïd> M, Tardivo D, Foletti JM, Chossegros C (2018) Extracorporeal lithotripsy of salivary gland stone: a 55 patients study. J Stomatol Oral Maxillofac Surg 119(5):375–378
Kopec T et al (2013) Algorithm changes in treatment of submandibular gland sialolithiasis. Eur Arch Otorhinolaryngol 270(7):2089–2093
Makdissi J et al (2004) Glandular function after intraoral removal of salivary calculi from the hilum of the submandibular gland. Br J Oral Maxillofac Surg 42(6):538–541
Marchal F, Becker M, Kurt AM, Oedman M, Dulguerov P, Lehmann W (2001) Histopathology of submandibular glands removed for sialolithiasis. Ann Otol Rhinol Laryngol 110(5 Pt 1):464–469
McGurk M, Makdissi J, Brown JE (2004) Intra-oral removal of stones from the hilum of the submandibular gland: report of technique and morbidity. Int J Oral Maxillofac Surg 33(7):683–686
Eun YG, Chung DH, Kwon KH (2010) Advantages of intraoral removal over submandibular gland resection for proximal submandibular stones: a prospective randomized study. Laryngoscope 120(11):2189–2192
Schapher M, Mantsopoulos K, Messbacher ME, Iro H, Koch M (2017) Transoral submandibulotomy for deep hilar submandibular gland sialolithiasis. Laryngoscope 127:2038–2044
Moreland LW (2004) Schirmer’s tear test, in Rheumatology and Immunology Therapy. Springer, Berlin, Heidelberg, pp 781–782
Schwarz D, Kabbasch C, Scheer M, Mikolajczak S, Beutner D, Luers JC (2015) Comparative analysis of sialendoscopy, sonography, and CBCT in the detection of sialolithiasis. Laryngoscope 125(5):1098–1101
Koch M et al (2017) Multimodal treatment in difficult sialolithiasis: role of extracorporeal shock-wave lithotripsy and intraductal pneumatic lithotripsy. Laryngoscope 128(10):E332–E338
Koch M, Zenk J, Iro H (2009) Algorithms for treatment of salivary gland obstructions. Otolaryngol Clin N Am 42(6):1173–1192 Table of Contents
Capaccio P, Bottero A, Pompilio M, Ottaviani F (2005) Conservative transoral removal of hilar submandibular salivary calculi. Laryngoscope 115(4):750–752
Bates D, O’Brien CJ, Tikaram K, Painter DM (1998) Parotid and submandibular sialadenitis treated by salivary gland excision. Aust N Z J Surg 68(2):120–124
Kennedy PJ, Poole AG (1989) Excision of the submandibular gland: minimizing the risk of nerve damage. Aust N Z J Surg 59(5):411–414
Winkel R et al (2000) Surgical results of submandibular gland excision. Ugeskr Laeger 162(40):5354–5357
Hald J, Andreassen UK (1994) Submandibular gland excision: short- and long-term complications. ORL J Otorhinolaryngol Relat Spec 56(2):87–91
Kukuckova B, Svec M (2011) Surgical management of submandibulary gland diseases: ten years of experience. Bratisl Lek Listy 112(5):264–268
Jokela J, Haapaniemi A, Mäkitie A, Saarinen R (2017) Sialendoscopy under local anaesthesia. Acta Otolaryngol 137(3):310–314
Koch M, Künzel J, Iro H, Psychogios G, Zenk J (2014) Long-term results and subjective outcome after gland-preserving treatment in parotid duct stenosis. Laryngoscope 124(8):1813–1818
Nahlieli O, Baruchin AM (2000) Long-term experience with endoscopic diagnosis and treatment of salivary gland inflammatory diseases. Laryngoscope 110(6):988–993
Nahlieli O et al (2001) Diagnosis and treatment of strictures and kinks in salivary gland ducts. J Oral Maxillofac Surg 59(5):484–490 discussion, 490–2
Nahlieli O (2015) Complications of sialendoscopy: personal experience, literature analysis, and suggestions. J Oral Maxillofac Surg 73(1):75–80
Kim JK, Park JS (2007) Ultrasound-guided transoral removal of impalpable hilar submandibular salivary stones. Laryngoscope 117(8):1373–1375
Ardekian L, Klein HH, Araydy S, Marchal F (2014) The use of sialendoscopy for the treatment of multiple salivary gland stones. J Oral Maxillofac Surg 72(1):89–95
Zhang L, Escudier M, Brown J, Capaccio P, Pignataro L, McGurk M (2010) Long-term outcome after intraoral removal of large submandibular gland calculi. Laryngoscope 120(5):964–966
Roh JL, Park CI (2008) Transoral removal of submandibular hilar stone and sialodochoplasty. Otolaryngol Head Neck Surg 139(2):235–239
Author information
Authors and Affiliations
Contributions
CS and JL worked out the concept and wrote the manuscript. JL carried out the follow-up examinations. JL and CS conducted follow-up sonographies. CS, CN, and DS carried out the operational procedures. JL assisted the operations. NK, HH, MR, and CN gave critical scientific input for the study design and engaged in manuscript creation.
Corresponding author
Ethics declarations
Competing interests
The authors declare that they have no competing interests.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Ethics approval was granted by the Ethics Committee of the Heinrich-Heine-University of Düsseldorf and given the reference number 5586.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Consent for publication
Patients gave their written consent to take part in the study. The forms can be obtained from the corresponding author in German language..
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sproll, C., Naujoks, C., Holtmann, H. et al. Removal of stones from the superficial lobe of the submandibular gland (SMG) via an intraoral endoscopy-assisted sialolithotomy. Clin Oral Invest 23, 4145–4156 (2019). https://doi.org/10.1007/s00784-019-02853-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-019-02853-9