Abstract
Objective
The objective of the present study is to compare the effects on soft tissue profile in class II patients after treatment with either “Functional Mandibular Advancer” (FMA) or Herbst appliance.
Materials and methods
The study included n = 42 patients treated with either FMA (n = 21) or Herbst appliance (n = 21) by the same experienced orthodontist. The treatment followed a single-step advancement protocol. Lateral cephalograms were analyzed through a set of customized measurements. The actual therapeutic effect was calculated using data from a growth survey. After testing for normal distribution and homogeneity of variance, data were analyzed by one-sample Student’s t tests and independent Student’s t tests. Statistical significance was set at p < 0.05.
Results
For both FFAs, significant upper lip retrusion, increase in lower lip’s thickness, and length of the lower face occurred. Additionally, significant lower lip retrusion and straightening of the profile were found in FMA and Herbst appliance patients. All remaining variables revealed no significant differences.
Conclusions
Treatment-related changes on the facial soft tissue profile could be regarded similar in class II patients treated with FMA or Herbst appliance. No treatment-related changes that were specific for FMA or Herbst appliance could be identified. Only moderate changes were noted comparing pre- and posttreatment soft tissue profiles.
Clinical relevance
Despite proven differences in skeletal and dental treatment effects, the facial profile has not to be taken into consideration when choosing between FMA and Herbst appliance for class II treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Angle class II malocclusions are frequently diagnosed in orthodontic patients [1]. Class II malocclusions with a mandibular deficiency have been treated with different functional appliances (FAs) [2] for more than a century. Apart from removable functional appliances (RFAs) [3], fixed functional appliances (FFAs) can be used for class II correction without patient’s cooperation [2]. Apart from skeletal and dental changes during treatment [4], facial soft tissue profile [5] and esthetics also ought to be improved during class II correction [2, 6].
FFAs, like Herbst appliance [7] or “Functional Mandibular Advancer” (FMA) [8], exert an anteriorly directed force to the mandible through rigid mechanisms.
Emil Herbst introduced his “Retentions-Scharnier,” later commonly called Herbst appliance, in 1909 at an international dental congress in Berlin/Germany. The Herbst appliance has become the most frequently used FFA for class II correction [9]. In 1934, he summarized his 25 years’ experience with the appliance in a series of three articles [10,11,12]. After that, the appliance literally disappeared for more than four decades until 1979, when Pancherz [7] reintroduced and continued the development of the Herbst appliance [9, 13]. The Herbst appliance rigidly connects the first upper molar with the mandibular first bicuspid on both sides through a telescopic (rod and tube) mechanism [9] for permanent advancement of the mandible into a protruded position.
In 2002, Kinzinger et al. [8] introduced the FMA pursuing a novel biomechanical concept in FFAs. Other than the Herbst appliance, the FMA exerts a rigid intergnathic force from upper to lower first molars for mandibular advancement. Adopting an established concept from functional jaw orthopedics, the FMA uses inclined planes at 60° to horizontal for this purpose [14].
Apart from feasible dentoskeletal effects [15,16,17,18], treatment-related changes of the patient’s soft tissue profile have been described for different FFAs [5, 19, 20]. However, availability of data is limited [20]. While some studies assessing soft tissue changes are available for the Herbst appliance [5, 21,22,23], corresponding data for the FMA are unavailable. It can be hypothesized that treatment effects might vary because of the diverse design of FMA and Herbst appliance. This has not been investigated to date.
Therefore, this retrospective investigation compares effects on the soft tissue profile in patients with a skeletal class II, who were treated successfully with either FMA or Herbst appliance. The study analyzes lateral cephalograms which were routinely obtained during orthodontic treatment.
Material and methods
Patients
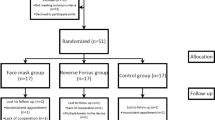
Ethical approval for this retrospective study was granted (Ethics Commission of University of Aachen, Germany, No. 171/08). In agreement with a recent study [4], the sample size was calculated based on a significance level of 0.05 and a power of 80% to detect a clinically meaningful difference of 2.0 (±2.0 mm/±2.0°). Patients were recruited throughout a 3-year period. The power analysis showed that at least 17 patients per group were required. However, more patients were included in the sample to compensate for possible dropouts during the study period. All patients showed the need for mandibular advancement because of a class II malocclusion. The allocation to either FMA or Herbst appliance was random. Cephalometric measurements prior to treatment (T1) ensured that no significant differences between FMA and Herbst appliance patients existed. Treatment was always performed by the same experienced orthodontist. In all patients, a single-step advancement protocol was employed. The mandible was always initially protruded into an edge-to-edge position.
Inclusion criteria were as follows: fully dentate patients in permanent dentition (except for third molars), and no teeth were lost during treatment, no history of previous orthodontic treatment, pretreatment ANB angle ≥4°, and distal molar relationship of at least one-half cusp width. Exclusion criteria included craniofacial anomalies, loss or congenital agenesis of permanent teeth (except for third molars), or planned extraction protocol.
The patients were divided into two groups and received treatment with FMA (group 1) [8] (Functional Mandibular Advancer®, Forestadent, Pforzheim, Germany) or cast splint Herbst appliance (group 2) [9, 13] (Herbst®, Dentaurum, Ispringen, Germany) based on their choice after being shown images from each appliance (Fig. 1).
A total of five patients dropped out. Three Herbst appliance patients and one FMA patient moved away, and another FMA patient discontinued due to medical reasons. Thus, the FMA group consisted of 21 patients (11 males, 10 females). Pretreatment age (T1) was mean 16 years and 2 months for males and 15 years and 9 months for females. The Herbst appliance group also included 21 patients (11 males, 10 females). Pretreatment age (T1) was mean 12 years and 1 month for males and 13 years and 2 months for females. Similar to other Herbst [24] and FMA studies [25], a control group was set up on the basis of data published by Bhatia and Leighton [26] in 1993. Their longitudinal facial growth data were retrieved from Caucasian subjects who were approached at King’s College School of Medicine and Dentistry in London/UK.
According to an earlier investigation [17], the chronological age of the subjects was recorded rather than the skeletal maturation stage. The corresponding values for the control group were then matched to ages recorded at T1 and T2. The difference between T1 and T2 in study and control groups was then assumed to represent growth effects. This difference was then subtracted from the measurements between T1 and T2 in both groups. This result represented the treatment effect, referred to as ‘Net’ effect.
Cephalometric headfilms
Conventional cephalometric headfilms were available pretreatment (T1) and immediately after appliance removal (T2) for all patients. All headfilms were taken using an analogue X-ray cephalograph (Orthophos®, Sirona, Bensheim, Germany). The focus film distance was 1.5 m. Head posture and maximal intercuspation were standardized: the X-ray device fixated the head through ear olive holders and a nose rest. A line is projected on the patient’s head, allowing to adjust the head posture according to the Frankfort horizontal. The patients were previously instructed to apply maximal intercuspation. A scale was projected into each image. The radiation data were matched to the patient and varied between 73 kV/15 mA and 77 kV/14 mA with an exposure time of 9 s. The lateral cephalograms were then digitalized using an Epson Expression 1680 scanner (Epson Deutschland GmbH, Meerbusch, Germany) and analyzed using “fr-win®, version 7.0” software (Computer Konkret, Falkenstein, Germany). The image viewing system was officially certified for radiographic diagnostics. This dedicated tracing software can measure two decimals if the magnification factor of the X-ray is known. The latter has been ensured by projection of a scale into each image.
To minimize the patient’s radiation burden according to the ALARA (as low as reasonably achievable) [27] principle, hand-wrist X-rays were not taken. The control group data [26] were gathered using chronological age instead of skeletal maturation stages. The lateral cephalograms were analyzed according to the method described by Kinzinger et al. [19] by a single blinded examiner. The analysis included a set of linear (horizontal and vertical) and angular soft tissue and selected angular dentoalveolar measurements (Table 1). Figure 2 shows a graphical representation of the measurements.
Cephalometric measurements. a Linear measurements in relation to Frankfort horizontal (FH) and Ricketts’ Esthetic line (E-Line): Pog’-Sn on FH, Li-Sn on FH, Ls-Sn on FH, Li-E-Line, and Ls-E-Line. b Linear measurements in relation to Frankfort Horizontal (FH): Me’-FH, Sn-FH, Li-FH, and Ls-FH. c Linear measurements in relation to mandibular plane (MP): Sn-MP, Li-MP, and Ls-MP. d Linear measurements in relation to palatal plane (PP) and mandibular plane (MP): A-A’ on PP, B-B’ on MP, and Pog-Pog’ on MP. e Soft tissue profile angular measurements: N’-Pn-Pog’, N’-Sn-Pog’, and Cm-Sn-Ls. f Inclination of upper and lower central incisors: U1/PP and L1/MP
Statistical analysis
The same examiner retraced and remeasured selected headfilms of both groups after an interval of 1 month. The method error (ME) was then calculated using the Dahlberg-formula (ME = √(∑d 2/2n)) [28]. ME was 0.78 mm for linear and 0.57 ° for angular measurements. The ME was <1 for all measurements. Data were recorded using spreadsheet software (Excel®, Microsoft Corporation, Redmond, Washington, USA). The Kolmogorov-Smirnov test confirmed normal distribution of the data. Homogeneity of variance was tested using Levene’s method. Treatment-related changes were analyzed with one-sample Student’s t tests for intragroup comparisons and independent Student’s t tests for intergroup comparisons. Descriptive statistics mean (M) and standard deviation (SD) are recorded for each variable. Additionally, 95% confidence intervals (95% CI) were calculated. All statistical analyses were performed using SAS® for Windows® 9.1 (SAS Institute Inc., Cary, NC, USA). Statistical significance was set at p < 0.05.
Results
Prior to treatment (T1), cephalometric measurements revealed no statistically significant (p > 0.05) differences between FMA and Herbst appliance patients.
Total treatment time was in FMA patients, mean 1.32 ± 0.71 years, and mean 1.46 ± 0.38 years in Herbst appliance patients. These treatment periods included the necessary leveling and aligning with a comprehensive fixed appliance after FFA removal. The average application of the fixed functionals within this period was 7.2 months in the FMA and 7.3 months in the Herbst appliance group. No significant difference was found (p = 0.6223 and p = 0.7285).
The results of the cephalometric measurements are shown in Tables 2, 3, and 4. No significant intergroup differences were found. In both appliances, significant (p < 0.05) intragroup changes were found for Ls-E-Line, B-B’ on MP, and Me’-FH. In our study sample, significant lower lip protrusion (Li-Sn on FH) (p < 0.01) and straightening of the profile (N’-Sn-Pog’, soft tissue profile excluding nose) (p < 0.05) were found in FMA patients only. In Herbst appliance patients, significant (p < 0.01) lower lip retrusion (Li-E-Line) and a straightening of the profile (N’-Pn’-Pog’, soft tissue profile including nose) (p < 0.05) occurred. Moreover, vertical linear measurements Li-FH (p < 0.001) and Ls-MP (p < 0.01) increased corresponding with the increased length of the lower face. All remaining variables revealed no significant differences.
Discussion
Treatment-related changes of the soft tissue profile between patients treated either with FMA or Herbst appliance by analyzing lateral cephalograms have not been studied to date. Hence, our investigation adds new data to the literature.
As expected, some studies assessing soft tissue changes are available for the Herbst appliance [5, 21,22,23] but none specifically for the FMA. Due to methodological differences between these investigations, direct comparison with our values is partially impossible.
Similarly, in both groups, the upper lip was retruded (Ls-E-Line), but the lower lip’s thickness (B-B’ on MP) and the length of the lower face (Me’-FH) increased statistically significant. The results of these linear measurements were quite similar. Differences between the mean values were approximately 0.2 mm, which is in agreement with data from the literature [5]. Obviously, the mean changes of these variables were clinically insignificant.
Although no statistically significant differences between both FFAs existed, the nasolabial angle (Cm-Sn-Ls) showed more pronounced Net changes in our Herbst appliance patients. Surprisingly, posttreatment (T2) nasolabial angles were mean 114.78° for FMA and 118.64° for Herbst appliance and hence greater than the proposed “normal” values—ranging from 85° to 105° [29, 30]—and also greater than an “ideal” nasolabial angle [31]. However, race and gender differences have to be considered [30, 31].
One aim of class II correction is the reduction in profile convexity [5]. In both studied FFAs, a straightening of the soft tissue profile occurred: N’-Sn-Pog’ (soft tissue profile, excluding nose) and N’-Pn’-Pog’ (soft tissue profile, including nose) showed a mean increase, ranging from +0.04 to 2.72 mm, which was smaller than reported in the literature [5, 21].
A recent systematic review and meta-analysis by Zymperdikas et al. [20] found that FFAs had statistically significant influence on patients’ soft tissue profiles. The authors found that the N’-Sn-Pog’ angle (soft tissue profile, excluding nose) increased on average by 2.01° per year, thus also confirming straightening of the soft tissue profile. Interestingly, only one [22] of the four [22, 32,33,34] included studies investigated a cast splint Herbst appliance type, whereas the remaining three studies [32,33,34] focused on nonrigid Herbst appliance hybrids. Based on the results of their review, Zymperdikas et al. [20] stated that soft tissues were significantly affected in favor of profile improvement by FFAs.
Meyer-Marcotty et al. [35] investigated treatment-related alterations of the facial soft tissues in Herbst appliance patients using three-dimensional face scans based on a stereophotogrammetric method. The authors also found favorable effects on the facial soft tissue profile, particularly in patients with a convex profile and a retrusive lower lip. There is considerable variation in how attractive raters judge a face to be [36,37,38,39]. Although there is no accepted standard as to what constitutes an attractive soft tissue profile, a general preference for relatively straight profiles has been reported [40, 41]. At least Caucasians prefer a straight profile [2, 6], and this was achieved in our sample with both FFAs, since the soft tissue profile was always straightened.
In our study sample, the upper lip (Ls-E-Line) retruded similarly in FMA and Herbst appliance patients. However, contradictory results have been published regarding the positional changes of the upper lip [2]. Whereas one study [5] reported a retrusion, another showed protrusion of the upper lip [42]. In agreement with the literature [5, 42, 43], the lower lip (Li-E-Line) showed marginal retrusion in our patients. This seemed contradictory because significant proclination occurred in our sample after treatment with both FFA types. Similar to other investigators [5, 43], we used the Esthetic line (E-Line) as reference to record positional changes of the upper and lower lips. However, this is not without controversy. Flores-Mir et al. [2] stated that E-Line is not a good reference to quantify changes in the lips because simultaneous changes in the soft tissue pogonion (Pog’) or pronasale (Pn) could create the impression of lip changes that are really nonexistent. We accounted for growth-related changes by calculating the treatment effect, referred to as the Net effect.
Bhatia and Leighton’s [26] longitudinal survey of facial growth was used as control and basis for the calculation of the Net effect. Individuals with and without malocclusion included in their survey were between 4 and 20 years of age and age-matched to our study sample. However, an ideal control group would comprise untreated class II subjects followed up on a regular basis, which is not available. Thus, limitations are inevitable when employing data from growth studies [44].
Typical dental changes as described in the literature [45, 46] occurred in both groups. All patients experienced proclination of mandibular incisors and retroclination of maxillary incisors. The FMA patients showed greater proclination of mandibular incisors than the Herbst appliance patients, but the differences were not statistically significant. Besides the size of the nasolabial angle or the sagittal position of the lips, the thickness of the upper lip might also be altered by changes in upper incisor inclination [47,48,49,50]. In our sample, the average upper lip thickness (A-A’ on PP) remained nearly unchanged in both groups despite the retraction of maxillary incisors. Contradictory to our results, some authors [47, 48] reported increases in upper lip thickness whereas other investigators [49, 50] described decreases. However, different methodologies should be considered when judging the results of those studies. The extent and predictability of changes in incisor’s axial inclination on soft tissue profile remain a matter to debate [2].
Our study analyzed lateral cephalograms which were routinely obtained during orthodontic treatment. Cephalometric measurements were found suitable to describe changes of the soft tissue profile due to FFA treatment [5, 21,22,23]. Still, lateral cephalometry is a two-dimensional imaging modality which is not able to detect three-dimensional (3D) alterations of the facial soft tissues. To overcome these drawbacks, different 3D approaches have been described in the literature [51]. Data on functional appliance treatment are rather scarce [35]. However, reliable superimposition of soft tissue structures is difficult, and many unsolved questions have to be addressed in future research [51, 52]. These studies also state that none of the modalities is superior to the other.
In our study sample, treatment-related changes of the patients’ soft tissue profiles were similar between the examined FFAs, and hence, no significant intergroup differences were found. Therefore, our results suggest that none of the two appliances was superior in altering the facial profile. Still, it is possible to improve the patients’ soft tissue profiles using FFAs [20]. However, treatment-related soft tissue changes are difficult to predict [35] and may differ from patient to patient.
Conclusions
-
Treatment-related changes on the facial soft tissue profile were similar in patients treated with FMA or the Herbst appliance.
-
Results suggest that none of the measurements exhibited treatment-related changes that were specific for FMA or Herbst appliance.
-
Only moderate changes of the soft tissue profile were noted.
References
Bishara SE (2006) Class II malocclusions: diagnostic and clinical considerations with and without treatment. Semin Orthod 12:11–24
Flores-Mir C, Major MP, Major PW (2006) Soft tissue changes with fixed functional appliances in class II division 1. Angle Orthod 76:712–720
Koretsi V, Zymperdikas VF, Papageorgiou SN, Papadopoulos MA (2015) Treatment effects of removable functional appliances in patients with class II malocclusion: a systematic review and meta-analysis. Eur J Orthod 37:418–434
Kinzinger GSM, Lisson JA, Frye L, Gross U, Hourfar J (2017) A retrospective cephalometric investigation of two fixed functional orthodontic appliances in class II treatment: Functional Mandibular Advancer vs. Herbst appliance. Clin Oral Investig 1–12
Pancherz H, Anehus-Pancherz M (1994) Facial profile changes during and after Herbst appliance treatment. Eur J Orthod 16:275–286
Peck H, Peck S (1970) A concept of facial esthetics. Angle Orthod 40:284–318
Pancherz H (1979) Treatment of class II malocclusions by jumping the bite with the Herbst appliance. A cephalometric investigation. Am J Orthod 76:423–442
Kinzinger G, Ostheimer J, Förster F, Kwandt PB, Reul H, Diedrich P (2002) Development of a new fixed functional appliance for treatment of skeletal class II malocclusion first report. J Orofac Orthop 63:384–399
Pancherz H (2003) History, background, and development of theHerbst appliance. Semin Orthod 9:3–11
Herbst E (1934) Dreißigjährige Erfahrungen mit dem Retentions-Scharnier. Zahnärztl Rundsch 43:1515–1524
Herbst E (1934) Dreißigjährige Erfahrungen mit dem Retentions-Scharnier. Zahnärztl Rundsch 43:1563–1568
Herbst E (1934) Dreißigjährige Erfahrungen mit dem Retentions-Scharnier. Zahnärztl Rundsch 34:1611–1616
Pancherz H, Ruf S (2008) The Herbst appliance: research-based clinical management. Quintessence, Chicago
Kinzinger GS, Diedrich PR (2005) Bite jumping with the Functional Mandibular Advancer. J Clin Orthod 39:696–700
Pancherz H (1985) The Herbst appliance—its biologic effects and clinical use. Am J Orthod 87:1–20
Ruf S, Pancherz H (1999) Temporomandibular joint remodeling in adolescents and young adults during Herbst treatment: a prospective longitudinal magnetic resonance imaging and cephalometric radiographic investigation. Am J Orthod Dentofac Orthop 115:607–618
Frye L, Diedrich PR, Kinzinger GS (2009) Class II treatment with fixed functional orthodontic appliances before and after the pubertal growth peak - a cephalometric study to evaluate differential therapeutic effects. J Orofac Orthop 70:511–527
Kinzinger G, Kober C, Diedrich P (2007) Topography and morphology of the mandibular condyle during fixed functional orthopedic treatment—a magnetic resonance imaging study. J Orofac Orthop 68:124–147
Kinzinger G, Frye L, Diedrich P (2009) Class II treatment in adults: comparing camouflage orthodontics, dentofacial orthopedics and orthognathic surgery—a cephalometric study to evaluate various therapeutic effects. J Orofac Orthop 70:63–91
Zymperdikas VF, Koretsi V, Papageorgiou SN, Papadopoulos MA (2016) Treatment effects of fixed functional appliances in patients with class II malocclusion: a systematic review and meta-analysis. Eur J Orthod 38:113–126
Ruf S, Pancherz H (1999) Dentoskeletal effects and facial profile changes in young adults treated with the Herbst appliance. Angle Orthod 69:239–246
Baysal A, Uysal T (2013) Soft tissue effects of twin block and Herbst appliances in patients with class II division 1 mandibular retrognathy. Eur J Orthod 35:71–81
de Almeida MR, Flores-Mir C, Brandao AG, de Almeida RR, de Almeida-Pedrin RR (2008) Soft tissue changes produced by a banded-type Herbst appliance in late mixed dentition patients. World J Orthod 9:121–131
Ruf S, Pancherz H (2006) Herbst/multibracket appliance treatment of class II division 1 malocclusions in early and late adulthood. A prospective cephalometric study of consecutively treated subjects. Eur J Orthod 28:352–360
Kinzinger G, Diedrich P (2005) Skeletal effects in class II treatment with the Functional Mandibular Advancer (FMA)? J Orofac Orthop 66:469–490
Bhatia SN, Leighton BC (1993) A manual of facial growth: a computer analysis of longitudinal cephalometric growth data. Oxford University Press, Oxford
IRCP (2001) Radiation and your patient—a guide for medical practitioners. ICRP Supporting Guidance 2. Available at: http://www.icrp.org/publication.asp?id=ICRP%20Supporting%20Guidance%202. Accessed: 2016-15-03. Ann IRCP 31
Dahlberg G (1940) Statistical methods for medical and biological students. Interscience Publications, New York
Lines PA, Lines RR, Lines CA (1978) Profilemetrics and facial esthetics. Am J Orthod 73:648–657
Burstone CJ (1967) Lip posture and its significance in treatment planning. Am J Orthod Dentofac Orthop 53:262–284
Sinno HH, Markarian MK, Ibrahim AM, Lin SJ (2014) The ideal nasolabial angle in rhinoplasty: a preference analysis of the general population. Plast Reconstr Surg 134:201–210
Gunay EA, Arun T, Nalbantgil D (2011) Evaluation of the immediate dentofacial changes in late adolescent patients treated with the Forsus FRD. Eur J Dent 5:423–432
Oztoprak MO, Nalbantgil D, Uyanlar A, Arun T (2012) A cephalometric comparative study of class II correction with Sabbagh Universal Spring (SUS(2)) and Forsus FRD appliances. Eur J Dent 6:302–310
Uyanlar A, Nalbantgil D, Arun T (2014) Evaluation of dentofacial changes caused with Sabbagh Universal Spring in mandibular retrognathic patients: a pilot study. Dentistry 4:237
Meyer-Marcotty P, Kochel J, Richter U, Richter F (2012) Reaction of facial soft tissues to treatment with a Herbst appliance. J Orofac Orthop 73:116–125
Tatarunaite E, Playle R, Hood K, Shaw W, Richmond S (2005) Facial attractiveness: a longitudinal study. Am J Orthod Dentofac Orthop 127:676–682
Xu TM, Korn EL, Liu Y, Oh HS, Lee KH, Boyd RL, Baumrind S (2008) Facial attractiveness: ranking of end-of-treatment facial photographs by pairs of Chinese and US orthodontists. Am J Orthod Dentofac Orthop 134:74–84
Varlık SK, Demirbas E, Orhan M (2010) Influence of lower facial height changes on frontal facial attractiveness and perception of treatment need by lay people. Angle Orthod 80:1159–1164
von Bremen J, Erbe C, Pancherz H, Ruf S (2014) Facial-profile attractiveness changes in adult patients treated with the Herbst appliance. J Orofac Orthop 75:167–174
Mees S, Jimenez Bellinga R, Mommaerts MY, De Pauw GA (2013) Preferences of AP position of the straight Caucasian facial profile. J Craniomaxillofac Surg 41:755–763
Naini FB, Donaldson AN, McDonald F, Cobourne MT (2012) Assessing the influence of lower facial profile convexity on perceived attractiveness in the orthognathic patient, clinician, and layperson. Oral Surg Oral Med Oral Pathol Oral Radiol 114:303–311
Ruf S, Pancherz H (2004) Orthognathic surgery and dentofacial orthopedics in adult class II division 1 treatment: mandibular sagittal split osteotomy versus Herbst appliance. Am J Orthod Dentofac Orthop 126:140–152
Booij JW, Goeke J, Bronkhorst EM, Katsaros C, Ruf S (2013) Class II treatment by extraction of maxillary first molars or Herbst appliance: dentoskeletal and soft tissue effects in comparison. J Orofac Orthop 74:52–63
Barnett GA, Higgins DW, Major PW, Flores-Mir C (2008) Immediate skeletal and dentoalveolar effects of the crown- or banded type Herbst appliance on class II division 1 malocclusion. Angle Orthod 78:361–369
Pancherz H (1982) The mechanism of class II correction in Herbst appliance treatment. A cephalometric investigation. Am J Orthod Dentofac Orthop 82:104–113
Aras I, Pasaoglu A, Olmez S, Unal I, Tuncer AV, Aras A (2016) Comparison of stepwise vs single-step advancement with the Functional Mandibular Advancer in class II division 1 treatment. Angle Orthod 1:1
Talass MF, Talass L, Baker RC (1987) Soft-tissue profile changes resulting from retraction of maxillary incisors. Am J Orthod Dentofac Orthop 91:385–394
Ricketts RM (1960) Cephalometric synthesis. Am J Orthod 46:647–673
Ramos AL, Sakima MT, Pinto Ados S, Bowman SJ (2005) Upper lip changes correlated to maxillary incisor retraction—a metallic implant study. Angle Orthod 75:499–505
Hershey HG (1972) Incisor tooth retraction and subsequent profile change in postadolescent female patients. Am J Orthod 61:45–54
Nanda V, Gutman B, Bar E, Alghamdi S, Tetradis S, Lusis AJ, Eskin E, Moon W (2015) Quantitative analysis of 3-dimensional facial soft tissue photographic images: technical methods and clinical application. Prog Orthod 16:015–0082
Cevidanes LHC, Motta A, Proffit WR, Ackerman JL, Styner M (2010) Cranial base superimposition for 3D evaluation of soft tissue changes. Am J Orthod Dentofac Orthop 137:S120–S129
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Funding
The work received no funding.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors. Ethical approval for this retrospective study was granted by the Ethics Commission of University of Aachen, Germany, No. 171/08.
Informed consent
For this type of study, formal consent is not required.
Rights and permissions
About this article
Cite this article
Hourfar, J., Lisson, J.A., Gross, U. et al. Soft tissue profile changes after Functional Mandibular Advancer or Herbst appliance treatment in class II patients. Clin Oral Invest 22, 971–980 (2018). https://doi.org/10.1007/s00784-017-2177-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-017-2177-0