Abstract
Objective
To assess the effectiveness of atraumatic restorative treatment (ART) performed 4 years ago in babies suffering from early childhood caries (ECC), and to compare the clinical performance of ART atraumatic restorations performed with two different high-viscosity glass ionomer cements (GIC).
Materials and methods
This was a longitudinal follow-up of a randomized, double-blind, split-mouth-type clinical trial. The initial sample was composed of 100 deciduous molars with occlusal lesions in 25 children with ages between 18 and 36 months who received ART with two different GICs: Ketac Molar Easymix® (3 M ESPE) and Vitro Molar® (DFL). The clinical assessments were performed by a trained, blind examiner gauged by the parameters assessed in 1, 2, and 4 years (ART and USPHS criteria).
Results
For the analysis of the clinical performance of ARTs between the different GICs, the chi-square and Mann–Whitney tests were applied (p < 0.05). In the 4 years of evaluation, the sample was composed by 76 ARTs and 19 children, with 94.7% of the treatments having inactivated the cavity process. The total success percentage of the ARTs was 94%, 87.5%, and 82.9%, in 1, 2, and 4 years of follow-up, respectively. Moreover, among the GICs studied, this difference was not statistically significant (p > 0.05) (ClinicalTrials.gov NCT03756025).
Conclusion
ART was effective in handling ECC, with an excellent clinical performance of ART restorations, for both GICs, during the 4 years of follow-up.
Clinical relevance
ART, with both GIC studied, is an alternative therapy for ECC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Dental cavity is one of the most prevalent diseases in childhood, and for this reason it is considered a major public health problem [1, 2]. Despite the efforts to control the disease at the global level, the percentage of untreated cavities is still high, and the reparation of its sequels generates significant economic impact [3, 4]. Cavity development results from the interaction of a series of factors that incur in the loss of mineral structures of the dental element. The cavity process is dynamic and fluid in nature, characterized by an imbalance between etiological and protective factors, the main pathological determinants being bacteria and the consumption of fermentable carbohydrates (sugars), while protective factors include salivary flow and exposure to fluorides [5]. Thus, a caries reduction in adolescents of 8 to 37% by water fluoridation has been observed [6], and around 25% by topical fluoride therapies when compared with no treatment with fluoride [7]. Despite the access to fluoridated water and the use of homemade or professional fluorides, tooth decay remains a challenge. Sheiham and James [8] point to sugar as the primary and necessary factor for the development of caries, emphasizing the cumulative effect of sugar consumption throughout life. For small children, contact with sugary foods should be delayed as long as possible, preferably past 2 years of age, and limited to a maximum of 10% of daily caloric intake being composed of free sugar [9].
When caries affect children under 6 years of age, it is called early childhood caries (ECC), and is considered severe childhood caries (SCC) when it occurs in children less than 3 years of age [10]. In those young children, caries disease manifests aggressively, leading to the complete destruction of dental crowns in a short period of time, which can develop into situations so severe that it will negatively affect the growth and development of affected babies. Due to its crippling features, ECC has the potential to adversely impact a child’s quality of life; for example, severe caries lesions cause discomfort, pain, infection, and abscesses that hinder adequate food consumption and consequently cause malnutrition, which, in turn, can lead to retardation of physical growth and cognitive behavior. In addition, esthetic discomfort can cause relationship and self-esteem psychological problems [11].
Some researchers sought to expand the basic microbiological model of early-onset cavities, including social factors, as well as demographic and behavioral factors such as ethnicity, income, family status, level of maternal education, brushing habits and oral hygiene knowledge, and parents’ beliefs [12,13,14]. Some clinical trials have demonstrated the effectiveness of health promotion programs and education on ECC reduction through early intervention with pregnant women and mothers of newborns, providing information on how to deal with food intake, breastfeeding, and oral hygiene compatible with good oral health for children [15,16,17,18]. In this sense, any dental treatment that is based only on curative and punctual interventions, while disregarding the multifactorial nature of dental caries and periodontal disease, will fail in achieving positive child health. Therefore, the use of a comprehensive approach that can control the disease, rehabilitate through restorative procedure, and also promote good patient health is paramount.
Within this perspective, an unconventional method for caries treatment called atraumatic restorative treatment (ART) was developed in the mid-1980s and presented to the members of the World Health Organization (WHO) in 1994. The ART program has three bases: education for health; efforts toward caries and gingivitis diseases prevention; and atraumatic restorative technique, based on minimal intervention (MI) principles. ART with MI consists of the removal of the cavity tissue through excavation of infected dentine only with manual sharp instruments, under relative isolation, without the use of anesthesia, and, after cavity cleaning, filling with a fluoride-releasing adhesive material called glass ionomer cement (GIC) [19, 20].
Clinical trials have evaluated the performance of ART in deciduous teeth, showing quite acceptable survival rates, ranging between 65 and 96.7% for restoration of a surface. However, the ART of one or more surfaces has presented lower success rates (31–76.1%), even using GIC with better properties [21,22,23,24,25]. When comparing ART with restorations of amalgam in deciduous teeth, statistically significant differences have not been found among the groups after 12 and 24 months [26].
Considering the severity and high prevalence of ECC, as well as the importance of early intervention and approach, the Atraumatic Restorative Treatment program, because of its advantages, consists of an important treatment alternative. However, only a few studies assess ART in babies affected by ECC. For this practice to be accepted as safe, scientific evidence must be built through longitudinal studies to evaluate ART performance, and to this end, the present study is justified. Therefore, the aim of this research was to evaluate the effectiveness of atraumatic restorative treatment performed in babies suffering from ECC after a 4-year period and compare the clinical performance of atraumatic restorations performed with two different glass ionomer cements. Our hypothesis is that there is no difference in the clinical performance of ARTs performed with the different GICs.
Materials and methods
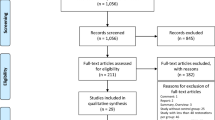
The study is characterized by longitudinal follow-up of a randomized, double-blind, split-mouth-type clinical trial performed in babies affected by early childhood caries. The subjects were children of both sexes, aged between 18 and 36 months, with at least one deciduous molar in each of the different dental quadrants, presenting active cavitated lesions of shallow or medium depth, involving only the occlusal surface. The initial convenience sample consisted of 100 deciduous molars of 25 children attending Bebê Clínica of the School of Dentistry of the Federal University of Rio Grande do Sul-FO/UFRGS, Porto Alegre-RS, Brazil, this number being based on similar studies published in the literature [27,28,29]. The power of the sample was calculated using the PEPI program, version 4 (Computer Programs for Epidemiologists), for a significance level of 5%. Considering that the average success percentage in 2 years of ART on primary teeth facings was 88%, and the worst result found was 67% [30], the power obtained was of 70.1%.
All children in the study were enrolled in the oral health promotion program for babies, in which mothers accompanied by their children individually received information and guidance on food intake, breastfeeding, and oral hygiene. In addition to the guidance that was reinforced at each visit, children received topical application of fluoride by brushing with acidulated phosphate fluoride gel in four applications with intervals of 1 week, considering that all had active cavities [31].
The clinical trial was performed through the experimental split-mouth model, in which the 25 selected children had their teeth (deciduous molar in each of the different dental quadrants) distributed randomly through a random number table, receiving ART restorations of a face with one of the two high-viscosity conventional glass ionomer cements studied: Vitro Molar® (DFL, Rio de Janeiro, Brazil) and Ketac Molar Easymix® (3 M ESPE, St. Paul, MN, USA). The atraumatic restorations were performed in the dental office by a single operator trained in the ART Technique [20], who received the restorative material already prepared by a trained auxiliary, ensuring blinding of the study. The restorative procedure performed in relative isolation and without the use of anesthesia consisted of removal of the carious tissue using hand instrument excavators and dentin spoons, with subsequent conditioning of the cavity with a polyacrylic acid solution at 11.5% (DFL) applied with a microbrush for 10 s. Immediately after, the cavity was washed and dried with cotton balls. In this step, according to the randomization, the respective GIC was inserted and subsequent digital compression was performed for 30 s. After occlusal adjustment, the ARTs were protected with finish gloss Alfa Bond® (DFL).
Clinical assessments were carried out in three stages: after 1, 2, and 4 years. For this, the oral health status of the children was assessed by the presence of visible plaque and caries activity, and the quality of ART restorations by the ART criterion (Table 1) [20]. In the exams at 4 years, an additional assessment was done by means of the modified United States Public Health Service (USPHS) criteria (Table 2) [32] and the Visible Plaque Index (VPI) and Gingival Bleeding Index (GBI) [33]. Each evaluation was performed by a different blind examiner for the type of GIC used in ART and calibrated with the respective intra-examiner correlation coefficients: 1 year (ART criterion: kappa = 0.81), 2 years (ART criterion: kappa = 0.83), and 4 years (ART criterion: kappa = 0.86; modified USPHS criteria: kappa average = 0.73; VPI: kappa = 0.79; caries activity: kappa = 1.0).
For the analysis of the general clinical performance of ART, through the success rate among the different GICs, the chi-square test was applied. In addition, the Mann–Whitney test was used to compare each individual clinical criterion between the materials (retention and anatomical shape, integrity and marginal discoloration, color of material, surface roughness, and secondary caries), with all tests at the level of significance of 5% (p < 0.05). The visible plaque index (VPI) and gingival bleeding index (GBI) as well as caries activity were expressed through frequency distribution.
Database construction and analysis and interpretation of results were obtained by using the Statistical Package for the Social Sciences (SPSS), version 19.0.
The initial research project, as well as the longitudinal evaluation, were submitted to and approved by the Research Ethics Committee of the School of Dentistry/UFRGS, recorded respectively by processes # 160/04 - Minutes No. 11/04 and No. 13027 - Minutes No. 03/08. All parents or guardians of the children signed a consent form. The trial was registered at ClinicalTrial.gov (NCT03756025).
Results
The initial study consisted of 25 children and 100 ART restorations, and at the 1-year evaluation there were no losses in the sample. However, at the 2-year evaluation, it changed to 20 children and 80 ARTs, totaling a loss percentage of 20% of subjects and restorations. At the last evaluation, at 4 years, this number remained almost the same, closing with a sample of 19 children and 76 atraumatic restorations, with a mean age of 6.2 years at that stage, harmoniously shared between the sexes: female (52.6%) and male (47.4%).
The oral health status of children during the study period is shown in Table 3. It is observed that the caries activity was controlled within 4 years, ending with 94.7% of children without disease activity. Regarding the presence of visible plaque, the percentages varied; however, low VPI and GBI (< 20%) prevailed in the 4 years of evaluation.
Regarding the clinical performance of ART restorations, as shown in Table 4, there is a percentage of overall success of 94%, 87.5%, and 82.9% in 1, 2, and 4 years of follow-up, respectively. Moreover, among the GICs studied, this difference was not statistically significant (p > 0.05).
In Fig. 1, statistically significant difference is not observed over the 4 years when comparing the losses of atraumatic restorations using two different GICs through the log-rank test (p = 0.223).
Table 5 shows the clinical performance of ARTs according to each individual criterion (USPHS) between the GICs in the 4-year evaluation. It is observed that in all individual clinical criteria the success percentage was considered high for both GICs, with no statistically significant difference between them (p > 0.05). The criteria that showed greater failure were anatomical shape (n = 8), marginal integrity (n = 8), and retention (n = 6). Five of the ARTs have been replaced by other restorations at other dental services, which rendered the evaluation impossible.
Discussion
Longitudinal clinical trials are among the studies with a higher degree of scientific evidence, on which clinical practices should be based. However, they present, as a limiting factor, the loss of follow-up with patients, which in many cases might compromise the validity of the results. In this study, in a 4-year follow-up that began with 25 patients and 100 restorations, the sample loss was considered low (20% and 24% of teeth in 2 and 4 years, respectively), compatible with other studies on ART, but with more follow-up time (6 years) [34, 35]. Among the six patients lost, the reason for the loss of five of them was change in phone contact and address information and one who had the follow-up done at a private dental care service, refusing to return to the research.
The clinical criteria used for evaluation of restorative treatments are of utmost importance in the validity of the results. Traditionally, studies evaluating ART in the field used their own criteria developed to assess ARTs, which includes technical particularities [20]. However, the need to compare the quality of ART with traditional restorative treatments boosted the modification of the evaluation criteria, and from then on, the USPHS criteria by Ryge [32] became prevalent. However, some studies on ART proposed to use both methods simultaneously in order to compare them, and the results suggest similarity and comparability between ART and USPHS criteria [36, 37] and other more recent ones, such as the FDI criteria [38]. This justifies the use of the USPHS criteria in addition to the ART criteria in the 4-year evaluation in the present study. Thus, it is possible to carry out a more detailed assessment through USPHS and compare these findings with the study that used both criteria.
According to Tinanoff and Reisine [13], due to its high prevalence, its impact on quality of life of young children, and the potential risk factor for caries in the permanent dentition, early childhood caries is undoubtedly one of the most serious health conditions among children. A necessary first step in preventing dental caries in preschool children is to understand and assess the child’s caries risk factors. Previous experience of caries and white spot lesions should automatically be classified as high caries risk. In addition, frequency of sugar consumption, hypoplasia, and enamel defects, socioeconomic, psychosocial, and ethnic factors have also been relevant in determining the risk of caries. Based on this knowledge of specific risk factors for each individual, different strategies for prevention and treatment should be implemented, including parent-supervised fluoride therapy by daily tooth brushing with fluoride toothpaste, and professional topical fluoride application with varnish or fluoride gel. Guidance and intensive counseling with parents should also be highlighted, considering that motivating the change of specific habits and behaviors can reduce the occurrence of caries in children [13]. Based on these principles and on atraumatic restorative treatment, the Bebê Clínica program of the School of Dentistry/UFRGS has been supporting ECC management [31].
The oral health status of children involved in the study was assessed based on the caries activity, visible plaque, VPI, and GBI. From the point of view of caries disease management, the ART program has proven to be effective, because after 4 years of evaluation, 94.7% of children had inactive caries, featuring control of the carious process. There is evidence in the literature indicating that good oral hygiene reduces plaque and prevents gingivitis; thus, manual brushing with fluoridated toothpaste remains the most widely used and effective method for the prevention of caries and gingivitis [39, 40]. For this reason, in order to infer the quality of oral hygiene of the children, the presence of visible plaque was evaluated, and these results showed a considerable number of variables over the three assessments. This can be partly explained by the fact that the evaluation of the visible plaque presents some limitations, in that it does not determine the amount and extent of plaque buildup, and therefore, regardless of whether the child has plaque buildup on one or all dental surfaces, it will be considered the same way.
In an attempt to minimize this bias in the 4-year assessment, VPI and GBI, which represent the percentage of affected surfaces, have been included, allowing for the results to be better analyzed. Although 89.5% of children have visible plaque, the VPI and GBI data lead us to a small extent of plaque buildup, as 94.7% of children had rates lower than 20%, and only one child had VPI and GBI greater than 20% (the same child who had caries activity), which denotes the lack of control of etiological factors in general. Despite the importance of these indexes for assessing the quality of oral hygiene, few studies consider VPI and GBI in young children, making it difficult to compare the data obtained in this study.
Some intervention programs based on educational and preventive activities with preschool children have shown significant improvements in their oral hygiene pattern. Junqueira [41] observed reduction of the VPI from 58.98% to 10.00% in all children who participated in his study. Guarienti [42] achieved a VPI reduction from 33.4% to 6.9%, and from 24.0% to 2.6% in GBI of preschool children after a year of preventive work and education in oral health. When compared to these results, the conditions of oral hygiene and biofilm control account for the effectiveness of the ART program for children with ECC, using the individual approach.
Few studies published evaluate ART in infants who were affected by ECC, and there are few longitudinal follow-up reports of more than 3 years in primary teeth. The findings of this study reflect an optimal clinical performance of ARTs through a percentage of overall success of 94%, 87.5%, and 82.9% in 1, 2, and 4 years of follow-up, respectively. In a meta-analysis conducted by van’t Hof et al. (2006), a median survival of ARTs of one surface in primary teeth of 95% (87–99%) and 91% (67–94%) were found at the 1- and 2-year follow-up, respectively. In a more recent meta-analysis [43], the authors found the following success percentages for one-face ARTs in primary teeth: 1 year (95% IC91–98), 2 years (93% IC91–94), and 3 years (66% IC13–99), rates similar to the ones found in this study. Even with similar success percentages, it should be noted that the studies evaluated by meta-analysis were performed with older children with an average age of 6 years, who presented a more favorable behavioral management than very young babies, which may influence the outcome of the treatment.
Faccin et al. [44] evaluated ARTs in preschool children, aged 31 months on average, performed by dental students at the dental office. They found a lower survival percentage (72%) than those in the present study (82.9%), with a trial period between 25 and 48 months, even using a resin-modified glass ionomer cement RMGIC, which usually has a better performance than the conventional GIC. The authors have also found that the success rates were not influenced by age, suggesting the feasibility of ART in young children, a fact confirmed by the current study findings. Thus, it is possible to assert that ART is a child-friendly technique because it is less uncomfortable, painful, and traumatic for them.
By comparing the clinical performance between the GICs studied based on the individual criteria of UPSHS, no statistically significant difference was observed. Among the criteria that presented more failures, the highlights are anatomical shape, marginal integrity, and retention. Possible causes of such failures that may be associated with physical properties of the GICs have been reported in the literature [45,46,47], the caries removal technique [47], and the skill and training of the operator [30, 46, 47]. The low failure rates may be associated with control of these variables in this study, considering that the ARTs were performed by a single operator trained in the technique with two high-viscosity GICs appropriate for ART. Besides, it is important to note that even though some ARTs failed due to total or partial loss of the material or an unacceptable marginal condition, none of them showed secondary caries. This situation must be linked to the fact that children have controlled their caries processes through educational and preventive programs, in addition to the GIC fluoride-release property associated with low-caries recurrence rates in other studies as well [23, 45, 48].
The general comparison between different GICs showed that the two materials behave similarly in ART restorations in babies with ECC, given that the two GICs are of high viscosity and developed specifically for the ART technique. Therefore, the hypothesis of this study was accepted.
Conclusion
It is concluded that atraumatic restorative treatment was effective in handling early childhood caries, with an excellent clinical performance of ART restorations, for both GICs, during the 4 years of follow up.
References
Weinstein P (1998) Public health issues in early childhood caries. Community Dent Oral Epidemiol 26:84–90
Berkowitz RJ (2003) Causes, treatment and prevention of early childhood caries: a microbiologic perspective. J Can Dent Assoc 69:304–307
Listl S, Galloway J, Mossey PA, Marcenes W (2015) Global economic impact of dental diseases. J Dent Res 94:1355–1361. https://doi.org/10.1177/0022034515602879
Kassebaum NJ, Bernabé E, Dahiya M, Bhandari B, Murray CJ, Marcenes W (2015) Global burden of untreated caries: a systematic review and metaregression. J Dent Res 94:650–658. https://doi.org/10.1177/0022034515573272
Featherstone JB (2004) The continuum of dental caries—evidence for a dynamic disease process. J Dent Res 83(Spec Issue C):C39–C42
Newbrun E (1989) Effectiveness of water fluoridation. J Public Health Dent 49(5):279–289
Marinho VC, Higgins JP, Sheiham A, Logan S (2004) Combinations of topical fluoride (toothpastes, mouthrinses, gels, varnishes) versus single topical fluoride for preventing dental caries in children and adolescents. Cochrane Database Syst Rev 1:CD002781
Sheiham A, James WP (2015) Diet and dental caries—the pivotal role of free sugars reemphasized. J Dent Res 94:1341–1347. https://doi.org/10.1177/0022034515590377
World Health Organization (2015) Guideline: sugars intake for adults and children. World Health Organization, Geneva
American Academy of Pediatric Dentistry (AAPD) (2003) Policy on early childhood caries (ECC): unique challenges and treatment options. Pediatr Dent 24(Suppl):24–25
Graves CE, Berkowitz RJ, Proskin HM, Chase I, Weinstein P, Billings R (2004) Clinical outcomes for early childhood caries: influence of aggressive dental surgery. J Dent Child 71:114–117
Fraiz FC, Walter LRF (2001) Estudo de fatores associados à cárie dental em crianças que recebem atendimento odontológico precoce [study of factors associated with dental caries in children receiving early dental care]. Pesqui Odontol Bras 15:201–207
Tinanoff N, Reisine S (2009) Update on early childhood caries since the surgeon general's report. Acad Pediatr 9:396–403
Fontana M (2015) The clinical, environmental, and behavioral factors that foster early childhood caries: evidence for caries risk assessment. Pediatr Dent 37:217–225
Feldens CA, Vítolo MR, Drachler ML (2007) A randomized trial of the effectiveness of home visits in preventing early childhood caries. Community Dent Oral Epidemiol 35:215–223. https://doi.org/10.1111/j.1600-0528.2006.00337.x
Feldens CA, Giugliani ERJ, Duncan BB, Drachler ML, Vítolo MR (2010) Long-term effectiveness of a nutritional program in reducing early childhood caries: a randomized trial. Community Dent Oral Epidemiol 38:324–332. https://doi.org/10.1111/j.1600-0528.2010.00540.x
Plutzer K, Spencer AJ (2008) Efficacy of an oral health promotion intervention in the prevention of early childhood caries. Community Dent Oral Epidemiol 36:335–346. https://doi.org/10.1111/j.1600-0528.2007.00414.x
Harrison RL, Veronneau J, Leroux B (2012) Effectiveness of maternal counseling in reducing caries in Cree children. J Dent Res 91:1032–1037. https://doi.org/10.1177/0022034512459758
Frencken JE, Sognpaisan Y, Phantumvanit P (1994) Atraumatic restorative technique: evaluation after one year. Dent J London 44:460–464
Frencken JE, Holmgren CJ (2001) Tratamento Restaurador Atraumático (ART), para a cárie dentária [Atraumatic Restorative Treatment (ART) for dental caries]. Ed. Santos, São Paulo
Ersin N, Candan U, Aykut A, Önçag Ö, Eronat C, Kose T (2006) A clinical evaluation of resin-based composite and glass ionomer cement restorations placed in primary teeth using the ART approach – results at 24 months. Am Dent Assoc 137:1529–1536
van Den Dungen GM, Huddleston Slater AE, van Amerongen WE (2004) ART or conventional restorations? A final examination of proximal restorations in deciduous molars. Ned Tijdschr Tandheelkd 111:345–349
Lo E, Holmgren C (2001) Provision of atraumatic restorative treatment (ART) restorations to Chinese pre-school children at 30 month evaluation. Int J Paed Dent 11:3–10
Honkala E, Behbehani J, Ibricevic H, Kerosuo E, Al-Jame G (2003) The atraumatic restorative treatment (ART) approach to restoring primary teeth in a standard dental clinic. Int J Pediatr Dent 13:172–179
van Gemert-Schriks MCM, van Amerongen WE, Ten Cate JM, Aartman IHA (2007) Three-year survival of single- and two-surface ART restorations in a high-caries child population. Clin Oral Investig 11:337–343. https://doi.org/10.1007/s00784-007-0138-8
Mickenautsch S, Yengopal V, Banerjee A (2010) Atraumatic restorative treatment versus amalgam restoration longevity: a systematic review. Clin Oral Investig 14:233–240. https://doi.org/10.1007/s00784-009-0335-8
Figueiredo MC, Granville-Garcia AF (1996) A utilização do cimento ionômero de vidro FUJI IX na técnica de restauração atraumática (ART) em dentes decíduos [The use of FUJI IX glass ionomer cement in the technique of atraumatic restoration (ART) in deciduous teeth]. Rev Fac Odont UPF 1:31–38
Souza MIC, Medeiros UV, Santos PKG (1999) Avaliação clínica de alterações da microflora oral por meio da utilização do tratamento restaurador atraumático [clinical evaluation of oral microflora alterations through the use of atraumatic restorative treatment]. Rev Bras Odontol 56:34–37
Bresciani E, Nogueira DA, Henostroza QN, Barata TJE, Lauris JRP, Navarro MFL (2002) Influência do isolamento absoluto sobre o sucesso do tratamento restaurador atraumático (ART), em cavidades II em dentes decíduos [Influence of absolute isolation on the success of atraumatic restorative treatment (ART) in II cavities in deciduous teeth]. Rev Fac Odontol Bauru 10:231–237
van’t Hof MA, Frencken JE, van Palenstein Helderman WH, Holmgren CJ (2006) The atraumatic restorative treatment (ART) approach for managing dental caries: a meta-analysis. Int Dent J 56:345–351
Figueiredo MC, Guarienti CAD, Michel JA, Sampaio MS (2008) Comprehensive attention to oral health in early childhood: a longitudinal evaluation of the infant of the infant clinic program of the Federal University of Rio Grande do Sul, Brazil. Acta Odontol Latinoam 21:181–187
Ryge G (1980) Clinical criteria. Int Dent J 30:347–358
Ainamo J, Bay I (1975) Problems and proposals for recording gingivitis and plaque. Int Dent J 25:229–235
Lo EC, Holmgren CJ, Hu D, van Palenstein Helderman W (2007) Six-year follow up of atraumatic restorative treatment restorations placed in Chinese school children. Community Dent Oral Epidemiol 35:387–392
Frencken JE, Taifour D, van’t Hof MA (2006) Survival of ART and amalgam restorations in permanent teeth after 6.3 years. J Dent Res 85:622–626
Holmgren CJ, Lo EC, Hu D, Wan H (2000) ART restorations and sealants placed in Chinese school children: results after three years. Community Dent Oral Epidemiol 28:314–320
Ercan E, Dülgergil CT, Soyman M, Dalli M, Yildirim I (2009) A field-trial of two restorative materials used with atraumatic restorative treatment in rural Turkey: 24-month results. J Appl Oral Sci 17:307–314
Farag A, van der Sanden WJM, Abdelwahab H, Frencken JE (2011) Survival of ART restorations assessed using selected FDI and modified ART restoration criteria. Clin Oral Invest 15:409–415. https://doi.org/10.1007/s00784-010-0403-0
Leal SC, Bezerra ACB, Toledo AO (2002) Effectiveness of teaching methods for toothbrushing in preschool children. Braz Dent J 13:133–136
Conrado CA, Maciel SM, Oliveira MR (2004) A school-based oral health educational program: the experience of Maringá-PR, Brazil. J Appl Oral Sci 12:27–33
Junqueira FP (2004) Avaliação de um programa de tratamento restaurador atraumático modificado em crianças institucionalizadas de 02 a 05 anos. 89 p. Dissertação (Mestrado) [Evaluation of a modified atraumatic restorative treatment program in institutionalized children from 02 to 05 years old. 89 p. Dissertation (Master degree)] – Universidade Camilo Castelo Branco, Campinas
Guarienti CAD (2007) Avaliação da efetividade do Tratamento Restaurador Atraumático (ART) inserido em uma creche do município de Porto Alegre – RS. 93 p. Dissertação (Mestrado) [ Evaluation of the effectiveness of Atraumatic Restorative Treatment (ART) inserted in a day care center in the city of Porto Alegre - RS. 93 p. Dissertation (Master degree)] – Universidade Federal do Rio Grande do Sul, Porto Alegre
Amorim RG, Leal SC, Frencken JE (2012) Survival of atraumatic restorative treatment (ART) sealants and restorations: a meta-analysis. Clin Oral Invest 16:429–441. https://doi.org/10.1007/s00784-011-0513-3
Faccin ES, Ferreira SH, Kramer PF, Ardenghi TM, Feldens CA (2009) Clinical performance of ART restorations in primary teeth: a survival analysis. J Clin Pediatr Dent 33:295–298
Mallow PK, Durward CS, Klaipo M (1998) Restoration of permanent teeth in young rural children in Cambodia using the atraumatic restorative treatment (ART) technique and Fuji II glass ionomer cement. Int Paediatr Dent 8:35–40
Smales RJ, Yip HK (2000) The atraumatic restorative treatment (ART) approach for primary: review of literature. Pediatr Dent 22:294–298
Yip HK, Smales RJ (2002) Glass ionomer cements used as fissure sealants with the atraumatic restorative treatment (ART) approach: review of literature. Int Dent J 52:67–70
Rahimtoola S, van Amerongen E (2002) Comparison of two tooth-saving preparation techniques for one-surface cavities. ASDC J Dent Child 69:16–26
Acknowledgements
Mircelei Saldanha Sampaio and Cinthya Aline das Dores Guarienti are acknowledged for the help in the children’s care and the conduction of the clinical trial.
Funding
The study was supported by Federal University of Rio Grande do Sul (UFRGS) School of Dentistry, Rio Grande do Sul, Porto Alegre, Brazil.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in the study involving human participants were in accordance with the ethical standards of the institution and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Faustino-Silva, D.D., Figueiredo, M.C. Atraumatic restorative treatment—ART in early childhood caries in babies: 4 years of randomized clinical trial. Clin Oral Invest 23, 3721–3729 (2019). https://doi.org/10.1007/s00784-019-02800-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-019-02800-8