Abstract
Objectives
Tumor invasion into blood and/or lymphatic vessels, perineural invasion, and histopathological grading are evaluated to assess the biological aggressiveness of oral squamous cell carcinoma (OSCC). We aim to assess the prognostic impact of a novel scoring system, based upon the aforementioned histological parameters.
Materials and methods
Retrospective chart review of 334 patients with treatment-naive squamous cell carcinoma of the oral cavity. Statistical analysis was performed using univariate and multivariate analysis. Histological grade G1 or G2 were assigned 0 points and G3 or G4 1 point. Invasion of the lymphatic vessels, blood vessels, or perineural space was given 1 point. Zero points were given, when invasion was not detectable. The final score was conducted through addition of each parameter. Therefore, our scoring system ranged between 0 and 4 points.
Results
T-classification (p < 0.001), N-classification (p < 0.001), UICC stage (p < 0.001), extracapsular spread (p < 0.001), locoregional recurrence (p < 0.001), and overall survival (p < 0.001) were significantly associated with the OSCC-Histoscore. In multivariate analysis, T-classification (p = 0.001), N-classification (p = 0.039), resection margins (p = 0.038), and OSCC-Histoscore (p < 0.001) were independent prognostic markers for overall survival rate.
Conclusion
Our presented OSCC-Histoscore serves as a strong independent prognostic parameter for 5-year overall survival (OS) and predicts OS better than T-classification, N-classification, and resection margins.
Clinical relevance
Our presented histoscore improves prediction of the overall survival of patients with OSCC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Head and neck cancer is the sixth most common cancer worldwide with an annual incidence of more than 500,000 [1, 2]. Approximately 50% originate from the oral cavity with 90% of these being squamous cell carcinoma (OSCC) [3]. Albeit there have been significant advances in diagnostic and therapeutic techniques, the 5-year overall survival rate has not improved within the last three decades and still remains below 50% [4,5,6,7,8,9,10]. One of the main reasons for this is the lack of suitable markers that enable appropriate prognostic differentiation and thus improve therapeutic decision-making [11, 12]. In daily clinical routine, the TNM Classification is primarily used for these purposes [4,5,6,7,8, 13]. However, since the TNM classification does not take into account the biologic characteristics of OSCC, there is wide consensus to consider additional parameters, such as perineural invasion, lymph vessel invasion, blood vessel invasion, and histopathological grading [14, 15]. Their significant prognostic and therapeutic importance for OSCC has led many authors to demand their implementation into the TNM system [14, 15]. However, a major drawback of this requirement is that a significantly higher number of TNM subgroups would arise. This would, on the one hand, hinder comparison and comprehensibility of the TNM system and on the other lead to a more complex and less representative classification [14, 15]. Hence, to address this conceptual shortcoming, we created an easily applicable scoring system, consisting of tumor invasion into lymphatic and/or blood vessels, perineural invasion, and histopathological grading, and examined whether this might serve as a prognostic tool for patients with OSCC.
Material and methods
Patients and data collection
The retrospective study included 334 patients, who were diagnosed with a treatment-naive squamous cell carcinoma of the oral cavity between 2001 and 2009.
All cases were staged histopathologically according to l’Union Internationale Contre le Cancer (UICC) tumor, node, metastasis (TNM) classification, 7th edition. Staging was updated retrospectively to the 7th edition by using the histopathological reports. Clinicopathological data were obtained from medical charts as well as pathological and surgical reports. The pathological parameters were carefully reviewed in all cases and included age, sex, T-classification, N-classification, resection margins, UICC stage, extracapsular spread, histologic grade (G), treatment, lymphangiosis, hemangiosis, perineural invasion, and survival data. The clinical characteristics of the patients are listed in Table 1. The mean patient follow-up time for all patients was 46.1 months. Median follow-up for all patients was 39 months with standard deviation of 38 months.
Treatment strategies
Treatment included radical surgery and neck dissection depending on the tumor stage. Patients, who were clinically classified as cN0 received selective neck dissection at least of the level I-III/IV. Patients with clinically positive cervical lymph node status (cN+) or histopathologically proven lymph node metastasis (pN+) were treated with a modified radical neck dissection of levels I–V. Whenever bilateral cervical lymph node metastasis was present, we performed a bilateral neck dissection. Surgery in combination with postoperative radiotherapy was chosen for locally advanced disease. Radiotherapy included daily doses of 1.8–2.0 Gy 5 days per week for a total dose of 60–65 Gy, as chemotherapy regimen carboplatin was administered in weeks 1 and 5. In cases with limited disease, only surgery was performed.
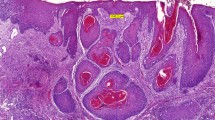
Tissue samples
Histopathological analysis of lymph nodes was performed at the Institute of Pathology, University of Cologne. After fixation of the lymph nodes in 5% formaldehyde, they were embedded in paraffin. Longitudinal bisection and further sectioning were obtained if the thickness was larger than 2 mm. From each paraffin block, two-step sections were cut at 50 μm levels. Afterward, staining was performed with hematoxylin and eosin, as well as periodic acid-Shiff, to histologically examine the presence or absence of metastatic disease. All specimens were evaluated by two independent, experienced pathologists.
Statistical analysis
Survival data were calculated by using the Kaplan-Meier method. Prognostic factors were identified in univariate analysis through the log-rank test. Clinicopathological parameters were explored in multivariate analysis through the Cox proportional hazard regression model. The significance level was set at p < 0.05. All statistical analyses were performed using SPSS Statistics 24.0 (IBM Corporation, Armonk, NY, USA).
Scoring system
Histological grade G1 or G2 were assigned 0 points and G3 or G4 1 point. Invasion of the lymphatic vessels, blood vessels, or perineural space was given 1 point. Zero points were given, when invasion was not detectable. The final score was conducted through addition of each parameter. Therefore, our scoring system ranged between 0 and 4 points.
Results
Patient characteristics
At the time of diagnosis, patients had a mean age of 61.46 years (standard deviation 11.5). Median age was 61.50 years.
Parameters predicting overall survival and disease-free survival in patients with OSCC
Table 2 displays the results from the univariate analysis of associations between the OSCC-Histoscore and clinicopathologic parameters. T-classification (p < 0.001), N-classification (p < 0.001), cervical lymph node metastasis (p < 0.001), UICC stage (p < 0.001), extracapsular spread (p < 0.001), and locoregional recurrence (p < 0.001) correlated significantly with the OSCC-Histoscore. None of the pathological specimens were classified as G4 (see Table 1).
Five-year OS was associated significantly with hemangiosis carcinomatosa (p < 0.001), lymphangiosis carcinomatosa (p < 0.001), perineural invasion (p < 0.001), and histological grade (p < 0.001). Also, OSCC-Histoscore was significantly associated with OS (p < 0.001). The higher the score, the poorer the prognosis. As shown in Fig. 1, overall survival noticeably decreased for patients with an OSCC-Histoscore more than 1. Patients with 4 points even had a 5-year OS rate of 0%. As shown in Fig. 2, the higher the score, the higher the risk of locoregional recurrence in the next 5 years. For patients with 3 or 4 points, locoregional control over the next 5 years was 0%. For patients with an OSCC-Histoscore of 1 point or more, we observed that a surgical therapy combined with radiochemotherapy was associated with a higher overall survival rate (45%) than surgery with radiotherapy (28%) alone. For patients classified with an OSCC-Histoscore of 0 points, surgery alone was associated with the highest 5-year OS compared to surgery combined with radiotherapy or radiochemotherapy.
In multivariate analysis, as shown in Table 3, T-classification (p = 0.001), N-classification (p = 0.039), and resection margins (p = 0.038) were independent prognostic factors for overall survival rate. The most significant independent prognostic factor was OSCC-Histoscore (p < 0.001). Especially, an OSCC-Histoscore of 0 vs. 1 showed the most significant difference.
Discussion
Tumor invasion into lymphatic and/or blood vessels, perineural invasion, and grading are frequently determined for histological evaluation of tumor progression and prognosis of oral squamous cell carcinoma (OSCC) [16,17,18,19]. A large number of studies demonstrated the significant importance of these parameters for assessment of tumor aggressiveness and therefore demanded their implementation into TNM classification [16,17,18,19]. However, the notable increase in the number of subgroups would lead to a more difficult and less representative staging system. Hence, an easily applicable scoring system, considering the histopathological characteristics of OSCC, would be of high prognostic and therapeutic value. Therefore, we investigated statistically, whether a combination of perineural invasion, blood vessel invasion, lymph vessel invasion and grading, into a novel scoring system (OSCC-Histoscore), might be helpful to overcome this issue. Uni- and multivariate analysis determined the OSCC-Histoscore as a strong independent prognostic parameter. Interestingly, multivariate analysis revealed a prognostic superiority of the OSCC-Histoscore compared to the T- and N-classification, showing the significant importance of the biological characteristics of OSCC (see Table 3).
Within the scoring system, we found that the higher the score, the worse the prognosis. For example, patients, assigned with 0 points had a 5-year overall survival rate of 89%, whereas none (0%) of the patients with 3 points had a 5-year overall survival (see Fig. 1).
Furthermore, we discovered a strong significant correlation between the OSCC-Histoscore and the occurrence of cervical lymph node metastasis (N-classification) and extracapsular spread. This reflects the fact that especially invasion into lymph vessels and blood vessels shows the metastasizing potential of OSCC [20, 21].
Invasion of lymphatic and/or blood vessels is defined as the presence of neoplastic epithelium within an endothelial-lined channel [22]. Approximately 50% of head and neck squamous cell carcinoma shows vascular invasion ([19]. Tumors with aggressive biological activity and therefore poor prognosis are significantly associated with vascular invasion [19]. In particular, lymphatic vessel invasion represents an independent prognostic factor for cervical lymph node metastasis [23]. A shortcoming of our study, which includes patients with OSCC from 2002 to 2009, is the technique of staining, as this plays a significant role for identification of blood vessel and lymph vessel invasion [24]. Due to our H&E staining technique, it might be that more specific methods, such as D2-40 would have been a better choice to differentiate such pathological alterations [24]. Van den Eyden et al. indicated that D2-40 and podoplanin are the most sensitive and specific antibodies for the detection of lymphatic endothelium [24]. Hence, it would be advisable in future studies to use more specific and more sensitive staining techniques.
In addition, the OSCC-Histoscore was significantly associated with T-classification. This might be explained by the finding that the histopathological parameters considered in the OSCC-Histoscore commonly occur in advanced stage diseases [16,17,18,19,20,21].
Furthermore, our multivariate analysis indicated that the OSCC-Histoscore is a better prognostic marker than the status of the resection margins (see Table 3). We assume that this might be associated with the fact that the OSCC-Histoscore is a combination of independent prognostic parameters, which significantly increase the prognostic power, thus leading to an even higher prognostic impact than the resection margins. On the other hand, this finding might be associated with the relatively small patient groups included into our subgroup analyses, as a result of the retrospective nature and single-center data of our study.
The first published biological scoring system for malignancies was published by Broders et al. in 1920 [15]. Their classification system was based upon the biological activity of tumors, graded as poorly, moderately, or highly differentiated [15]. They pointed out that poorly differentiated tumors, in particular, were associated with lower survival rates, due to their significant association with cervical lymph node metastasis [15]. Multiple subsequent studies confirmed these results, so that implementation of histological grading into the assessment of malignancies became diagnostic standard [14, 19, 25]. In accordance with Frierson et al. and Brandwein-Gensler et al., we differentiated between G1/G2 and G3, because patients with G3 have a significantly higher risk to develop cervical lymph node metastasis [26,27,28]. Furthermore Giacomarra et al. found out that prognosis for patients with a high grade OSCC is significantly worse than patients with G1 or G2 tumors [29].
In 1973, Jacobsson et al. propagated a new scoring system, which mainly focused on tumor cell population and tumor host relation [30]. They included the following eight histological features: tumor cell structure, differentiation, nuclear polymorphism, mitosis, mode of invasion, stage of invasion, vascular invasion, and cellular response [30]. In accordance with the malignancy grade of the tumor, they assigned for each feature 0 to 4 points [30]. Although this classification system allows a very detailed and informative description of the tumor biology, the main disadvantage is the unprecise definition of the included tumor parameters [14, 19]. Therefore, standardization and comparison of the gathered data have a high risk of being biased [14, 19]. In 1997, Bryne et al. developed a modification of the system of Jacobsson et al. and focused on the invasive front of the tumor (IFG) [31]. They assessed the degree of keratinization, nuclear polymorphism, pattern of invasion, and host inflammatory response [31]. IFG was highlighted and confirmed by multiple subsequent studies as an independent prognostic parameter for patients with OSCC [14, [19, 25]. Further modifications of the system of Jacobsson et al. were made by Lund et al., Willen et al., Anneroth et al., Crissman et al., or Martinez-Gimeno et al. [32,33,34,35,36]. However, their implementation into clinical practice has not been established yet [14, 19, 25]. Compared with these grading systems, the main advantages of our presented OSCC-Histoscore are, on the one hand, that the included parameters are determined routinely in daily clinical practice and, on the other hand, that it is easily applicable.
Conclusions
For patients with oral squamous cell carcinoma (OSCC), our presented OSCC-Histoscore serves an independent prognostic parameter for 5-year overall survival (OS) and predicts OS better than T-classification, N-classification, and resection margins. However, further studies, especially conducted on larger cohorts, are necessary to evaluate our findings and to improve understanding of the biological behavior of OSCC.
References
Vormittag L, Thurnher D, Geleff S, Pammer J, Heiduschka G, Brunner M, Grasl M, Erovic BM (2009) Co-expression of Bmi-1 and podoplanin predicts overall survival in patients with squamous cell carcinoma of the head and neck treated with radio (chemo)therapy. Int J Radiat Oncol Biol Phys 73(3):913–918
Kreppel M, Dreiseidler T, Rothamel D, Eich HT, Drebber U, Zoller JE, Scheer M (2013) The role of clinical versus histopathological staging in patients with advanced oral squamous cell carcinoma treated with neoadjuvant radiochemotherapy followed by radical surgery. J Craniomaxillofac Surg 41(1):22–27
Jemal A, Siegel R, Ward E, Hao Y, Xu J, Thun MJ (2009) Cancer statistics, 2009. CA Cancer J Clin 59(4):225–249
Safi AF, Kauke M, Grandoch A, Nickenig HJ, Zoller JE, Kreppel M (2017) Analysis of clinicopathological risk factors for locoregional recurrence of oral squamous cell carcinoma - retrospective analysis of 517 patients. J Craniomaxillofac Surg 45(10):1749–1753
Safi AF, Kauke M, Grandoch A, Nickenig HJ, Drebber U, Zoller J, Kreppel M (2017) Clinicopathological parameters affecting nodal yields in patients with oral squamous cell carcinoma receiving selective neck dissection. J Craniomaxillofac Surg 45:2092–2096
Safi AF, Kauke M, Grandoch A, Nickenig HJ, Drebber U, Zoller J, Kreppel M (2017) The importance of log odds of positive lymph nodes for locoregional recurrence in oral squamous cell carcinoma. Oral Oncol 72:48–55
Safi AF, Grandoch A, Nickenig HJ, Zoller JE, Kreppel M (2017) Importance of lymph node ratio for locoregional recurrence of squamous cell carcinoma of the buccal mucosa. Head Neck 39:2488–2493
Safi AF, Grandoch A, Nickenig HJ, Zoller JE, Kreppel M (2017) The importance of lymph node ratio for locoregional recurrence of squamous cell carcinoma of the tongue. J Craniomaxillofac Surg 45(7):1058–1061
Bloebaum M, Poort L, Bockmann R, Kessler P (2014) Survival after curative surgical treatment for primary oral squamous cell carcinoma. J Craniomaxillofac Surg 42(8):1572–1576
Feller L, Lemmer J (2012) New ‘second primary’ cancers. SADJ 67(4):175–178
Martin-Villar E, Scholl FG, Gamallo C, Yurrita MM, Munoz-Guerra M, Cruces J, Quintanilla M (2005) Characterization of human PA2.26 antigen (T1alpha-2, podoplanin), a small membrane mucin induced in oral squamous cell carcinomas. Int J Cancer 113(6):899–910
Patel V, Leethanakul C, Gutkind JS (2001) New approaches to the understanding of the molecular basis of oral cancer. Crit Rev Oral Biol Med 12(1):55–63
Greene FL, Sobin LH (2002) The TNM system: our language for cancer care. J Surg Oncol 80(3):119–120
Po Wing Yuen A, Lam KY, Lam LK, Ho CM, Wong A, Chow TL, Yuen WF, Wei WI (2002) Prognostic factors of clinically stage I and II oral tongue carcinoma-a comparative study of stage, thickness, shape, growth pattern, invasive front malignancy grading, Martinez-Gimeno score, and pathologic features. Head Neck 24(6):513–520
Broders AC (1920) Squamous-cell epithelioma of the lip: a study of five hundred and thirty-seven cases. J Am Med Assoc 74(10):656–664
Maddox WA, Urist MM (1990) Histopathological prognostic factors of certain primary oral cavity cancers. Oncology (Williston Park, NY) 4(12):39–42 discussion 42, 45–6
Olsen KD, Caruso M, Foote RL, Stanley RJ, Lewis JE, Buskirk SJ, Frassica DA, DeSanto LW, O'Fallon WM, Hoverman VR (1994) Primary head and neck cancer: histopathologic predictors of recurrence after neck dissection in patients with lymph node involvement. Arch Otolaryngol Head Neck Surg 120(12):1370–1374
Woolgar JA (1999) T2 carcinoma of the tongue: the histopathologist’s perspective. Br J Oral Maxillofac Surg 37(3):187–193
Smith BD, Haffty BG (2009) Prognostic factors in patients with head and neck cancer. Head and neck cancer: a multidisciplinary approach, 3rd edn. Lippincott Williams & Wilkins, Philadelphia, pp 51–75
Kreppel M, Scheer M, Drebber U, Ritter L, Zoller JE (2010) Impact of podoplanin expression in oral squamous cell carcinoma: clinical and histopathologic correlations. Virchows Arch 456(5):473–482
Safi AF, Nickenig HJ, Rothamel D, Zirk M, Thiele O, Grandoch A, Scheer M, Zinser M, Zoller J, Drebber U, Kreppel M (2015) Expression of ezrin in oral squamous cell carcinoma: prognostic impact and clinicopathological correlations. J Craniomaxillofac Surg 43(9):1899–1905
Close LG, Brown PM, Vuitch MF, Reisch J, Schaefer SD (1989) Microvascular invasion and survival in cancer of the oral cavity and oropharynx. Arch Otolaryngol Head Neck Surg 115(11):1304–1309
Michikawa C, Uzawa N, Kayamori K, Sonoda I, Ohyama Y, Okada N, Yamaguchi A, Amagasa T (2012) Clinical significance of lymphatic and blood vessel invasion in oral tongue squamous cell carcinomas. Oral Oncol 48(4):320–324
Van den Eynden GG, Van der Auwera I, Van Laere SJ, Colpaert CG, van Dam P, Dirix LY, Vermeulen PB, Van Marck EA (2006) Distinguishing blood and lymph vessel invasion in breast cancer: a prospective immunohistochemical study. Br J Cancer 94(11):1643–1649
Doshi NP, Shah SA, Patel KB, Jhabuawala MF (2011) Histological grading of oral cancer: a comparison of different systems and their relation to lymph node metastasis. National Journal of Community Medicine 2(1):136–142
Brandwein-Gensler M, Smith RV, Wang B, Penner C, Theilken A, Broughel D, Schiff B, Owen RP, Smith J, Sarta C, Hebert T, Nason R, Ramer M, DeLacure M, Hirsch D, Myssiorek D, Heller K, Prystowsky M, Schlecht NF, Negassa A (2010) Validation of the histologic risk model in a new cohort of patients with head and neck squamous cell carcinoma. Am J Surg Pathol 34(5):676–688
Frierson HF Jr, Cooper PH (1986) Prognostic factors in squamous cell carcinoma of the lower lip. Hum Pathol 17(4):346–354
Hibbert J, Marks NJ, Winter PJ, Shaheen OH (1983) Prognostic factors in oral squamous carcinoma and their relation to clinical staging. Clin Otolaryngol Allied Sci 8(3):197–203
Giacomarra V, Tirelli G, Papanikolla L, Bussani R (1999) Predictive factors of nodal metastases in oral cavity and oropharynx carcinomas. Laryngoscope 109(5):795–799
Jakobsson P, Eneroth CM, Killander D, Moberger G, Mårtensson B (1973) Histologic classification and grading of malignancy in carcinoma of the larynx. Acta radiologica: therapy, physics, biology 12(1):1–8
Bryne M, Boysen M, Alfsen CG, Abeler VM, Sudbø J, Nesland JM, Kristensen GB, Piffko J, Bankfalvi A (1997) The invasive front of carcinomas. The most important area for tumour prognosis? Anticancer Res 18(6B):4757–4764
Lund C, Sosgaard H, Elbrønd O, Jørgensen K, Andersen AP (1975) Epidermoid carcinoma of the lip histologic grading in the clinical evaluation. Acta radiologica: therapy, physics, biology 14(5):465–474
Willen R, Nathanson A, Moberger G, Anneroth G (1975) Squamous cell carcinoma of the gingiva: histological classification and grading of malignancy. Acta Otolaryngol 79(1–2):146–154
Anneroth G, Batsakis J, Luna M (1987) Review of the literature and a recommended system of malignancy grading in oral squamous cell carcinomas. Scand J Dent Res 95(3):229–249
Crissman JD, Gluckman J, Whiteley J, Quenelle D (1980) Squamous-cell carcinoma of the floor of the mouth. Head Neck Surg 3(1):2–7
Vila CN, Martínez-Gimeno C, Rodríguez EM, Varela CL (1995) Squamous cell carcinoma of the oral cavity: a clinicopathologic scoring system for evaluating risk of cervical lymph node metastasis. Laryngoscope 105(7):728–733
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical approval
Due to the retrospective nature of this study, it was granted an exemption in writing by the University Hospital of Cologne IRB. Our investigation followed the guidelines of the Helsinki Declaration. This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
For this type of study, formal consent is not required.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Safi, AF., Grochau, K., Drebber, U. et al. A novel histopathological scoring system for patients with oral squamous cell carcinoma. Clin Oral Invest 23, 3759–3765 (2019). https://doi.org/10.1007/s00784-019-02804-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-019-02804-4