Abstract
Objectives
The aim of this study was to analyze the influence of dental treatment on the development of osteoradionecrosis (ORN) of the jaw.
Methods
This study included the data of 776 patients who underwent 3D-CRT or IMRT because of head and neck cancer. Sex, dental status before and after radiotherapy (RT), tumor site, bone surgery during tumor operation, concomitant chemotherapy, and the development of an advanced ORN were documented for each patient. The patients’ dentitions before and after RT were classified into four groups with regard to the number and localization of the remaining teeth. Differences between the patients with ORN and patients without ORN with regard to the teeth’s condition before and after RT, and with regard to the extent of dental treatment were determined descriptively. Cox proportional hazards regression to study the association between dentition and the development of ORN.
Results
The extent of dental treatment in patients with and without ORN did not differ in a clinically relevant way. The highest risk of developing ORN was observed in patients who had undergone primary bone surgery during the tumor operation (HR = 5.58, 95%CI 2.91–10.7) and patients who had a tumor in the oral cavity (HR = 4.84, 95%CI 1.37–17.11).
Conclusions
Based on the results of this study, tumor localization and its required treatment are prognostic factors for the development of ORN.
Clinical significance
After implementing a consequent dental treatment scheme, no influence of dentition on the risk of developing ORN could be demonstrated. Patients with a lower risk could prospectively benefit from a more moderate dental treatment scheme.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The treatment of advanced tumors of the upper respiratory and digestive tracts (i.e., head and neck area) is a multidisciplinary task by current standards [1–4]. The medical team consists of oral and maxillofacial surgeons, radiation therapists, hematology oncologists, diagnostic radiologist, pathologists, and, in special cases, specialists in nuclear medicine. For tumors within the oral cavity, the early integration of a dentist in the therapy management may be especially necessary to perform prophylactic measures on mucous membranes, teeth, and dentures [5, 6]. The central task is to implement an infectious source control before radiotherapy (RT).
However, recent surveys suggest that dentists find it difficult to provide this task and want to be specifically trained for this purpose [7, 8]. This uncertainty originates from the necessity to make decisions and implement measures before RT, which can have far-reaching consequences in the course of treatment that are difficult to evaluate before treatment. In addition, dental treatment has to be performed within a short time frame of a few days or weeks. However, a particular problem is that infectious source control before RT includes a comprehensive extraction of teeth in accordance with the recommendations of the German Society of Radiooncology, Medical Physics and Radiation Biology and the German Society for Dental and Oral Medicine [9]. This therapy option instead represents the ultima ratio in dentistry. Furthermore, most patients remain skeptical about undergoing an extraction before RT because of surgical treatment received previously.
Furthermore, a treatment plan (e.g., determining which teeth have to be extracted) often has to be created after the initial contact and implemented immediately [10]. The treatment plan has to take into account the available time frame, the patient’s oral hygiene (for its evaluation, a potential or progredient restriction of mouth opening should be considered), the expected xerostomia, the development of radiation caries and later oral rehabilitation, and the greatest possible risk reduction of osteoradionecrosis (ORN) of the jaw.
An ORN of the jaw is an unwanted adverse effect of therapeutic irradiation of tumors of the head and neck area. The frequency of this effect is 40%, as reported in the literature [11]. Its subsequent treatment can lead to the complete loss of the jaws and a considerable reduction in chewing, speaking, and swallowing function. In addition to functional limitations and disfiguring facial deformities often occur and result in psychological stress and social marginalization. According to accepted theories, a substantial cause for ORN (in addition to the irradiation dose) is teeth destroyed by radiation caries [11]. Radiation caries may be an entry port for pathogenic germs into the bone that induce its necrosis. The development of radiation caries, its onset, and effective treatment often cannot be predicted adequately.
For a long time, the simplest solution was to extract all teeth before RT [12]. This approach is obsolete today. It is contradictory to the efforts of modern oncology to achieve a high quality of life standard after therapy. On the other hand, the implementation of modern three-dimensional (3D) irradiation techniques such as 3D conformal radiation therapy (3D-CRT) or intensity-modulated radiation therapy (IMRT) allows a more distinct preservation of adjacent tissues and a more precise assessment of high-irradiation and high-risk areas. It may be prospectively possible to perform dental infectious source control that is especially adapted to a patient’s situation before administering RT.
The current recommendations for dental treatment before RT take into account the former irradiation techniques. The recommendations have to be re-evaluated with regard to the modern 3D methods concerning their extent and effectiveness. This investigation attempted to define the actual ORN risk with modern irradiation techniques and a consequent dental treatment scheme before RT. The influence of the tumor site, sex, chemotherapy, the necessity for bone surgery, and changes in dentition before and after dental treatment were considered.
Patients and methods
Patients who underwent high-dose RT for head and neck cancer between January 1, 2003, and January 31, 2013, at the Department for Radiotherapy at the University Hospital of Halle were included. Inclusion criteria were primary tumors in the nasopharynx, oropharynx, uvula, tongue base, oral cavity, parotid gland, or larynx/hypopharynx. The protocols were approved by the medical faculty’s ethics committee at the Martin-Luther-University Halle-Wittenberg and conducted in accordance with the Declaration of Helsinki on Ethical Principles for Medical Research.
Surgery
Tumor and neck lymph node removal was performed in patients with early or locally advanced tumors who were in good general condition.
Bone surgery during tumor resection
Bone surgery was defined as a risk factor if removal of the jaw bone was necessary during tumor resection. This also included tumor operations that involved temporary splitting of the mandible in order to gain access to the pterygopalatine fossa, the parapharyngeal space, and the oropharynx [13, 14].
RT
Three-dimensional treatment planning with 3D-CRT (from 2003 to 2013) or IMRT (from 2006 to 2013) was performed in all patients. Treatment planning was based on a computed tomography (CT) scan of the head and neck region, with a slice thickness of 5 mm (Lightspeed; General Electric, Fairfield, USA). Patients were immobilized using a custom-made thermoplastic head–neck–shoulder mask. Two planning systems (Helax TMS version 6.1 and Oncentra Masterplan version 1.5/3.0; Nucletron, Veenendaal, Netherlands) were used for the 3D treatment planning. 3D-CRT was performed using standardized six to seven portal arrangements as described previously [15]. Patients receiving 3D-CRT were treated with 6- and 10-MV photons from a linear accelerator (Primus and Oncor; Siemens Medical Solutions, Erlangen, Germany). IMRT was based on the step-and-shoot approach with seven or nine equidistant 6-MV beams and five to eight subsegments, respectively. The treatment technique was similar to the one described by Georg et al. [16]. The planning strategy was to cover 95% of the planning target volume (PTV) with 95% of the prescribed dose. The mean dose given to at least one parotid gland was limited to 26 Gy without compromising the PTV. The maximum dose to the spinal cord was 45 Gy. Irradiation planning was performed according to reports 50 and 62 of the Commission on Radiation Units and Measurements (ICRU) [17, 18]. Planning, performance, and quality assurance were undertaken according to ICRU report 83 [19].
-
Postoperative RT
The fractionation schedule was the traditional 2.0 Gy/day, 5 days a week. A total dose of 64 to 70 Gy was delivered for each patient.
-
Definitive RT
Patients received hyperfractionated-accelerated RT with 70.6/77.6 Gy in 15 fractions of 2 Gy followed by 1.4 Gy twice a day or with 72 Gy in 14 fractions of 1.8 Gy followed by 1.8 and 1.6 Gy twice daily.
Chemotherapy
Some patients received postoperative adjuvant or definitive radiochemotherapy. The indication for chemotherapy was determined by a specialist in RT in the University Clinic Halle, who also then prescribed the following regimen:
-
Concomitant adjuvant chemotherapy with standard fractional RT
Cisplatin (20 mg/m2/day as a 30-min infusion) administered on days 1–5 and 29–33 of RT
-
Concomitant definitive chemotherapy with hyperfractionated-accelerated RT
Cisplatin (40 mg/m2/day as a 30-min infusion) administered on days 1, 8, 15, 22, and 29 of RT
-
Concomitant adjuvant chemotherapy with standard fractional RT
Cisplatin (20 mg/m2/day as a 30-min infusion) and 5-fluorouracil (600 mg/m2/day as a 120-h continuous infusion), administered on days 1–5 and 29–33 of RT. The maximum daily dose was 1800 mg
-
Concomitant definitive chemotherapy with hyperfractionated-accelerated RT
Cisplatin (20 mg/m2/day as a 30-min infusion) administered on days 1–5 and 29–33 of RT and paclitaxel (25 mg/m2/day as a 30-min infusion) twice a week during the course of RT
-
Concomitant palliative chemotherapy
Mitomycin-C (10 mg/m2/day as a 30-min infusion) administered on day 1 and, if necessary, on day 29 during RT. The maximum daily dose was 18 mg [20]
Oral treatment
Before radiotherapy
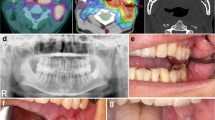
From 2003 onwards, nearly all patients were referred to the Department of Dental, Oral and Maxillofacial Medicine (Martin Luther University Halle-Wittenberg, Germany) for dental infectious source control before they underwent RT. The recommendations of “Dental treatment of patients undergoing head and neck cancer radiotherapy” by the German Society for Dental and Oral Medicine (Martin Luther University Halle-Wittenberg, Germany) were used as the basis for dental treatment [9]. A dental assistant of the University Clinic of Prosthodontics (Martin Luther University Halle-Wittenberg, Germany) performed the initial clinical examination. In coordination with a medical or dental assistant of the University Clinic of Oral and Maxillofacial Surgery, the extent of treatment was determined by the clinical and radiological findings [21–23].
By referring to the guidelines and recommendations of the German Society of Dental, Oral and Craniomandibular Sciences, the patients’ teeth were extracted before radiotherapy if they had the following criteria: (1) periodontal probing depth equal to or greater than 5 mm; (2) furcation involvement; (3) carious lesions that reached the pulp; (4) were impacted and retained; (5) large fillings, fractures, or significant occlusal wear; (6) positioned in a high dose region of >55 Gy; (7) nonvital and without sufficient root canal filling; and (8) painful, sensitive to percussion, or showed apical radiolucency.
Teeth were also removed that were predestinated to be severely affected by compromised mouth hygiene because of radiogenic trismus. The situation of a shortened dental arch was intended to avoid the complications of molar teeth extractions after radiotherapy [24]. If a shortened dental arch was impossible, the canines were preserved for later prosthodontic treatment, if possible. Initial caries and medium carious lesions were treated conventionally. All patients received a professional tooth cleaning before radiotherapy.
During radiotherapy
During the treatment course of radiotherapy, the oral cavity was inspected weekly by a radiation oncologist. At each appointment, oral hygiene instructions were reinforced. Patients who were adversely affected by mucositis up to level 1 received dexpanthenol-containing mouthwash solutions. All patients received custom-made fluoride carriers of 5 mm-thick ethylene vinyl acetate. Patients were instructed to use the carriers without fluoride gel during radiation to keep the cheek and tongue away from locally increased radiation doses caused by scattered radiation from metallic crowns. In addition, patients were instructed to use fluoride gel on their carriers for 10 min at least once daily after tooth brushing.
After radiotherapy
All patients were advised to take part in a special dental follow-up treatment. Patients were offered free professional tooth cleaning quarterly. In addition, a dental check-up was performed during these appointments. In patients with carious lesions, the teeth were treated by following the recommendations of Kielbassa et al. and Grotz [9, 21].
Dentition
Classification of dentition
To analyze the risk factors, teeth, and prosthesis, the different arrangements of the patients’ remaining teeth were summarized in groups. For patients who have undergone RT because of head and neck cancer, it seems reasonable to consider the criteria “pressure points by prostheses” and “extent of the prosthetic masticatory rehabilitation.” The literature indicates that traumatic pressure points are associated with a higher risk for the development of ORN [25]. Therefore, the classification took into consideration the system of Elbrecht who proposed classifications by “gingival,” “periodontal-gingival,” and “periodontal” [26].
The situation of a shortened dental arch was intended for prosthetic masticatory rehabilitation [27]. The category “fully dentulous” was used if all teeth existed, except for the molars. For patients with missing teeth because of agenesis (e.g., the lateral incisors or, after orthodontic treatment, the first premolars), the category “fully dentulous” was used if the first molars existed. For patients whose missing teeth were replaced by fixed partial dentures, except for the molars, the category “partially dentulous I” was used. If one canine and adjacent teeth were missing so that at least three teeth (including the canine) subsequently had to be replaced, a periodontal-supported denture was no longer possible. This situation and all other situations in which removable partial dentures had to be used were defined as “partially dentulous II” (Table 1).
The extent of change in dentition
To clarify the extent of necessary surgical intervention, which indicates the “maintenance condition” of the dentition before dental treatment, the parameter “extent of change in dentition” was calculated. Therefore, the existing dentition was encoded, based on the following four classifications: 4 is “dentulous”; 3 is “partially dentulous I”; 2 is “partially dentulous II”; and 1 is “edentulous.” To calculate the extent of change in dentition before and after dental treatment before RT, the differences in the changes in dentition in the lower and upper jaw were summed. For patients who were edentulous in the lower or upper jaw, the generated value was doubled if the antagonistic jaw deteriorated by two classes or more. This doubling should facilitate the discrimination of the patients whose dentitions deteriorated by only one class in each jaw.
This calculation resulted in values between 0 and 6, which allowed an evaluation of the extreme values: the value “0” indicated that no change was incurred by the dental treatment. This was interpreted as an indication of stable oral conditions and good oral hygiene. It may be that these patients had good compliance. The value “6” indicated that all teeth of a previously complete dentition had to be extracted before RT. This was interpreted as an indication of unstable oral conditions and poor oral hygiene—situations that are associated with an increased risk of ORN [28].
The prevalence of “unfavorable conditions” that result from different classifications of dentition
The classification of dentition distinguishes between the upper and lower jaw. This makes it possible to determine the prevalence of unfavorable combinations between both jaws. For example, an “unfavorable” combination from a clinical point of view is the interaction between a fully dentulous upper jaw and an edentulous lower jaw treated with a complete denture. The periodontal support of natural teeth transforms the masticatory compressive forces into tensile forces that contribute to stabilizing the alveolar bone [29]. Gingival-supported dentures transfer the compressive forces without transformation directly to the alveolar bone and are implicated in its degradation. Pronounced differences between both jaws may unilaterally lead to increased bone resorption of the pressure recording areas [30].
Resorption of the alveolar bone then leads to an insufficient fit of the dentures and increases the risk of traumatic pressure points [31, 32]. The analysis of the prevalence of “unfavorable combinations” should allow an adequate risk assessment for bone resorption and the development of traumatic pressure points. Because the risk for ORN seems to be higher in the mandible, emphasis was placed on the lower jaw. In total, the four classifications of dentition resulted in 16 different combinations of the lower and the upper jaw, which were pooled into the three groups: “uncritical,” “moderately critical,” and “very critical” (Table 2).
Evaluation of ORN
Diagnosis and surgical therapy of advanced ORN was performed by a specialist of oral and maxillofacial surgery at the University Clinic Halle. The advanced ORN stage was classified as grade 3, 4, or 5 according to the Radiation Therapy Oncology Group/European Organization for Research and Treatment of Cancer classification or as grade 3 or 4 according to the late effects in normal tissue/subjective, objective, management, and analytic scale. All tumor stages were ≥II according to Schwartz and Kagan, stage 3 according to Store and Boysen, and grade 3, 4, or 5 according to Glanzmann and Gratz [33–35].
Statistical analysis
Patients were included into the study from January 1, 2003, through January 31, 2013. The last date of follow-up was November 15, 2013, when the study was terminated. The start date was the first day of RT. Data on patients were censored at the termination of the study, on the last date of contact for patients lost to follow-up, or on the date of death, whatever came first. The date of incident ORN was defined as the day of diagnosis of ORN.
The different classifications of dentition were determined descriptively for the whole cohort and for the patients who developed ORN and were tested for clinical relevant differences using the chi-square test.
The associations of sex, tumor site, bone surgery during tumor resection, chemotherapy, and dentition with ORN risk was assessed using Cox proportional hazards regression [36]. We estimated adjusted hazard ratios (HRs) and corresponding 95% confidence intervals. We also report confidence limit ratios (CLR) that help to assess the precision of the effect estimates. In principal, CLRs have a range of 1 to plus infinity. As closer the CLR to 1, as more precise the effect estimate [37].
All variables were mutually adjusted. Analyses were performed with IBM SPSS Statistics 22 (IBM Incorp., SPSS Inc., Chicago, IL, USA) and SAS 9.3 (SAS Incorp., Cary, NC, USA).
Results
Patient characteristics
The analysis included 776 patients. The average age was 58.6 ± 11.4 years. At the time of radiotherapy, the youngest patient was 21 years old and the oldest patient was 90 years old. Seventy-nine percent of all patients were male. On the basis of anatomical region and the resultant target volume, most of the patients had tumors in the oral cavity. Only a few patients had tumors in the uvula. Nearly half of the patients (47%) were treated with concomitant chemotherapy. About one-eighth underwent bone surgery during tumor resection prior to RT. A detailed breakdown of data concerning tumor site and bone surgery is provided in Table 3.
ORN
Of the 776 patients, 51 (6.6%) developed advanced ORN that required extensive surgical intervention. About 78% of patients were male, with an age average of 55.2 ± 10.1 years. Most of the patients (67%) had tumors in the oral cavity. By contrast, no patient with a tumor in the nasopharynx developed ORN. Almost half of these patients underwent bone surgery during surgical tumor resection prior to RT. Fifty-one percent received concomitant chemotherapy. Of the 51 patients who developed ORN, 42 were treated with 3D-CRT and 9 with IMRT. The median latency period was 9 months (range, 0–90 months).
The extent of dental treatment
More than one-fifth of patients were edentulous before the dental treatment. In 22% of the dentulous patients, no teeth had to be extracted before RT. In 12% of the dentulous patients, extended extractions of 11 teeth or more had to be performed during the dental treatment. For patients who developed ORN after RT, more than one-fifth (n = 11) of the patients were edentulous before the dental treatment. In 27.5% of the dentulous patients, no tooth had to be extracted before RT. In 10% of the dentulous patients, extended extractions of 11 teeth or more had to be performed during the dental treatment. Table 4 provides a precise breakdown of the extent of necessary extractions of the whole cohort and the patients with ORN.
The extent of changes in the classification of dentition
For most patients, no teeth had to be extracted or teeth extractions did not lead to a change in the classification of dentition. All teeth had to be removed in only one patient who previously had complete dentition (Table 5).
In 50% of the patients who developed ORN, no tooth had to be extracted or the extractions did not lead to a change of the classification of dentition. No patient with ORN needed such an extent of surgical treatment that a sum of 5 or 6 points was generated. In general, only a few patients of the whole cohort needed such an extended surgical treatment. There was no clinically relevant difference between the patients who developed ORN and the patients who did not develop ORN (p = 0.9, based on the chi-square test). Table 5 lists a precise breakdown.
Changes in dentition by dental treatment
After the dental treatment, the number of edentulous patients doubled from 21 to 39%. The proportion of fully dentulous patients decreased from 11.5 to 7.1%. A precise breakdown of the classifications of dentition before and after dental treatment is listed separately for the upper and lower jaw in Table 6.
In the ORN patient group, the number of edentulous patients increased from 21.6 to 23.5% after dental treatment. The proportion of fully dentulous patients decreased from 5.9 to 4.9%. A precise breakdown of the classifications of dentition before and after dental treatment is listed separately for the upper and lower jaw in Table 7.
The frequency of “unfavorable” combinations of the classifications of dentition
After dental treatment, 25% of all patients had an “uncritical” combination classification of dentition in the upper and lower jaw. In 68% of all patients, the classification was “moderately critical.” In 7% of patients, the classification was evaluated as “very critical” with regard to the potential risk of developing ORN. The distribution of the “critical,” “moderately critical,” and “very critical” combinations among patients who developed ORN did not differ from the distribution in the whole cohort (p = 0.4, based on the Pearson chi-square test).
The influence of dentition on the development of ORN
For multivariate analysis, the tumor site “hypopharynx/larynx” and the classification “fully dentulous” were chosen as the reference groups. The dominant influences on the development of ORN were the factors “oral cavity” as the tumor site and the need for bone surgery. No clinical relevant influence of dentition was demonstrated within the observation period. For the classification “partially dentulous I,” the highest hazard ratio was nominally determined; for the classification “edentulous,” the lowest hazard ratio was nominally determined. The 95% confidence intervals of the calculated hazard ratios of the different classifications of dentition overlapped each other in wide areas (Table 8).
Discussion
Based on the classification of dentition in the mandible, the relative frequency for the development of ORN was approximately 9% for patients with the classifications of “partially dentulous I” and “partially dentulous II,” respectively. However, the relative frequency of dentulous patients was 5.4%, which is close to the relative frequency of the edentulous patients at 4.6%. The existence of a large number of teeth did not unavoidably result in more cases of ORN.
In contrast to the number of the remaining teeth, the multivariate analysis showed that the factor “bone surgery during tumor operation” showed a considerable influence on the relative frequency of the development of ORN. In patients with the tumor site “tonsil,” bone surgery was necessary in 44% (4/9) of patients before RT. Eighty percent (20/34) of patients who had ORN and tumors in the oral cavity underwent bone surgery. The fact that 10 of these 20 patients were edentulous in the mandible before RT emphasizes the relationship between bone surgery and the risk of developing ORN and relativizes the meaning of extracted teeth in this connection. On reducing the whole cohort number by the patients who underwent bone surgery during tumor operation, the relative frequency of ORN decreased from 6.6 to 3.6%.
The extent of dental treatment of the patients with ORN in relation to the number of extracted teeth in the mandible (which indicates the difference of the classification of the dentition in the mandible before and after dental treatment) did not differ from the patients without ORN in a clinical relevant way. The extent of the change in the classification of dentition as an indicator for the oral conditions before RT also showed no clinically relevant differences between the patients with and without ORN. The data instead suggest that patients with ORN had a comparatively little necessity of dental treatment.
In 12 (1.5%) of the 776 patients, reconstructive dental treatment before RT was not reliably possible. It could not be excluded that no dental treatment of these patients was performed before RT. In this context, it may be important that ORN developed in two patients of these 12 patients. In these two patients, it could be demonstrated that no dental treatment was performed before RT. According to the information in the patients’ files, ORN occurred after the extensive extraction of teeth that were deeply destroyed by radiation caries. In both patients, no bone surgery was performed during tumor operation and the tumor site “hypopharynx/larynx” was regularly associated with a lower relative frequency of ORN.
With regard to the risk for the development of traumatic pressure points in the mandible, dental treatment led to a moderately critical combination in 68% of patients and to a very critical dentition combination in 7% of patients. According to the results of previous studies, pressure points from dental prostheses can influence the development of ORN [25]. Higher risk occurs with dentures that rest on the mucosa of the mandible [30].
In this investigation, the risk of patients with and without ORN to develop a traumatic pressure spot by prosthetic dentures did not differ in a clinically relevant way. In this cohort, no finding indicated that traumatic pressure points could have been associated with the development of ORN. Singular clinical patient files indicated that some patients had pressure points before RT because they had neglected dental treatment for many years before RT. It is conceivable that such pressure points could broaden during RT and subsequently lead to exposed bone.
Based on the results of this study, it was not possible to determine the patients who had a higher risk of developing ORN, based on the extent of dental treatment before RT or to deduce adequate treatment options. However, single-patient cases indicate that even in situations regularly associated with a lower risk, neglected dental treatment before RT can lead to the development of ORN. A correlation between pressure points and the development of ORN could not be determined.
In the Cox regression analysis, no clinical relevant influence of dentition on the development of ORN could be demonstrated. Edentulous patients had the lowest hazard ratio; however, because of the wide range of the values and the overlapping confidence intervals, a substantial uncertainty remained on evaluating the differences between the classifications. Hence, there is no indication from the experimental and analysis data that failures in dental treatment occurred with regard to the risk for the development of ORN.
The analysis also emphasized that, if an adequate dental treatment scheme prior to RT is followed, existing teeth are of minor importance for the development of ORN.
The development of ORN was highly influenced by the variables “bone surgery during tumor resection” (HR = 5.58, CLR = 3.68) and “oral cavity” as the tumor site (HR = 4.84, CLR = 12.49). The tumor site represents the anatomical localization of the irradiation volume. In patients with tumors in the oral cavity, the mandible was at least partially included in the primary PTV and received a high (not less than 60 Gy) therapeutic dose. After bone surgery, the already operated on arch segments, e.g., in cases of squamous cell carcinoma with jaw bone infiltration (pT4), the former tumor bed within the primary PTV received the highest prescribed dose (between 64 and 66 Gy). It does not seem surprising that these patients had, compared to patients without bone surgery, a considerably higher risk of developing ORN. These findings are confirmed by the results of Parliament et al. who showed that the mean dose found in the mandible using IMRT is higher in oral cancer than in other tumor sites [38].
This investigation could not demonstrate that any of the four classifications of dentition was accompanied with a clinical relevant enhanced risk for the mandible to develop ORN. If this assumption is still justified if only one tumor site (e.g., the oral cavity), is considered, could not be evaluated due to the considerably reduced amount of data. From the dentist’s point of view, it can be assumed that, having performed a consequent dental treatment according to the current recommendations prior to RT, the major causes for the development of ORN is outside of his responsibility. A significant reduction of the ORN frequency by optimizing the dental treatment scheme may be difficult. Extensive analysis of the data does not reveal considerable failures of the dental treatment scheme and no approaches for its optimization. However, the treatment scheme increased the number of edentulous patients and significantly reduced the number of dentulous and partially dentulous patients. If these treatment dimensions have to be necessary as the upper and the lower jaw are much less stressed by the new irradiation techniques like IMRT, they have to be evaluated prospectively. In particular, it is questionable whether patients without bone surgery and a tumor site in the hypopharynx/larynx or nasopharynx could benefit from a more moderate dental treatment scheme. This should be the subject of further clinical investigations.
Conclusion
On implementing a consequent dental treatment scheme, no influence of the dentition on the risk of developing ORN could be demonstrated. A relevant reduction of the ORN frequency by optimization of the dental treatment scheme may be difficult. Based on the results of this study, tumor site and its required treatment are the main risk factors for the development of ORN. It is questionable whether patients with a lower risk (e.g., patients who did not have bone surgery, patients with a tumor site in the hypopharynx/larynx or nasopharynx) could prospectively benefit from a more moderate dental treatment scheme.
References
Demian NM, Shum JW, Kessel IL et al (2014) Oral surgery in patients undergoing chemoradiation therapy. Oral Maxillofac Surg Clin North Am 26:193–207
Purohit S, Bhise R, Lokanatha D et al (2013) Systemic therapy in head and neck cancer: changing paradigm. Indian J Surg Oncol 4:19–26
Saloura V, Langerman A, Rudra S et al (2013) Multidisciplinary care of the patient with head and neck cancer. Surg Oncol Clin N Am 22:179–215
Epstein JB, Thariat J, Bensadoun RJ et al (2012) Oral complications of cancer and cancer therapy: from cancer treatment to survivorship. CA Cancer J Clin 62:400–422
Beech N, Robinson S, Porceddu S et al (2014) Dental management of patients irradiated for head and neck cancer. Aust Dent J 59:20–28
Brody S, Omer O, McLoughlin J et al (2013) The dentist’s role within the multi-disciplinary team maintaining quality of life for oral cancer patients in light of recent advances in radiotherapy. J Ir Dent Assoc 59:137–146
Patel Y, Bahlhorn H, Zafar S et al (2012) Survey of Michigan dentists and radiation oncologists on oral care of patients undergoing head and neckradiation therapy. J Mich Dent Assoc 94:34–45
Husein AB, Butterworth CJ, Ranka MS et al (2011) A survey of general dental practitioners in the north west of England concerning the dental care of patients following head and neck radiotherapy. Prim Dent Care 18:59–65
Grötz KA (2002) Zahnärztliche Betreuung von Patienten mit tumortherapeutischer Kopf-Hals-Bestrahlung. Dtsch Zahnarztl Z 57:509–511 German
Schiødt M, Hermund NU (2002) Management of oral disease prior to radiation therapy. Support Care Cancer 10:40–43
Niewald M, Fleckenstein J, Mang K et al (2013) Dental status, dental rehabilitation procedures, demographic and oncological data as potential risk factors for infected osteoradionecrosis of the lower jaw after radiotherapy for oral neoplasms: a retrospective evaluation. Radiat Oncol 8:227
Gehrig JD (1969) Should teeth be removed prior to radiation therapy? Dent Clin N Am 13:929–938
Steinhart H, Schroeder HG, Kleinsasser O (1993) Temporäre sagittale Unterkieferspaltung zur Eröffnung eines Zuganges in die Fossa pterygopalatina, den Parapharyngealraum und den Oropharynx. Laryngo Rhino Otol 72:532–536 German
Kolokythas A, Eisele DW, El-Sayed I et al (2009) Mandibular osteotomies for access to select parapharyngeal space neoplasms. Head & Neck 31:102–110
Kuhnt T, Janich M, Götz U et al (2006) Etablierung einer 3D-Konformationstechnik zur Radio therapie von Kopf-Hals-Tumoren unter Berücksichtigung der Parotisschonung. Strahlenther Onkol 182:325–330 German
Georg D, Kroupa B, Georg P et al (2006) Inverse planning—a comparative intersystem and interpatient constraint study. Strahlenther Onkol 182:473–480
International Commission on Radiation Units and Measurements (1993) ICRU 50: Prescribing and reporting photon beam therapy
International Commission on Radiation Units and Measurements (1999) ICRU 62: Prescribing, recording and reporting photon beam therapy
International Commission on Radiation Units and Measurements (2010) ICRU 83 Prescribing, Recording, and Reporting Intensity-Modulated Photon-Beam Therapy (IMRT)
Budach V, Stuschke M, Budach W et al (2005) Hyperfractionated accelerated chemoradiation with concurrent fluorouracil-mitomycin is more effective than dose-escalated hyperfractionated accelerated radiation therapy alone in locally advanced head and neck cancer: final results of the radiotherapy cooperative clinical trials group of the German Cancer Society 95-06 Prospective Randomized Trial. J Clin Oncol 23:1125–1135
Kielbassa AM, Hinkelbein W, Hellwig E et al (2006) Radiation-related damage to dentition. Lancet Oncol 7:326–335
Koga DH, Salvajoli JV, Alves FA (2008) Dental extractions and radiotherapy in head and neck oncology: review of the literature. Oral Dis 14:40–44
Hey J, Seidel J, Schweyen R et al (2013) The influence of parotid gland sparing on radiation damages of dental hard tissues. Clin Oral Invest 17:1619–1625
Witter DJ, van Palenstein Helderman WH, Creugers NH et al (1999) The shortened dental arch concept and its implications for oral health care. Community Dent Oral Epidemiol 27:249–258
Beumer J, Curtis TA, Morrish RB (1976) Radiation complications in edentulous patients. J Prosthet Dent 36:193–203
Elbrecht, A (ed) (1937) Systematik der abnehmbaren partiellen Prothese. Hermann Meusser, Leipzig pp 123–128. German
Luthardt R, Spieckermann J, Böning K et al (2000) Therapie der verkürzten Zahnreihe – eine systematische Literaturübersicht. Dtsch Zahnärztl Z 55:592–609 German
Bonan PR, Lopes MA, Pires FR et al (2006) Dental management of low socioeconomic level patients before radiotherapy of the head and neck with special emphasis on the prevention of osteoradionecrosis. Braz Dent J 17:336–342
Turner CR (1907) The dental mechanism; its structures, functions, and relations. Changes in the jaws following the loss of teeth. In: Turner CR (ed) The American text-book of prosthetic dentistry. Henry Kimpton, London, pp 230–292
Palmqvist S, Carlsson GE, Owall B (2003) The combination syndrome: a literature review. J Prosthet Dent 90:270–275
Jorge JH, Quishida CC, Vergani CE et al (2012) Clinical evaluation of failures in removable partial dentures. J Oral Sci 54:337–342
Martori E, Ayuso-Montero R, Martinez-Gomis J et al (2014) Risk factors for denture-related oral mucosal lesions in a geriatric population. J Prosthet Dent 111:273–279
Schwartz HC, Kagan AR (2002) Osteoradionecrosis of the mandible: scientific basis for clinical staging. Am J Clin Oncol 25:168–171
Støre G, Boysen M (2000) Mandibular osteoradionecrosis: clinical behaviour and diagnostic aspects. Clin Otolaryngol Allied Sci 25:378–384
Glanzmann C, Gratz KW (1995) Radionecrosis of the mandibula: a retrospective analysis of the incidence and risk factors. Radiother Oncol 36:94–100
Ziegler A, Lange S, Bender R (2007) Überlebenszeitanalyse: Die Cox Regression. Dtsch Med Wochenschr 132:42–44 German
Poole C (2001) Low p-values or narrow confidence intervals: which are more durable? Epidemiology 12:291–294
Parliament M, Alidrisi M, Munroe M et al (2005) Implications of radiation dosimetry of the mandible in patients with carcinomas of the oral cavity and nasopharynx treated with intensity modulated radiation therapy. Int J Oral Maxillofac Surg 34:114–121
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Funding
The work was not supported by any financial assistance.
Ethical approval
The study protocols were approved by the medical faculty’s ethics committee at the Martin-Luther-University Halle-Wittenberg and conducted in accordance with the Declaration of Helsinki on Ethical Principles for Medical Research.
Informed consent
For this type of study, formal consent is not required.
Rights and permissions
About this article
Cite this article
Schweyen, R., Stang, A., Wienke, A. et al. The influence of dental treatment on the development of osteoradionecrosis after radiotherapy by modern irradiation techniques. Clin Oral Invest 21, 2499–2508 (2017). https://doi.org/10.1007/s00784-017-2048-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-017-2048-8