Abstract
Objectives
Actually, there is no detailed guidance on how to deal with wound closure after surgical removal of medication-related osteonecrosis of the jaw (MRONJ) lesions. This study attempts to compare the difference in outcome between the mucosal and the mucoperiosteal flap closure after surgery.
Patients and methods
In this retrospective monocentric cohort study, patients (n = 61; 35 female/26 male) suffering from MRONJ and requiring surgical therapy at the University of Aachen between 2013 and 2015 were included. Due to intra-institutional variances, one group was treated with the mucosal, the other group with the mucoperiosteal technique. The success rate, i.e., mucosal closure and no relapse at the point of follow-up, was evaluated and compared. All patients were clinically investigated for the postoperative follow-up during a special consultation appointment.
Results
The success rates between the different techniques after 2 years follow-up were very similar. In the group of mucosal wound closure, 22 of 29 (75.86%) patients revealed mucosal integrity without signs of MRONJ. The rate in the mucoperiosteal wound closure group was almost identical (24 of 32 (75%)).
Conclusion
No differences in the success rates between the two different techniques could be evaluated.
Clinical relevance
The results of this study suggest that the complete removal of the necrotic bone might have a higher impact on the success rates than the technique of the wound closure. Due to the fact that the mucoperiosteal wound closure technique offers a better overview of the extent of the MRONJ lesion, the authors advise to use this technique.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Medication- related osteonecrosis of the jaw (MRONJ) is an undesired side effect of the therapy with antiresorptive agents used in patients suffering from malignant diseases or metabolic bone diseases [1, 2]. Bisphosphonates inhibit the activity of osteoclasts and therefore they are responsible for the suppression of bone turnover. The exact pathomechanism leading to the onset of MRONJ still needs to be elucidated [3, 4]. Denosumab is an antibody against RANK-ligand and so also results in reduced bone turnover because of the inhibition of osteoclastic activity. Likewise, denosumab causes osteonecrosis of the jaws. This encourages the assumption that suppression of osteoclastic activity plays a central role in pathogenesis of necrosis caused by the intake of bisphosphonates and denosumab [5, 6] in particular in areas of chronic infections. With the appearance of MRONJ, conservative treatment and palliative approaches of bisphosphonate-related osteonecrosis of the jaw (BRONJ) symptoms, such as infection signs and pain, were the first-choice therapy in handling this new clinical picture [7,8,9]. Although there were many debates regarding the surgical management of MRONJ, numerous scientists have reported high cure rates, which ranged from 59% [8, 10] to more than 90% [10,11,12,13,14] in terms of surgical treatments of MRONJ. The outcomes of surgical management were affected by many factors like the timing of intervention, the technique used, and the extension of resection—for example, local debridement with epiperiosteal wound closure or the resective more aggressive debridement with mucoperiosteal wound closure. In the actual German S3 Guideline of the DGZMK, the central aim of the guideline (04/2012) is to remove the necrosis in an atraumatic approach but completely. For surgical wound closure, a safe, well-vascularized primary wound closure is cautiously recommended by the DGZMK [15]. Despite a plurality of studies with different interpretations of the given guidelines, until now there is no evidence-based consensus on the preferred treatment modality even in wound closure technique after necrosis removal [11, 16,17,18]. To our best knowledge, there is no data that has evaluated this shortcoming. Obviously, the adequate handling of MRONJ is still a controversial and insufficiently investigated topic. Therefore, the purpose of this study was to investigate the success rate of the mucoperiosteal (subperiosteal) wound closure technique and compare this technique to the mucosal wound closure technique (epiperiosteal) after removal of MRONJ lesions in antiresorptive-related osteonecrosis of the jaw patients. Given that the subperiosteal technique provides a better overview of the surgical field thus enabling the surgeon to remove all necrotic bone securely, the investigators hypothesize that the mucoperiosteal (subperiosteal) technique outmatches the mucosal wound closure technique (epiperiosteal technique). We also prefer a more aggressive treatment of MRONJ like Graziani [19] and Carlson [11] because we are convinced that regardless of the stage of the necrotic bone disease, the affected area should be completely removed in order to enable an accurate healing [20, 21]. The specific aims of the study were (i) to assess postoperative mucosal integrity, (ii) no flush, (iii) no swelling, (iv) no subjective pain, and (v) no loss of sensitivity.
Patients and methods
We conducted a retrospective review of all log books and a health plan database to identify all patients who received bone surgery at the Department of Oral and Maxillofacial Surgery of the RWTH University of Aachen with the diagnosis of MRONJ due to antiresorptive intake and a metastatic malignancy or osteoporosis in the patient history between 2013 and 2015. We included bisphosphonate and denosumab patients, because point of connection is that the appearance of necrosis rises proportional to the quantity/period of drug intake. From this follows that for both drug intakes, it is important to eliminate the necrosis as soon as possible. Detailed case history and medication were recorded for all patients included (see Table 1 annexed). After screening all surgery reports, patients were divided into two groups: due to surgeon-dependent intra-institutional variations, one patient group had been treated with the mucosal (epiperiosteal) and the other group with the mucoperiosteal (subperiosteal) wound closure technique after the removal of the necrotic bone. The allocation to the wound closure technique was performed with conditions which were determined by factors beyond any control of the investigator. This procedure is comparable to a random assignment. As a result, all disturbing factors with regard to the allocation to a special operation method like gender, age, duration of medication intake, or localization of necrosis were eliminated. The number of and the interval between the patients’ visits varied. However, a data set with information about actual health status was created by screening all log books for follow-up checks of each patient over a period of maximum 2 years unless the patient fell into relapse. The evaluation of patients, who were deceased in the follow-up period, was based on their last visit. As specified by our institutional standard protocol, all patients were evaluated at least once a month over a 2-year period during our specialized consultation appointment. Due to the retrospective nature of this study, it was granted a written exemption from the IRB of the University of Aachen.
Surgery
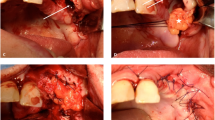
All operation procedures were performed by board-certified and specialized oral and maxillofacial surgeons in general anesthesia using a nasal intubation. Surgery was performed in sterile condition following a standardized operation protocol. As this study was carried out over a period of several years, there were changes in the operating staff within the team. Long-standing surgeons performed the epiperiosteal technique, while surgeons recruited later performed the subperiosteal method. The choice of the surgical technique for the patients was random. In the mucoperiosteal group (full-thickness flap, Fig. 1a), the first incision was extended to the alveolar bone. Afterwards, the operative surgeon carefully removed the periosteum including the flap from the bone with the help of a raspatory and detached it to expose the alveolar process [22]. The mucosal flap (split-thickness flap, Fig. 1b) is solely formed in fascia. The periosteum remains unaffected and therefore totally intact. Contrary to the full-thickness flap, the first incision remains supraperiosteal. The alveolar mucosa is divided from the periosteum without touching the alveolar bone. The periosteum remains unchanged so the alveolar process is not visible here. After flap preparation pictured in Fig. 1a, b, the affected bone was removed with a bur and was performed until all necrotic bone was removed and a sufficient bleeding of the bone was regained. Thorough smoothening of all sharp bone edges was performed with a rotating bur. After diligent lavage of the wound with an iodine solution, wound closure was carried out with vicryl sutures. The removal of external sutures was not performed earlier than 10 days after surgical management.
Measurements
In keeping with the institutional standard, all patients were evaluated and supervised during the clinic’s special consultation appointment. The follow-up we selected for the special consultation appointment was at least once a month over a period of 2 years. Except for the standardized check-up every 4 weeks, the aim was to evaluate the success rate of the operation in the long run. Therefore, the postoperative recall examination was continued for a period of maximum 2 years. Treatment was considered successful if mucosal integrity and no signs of necrosis were present. Therefore, as the primary outcome, we defined the full mucosal closure after surgical intervention with no indication for the secondary outcome, which was defined with infection signs like (i) flush, (ii) swelling of mucosa in the affected area, (iii) subjective pain, and (iv) loss of sensitivity.
Statistical analysis
We applied the chi-square test to our data set. The chi-square test is a standardized screening process to compare frequency of attributes and is developed to examine group deviations when the analyzed attribute is metered at a nominal level. Differences were defined as significant if the p value was less than 0.05. If the value p > 0.05, there is no significant association between the two attributes compared.
Results
Baseline characteristics
A total of 61 patients (mean age and standard deviation, 70.08 ± 11.81 years), 35 female (mean age, 68.86; standard deviation, ± 12.75; range, 162.56) and 26 male (mean age, 71.73; standard deviation, ± 10.42; range: 108.52), were included retrospectively in the present study. All patients have received antiresorptive therapy (details of antiresorptive agents are listed in Table 2), because of either malignant disease with bone metastasis (mamma carcinoma, n = 18; prostate carcinoma, n = 11; plasmocytome, n = 13) or other diseases (osteoporosis, n = 15; other diseases, n = 4). The period patients had taken their bisphosphonate ranged from 3 months to 12.25 years. The localization of lesions in order of decreasing appearance was listed as follows: 39 patients presented with mandibular disease, 13 patients with maxillary disease, and 8 involving both jaws. Forty-one of the patients had received chemotherapy in their medical records and 18 were smokers. We identified 29 patients that were operated with the mucoperiosteal technique (subperiosteal) and 32 patients with the mucosal technique (epiperiosteal). Mucosal healing with no signs of wound dehiscence was observed in 24 cases of patient base, which was treated with the full-thickness flap. In comparison, there were 22 positive treatment outcomes in the case of patients, who underwent the mucosal technique. The recidivism rate with 7 affected patients in the case of mucoperiosteal preparation and 8 affected patients in the case of the mucosal technique is almost equal (see Table 3). This is also illustrated in the statistical analysis, which implies that there is almost no significance regarding the success quotient of both operation methods.
The chi-square test shows that there was no statistically significant difference in mucosal integrity between the type of epiperiosteal and subperiosteal preparation technique χ2(1) = 0.006. The p value was > 0.05.
Discussion
The purpose of this retrospective study was to investigate the success rates of two different surgical wound closure techniques (mucoperiosteal versus epiperiosteal) after surgical removal of MRONJ lesions, and could we support our thesis that the more invasive subperiosteal preparation technique results in better treatment outcome? First reports and latter studies described that surgical management of BRONJ could not lead to complete healing [23,24,25]. These reports are responsible for the assumption that patients concerned should obtain palliative conservative therapies instead of more aggressive intervention. Consistent with this supposition, in 2009 the AAOMS position paper provided the recommendation to exercise surgical intervention not before stage III of BRONJ [20]. By contrast, several studies published have reported successful disease-free surgical treatment outcomes [17, 18, 26,27,28]. Given that the subperiosteal technique provides a better overview of the surgical field thus enabling the surgeon to securely remove all necrotic bone, the investigators hypothesize that the mucoperiosteal technique outmatches the mucosal wound closure technique. However, both surgical techniques revealed no statistically significant differences in mucosal integrity for all evaluated measurement points (p > 0.05). These results might be due to the fact that based on the odds ratio, the success rate of the epiperiosteal wound closure technique is insignificantly different from the success rate of the patients who were treated with the subperiosteal technique. Treatment success declared as full mucosal closure with absence of exposed bone was defined as the primary endpoint. Two years after the operation, 75.86% of the mucoperiosteal group and 75% of the mucosal group presented complete mucosal coverage. Although all secondary study parameters (flush, swelling, subjective pain, loss of sensitivity) showed no significant difference between the two techniques, there were 8 patients for the mucosal surgery technique and 7 patients for the mucoperiosteal group. These secondary parameters were investigated every 4 weeks after surgery during the special consultation appointment. Indeed, surgical management has a rising importance and with regard to the existing data, it is proven that the treatment of MRONJ in a surgical manner generates higher cure rates than conservative handling [29] but predictable courses of disease are not known at present. In addition, Pautke underlines the importance of complete removal of infected bone for a successful therapy [30]. This fact seems to be more important as the choice of wound closure technique. Also, Ristow reinforced that surgical treatment protocols can show success rates of over 90% [12]. Equally, Rupel reported that “outcome results for every BRONJ stage were low when patients were treated with nonsurgical therapies, higher when treated with conservative surgery and the highest when treated with extensive surgery or laser-assisted surgery” [31]. Furthermore, Kim reported that those who had received curettage showed the worst outcome results and the highest quote of reoperation [32]. In a systematic review, Fliefel et al. reported that a more successful treatment outcome was achieved in those patients who had received a more invasive surgery than those who had undergone minimally invasive surgery [33]. Equally, Comas-Colange presented in his article successful surgical treatment outcomes with success rates ranging from 58 to 100% [34]. In the present retrospective study, it is demonstrated that unique, more invasive surgical treatment in terms of preparing a full-thickness flap might be particularly more promising than using the minimal invasive option in terms of a split-thickness flap. The positive results of the follow-up confirm the assumption that there is no reason to favor the epiperiosteal treatment instead of directly using the subperiosteal operating technique. Rather, Mücke et al. 2010 supported the assertion by declaring that the quantity of failed operative interventions is a prognostic factor in handling MRONJ [35]. It also refers to the fact that a relapse encourages the appearance of complications [36]. The mucoperiosteal technique that is described in the present study shows a high success rate. Twenty-two of 29 patients (75.86%) showed a complete wound closure after using this operation technique. On the other hand, 24 of 32 patients (75%) who had undergone the other surgical treatment method were listed as having treatment success. Finally, the question arises whether there is a gold standard of the operation technique in handling MRONJ. The results point out that surgical treatment is promising regardless of which of the described surgical technique was used. That is why there is no valid reason to prefer one of the two; it is however beyond all questions that the mucoperiosteal technique offers a better overview of the operating field than the mucosal one and our first results give an initial foresight of the successful treatment of MRONJ in a more invasive way. Even Graziani [19], Carlson and Basile [11], and Kim [32] confirm our statement to prefer more aggressive surgery. Moreover, they report that the BRONJ should be eliminated to guarantee complete healing, regardless of the stage of the affected necrotic areas that are continual sources of soft tissue irritation [21, 37]. Regarding this discussion, it is evident that more long-term studies are needed to consolidate these first positive results in invasive MRONJ surgery. The reason for the modest recommendation on radical surgery is probably attributed to the fact that the MRONJ was originally described as avascular necrosis [23]. A reduced vascularization was supposed to be a possible crucial factor in the pathomechanism of MRONJ comparable to the entity of osteoradionecrosis (ORN) which is characterized as hypoxic-hypovascular-hypocellular tissue [38]. The clinical consequence to leave the periosteum—an important source of blood supply in ORN [39]—undisturbed resulted in unfavorable success rates. Equally, Pautke attaches great importance to the complete removal of necrotic bone in the affected area, no matter how small. Furthermore, Pautke points to the fact that necrotic and therefore avital bone will not be revitalized. In addition, residuals of affected bone can lead to a relapse of MRONJ [30]. Recent study results show that in the treatment of MRONJ, the complete removal of the necrotic tissue might have a higher impact on the success rates of the technique of mucosal closure of the wound. In this respect, the intraoperative guidance by bone fluorescence has revealed great advantages [40,41,42]. Given that the overview over a MRONJ lesion might be superior using the subperiosteal technique in comparison to the epiperiosteal approach, the authors of this study recommend to use the subperiosteal approach and mucoperiosteal flaps to cover the wounds in the treatment of MRONJ.
Limitation section
This study might have some limitations, including the following aspects. Due to the retrospective study design and the heterogeneity of intervention, evidence is low; thus, data needs to be carefully interpreted. There is no doubt that in a retrospective study the quality of the data set could be incomplete. On the one hand, this could result from the incomplete documentation and on the other hand from the fact that the patients do not keep all relevant information in mind. However, we affirm that we exclude all incomplete case histories. Retrospective studies create hypothesis and it is beyond question that there is a need for prospective studies to confirm the results of such studies. However, we did our best to interpret the available data over a long period executed in a clinical setting without specifying information on the disease. Indeed, a study with a prospective experimental design and a larger case number is essential to provide a clearer understanding of MRONJ and its surgical management. Consistent with the explorative and preliminary character of this study and the consequent small case number, the exact analysis of allocation to a special AAOMS stage was not renounced. We just included all patients with the diagnosis MRONJ according to stage I to stage III. According to the study design, the different techniques of preparation (epiperiosteal vs. subperiosteal) were consequently performed in the two groups. Even in stage III lesions, epiperiosteal preparation was performed as far as possible. Another disturbing factor may be the small case number, but the common problem of retrospective studies is the small sample sizes and the heterogeneous treatment concepts of therapy. Often, it is not possible to comprehend the art of elected operation method because of deficient documentation. Since we performed a retrospective study, power calculation was not performed. Furthermore, in order to estimate an adequate and effective size for this explorative study, 61 patients were recruited with the diagnosis of MRONJ between 2013 and 2015 and a follow-up over 1 year. The aim of this explorative study was to show the advantage of the submucosal technique over the epiperiosteal technique. There is no doubt that a study with a prospective experimental design and a larger case number is essential to provide a clearer understanding of BRONJ and its surgical management.
References
Berenson JR, Lichtenstein A, Porter L, Dimopoulos MA, Bordoni R, George S, Lipton A, Keller A, Ballester O, Kovacs MJ, Blacklock HA, Bell R, Simeone J, Reitsma DJ, Heffernan M, Seaman J, Knight RD (1996) Efficacy of pamidronate in reducing skeletal events in patients with advanced multiple myeloma. Myeloma Aredia Study Group. N Engl J Med 334(8):488–493. https://doi.org/10.1056/nejm199602223340802
Black DM, Cummings SR, Karpf DB, Cauley JA, Thompson DE, Nevitt MC, Bauer DC, Genant HK, Haskell WL, Marcus R, Ott SM, Torner JC, Quandt SA, Reiss TF, Ensrud KE (1996) Randomised trial of effect of alendronate on risk of fracture in women with existing vertebral fractures. Fracture Intervention Trial Research Group. Lancet 348(9041):1535–1541
Park JB, Cho SH, Kim I, Lee W, Kang SH, Kim H (2017) Evaluation of the bisphosphonate effect on stem cells derived from jaw bone and long bone rabbit models: a pilot study. Arch Oral Biol 85:178–182. https://doi.org/10.1016/j.archoralbio.2017.10.024
Ristow O, Gerngross C, Schwaiger M, Hohlweg-Majert B, Kehl V, Jansen H, Hahnefeld L, Otto S, Pautke C (2014) Is bone turnover of jawbone and its possible over suppression by bisphosphonates of etiologic importance in pathogenesis of bisphosphonate-related osteonecrosis? J Oral Maxillof Surg Off J Am Assoc Oral Maxillof Surg 72(5):903–910. https://doi.org/10.1016/j.joms.2013.11.005
Yoshimura H, Ohba S, Yoshida H, Saito K, Inui K, Yasui R, Ichikawa D, Aiki M, Kobayashi J, Matsuda S, Imamura Y, Sano K (2017) Denosumab-related osteonecrosis of the jaw in a patient with bone metastases of prostate cancer: a case report and literature review. Oncol Lett 14(1):127–136. https://doi.org/10.3892/ol.2017.6121
Egloff-Juras C, Gallois A, Salleron J, Massard V, Dolivet G, Guillet J, Phulpin B (2017) Denosumab-related osteonecrosis of the jaw: a retrospective study. J Oral Pathol Med Off Publ Int Assoc Oral Pathol Am Acad Oral Pathol. https://doi.org/10.1111/jop.12646
American Association of Oral and Maxillofacial Surgeons position paper on bisphosphonate-related osteonecrosis of the jaws (2007). J Oral Maxillof Surg Off J Am Assoc Oral Maxillof Surg 65(3):369–376. https://doi.org/10.1016/j.joms.2006.11.003
Holzinger D, Seemann R, Klug C, Ewers R, Millesi G, Baumann A, Wutzl A (2013) Long-term success of surgery in bisphosphonate-related osteonecrosis of the jaws (BRONJs). Oral Oncol 49(1):66–70. https://doi.org/10.1016/j.oraloncology.2012.07.008
Otto S, Schreyer C, Hafner S, Mast G, Ehrenfeld M, Sturzenbaum S, Pautke C (2012) Bisphosphonate-related osteonecrosis of the jaws—characteristics, risk factors, clinical features, localization and impact on oncological treatment. J Cranio-maxillo-facial Surg Off Publ Eur Assoc Cranio-Maxillo-Facial Surg 40(4):303–309. https://doi.org/10.1016/j.jcms.2011.05.003
Wutzl A, Pohl S, Sulzbacher I, Seemann R, Lauer G, Ewers R, Drach J, Klug C (2012) Factors influencing surgical treatment of bisphosphonate-related osteonecrosis of the jaws. Head Neck 34(2):194–200. https://doi.org/10.1002/hed.21708
Carlson ER, Basile JD (2009) The role of surgical resection in the management of bisphosphonate-related osteonecrosis of the jaws. J Oral Maxillof Surg Off J Am Assoc Oral Maxillofac Surg 67(5 Suppl):85–95. https://doi.org/10.1016/j.joms.2009.01.006
Ristow O, Otto S, Troeltzsch M, Hohlweg-Majert B, Pautke C (2015) Treatment perspectives for medication-related osteonecrosis of the jaw (MRONJ). J Cranio-maxillo-facial Surg Off Publ Eur Assoc Cranio-Maxillo-Facial Surg 43(2):290–293. https://doi.org/10.1016/j.jcms.2014.11.014
Lopes RN, Rabelo GD, Rocha AC, Carvalho PA, Alves FA (2015) Surgical therapy for bisphosphonate-related osteonecrosis of the jaw: six-year experience of a single institution. J Oral Maxillof Surg Off J Am Assoc Oral Maxillof Surg 73(7):1288–1295. https://doi.org/10.1016/j.joms.2015.01.008
Bedogni A, Saia G, Bettini G, Tronchet A, Totola A, Bedogni G, Ferronato G, Nocini PF, Blandamura S (2011) Long-term outcomes of surgical resection of the jaws in cancer patients with bisphosphonate-related osteonecrosis. Oral Oncol 47(5):420–424. https://doi.org/10.1016/j.oraloncology.2011.02.024
K.A.Grötz J-UP Al Nawas (2012) Bisphosphonat-assoziierte Kiefernekrose (BP-ONJ) und andere Medikamenten-assoziierte Kiefernekrosen.18
AAOMS (2007) American Association of Oral and Maxillofacial Surgeons position paper on bisphosphonate-related osteonecrosis of the jaws. J Oral Maxillofac Surg 65(3):369–376. https://doi.org/10.1016/j.joms.2006.11.003
Stockmann P, Vairaktaris E, Wehrhan F, Seiss M, Schwarz S, Spriewald B, Neukam FW, Nkenke E (2010) Osteotomy and primary wound closure in bisphosphonate-associated osteonecrosis of the jaw: a prospective clinical study with 12 months follow-up. Supp Care Cancer Off J Multinatl Assoc Supp Care Cancer 18(4):449–460. https://doi.org/10.1007/s00520-009-0688-1
Wilde F, Heufelder M, Winter K, Hendricks J, Frerich B, Schramm A, Hemprich A (2011) The role of surgical therapy in the management of intravenous bisphosphonates-related osteonecrosis of the jaw. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 111(2):153–163. https://doi.org/10.1016/j.tripleo.2010.04.015
Graziani F, Vescovi P, Campisi G, Favia G, Gabriele M, Gaeta GM, Gennai S, Goia F, Miccoli M, Peluso F, Scoletta M, Solazzo L, Colella G (2012) Resective surgical approach shows a high performance in the management of advanced cases of bisphosphonate-related osteonecrosis of the jaws: a retrospective survey of 347 cases. J Oral Maxillof Surg Off J Am Assoc Oral Maxillof Surg 70(11):2501–2507. https://doi.org/10.1016/j.joms.2012.05.019
Ruggiero SL, Dodson TB, Assael LA, Landesberg R, Marx RE, Mehrotra B (2009) American Association of Oral and Maxillofacial Surgeons position paper on bisphosphonate-related osteonecrosis of the jaw—2009 update. Aust Endod J, J Aust Soc Endod Inc 35(3):119–130. https://doi.org/10.1111/j.1747-4477.2009.00213.x
Ruggiero SL, Dodson TB, Fantasia J, Goodday R, Aghaloo T, Mehrotra B, O'Ryan F (2014) American Association of Oral and Maxillofacial Surgeons position paper on medication-related osteonecrosis of the jaw—2014 update. J Maxillof Surg Off J Am Assoc Oral Maxillof Surg 72(10):1938–1956. https://doi.org/10.1016/j.joms.2014.04.031
Joda TGP, Ehmke B (2008) Arbeitshandbuch Parodontologie Band 2 Chirurgische Therapie. Books on Demand GmbH, Norderstedt, pp 11–99
Marx RE, Sawatari Y, Fortin M, Broumand V (2005) Bisphosphonate-induced exposed bone (osteonecrosis/osteopetrosis) of the jaws: risk factors, recognition, prevention, and treatment. J Oral Maxillofac Surg Off J Am Assoc Oral Maxillofac Surg 63(11):1567–1575. https://doi.org/10.1016/j.joms.2005.07.010
Ruggiero SL, Mehrotra B, Rosenberg TJ, Engroff SL (2004) Osteonecrosis of the jaws associated with the use of bisphosphonates: a review of 63 cases. J Oral Maxillofac Surg Off J Am Assoc Oral Maxillofac Surg 62(5):527–534
Magopoulos C, Karakinaris G, Telioudis Z, Vahtsevanos K, Dimitrakopoulos I, Antoniadis K, Delaroudis S (2007) Osteonecrosis of the jaws due to bisphosphonate use. A review of 60 cases and treatment proposals. Am J Otolaryngol 28(3):158–163. https://doi.org/10.1016/j.amjoto.2006.08.004
Voss PJ, Joshi Oshero J, Kovalova-Muller A, Veigel Merino EA, Sauerbier S, Al-Jamali J, Lemound J, Metzger MC, Schmelzeisen R (2012) Surgical treatment of bisphosphonate-associated osteonecrosis of the jaw: technical report and follow up of 21 patients. J Cranio-Maxillo-Facial Surg Off Publ Eur Assoc Cranio-Maxillo-Facial Surg 40(8):719–725. https://doi.org/10.1016/j.jcms.2012.01.005
Hoefert S, Eufinger H (2011) Relevance of a prolonged preoperative antibiotic regime in the treatment of bisphosphonate-related osteonecrosis of the jaw. J Oral Maxillofac Surg Off J Am Assoc Oral Maxillofac Surg 69(2):362–380. https://doi.org/10.1016/j.joms.2010.06.200
Schubert M, Klatte I, Linek W, Muller B, Doring K, Eckelt U, Hemprich A, Berger U, Hendricks J (2012) The saxon bisphosphonate register—therapy and prevention of bisphosphonate-related osteonecrosis of the jaws. Oral Oncol 48(4):349–354. https://doi.org/10.1016/j.oraloncology.2011.11.004
Hoff AO, Toth BB, Altundag K, Johnson MM, Warneke CL, Hu M, Nooka A, Sayegh G, Guarneri V, Desrouleaux K, Cui J, Adamus A, Gagel RF, Hortobagyi GN (2008) Frequency and risk factors associated with osteonecrosis of the jaw in cancer patients treated with intravenous bisphosphonates. J Bone Miner Res Off J Am Soc Bone Miner Res 23(6):826–836. https://doi.org/10.1359/jbmr.080205
Sven Otto M, DMD, FEBOMFS (2015) Medication-related osteonecrosis of the jaws Bisphosphonates, Denosumab and New Agents. Springer-Verlag Berlin, Heidelberg, pp 1–217
Rupel K, Ottaviani G, Gobbo M, Contardo L, Tirelli G, Vescovi P, Di Lenarda R, Biasotto M (2014) A systematic review of therapeutical approaches in bisphosphonates-related osteonecrosis of the jaw (BRONJ). Oral Oncol 50(11):1049–1057. https://doi.org/10.1016/j.oraloncology.2014.08.016
yKim HY, Lee SJ, Kim SM, Myoung H, Hwang SJ, Choi JY, Lee JH, Choung PH, Kim MJ, Seo BM (2017) Extensive surgical procedures result in better treatment outcomes for bisphosphonate-related osteonecrosis of the jaw in patients with osteoporosis. J Oral Maxillofac Surg Off J Am Assoc Oral Maxillofac Surg 75(7):1404–1413. https://doi.org/10.1016/j.joms.2016.12.014
Fliefel R, Troltzsch M, Kuhnisch J, Ehrenfeld M, Otto S (2015) Treatment strategies and outcomes of bisphosphonate-related osteonecrosis of the jaw (BRONJ) with characterization of patients: a systematic review. Int J Oral Maxillofac Surg 44(5):568–585. https://doi.org/10.1016/j.ijom.2015.01.026
Comas-Calonge A, Figueiredo R, Gay-Escoda C (2017) Surgical treatment vs. conservative treatment in intravenous bisphosphonate-related osteonecrosis of the jaws. Systematic review. J Clin Exp Dent 9(2):e302–e307. https://doi.org/10.4317/jced.53504
Mucke T, Koschinski J, Deppe H, Wagenpfeil S, Pautke C, Mitchell DA, Wolff KD, Holzle F (2011) Outcome of treatment and parameters influencing recurrence in patients with bisphosphonate-related osteonecrosis of the jaws. J Cancer Res Clin Oncol 137(5):907–913. https://doi.org/10.1007/s00432-010-0953-1
Wutzl A, Eisenmenger G, Hoffmann M, Czerny C, Moser D, Pietschmann P, Ewers R, Baumann A (2006) Osteonecrosis of the jaws and bisphosphonate treatment in cancer patients. Wien Klin Wochenschr 118(15–16):473–478. https://doi.org/10.1007/s00508-006-0644-8
Ruggiero SL, Dodson TB, Assael LA, Landesberg R, Marx RE, Mehrotra B (2009) American Association of Oral and Maxillofacial Surgeons position paper on bisphosphonate-related osteonecrosis of the jaws—2009 update. J Oral Maxillofac Surg Off J Am Assoc Oral Maxillofac Surg 67(5 Suppl):2–12. https://doi.org/10.1016/j.joms.2009.01.009
Marx RE (1983) Osteoradionecrosis: a new concept of its pathophysiology. J Oral Maxillofac Surg Off I Am Assoc Oral Maxillofac Surg 41(5):283–288
Pautke C, Tischer T, Neff A, Horch HH, Kolk A (2006) In vivo tetracycline labeling of bone: an intraoperative aid in the surgical therapy of osteoradionecrosis of the mandible. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 102(6):e10–e13. https://doi.org/10.1016/j.tripleo.2006.05.007
Ristow O, Otto S, Geiss C, Kehl V, Berger M, Troeltzsch M, Koerdt S, Hohlweg-Majert B, Freudlsperger C, Pautke C (2017) Comparison of auto-fluorescence and tetracycline fluorescence for guided bone surgery of medication-related osteonecrosis of the jaw: a randomized controlled feasibility study. Int J Oral Maxillofac Surg 46(2):157–166. https://doi.org/10.1016/j.ijom.2016.10.008
Pautke C, Bauer F, Otto S, Tischer T, Steiner T, Weitz J, Kreutzer K, Hohlweg-Majert B, Wolff KD, Hafner S, Mast G, Ehrenfeld M, Sturzenbaum SR, Kolk A (2011) Fluorescence-guided bone resection in bisphosphonate-related osteonecrosis of the jaws: first clinical results of a prospective pilot study. J Oral Maxillofac Surg Off J Am Assoc Oral Maxillofac Surg 69(1):84–91. https://doi.org/10.1016/j.joms.2010.07.014
Otto S, Ristow O, Pache C, Troeltzsch M, Fliefel R, Ehrenfeld M, Pautke C (2016) Fluorescence-guided surgery for the treatment of medication-related osteonecrosis of the jaw: a prospective cohort study. J Cranio-Maxillo-Facial Surg Off Publ Eur Assoc Cranio-Maxillo-Facial Surg 44:1073–1080. https://doi.org/10.1016/j.jcms.2016.05.018
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The study does not include any personal information of patients.
Informed consent
For this type of study formal consent is not required.
Rights and permissions
About this article
Cite this article
Nonnenmühlen, N., Burnic, A., Bartella, A. et al. Comparison of mucosal and mucoperiosteal wound cover for the treatment of medication-related osteonecrosis of the jaw lesions: a retrospective cohort study. Clin Oral Invest 23, 351–359 (2019). https://doi.org/10.1007/s00784-018-2443-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-018-2443-9