Abstract
Objectives
The aim of this in vitro study was an analysis of the impact of simulated reduced alveolar bone support and post-restored, endodontically treated distal abutment tooth on load capability of all-ceramic zirconia-based cantilever-fixed dental prosthesis (CFDP).
Material and methods
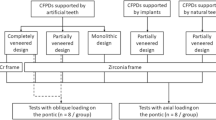
The roots of human lower sound premolars (n = 80) were divided into five experimental groups to be restored with all-ceramic zirconia-supported three-unit CFDP regarding bone loss (BL) relative to the cement-enamel junction (CEJ): 2 mm below CEJ = 0% BL (control group), group 25% distal BL, group 50% distal BL, group 50% mesial and distal BL, and group 50% distal BL and adhesive post-supported restoration. Specimens were exposed to simulated clinical function by thermo-mechanical loading (6.000 cycles 5°–55°; 1.2 × 106 cycles 0–50 N) and subsequent linear loading until failure.
Results
Tooth mobility increased significantly for groups with simulated bone loss (p < 0.001). Four specimens failed during thermal cycling and mechanical loading (TCML). The maximum load capability ranged from 350 to 569 N, and did not differ significantly between experimental groups (p = 0.095). Groups with simulated bone loss revealed more tooth fractures at distal abutment teeth, whereas technical failures were more frequent in the control group (p = 0.024).
Conclusions
Differences of alveolar bone support and respectively increased tooth mobility between mesial and distal abutments did not influence load capability. A distal adhesively post-and-core-supported, root-treated abutment tooth did not increase risk of three-unit CFDP failure.
Clinical relevance
CFDPs are a treatment option used with caution when reduced alveolar bone support, increased tooth mobility, and distal post-supported, root-treated abutment teeth are involved.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cantilever-fixed dental prostheses (CFDPs) have been defined as retainers holding one or more unsupported free-end extensions [1]. CFDPs are described as a treatment option for medically compromised patients, when jeopardizing anatomical structures are present, in order to reduce treatment costs or when implant placement is not possible. In terms of patient satisfaction, they are regarded as more favorable tooth replacement alternative compared to removable partial dentures [2].
Clinically, a meta-analysis on CFDPs estimated a survival rate of about 82%, and a 10-year success rate, i.e., free of all complications over the entire observation period, of 63%. About 3% of vital and non-vital abutment teeth fractured over the 10-year observation period, despite the fact that unfavorable extra non-axial loading occurred.
Several clinical needs were described: abutments teeth chosen for CFDPs should have sound periodontal bone support, satisfactory root morphology, and a favorable arch-to-arch relationship [3]. The use of Antes’s law was proposed, i.e., root surface of abutment teeth should exceed root surface of the substituted tooth [3]. However, a classical clinical study by Nyman et al. demonstrated that Ante’s law is not a prerequisite for long-term clinical success [4, 5].
For CFDP-abutment teeth without alveolar bone loss and CFDP with a distal abutment with a moderate bone loss, occlusal forces were distributed only to the three teeth closest to the loaded cantilever [6]. High stress concentrations were found around the connector and the tooth closest to the cantilever unit. When bone support is decreased, the deflection and stress concentrations were increased [7]. Hence, alveolar bone loss may go along with increased failure risks in particular when severely damaged abutment teeth were used. Data on the impact of periodontal disease on the survival of CFDPs on endodontically treated teeth (ETT) as abutments is limited. Increased periodontal pocket depths were described as a significant factor in the survival of restored ETT [8]. Slightly more attachment loss in ETT than in contra lateral untreated controls was shown [9]. In contrast, existence of appropriate root canal fillings in periodontitis patients has no effect on the extent of proximal attachment [10].
According to in vitro data, all-ceramic CFDPs cannot be recommended for clinical replacement of a missing molar, when a zirconia framework [11] or lithium disilicate [12] is used. In vivo 4-year clinical results showed no differences in complication rates when zirconia FDPs with end-standing abutments and zirconia CFDPs were compared [13]. In addition, a 3-year clinical study demonstrated an acceptable performance for veneered zirconia CFDPs when compared to metal-ceramic FDPs [14]. However, neither in vitro nor clinical evidence for the survival of CFDPs in situations with reduced alveolar bone support and/or endodontically treated abutment teeth is currently not available.
Thus, this in vitro pilot study aimed to investigate the impact of simulated reduced alveolar bone support and post-restored, endodontically treated distal abutment tooth on failure modes and load capability of three-unit veneered zirconia CFDPs. The CFDP substituted the first molar in the dimension of a premolar. They were exposed to preclinical functional and subsequent linear loading.
The null hypothesis were as follows:
-
1.
Simulated alveolar bone loss has no impact on functional and linear loading capability of CFPD and
-
2.
Simulated root canal treatment plus post-and-core restoration of the distal abutment tooth has no impact on functional and linear loading capability of CFPD.
Material and methods
The study protocol conformed to the principles outlined in the German Ethics Committee’s statement for the use of human body material in medical research (Central German Ethics Committee 2003). Human lower sound premolars were selected from a tooth bank and stored in 0.5% chloramine solution after extraction. The specimens were equally distributed to five groups (16 specimen teeth per group) according to their cross-sectional dimension at the level of cement-enamel junction (CEJ) (Fig. 1).
Assessment of tooth mobility
Tooth mobility was simulated for static and dynamic load tests using a validated in vitro system [15]. It was measured three times for each specimen by means of a Periotest device perpendicular to tooth axis (PERIOTEST Classic, Medizintechnik Gulden, Modautal, Germany). One out of at least two equal Periotest values was taken for further analysis.
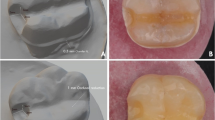
To simulate tooth mobility, the roots were coated with a thin layer of autopolymerizing acrylic resin (Paladur; Heraeus Kulzer). After polymerization, the adhesive was applied on the resin-coated roots. A-polysiloxane soft cushion material (Mollosil; DETAX, Ettlingen, Germany) was placed into the simulated socket, and specimens were relocated with the aid of the positioning unit into the mold. Prior to tooth preparation, silicon impressions (Provil novo, Heraeus Kulzer) were taken and the specimens were digitized using a model scanner (inEOS; Sirona, Bensheim, Germany) from each specimen.
Specimen pre-treatment and embedding procedure
The specimens that received post-and-core restorations were endodontically treated by gradual reaming to ISO size 40 (ProTaper, Dentsply DeTrey, Konstanz, Germany) and intermittent rinsing with 2.5% sodium hypochlorite. The root canals were obturated with gutta-percha (Roeko, Langenau, Germany) and sealer (AH 26, Dentsply DeTrey). The access cavity was adhesively filled with a flowable composite (CeramX flow, Dentsply DeTrey).
For each specimen, two premolars were embedded perpendicular to tooth axis ensuring a tight proximal contact and parallel directions of roots. To provide the center of the cantilevered pontic, 3.5 mm distal from the second abutment tooth, the embedding procedure was realized with a guided appliance.
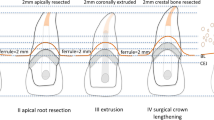
In a first step, roots were coated with a thin layer of wax (0.3-mm casting wax veined green, Dentaurum, Pforzheim, Germany). To simulate biological width, a circumferential wax wire was adapted below the CEJ in control group (wax wire round, Ø 2 mm; Dentaurum). Bone loss was simulated by adapting the wax wire several times: 4 mm apical from the CEJ simulating 25% bone loss and 6 mm were blocked out for 50% bone loss.
In a second step, teeth were retained in a guided manner according to the tooth axis using an individualized unit and mounted in an acrylic resin block (Technovit 4004, Heraeus Kulzer, Hanau, Germany) (Fig. 2). After polymerization, roots were removed and cleaned.
Specimen preparation, in particular efforts regarding imitation of periodontal ligament: (I) natural human premolars, (II) covered with wax for periodontal ligament simulation and wax wire simulating bone loss, (III) setting for specimen embedding perpendicular to tooth axis, step shown here: wax cover for periodontal ligament simulation, (IV) embedded specimens to cover root surface with artificial periodontal ligament (silicon, Mollosil), (VI) finally covered root surface after removal; periodontal ligament simulated, (VI) embedded in a bone simulation material (Technovit 4000), and finally prepared specimens
Adhesive post-and-core restoration
After the embedding procedure, clinical crowns of the endodontically treated specimens were cut 2 mm above the CEJ to leave sufficient dentin height to ensure a 2-mm ferrule. Gutta-percha was removed (Gates-Glidden-burs) and the post space cavity was prepared with a tapered drill corresponding to the glass fiber-reinforced composite post FRC Postec Plus Size 1 (Ø post tip = 0.8 mm, conicity of 5°18′, Ivoclar-Vivadent, Schaan, Lichtenstein). The root canals were enlarged to achieve an intraradicular post length of 8 mm leaving at least 4-mm root canal filling apically. Prior to adhesive fiber post luting with a self-adhesive resin-cement (RelyX Unicem; 3 M ESPE, Seefeld, Germany), irrigation of the post cavity was performed using 5 ml of 1% NaOCl solution with passive ultrasonic irrigation for 1 min, followed by water rinsing of 5 ml for 1 min, and finally ethanol pre-treatment with 5 ml of a 99% solution for 1 min. Adhesive procedure was performed under room temperature. The luting composite was filled in the root canal with elongation tips by slowly pulling out the tip during cement application. Post was slowly inserted, and kept in place. Light curing was performed for 2 s (Optilux light curing unit, Demetron Research Corp., Danbury, USA), and excess material was removed. Final light curing was performed for 1 min. Core buildups were prepared with the aid of transparent strip crowns (Frasaco, Tettnang, Germany) using MultiCore Flow with the corresponding adhesive Multilink primers A and B (Ivoclar-Vivadent). The adhesive (primers A and B) was mixed for 30 s und applied for 30 s on dentin. After air drying for 30 s, the strip crown was filled with MultiCore, adapted on the tooth, and finally light cured for 40 s. Specimens were stored for 24 h in 37 °C in water.
Three-unit zirconia cantilever FDP
All teeth were prepared using Guide-pin-Diamonds (tapered chamfer, round, size 021, grit size coarse 151 μm and fine 46 μm, Komet Dental, Gebr. Brasseler, Lemgo, Germany) fixed in a surveyor with a chamfer design (circumferential depth of 1 mm, occlusal reduction of 1.5 mm) to meet all-ceramic requirements. The finishing line was prepared following the CEJ. Specimens were scanned within EOS and all CFDP frameworks and were CAD-CAM generated (inLab 3D V3.10, Sirona) from zirconia (IPS e.max ZirCAD, Ivoclar-Vivadent). With the aid of the software tool Bio-Referenz, frameworks were fabricated according to cusp supporting, anatomical-shaped design to realize a target veneering thickness of max 1 mm. Connector diameter was defined with 9 mm2. After the milling (MCXL, Sirona) and sintering process, the frameworks were layered with a liner inherent to the system (IPS e.max Ceram ZirLiner), and fired at a temperature of 960 °C. The frameworks were fixed at prepared teeth (Xantopren L blue, Heraeus Kulzer). With the aid of the silicon molds taken from the unprepared teeth, the veneering wax-up was realized. The cantilever unit was standardized in the mesio-distal (7 mm) and in lingual/buccal (5 mm) dimension. The waxed surface was finished, and the specimens were invested in a muffle according to the manufactures’ instruction (IPS PressVEST Speed, Ivoclar-Vivadent). The frameworks were over-pressed by a fluor-apatite ceramic (IPS e.max ZirPress LT A2, Ivoclar-Vivadent). Finally, the CFDPs were glazed (IPS e.max Cerm Glaze paste, Ivoclar-Vivadent). After sandblasting of the core buildups and selective enamel etching, the primers Multilink A and B (Ivoclar-Vivadent) were applied for 30 s, and evaporated with oil-free air stream. The CFDPs were adhesively luted using Multilink automix (Ivoclar-Vivadent) seated and leaved undisturbed for chemical curing for 5 min.
Thermal cycling and mechanical loading and subsequent static loading
Thermal cycling and mechanical loading (TCML) was performed by computer-controlled chewing simulation with online failure control combined with simultaneous thermal cycling (manufacturer: type simulator II, EGO, Regensburg, Gernamy; 2 × 3000 thermal cycles, 5/55 °C, 2 min each cycle in distilled water; 1.2 × 106 mastication cycles with 50 N at 1.6 Hz) An oval-shaped steatite piston vertically loaded (1-mm lifting) the center of the cantilever unit only.
After TCML, surviving specimens were loaded at cantilever unit only until failure. (Zwick 1446, Zwick, Ulm, Germany; v = 1 mm/min, oval-shaped steel piston at cantilever unit only, 0.3-mm-thin tin foil to reduce excessive stress forces by peak loading, failure detection 10% loss of maximum force).
Statistical analysis
Group differences regarding the tooth mobility comparing the Periotest values were analyzed using one-way ANOVA. The crown-root ratio was calculated by effective crown length divided to effective root length. Effective crown length was defined from the level of simulated bone (embedment level) to the occlusal plane. The distance from the bone level to the apex was defined as effective root length. To level the impact of simulated alveolar bone loss on maximum load capability, Kruskal-Wallis and Mann-Whitney tests for group differences were calculated. Differences in the frequency of failure modes between experimental groups were evaluated by chi-square test. For each abutment tooth, the failure patterns were categorized into two major patterns: (1) technical failure as loss of retention of the FDP and (2) biological failure as fractures of the abutment tooth. The level of significance was α = 0.05.
Results
The descriptive data of the tooth characteristics showed similar means of root length and cross-sectional area at the CEJ level between the experimental groups (Table 1).
Tooth mobility
The measured tooth mobility was significantly (p = 0.001) different between the groups (Table 1). Abutment teeth with 50% bone loss revealed significantly (p < 0.001) higher tooth mobility compared to abutment teeth without simulated bone loss. Tooth mobility was significantly (p = 0.001) increased with higher simulated bone loss. Values for distal abutments with 50% bone loss were not significantly (p > 0.05) higher compared to those for distal abutment teeth with 25% simulated bone loss.
Crown-to-root ratio
The crown-root ratios differed significantly between the groups and abutment teeth, respectively, if bone loss was simulated (p < 0.001, for 25% bone loss compared to control p = 0.025). During TCML, four specimens failed and were not available for further load to fracture analysis. One root fracture of a distal abutment tooth occurred in group no. 1 (control group) and group 25% bone loss, respectively. Two specimens failed due to technical failures (one major chipping in group 50% and 25% distal bone loss). The maximum load capability did not differ significantly between the experimental groups (Kruskal-Wallis; p = 0.084) (Table 2 and Fig. 3).
Fracture modes
Fracture modes depended significantly on presence of simulated alveolar bone loss (chi-square; p = 0.006). The groups with simulated alveolar bone loss revealed more biological failures (e.g., abutment fracture). Mainly, technical failures (e.g., chipping of the veneering material) occurred in the control group (Table 2). Chipping of the veneering material of CFDPs alone without biological or loss of retention occurred each once in the control group and group 25% bone loss distal. The most common failure mode for the distal abutment teeth was tooth fracture if bone loss was present, while loss of retention of the FDP (technical failures) occurred more often in the control group (chi-square; p = 0.024). For the mesial abutment teeth, the number of technical failures increased for specimens with comparable abutment teeth mobility.
Discussion
The present in vitro study aimed to investigate the impact of (1) simulated alveolar bone loss and (2) presence of a post-endodontically restored distal abutment tooth on survival and maximum load capability of veneered zirconia framework CFDP to substitute the first molar after simulated clinical functional loading. We found no impact neither for alveolar bone loss nor presence of an endodontically and adhesively post-restored abutment tooth on restoration survival and maximum load capability. CFDPs with normal bone support tend to show more technical failures, and those with altered bone support experienced more biological failures as abutment fractures. Both null hypotheses were accepted.
Dynamic loading or the so-called artificial aging, which combines thermal cycling and mechanical loading (TCML) [16] provides a sufficient prognosis of probable clinical failure [17]. TCML includes fatigue phenomena and is of utmost importance to increase the predictive power of in vitro data with regard to clinical survival of restorations [18, 19]. Fatigue failures are defined as fractures of a material caused by cyclic or repeated sub-critical loads [20, 21]. The chewing simulation applied in this study aims to simulate the fatigue phenomenon, attempting to avoid false conclusions based on application of linear compressive loads only [22]. Findings based on simulated clinical function pre-tests may also help to exclude catastrophic clinical failure [18]. Physiologic tooth mobility was checked by Periotest control [15]. To test the experimental setting and to validate the specific test parameters, five metal-ceramic CFDPs were manufactured before and exposed to TCML and subsequent linear loading.
In the present study, forces were applied under adverse test conditions due to isolated loading on the distal aspect of cantilever extensions, which is clinically unlikely. In particular, when reduced bone support is present, bite forces are reduced compared to normal dentition [24]. Maximum load capability values after linear loading of 350 to 550 N are in agreement with other studies with normal bone support on vital teeth with zirconia framework [12] or lithium disilicate [13]. However, maximum bite force may in part significantly exceed bite force beyond 500 N. Thus, there is an increased likelihood of mechanical failure as fracture due to occlusal overload. Three-year clinical comparison of veneered zirconia CFDP and metal-ceramic FDP in a small group with 10 and 11 patients per group, respectively, was judged as acceptable [15]. Four-year clinical results comparing end abutments and cantilever designs of zirconia CFDPs with the Cercon system found no difference in complication rates [14]. In contrast, higher failure rates for CFDP compared to those for conventional end-abutment-supported FDPs were observed [23, 24].
A reason for the critical view on CFDP is the cantilever unit which creates a class I lever system, which dramatically alters the direction and magnitude of forces on the abutments [25]. Forces are transmitted through the cantilever pontics causing tilting and rotational movements of the abutments. The magnitude of rotational movements is increased as the crown-root ratio of abutments increases by simulated bone loss, and the length of the cantilever pontic increases [7]. In a three-dimensional finite element analysis on premolars, bone height was the predominant mechanical factor influencing the stress of the dentin on a post-restored root filled tooth, followed by the post diameter, post length, and ferrule height. Contribution of the bone height was more than 97%. Hence, for patients with severe bone destruction, a post might not be a good choice [26].
Wylie and Caputo [6] investigated using a photo-elastic model, CFDP-abutment teeth with healthy periodontal bone support and CFDP with a distal abutment with a moderate degree of mobility and bone loss. Occlusal forces were applied only to the teeth closest to the loaded cantilever [6]. Thus, higher loading stress on root dentine of abutment teeth with increased abutment tooth mobility will occur. This assumption is in agreement with the failure modes observed in our study, where significantly more distal abutment tooth fractured in groups with higher tooth mobility compared to that in the control group. Similarly, high stress concentrations were observed in a two-dimensional finite element analysis around the connector and the tooth closest to the cantilever unit. Reduced bone support increases the deflection and stress concentrations. Thus, only one cantilever unit supported by two abutment teeth is recommended [7]. In the present study, we chose two premolars as abutments for three-unit CFDP to substitute a first molar in the dimension of a premolar. No impact of alveolar bone loss regarding functional loading and maximum load capability was measured compared to normal bone support. However, abutments with any loss of simulated alveolar bone loss tend to show biological failure as fracture of the abutment supporting Wylie and Caputo’s findings [6].
It is generally accepted that ETTs as distal abutments for CFDP should be avoided [27]. A multilevel analysis revealed that in abutments in the combination of distal abutment with > 50% marginal bone loss and additional endodontic treatment, the probability of abutment tooth survival after up to 23 years was only 20% [28]. In 67% of the failed cantilever FDPs, the terminal abutments were ETTs [26]. Fractures and loss of retention occur more frequently when the distal abutments are endodontically treated [29, 30]. We set up this experimental group to test whether this is still true when adhesive core buildup protocol and zirconia framework-supported CFDP were chosen. To our own surprise, there was no difference between vital and endodontically treated abutment teeth with 50% bone loss. Even compared to vital normal bone-supported abutments, no differences in load capability could be revealed. However, abutments with bone loss tend to fracture more frequently compared to no-bone-loss group. This might be explained by applied oblique force producing a bending moment with the tooth structure above the periodontal bone as the moment arm. Substantial bone loss would enlarge this moment arm, hereby increasing the dentin peak stress at the fulcrum. This is consistent with in vitro load capability studies where ETT with simulated bone loss of 25% and 50% bone height had a markedly decreased load capability in a “dose”-dependent way [31,32,33]. In vivo CFDPs on abutment teeth with 25% or less bone loss after about 6 years of observation showed 36% failures. Abutment teeth were up to five times more frequently endodontically treated than teeth not serving as abutment [34]. Reinhardt et al. [35] reported with lower bone levels, stresses were increased considerably and concentrated in the small amount of dentin between the post and root periphery. They concluded that such an elevation in stress levels comes along with a significant increase in root fracture potential as described later clinically by Vire et al. [36]. Also, Nyman and Lindhe report that root fractures in post-restored periodontally compromised teeth are a significant problem. The risk of fracture is increased to periodontally comparable vital teeth [4]. Axelsson et al. reported root fractures as the main reason for failures (64%) in teeth exposed to endodontic treatment [37]. Reasons for extraction of ETT over a 1-year period were ca. 60% due to unrestorable tooth fracture and 32% due to periodontal problems, but only 6% due to endodontic failures [38]. However, treatment of ETT with severe coronal hard tissue loss has dramatically changed over the last 15 years. Current developments tend to adhesively restore ETT with fiber posts and direct composite core buildups to ensure the stabilization of the remaining tooth structure by creating mechanically homogenous units with favorable stress distribution within the root dentin, i.e., a so-called secondary monoblock [38]. The present results reveal no significant adverse influence of adhesively restored post-endodontic restorations on survival of CFDPs with altered alveolar bone support. We assume that the stress distribution in root dentin is comparable to vital abutment teeth when such tooth will be restored as secondary monoblock. These assumptions have to be clinically validated.
Conclusion
CFDP with unaltered alveolar bone support tended to have technical failures as chipping of the veneering material. CFDP with reduced alveolar bone support tended to experience biological failures as abutment fractures. Differences of alveolar bone support and thus tooth mobility between mesial and distal abutments of three-unit CFDP did not influence load capability. A distal post-supported, root-treated abutment tooth did not increase risk of restoration failure.
References
Pjetursson BE, Tan K, Lang NP, Bragger U, Egger M, Zwahlen M (2004) A systematic review of the survival and complication rates of fixed partial dentures (FPDs) after an observation period of at least 5 years. Clin Oral Implants Res 15(6):667–676. https://doi.org/10.1111/j.1600-0501.2004.01120.x
Jepson N, Allen F, Moynihan P, Kelly P, Thomason M (2003) Patient satisfaction following restoration of shortened mandibular dental arches in a randomized controlled trial. Int J Prosthodont 16(4):409–414
Ewing EE (1957) Reevaluation of the cantilever principle. J Prosthet Dent 7(1):78–92. https://doi.org/10.1016/0022-3913(57)90011-2
Lulic M, Bragger U, Lang NP, Zwahlen M, Salvi GE (2007) Ante’s (1926) law revisited: a systematic review on survival rates and complications of fixed dental prostheses (FDPs) on severely reduced periodontal tissue support. Clin Oral Implants Res 18(Suppl 3):63–72. https://doi.org/10.1111/j.1600-0501.2007.01438.x
Nyman S, Lindhe J (1979) A longitudinal study of combined periodontal and prosthetic treatment of patients with advanced periodontal disease. J Periodontol 50(4):163–169. https://doi.org/10.1902/jop.1979.50.4.163
Wylie RS, Caputo AA (1991) Fixed cantilever splints on teeth with normal and reduced periodontal support. J Prosthet Dent 66(6):737–742. https://doi.org/10.1016/0022-3913(91)90406-M
Yang HS, Chung HJ, Park YJ (1996) Stress analysis of a cantilevered fixed partial denture with normal and reduced bone support. J Prosthet Dent 76(4):424–430. https://doi.org/10.1016/S0022-3913(96)90549-1
Skupien JA, Opdam NJ, Winnen R, Bronkhorst EM, Kreulen CM, Pereira-Cenci T, Huysmans MC (2016) Survival of restored endodontically treated teeth in relation to periodontal status. Braz Dent J 27(1):37–40. https://doi.org/10.1590/0103-6440201600495
Iqbal MK, Johansson AA, Akeel RF, Bergenholtz A, Omar R (2003) A retrospective analysis of factors associated with the periapical status of restored, endodontically treated teeth. Int J Prosthodont 16(1):31–38
Rodriguez FR, Paganoni N, Eickholz P, Weiger R, Walter C (2017) Presence of root canal treatment has no influence on periodontal bone loss. Clin Oral Investig 21(9):2741–2748. https://doi.org/10.1007/s00784-017-2076-4
Ohlmann B, Marienburg K, Gabbert O, Hassel A, Gilde H, Rammelsberg P (2009) Fracture-load values of all-ceramic cantilevered FPDs with different framework designs. Int J Prosthodont 22(1):49–52
Gabbert O, Ohlmann B, Schmitter M, Gilde H, Ruef T, Rammelsberg P (2008) Fracture behaviour of zirconia ceramic cantilever fixed dental prostheses in vitro. Acta Odontol Scand 66(4):200–206. https://doi.org/10.1080/00016350802241555
Wolfart S, Harder S, Eschbach S, Lehmann F, Kern M (2009) Four-year clinical results of fixed dental prostheses with zirconia substructures (Cercon): end abutments vs. cantilever design. Eur J Oral Sci 117(6):741–749. https://doi.org/10.1111/j.1600-0722.2009.00693.x
Zenthofer A, Ohlmann B, Rammelsberg P, Bomicke W (2015) Performance of zirconia ceramic cantilever fixed dental prostheses: 3-year results from a prospective, randomized, controlled pilot study. J Prosthet Dent 114(1):34–39. https://doi.org/10.1016/j.prosdent.2015.02.006
Sterzenbach G, Kalberlah S, Beuer F, Frankenberger R, Naumann M (2011) In-vitro simulation of tooth mobility for static and dynamic load tests: a pilot study. Acta Odontol Scand 69(5):316–318. https://doi.org/10.3109/00016357.2011.563244
Rosentritt M, Behr M, Gebhard R, Handel G (2006) Influence of stress simulation parameters on the fracture strength of all-ceramic fixed-partial dentures. Dent Mater 22(2):176–182. https://doi.org/10.1016/j.dental.2005.04.024
Rosentritt M, Behr M, van der Zel JM, Feilzer AJ (2009) Approach for valuating the influence of laboratory simulation. Dent Mater 25(3):348–352. https://doi.org/10.1016/j.dental.2008.08.009
Anusavice KJ, Kakar K, Ferree N (2007) Which mechnical and physical testing methods are relevant for predicting the clinical performance of ceramic-based dental prostheses? Clin Oral Implants Res Suppl 3(18):218–231
Kelly JR (1999) Clinically relevant approach to failure testing of all-ceramic restorations. J Prosthet Dent 81(6):652–661. https://doi.org/10.1016/S0022-3913(99)70103-4
Bolhuis HP, de Gee AJ, Pallav P, Feilzer AJ (2004) Influence of fatigue loading on the performance of adhesive and nonadhesive luting cements for cast post-and-core buildups in maxillary premolars. Int J Prosthodont 17(5):571–576
Romeo E, Lops D, Margutti E, Ghisolfi M, Chiapasco M, Vogel G (2003) Implant-supported fixed cantilever prostheses in partially edentulous arches. A seven-year prospective study. Clin Oral Implants Res 14(3):303–311. https://doi.org/10.1034/j.1600-0501.2003.120905.x
Naumann M, Blankenstein F, Dietrich T (2005) Survival of glass fibre reinforced composite post restorations after 2 years-an observational clinical study. J Dent 33(4):305–312
Tan K, Pjetursson BE, Lang NP, Chan ES (2004) A systematic review of the survival and complication rates of fixed partial dentures (FPDs) after an observation period of at least 5 years. Clin Oral Implants Res 15(6):654–666. https://doi.org/10.1111/j.1600-0501.2004.01119.x
Karlsson S (1989) Failures and length of service in fixed prosthodontics after long-term function. A longitudinal clinical study. Swed Dent J 13(5):185–192
Rodriguez AM, Aquilino SA, Lund PS (1994) Cantilever and implant biomechanics: a review of the literature, Part 2. J Prosthodont 3(2):114–118. https://doi.org/10.1111/j.1532-849X.1994.tb00138.x
Wang CH, Du JK, Li HY, Chang HC, Chen KK (2016) Factorial analysis of variables influencing mechanical characteristics of a post used to restore a root filled premolar using the finite element stress analysis combined with the Taguchi method. Int Endod J 49(7):690–699. https://doi.org/10.1111/iej.12499
Goga R, Purton DG (2007) The use of endodontically treated teeth as abutments for crowns, fixed partial dentures, or removable partial dentures: a literature review. Quintessence Int 38(2):e106–e111
Soderfeldt B, Palmqvist S (1998) A multilevel analysis of factors affecting the longevity of fixed partial dentures, retainers and abutments. J Oral Rehabil 25(4):245–252. https://doi.org/10.1111/j.1365-2842.1998.00248.x
Randow K, Glantz PO (1986) On cantilever loading of vital and non-vital teeth. An experimental clinical study. Acta Odontol Scand 44(5):271–277. https://doi.org/10.3109/00016358609004733
Randow K, Glantz PO, Zoger B (1986) Technical failures and some related clinical complications in extensive fixed prosthodontics. An epidemiological study of long-term clinical quality. Acta Odontol Scand 44(4):241–255. https://doi.org/10.3109/00016358608997726
Naumann M, Rosentritt M, Preuss A, Dietrich T (2006) The effect of alveolar bone loss on the load capability of restored endodontically treated teeth: a comparative in vitro study. J Dent 34(10):790–795. https://doi.org/10.1016/j.jdent.2006.03.003
Tunjan R, Rosentritt M, Sterzenbach G, Happe A, Frankenberger R, Seemann R, Naumann M (2012) Are endodontically treated incisors reliable abutments for zirconia-based fixed partial dentures in the esthetic zone? J Endod 38(4):519–522. https://doi.org/10.1016/j.joen.2011.12.027
Sterzenbach G, Tunjan R, Rosentritt M, Naumann M (2014) Increased tooth mobility because of loss of alveolar bone support: a hazard for zirconia two-unit cantilever resin-bonded FDPs in vitro? J Biomed Mater Res B Appl Biomater 102(2):244–249. https://doi.org/10.1002/jbm.b.33001
Strub JR, Linter H, Marinello CP (1989) Rehabilitation of partially edentulous patients using cantilever bridges: a retrospective study. Int J Periodontics Restorative Dent Dent 9(5):364–375
Reinhardt RA, Krejci RF, Pao YC, Stannard JG (1983) Dentin stresses in post-reconstructed teeth with diminishing bone support. J Dent Res 62(9):1002–1008. https://doi.org/10.1177/00220345830620090101
Vire DE (1991) Failure of endodontically treated teeth: classification and evaluation. J Endod 17(7):338–342. https://doi.org/10.1016/S0099-2399(06)81702-4
Axelsson P, Lindhe J, Nystrom B (1991) On the prevention of caries and periodontal disease. Results of a 15-year longitudinal study in adults. J Clin Periodontol 18(3):182–189
Tay FR, Pashley DH (2007) Monoblocks in root canals: a hypothetical or a tangible goal. J Endod 33(4):391–398. https://doi.org/10.1016/j.joen.2006.10.009
Acknowledgements
Dentsply Sirona allowed the use of the milling machine to produce zirconia frameworks. No further external financial support was given.
Contribution to the paper
M. Naumann: idea, hypothesis, experimental design, and wrote the manuscript.
M. v. Stein-Lausnitz: idea, hypothesis, experimental design, and proofread the manuscript.
M. Rosentritt: performed TCML and proofread the manuscript.
C. Walter: contributed substantially to discussion and proofread the manuscript.
H. Meyer-Lückel: contributed substantially to discussion and proofread the manuscript.
G. Sterzenbach: experimental design, performed linear loading, and performed in part statistical evaluation.
Funding
The work was supported by the Department of Prosthodontics, Geriatric Dentistry and Craniomandibular Disorders, Charité – Universitätsmedizin Berlin, Aßmannshauser Str. 4-6, D-14197, Berlin, Germany. This research was also supported by Ivoclar-Vivadent by Materials.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors. All applicable international, national, and/or institutional guidelines for the care and use of animals were followed. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
For this type of study, formal consent is not required.
Additional information
M. Naumann and M. von Stein-Lausnitz shared first authorship.
Rights and permissions
About this article
Cite this article
Naumann, M., von Stein-Lausnitz, M., Rosentritt, M. et al. Impact of simulated reduced alveolar bone support, increased tooth mobility, and distal post-supported, root-treated abutment tooth on load capability of all-ceramic zirconia-supported cantilever FDP. Clin Oral Invest 22, 2799–2807 (2018). https://doi.org/10.1007/s00784-018-2366-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-018-2366-5