Abstract
Objectives
The aim of this study was to evaluate the effect of resin coating on the wear depth of highly viscous glass ionomer cements (HVGICs) after 40,000 cycles, corresponding to over 8 years of tooth brushing.
Materials and methods
A resin composite (Gradia Direct Posterior), two HVGICs (EQUIA Fil and Riva Self Cure), a resin coating (EQUIA Coat) and a conventional varnish (Fuji Varnish) were used in the study. The control groups were the resin composite group and the non-coated HVGICs groups. Samples (n = 8) were produced in flat plastic moulds at 23 ± 1 °C and stored in artificial saliva sodium acetate-acetic acid-glycerine formalin (SAGF medium) for 7 days at 37 ± 1 °C. The abrasion test was carried out in a toothbrush simulator (Willytec) with a load of 1 N using abrasive toothpaste slurry. Vertical loss was measured at different cycles under confocal laser scanning microscopy (CLSM). Data were analysed using one-way ANOVA, Tukey’s HSD test, repeated measures ANOVA and Bonferroni tests (p < 0.05).
Results
The resin composite group showed significantly lower vertical wear loss than the non-coated groups and the varnished groups of HVGICs (p < 0.05). HVGICs with resin coating had better wear resistance than the varnished and non-coated groups (p < 0.05). Furthermore, regarding the material-based wear, HVGICs with resin coatings abraded less than the resin composite group tested (Gradia Direct Posterior 5.06 ± 0.54 μm, EQUIA Fil 4.06 ± 1.68 μm, Riva Self Cure 4.73 ± 2.44 μm), but statistically, there were no significant differences between them after 40,000 cycles (p > 0.05). After 40,000 cycles, when the total wear loss of the materials including both coatings wear was compared, there were no differences between the non-coated and the resin-coated groups.
Conclusions
The results of this study indicate that the resin coating protects the glass ionomer materials from excessive wear until 20,000 cycles making both HVGICs to abrade in a similar manner as the resin composite. If we include the wear of the coating to the general material wear loss at 40,000 cycles, the total wear loss is quite similar for all HVGICs, regardless of the protection with varnish or resin coating.
Clinical relevance
Within the limitation of this study, we have foreseen that resin coating will protect and make the HVGIC materials as wear resistant as resin composites in clinical situations for a long time.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Modern restorative dentistry concepts focus on minimally invasive approaches to dental hard tissue removal and the remineralisation effects of restorative materials [1]. Chemical adhesion to tooth structures, remineralisation, caries prevention effects due to fluoride release, thermal expansion similar to tooth structures, biocompatibility and low toxicity have made glass ionomer cements (GICs) a clinically preferred restorative material compared to resin composites [2, 3]. Contrary to their many advantages, they also have lower mechanical and physical properties, such as low fracture strength, toughness and wear resistance, and they are very much affected by initial moisture contamination and dehydration [4]. Since their first introduction in the market and during many years, because of these drawbacks, GICs were considered only as semi-permanent dental material for posterior restorations. However, in recent years, encapsulated highly viscous GICs (HVGICs) having improved mechanical properties compared to conventional GICs have been developed [5–7]. Distinctively from their hand-mixing equivalents, encapsulation provides uniform proportioning and mixing under a standard mixing technique, time for clinical applications and less porosities [6].
During the setting process of GICs, water acts as a key factor for maturation [8]. Both moisture contamination and dehydration negatively affect the mechanical properties of GIC restorations during the initial maturation step [9]. Contamination by moisture decreases the mechanical toughness of the restoration and its wear resistance [10], while dehydration causes cracks on the surfaces of restorations [11]. To overcome these problems, the restoration must be protected during the initial setting stage [12]. A variety of surface coatings were proposed for isolating GIC restorations, including copal varnish, cocoa butter, Vaseline®, waterproof varnishes and glazes [13]. It is presumed that this layer will prevent the restoration from dehydration and maintain the water balance in the system. Following these suggestions, light-cured resin coatings were introduced to dental practice [14, 15]. A few years ago, restorative GIC systems combining encapsulated HVGICs and nano-filled resin coatings were launched into the market [16]. The manufacturer claimed that the nano-filled resin coating would improve the mechanical properties, wear resistance and surface appearance of the glass ionomer material [16, 17]. Moreover, these resin-coatings could adhere to tooth structures as well as other restorative materials, and the longer they will stay in contact with the restoration, the smaller the chance that the mechanical properties of the materials will decrease [18]. The first long-term clinical trials of 4 and 6 years with this system seem to be very promising [19; Turkun and Kanik, manuscript in preparation]. However, the nano-filled resin coating wears from the restoration surface with the effects of mastication, diet and tooth brushing in approximately 6 months [15], but recoating is not required after this period, as the proper maturation of the material is completed until that time [20].
Wear of dental restorative materials is one of the main concerns in long-term clinical success. It can be defined as a loss of anatomic contour, which occurs on dental hard tissues and restorations. In conjunction with current technological advances, wear on dental materials occurs on occlusal contact areas rather than contact-free areas. Regarding materials, we can say that GICs exhibit a wear rate five times higher than amalgam and three times higher than resin composite materials [21] and their reputation did not change many, and they are still considered as semi-permanent restorative material for small to moderate class I and II fillings in permanent teeth [22]. Dental hard tissue and restorative dental material losses are caused by several mechanisms. However, wear tests are based mainly on attrition depending on two-body interactions and abrasion caused by three-body interactions [23]. Simulating oral conditions is the main goal of in vitro wear tests. For years, toothbrush abrasion tests with or without toothpaste slurry and machine-driven wear tests like the ACTA machine have been widely used for investigating the wear of dental materials [24].
In recent decades, however, it has been found that an objective wear qualification method providing numeric values may also be needed in addition to a well-designed wear protocol. The best qualification method for wear tests has been found to be the three-dimensional (3D) imaging. Contact profilers, non-contact white light or laser scanners, and micro- or cone computed tomography (CT) scanners are among 3D wear qualification methods that are used in the research field today [23]. Moreover, they provide storable 3D databases that can be compared, and it is applicable to both the clinic and the laboratory [25]. However, this method also has disadvantages, including the need for specialised hardware and software, as well as associated costs. Due to all these disadvantages, until today, there are only a limited number of wear studies implementing this technology. In our opinion, when their costs decrease in a few years’ time, the use of these methods will become widespread.
One of these abrasion test devices providing high-quality focused optical 3D images is the confocal laser scanning microscopy (CLSM). In this technique, a computer is used to reconstruct 3D objects from point-by-point images. It can be used for surface profiling on opaque specimens and for imaging interior structures on non-opaque ones. The image quality of interior imaging is higher than that of simple microscopy, as a confocal microscope permits imaging of different levels, as opposed to the conventional imaging of simple microscopes limited by light penetration. Moreover, confocal microscopy allows intact, thick, living specimens to be sectioned optically in a direct and non-invasive manner [26].
Aim of the study
Based on the lack in the literature about the comparison of the effect of nano-filled resin coatings on the wear resistance of HVGICs compared to resin composites, the aim of the present study was to determine the toothbrush abrasion resistance of two encapsulated HVGICs covered with resin or varnish coatings in comparison to a resin composite using the CLSM method. The null hypothesis tested was that the nano-filled resin-coated groups would wear similarly to the resin composite group.
Materials and methods
Materials and instruments
Two HVGICs—EQUIA Fil (GC Europe, Leuven, Belgium) and Riva Self Cure (SDI, Bayswater, Australia)—were used as the main materials, and Gradia Direct Posterior (GC Europe) was used as the control. The composition, shade and batch numbers of the restorative materials used in the study are listed in Table 1. EQUIA Coat (GC Europe), a nano-filled resin coating, and GC Fuji Varnish (GC Europe), a classical varnish, were used to coat the sample surfaces; the vertical loss on the surface of the material was tested with a three-body toothbrush abrasion method at different cycle periods. A total of seven groups were studied: a positive control group (resin composite), two negative control groups (non-coated HVGIC groups), two resin-coated HVGIC groups and two varnished HVGIC groups. The abbreviations of the materials and the groups are listed in Table 2.
Preparation of samples
The samples were prepared according to the technical standards of ISO/TS 14569–1 [27] and ISO/FDIS 9917–1 [28] (n = 8) in a flat plastic mould (15-mm length × 7-mm width × 2-mm depth) at 23 ± 1 °C and stored in SAGF medium artificial saliva for 7 days before testing. The composition of SAGF medium is listed in Table 3. The resin composite sample was applied in the mould, covered with a polyester strip to flatten the surface and polymerised with a halogen-curing unit (Elipar TriLight; 3M ESPE, Seefeld, Germany) at 750 mW/cm2 for 80 s overlapping the surfaces due to the wideness of the sample surface.
All encapsulated HVGIC capsules were activated with a capsule applier first, then mixed (Silvermix90; GC Europe) for 10 s and placed into the moulds with the capsule applier according to the manufacturers’ instructions. Each sample from the non-coated group was covered with a polyester strip with slight pressure and stored for 3 min for initial maturation. Then, the samples were stored in SAGF medium for 7 days as well.
In addition to the preparation steps of the non-coated samples, the resin-coated and varnished samples were stored for 7 min in SAGF medium to simulate the clinical conditions while the occlusion is adjusted and the patient is closing his mouth before the application of the resin coating or varnish on the upper surfaces of the samples. A colour pigment (0.01 ‰ Rhodamine B isothiocyanate; Merck, Darmstadt, Germany) was added to the resin coating and the varnish to make them more visible for further analysis [15]. The varnish was applied on the samples, and it was waited 2 min until they get dry. The sample surfaces with resin coatings were polymerised for 40 s with a halogen-curing unit (Elipar TriLight; 3M ESPE, Seefeld, Germany) at 750 mW/cm2 due to the large surface area of the samples.
Then, all samples were left in artificial saliva for 7 days. The examination between fractured and finished interface sections of HVGIC and the resin coating thicknesses were evaluated with scanning electron microscopy (SEM) (Leitz ISI SR 50, Akashi, Japan). The finishing procedure of the selected specimens was performed using 1200-grit SiC paper under water. Then, the specimens were dried and gold sputtered under high vacuum. The SEM observation was operated under 20-kVa acceleration voltage with backscatter electron mode for improving the surface contrast. Resin coating thicknesses were measured from three different parts of randomly selected three samples of each resin-coated group of the HVGICs.
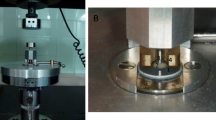
After the waiting period, the samples were embedded in epoxy resin (Technovit 4071; Heraeus Kulzer GmbH, Wehrheim, Germany) the day before testing and polished flat with 1000-grit silicon carbide paper under constant water cooling. Once polished, half of each resin composite and non-coated sample was covered with one-sided adhesive tape. As the resin coatings and varnishes were removed from the surfaces due to the polishing procedures, three quarters of the upper surfaces of the samples were recoated and re-varnished. Then, half of the surfaces of these samples were also covered with one-sided adhesive tape (Fig. 1) to protect them from abrasion and to create a reference surface. This procedure provided the opportunity to measure the thicknesses of the resin coatings and the varnishes as well.
A two-axis toothbrush abrasion testing machine (Willytec GmbH, Gräfelfing, Germany) and a computer-controlled (Controller C 1421; CNC Software, Germany) stepping motor were used together for the toothbrush abrasion experiment. Four parallel steel arms with toothbrush holders were fastened to the top of the two-axis table to enable vertical and horizontal movements of the toothbrushes. One toothbrush head (Oral B P-35, conic tip bristles, bristle Ø = 190 μm) was screwed to each arm, and 100-g brass weights (equal to 1 N of force) simulating the pressure of the patient during tooth brushing were mounted over the head of each arm. The samples were fixed in plastic containers with cylindrical steel sample holders. Enough toothpaste slurry (described below) was placed in the containers to sufficiently cover the samples. The slurry was refreshed each day of the experiment to prevent sedimentation. Brushing frequency, linear and diagonal brushing distances and cycle numbers were programmed through the software controls. A figure-eight brushing path was selected, with a linear brushing distance of 20 mm and a diagonal brushing distance of 2 mm. The brushing frequency was set at 1.25 Hz for 40,000 cycles, resulting in a total of 10 h of brushing. Four samples could be tested at the same time.
The toothpaste slurry used as the abrasive medium was mixed with a magnetic mixer until a 1000 g homogeneous mixture was obtained. Commercial toothpaste (Elmex; Gaba, Karlsruhe, Germany) was used as the compound of the slurry (500 g), a 6.24-g concentration of a complex polysaccharide macromolecule (tragacanth E413; Merck, Germany) was used as an emulsifying agent and stabiliser, and glycerine (246.88 g) and deionised water (246.88 g) were used based on ISO 11609 standards [29].
In the study, it was assumed that individuals brush their teeth twice a day for an average of 2 min. There were a total of four quadrants with three surfaces of teeth to be brushed. As a toothbrush length will cover approximately three to four teeth at the same time, each quadrant could be brushed in two parts. Then, it was reasonable to assume that a 10-s abrasion on each tooth surface would effectively represent one person’s daily tooth brushing habits. The toothbrush abrasion test mechanism, based on a 1.25-Hz frequency for 10,000 cycles, was equivalent to 8000 s of abrasion. According to this data, 10,000 cycles was calculated to be equivalent to 800 days (∼2 years) of brushing. Therefore, the wear of the samples was measured four times: at 2500- (∼6 -month brushing time), 7500- (∼18-month brushing time), 20,000- (∼4-year brushing time) and 40,000-cycle periods (∼8-year brushing time).
Test procedure
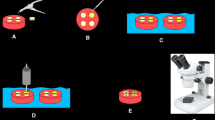
At 2500; 7500; 20,000; and 40,000 cycles, the samples were removed from the machine, the adhesive tape was peeled from the surfaces, and the samples were rinsed under running water. Then, duplicate models were prepared with polyvinyl siloxane impression material (Panasil Light; Kettenbach, Germany) and polyurethane replica material (AlphaDie Top; Schütz Dental, Rosbach, Germany). After that, the one-sided adhesive tape was replaced in the same position under ×10 magnification with a light microscope, and the samples were again fixed in their containers. The abrasion depths of the duplicate models were evaluated with CLSM (TCS SP2; Leica, Bensheim, Germany) in ×10 reflectance mode (488-nm wavelength).
The CLSM technique practically obtains a focal depth, which is controlled and highly limited. An objective lens focuses a laser beam, sent through the aperture of a light source, onto the surface of the specimen [26]. Reflected laser light and fluorescent light emitted from the focal point are reflected back through the objective lens. A beam splitter into the detection equipment, which blocks the original wavelength and permits fluorescent wavelengths by means of a filter, separates part of the light. Intensity of the light that passes through a pinhole is determined by a photo detection device, which converts the light into an electrical signal for a computer to record [30]. The detector aperture blocks light that is not emitted from the focal point. The pinhole blocks most of the returning light, thus yielding sharper images than conventional fluorescence microscopy techniques. The light emitted by an illuminated spot on the specimen creates each pixel of the image. When an image is obtained as the laser scans a surface, pixels in the image correspond to detected light intensity. The laser beam is scanned horizontally by means of oscillating mirrors.
A randomly selected 1.5 × 1.5-mm2 section on the borderline of the covered surface and the abraded surface was evaluated from each duplicate at every cycle period. The Leica Application Suite (LAS) (Leica, Bensheim, Germany) software was used for that purpose. The vertical wear loss of the duplicates was calculated with the software as the height difference between the highest and the deepest points in the graphic (Fig. 2). The mean of three measurements from different parts of the section of each duplicate was recorded.
Statistical analysis
The SPSS 18.0 (SPSS, Chicago, IL, USA) software program was used for the statistical analysis of the data. One-way ANOVA and Tukey’s HSD tests were used to determine the differences between the groups. Repeated measures ANOVA and Bonferroni tests were also applied to determine the differences between cycle periods at a 0.05 significance level.
Results
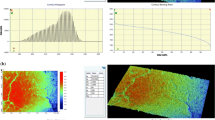
SEM analysis showed that the mean thickness of the resin coatings applied on HVGICs was 5 to 10 μm, depending on the tested samples. As the application procedure of the resin coating was without air blowing, the variation in thickness of this layer was expected (Fig. 3).
The mean values (in μm) and standard deviations of the wear loss of the tested groups with increasing cycle periods and the total wear loss including the coatings at 40,000 cycles are shown in Table 4.
Three-dimensional topographic CLSM images were evaluated for each specimen at various cycle periods. The vertical wear losses were measured on graphic profiles (Fig. 4). Repeated measures ANOVA and Bonferroni test results of wear depth for each group revealed significant paired differences among the various cycles at the 0.5 level. The surface varnishes of the EQUIA Fil and Riva Self Cure groups were totally abraded at 2500 cycles. Despite that result, the resin coatings of the EQUIA Fil and Riva Self Cure groups were still on the surface after 20,000 cycles.
The restorative material-based abrasion depths of the tested resin composite (5.06 ± 0.54 μm) and resin-coated groups (RE 4.06 ± 1.68 μm and RR 4.73 ± 2.44 μm) were found less than the half of the wear loss produced by the non-coated HVGIC groups (NE 10.26 ± 1.74 μm and NR 10.75 ± 2.11 μm) at the end of the 40,000 cycles (p < 0.05). Similarly, the second highest restorative material-based wear losses occurred in the varnished HVGIC groups (VE 9.08 ± 1.70 μm and VR 8.15 ± 0.55 μm). Therefore, the wear resistance of the varnished and non-coated HVGIC groups was significantly weaker than that of the control resin composite and the resin-coated HVGIC groups (p < 0.05).
Due to the protection of the resin coating, the HVGIC materials with resin coatings abraded less than the resin composite group tested (RE 4.06 ± 1.68 μm and RR 4.73 ± 2.44 μm). However, there were no significant differences between the statistical data of the resin-coated HVGIC and the resin composite groups. The null hypothesis tested was that the resin-coated groups would wear similarly to the resin composite tested was then accepted. Furthermore, the resin-coated HVGIC groups showed significantly higher wear resistance rate compared to all the other HVGIC groups at 40,000 cycles (p < 0.05). If we include the wear of the coatings to the general material wear loss at 40,000 cycles, the total wear loss is quite similar for all HVGICs, regardless of the protection with varnish or resin coating.
Discussion
Abrasive wear is defined as a progressive loss of material caused by a solid surface or some abrasive particles harder than the wearing solid surface [31]. Size, shape and type of abrasive particles; applied surface pressure; type of pressure; and the properties of the wearing surface are some of the conditions that may affect this process [32]. Material loss due to abrasive particles occurs by four different mechanisms: micro-cutting, microfracture, pull-out of individual grains and accelerated fatigue by repeated deformations. Two-body and three-body abrasive wear tests are two major types of abrasive wear that may occur in dental materials [32].
In the three-body wear test, hard free-particles roll and slide between two solid surfaces. The wear mechanisms of three-body abrasive wear are not totally known, but abrasive and fatigue wears seemed to have key roles [23]. In contrast to two-body wear, higher wear loss values are obtained in the three-body wear test due to the higher surface pressures applied. As three-body wear test was an easier, time-saving and cheaper abrasion test method, we decided to use this wear test with toothpaste slurry in our study.
The evaluation of wear by measuring the weight loss of materials [33, 34] and SEM observations [35] are commonly used techniques in wear studies. Recently, CLSM measurements were also used because they are more objective and time saving than the other techniques due to 3D computerised imaging [15, 36]. The CLSM method, which permits variable scanning speeds, often has low reaction latency. Slower scans have higher contrasts and resolutions due to a higher signal to noise ratio. The microscope stage or objective lens can be raised or lowered to obtain data from different levels. Certain software can be used to create 3D or 2D images using stacks composed of successive slices [25]. In order to increase the visibility of selected objects, fluorescent dyes can be used, in low concentrations, to treat biological samples without causing disturbances [30].
Different toothbrush simulator designs have been used in previous studies. However, there has been no consensus regarding the standard for toothbrush abrasion tests in terms of setting the parameters and applications for simulating oral conditions. Vertical loads of 1–3 N or 100–400 gf at different numbers of cycles had been used successfully in previous studies [35, 36] as an average applied force by a patient while tooth brushing. As a result, 100-g brass weights equal to a vertical load of 1 N were used in this study as a relevant parameter. Specimen weight losses have typically been used for measuring the two-body wear of restorative materials and tooth hard tissues in most studies [34, 35, 37]. Only few studies have been conducted on three-body wear depth measuring techniques of restorative materials, especially for conventional GICs; therefore, it is difficult to compare our results with those of other studies. However, we can say that our wear results follow the overall trend previously described in the literature.
The application of coatings is a common protective approach for GICs. In particular, resin coatings are effective in reducing the initial water contamination that plays a key role in the maturation and improvement of the mechanical durability of the material. Although nail varnishes have provided the best results in some studies [38, 39], the presence of toluene, a harmful component of nail varnish, is a valid reason to prefer resin coatings in clinical situations [38]. SEM observations in previous studies have shown the average thicknesses of different resin coatings without the use of air-blowing to be 6–12 μm [34], 13.8–17.2 μm [36] and 40–70 μm [15], depending of the product that had been used and the number of its applications. In this study, the average thickness of the one-coat resin coating Equia Coat was measured with SEM and was found to be 5 to 10 μm depending on the samples. Education in dental practice produces dexterity, and increased dental experience improves the handling abilities of clinicians influencing the obtained coating thicknesses. Moreover, one should keep in mind that the viscosity of the resin used and the number of applications would play a key role in the thickness of this layer. Therefore, the handling sensitivity of researchers based on whether or not they are clinicians could have an effect on these extreme differences in average thicknesses observed in previous studies.
The resin coating layer is not only protecting the GICs from initial water contamination but also aiming to improve their physical properties and wear resistance as well. In 2011, Lohbauer et al. [15] made an in vitro study to compare the effect of a resin coating, G-Coat Plus, on the three-point fracture strength (FS) and three-body wear of Fuji IX GP Extra GIC. According to their findings, it is needed to resin coat the GIC surface to improve its mechanical strength and wear resistance. Similarly, a year later, Bonifacio et al. [40] measured the FS and wear of coated vs uncoated Fuji IX GP Extra specimens and concluded that the resin coating improved the FS and wear resistance of the GIC tested. More recently, Diem et al. [41] conducted an in vivo study with the ART technique in field conditions comparing EquiaFil with and without coating (Equia Coat) to a resin composite. After 3 years, they concluded that EquiaFil, regardless of the coating application, showed acceptable clinical performance compared to the tested resin composite. However, even if the difference was not relevant in clinical situations, according to the cast obtained from these restorations, the application of Equia Coat was found beneficial in reducing the wear of this GIC clinically in class I restorations.
Until today, many in vitro studies have been performed in order to evaluate the influence of different resin coatings on the abrasion wear rate of GICs. In 2013, Gando et al. [35] abraded samples of resin-coated bovine incisor dentin surface in toothpaste slurry at 1.66 Hz with 300-gf surface pressure and measured an average abrasion depth of 4–6 μm for two different resin coatings (Shield Force; Tokuyama Dental, Tokyo, Japan and Hybrid Coat; Sun Medical, Moriyama, Japan) with SEM observations at 20,000 cycles. In our study, 100 gf of surface pressure was applied at a frequency of 1.25 Hz. As the resin coating was still on the surface of the samples at the end of 20,000 tooth brushing cycles, the average abrasion depth of EQUIA Coat was measured as 3.76 ± 0.41 μm for EQUIA Fil and 4.21 ± 0.29 μm for Riva Self Cure. Even different resin coatings were evaluated in Gando et al.’s study, we can still say that the abrasion depth results of EQUIA Coat were in the same range as the other resin-based coatings tested.
In another study performed by Belli at al. [36], the wear losses of one flowable hybrid resin composite and two conventional and eight self-adhesive resin cements were evaluated with the ACTA machine and a toothbrush abrasion test with toothpaste slurry at 1.25 Hz with a load of 100 gf (1 N). Even if the study was not recent, the parameters of the toothbrush abrasion test and the CLSM technique used to evaluate the wear depth of the materials were similar to our study. They found an abrasion depth of 2.44–8.70 μm for all tested groups at 20,000 cycles of tooth brushing. The value of 3.83 ± 1.65 μm was obtained for the tested flowable hybrid resin composite samples. In our study, at 20,000-cycle periods, the average wear loss values of non-coated HVGICs were found to be 5.10 ± 0.79 μm for EQUIA Fil and 5.27 ± 0.83 μm for Riva Self Cure, and the mean wear depth of the resin composite Gradia Direct Posterior was found 2.53 ± 0.20 μm. As all the testing conditions were the same (pressure force, frequency, toothpaste slurry and type of machine used for toothbrush abrasion), the results of our study were in the same range as the results of Belli et al.’s study.
Bonifacio et al. [40] conducted a three-body wear test with the ACTA machine using two different HVGICs (Fuji IX GP eXtra and Ketac Molar Applicap) and a light-cured resin coating (G-Coat PLUS). They tested non-coated and resin-coated groups at the end of the first and fourth days of storage at 200,000-cycle periods. After the storage times were completed, the non-coated Fuji IX GP eXtra samples (day 1, 93 μm; day 4, 70 μm) were significantly more abraded than the tested resin-coated Fuji IX GP eXtra samples were (day 1, 54 μm; day 4, 46 μm). The results of our three-body wear test were comparable with those of Bonifacio et al.’s ACTA test for Fuji IX GP eXtra (now called as EQUIA Fil).
To see the comparison of the wear rates between resin-coated and non-coated groups is important in order to observe the effect of these coatings on direct restorative glass ionomers. As the average abrasion depth of the resin composite tested was half that of the non-coated groups and almost the same as that of the resin-coated encapsulated HVGIC groups, the surface protection provided by EQUIA Coat seems to benefit encapsulated HVGICs in terms of wear. However, the results of short-term and long-term clinical studies on reinforced encapsulated HVGICs and resin-coating combinations would be beneficial for identifying the clinical performance and the limits of the HVGICs, as the results of in vivo and in vitro studies may differ.
Conclusion
Within the limitations of this study, we can say that the chemically cured classical varnish GC Fuji Varnish provided a negligible contribution to the wear potential of HVGICs. However, the application of the resin coating EQUIA Coat had a significant protective effect on the wear resistance of EQUIA Fil and Riva Self Cure until 20,000 cycles. Since the wear of this resin coating is less than that of HVGICs, the overall material loss is consequently lower making the tested GICs as wear resistant as the resin composite Gradia Direct Posterior tested after a wear simulation testing period corresponding to 8 years of wear. However, if we consider the total wear loss including the thickness of the coatings as well, the wear results were similar in both HVGISs regardless of the coatings applied.
References
Murdoch-Kınch C, Mclean ME (2003) Minimally invasive dentistry. J Am Dent Assoc 134:87–95
Mousavinasab M, Meyers I (2009) Fluoride release and uptake by glass ionomer cements, compomers and giomers. J Biol Sci 4:609–616
Kleverlaan CJ, Duinen RNB, Feilzer AJ (2004) Mechanical properties of glass ionomer cements affected by curing methods. Dent Mater 20:45–50
Lohbauer U (2010) Dental glass ionomer cements as permanent filling materials? – properties, limitations and future trends. Materials 3:76–96
Fleming GJP, Kenny SM, Barralet JE (2006) The optimisation of the initial viscosity of an encapsulated glass-ionomer restorative following different mechanical mixing regimes. J Dent 34:155–163
Dowling AH, Fleming GJP (2009) Are encapsulated anterior glass-ionomer restoratives better than their hand-mixed equivalents. J Dent 37:133–140
Torabzadeh H, Ghasemi A, Shakeri S, Baghban AA, Razmavar S (2011) Effect of powder/liquid ratio of glass ionomer cements on flexural and shear bond strengths to dentin. Braz J Oral Sci 10:204–207
Nicholson JW (2010) Review: glass ionomer dental cements: update. J Mater Tech 25:8–13
Nicholson JW, Amiri MA (1998) The interaction of dental cements with aqueous solutions of varying pH. J Mater Sci Mater Med 9:549–554
Gemalmaz D, Yoruc B, Ozcan M, Alkumru HN (1998) Effect of early water contact on solubility of glass ionomer luting cements. J Prosthet Dent 80:474–478
Nicholson JW, Czarnecka B (2008) Kinetic studies of water uptake and loss in glass ionomer cements. J Mater Sci Mater Med 19:1723–1727
Miyazaki M, Moore BK, Onose H (1996) Effect of surface coatings on flexural properties of glass ionomers. Eur J Oral Sci 104:600–604
Council on Dental Materials, Instruments and Equipment (1990) Using glass ionomers. J Am Dent Assoc 121:181–188
Kato K, Yarimizu H, Nakaseko H, Sakuma T (2008) Influence of coating material on conventional glass-ionomer cement. J Dent Res Abstr. No. 0487
Lohbauer U, Kramer N, Siedeschlag G, Schubert EW, Laurer B, Müller FA, Petschelt A, Ebert J (2011) Strength and wear resistance of a dental glass ionomer cement with a novel nanofilled resin coating. Am J Dent 24:124–128
http://www.gcamerica.com/products/operatory/equia/GCA_EQUIA_Brochure.pdf. Accessed 16 Dec 2015
http://www.voco.com/en/products/_products/easy_glaze/VC_8400_1016_GB_0710.pdf. Accessed 16 Dec 2015
Marquezan M, Osorio R, Ciamponi AL, Toledano M (2010) Resistance to degradation of bonded restorations to simulate caries-affected primary dentin. Am J of Dent 23:47–52
Gurgan S, Kutuk ZB, Ergin E, Oztas ZZ, Cakir FY (2015) Four-year randomized clinical trial to evaluate the clinical performance of a glass ionomer restorative system. Oper Dent 40:134–143
Sidhu SK (2011) Glass-ionomer cement restorative materials: a sticky subject? Austr Dent J 56(1 Suppl):23–30
Kunzelmann KH (1996) Glass-ionomer cements, cermet cements, hybrid-glass-ionomers and compomers—laboratory trials—wear resistance in: Dash W, Watt DC (eds) Clinically appropriate alternatives to amalgam: biophysical factors in decision making. Chicago: Trans Academic Dental Materials 9:89–104
Frankenberger R, Garcia-Godoy F, & Kramer N (2009) Clinical performance of viscous glass ionomer cement in posterior cavities over two years. Int J of Dent Article 2009:1–7. doi:10.1155/2009/781462
DeLong R (2006) Intra-oral restorative materials wear: rethinking the current approaches: how to measure wear. Dent Mater 22:702–711
Kunzelmann KH, Bürkle V, Bauer C (2003) Two-body and three-body wear of glass ionomer cements. Int J Paediatr Dent 13:434–440
Perry R, Kugel G, Kunzelmann KH, Flessa HP, Estefan D (2000) Composite restoration wear analysis: conventional methods vs. three dimensional laser digitizer. J Am Dent Assoc 131:1472–1477
Pawley JB (2006) Handbook of biological confocal microscopy (3rd ed.). Springer, Berlin
ISO/TR 14569-1:2007 Dental materials -- Guidance on testing of wear -- Part 1: Wear by toothbrushing
ISO 9917-1:2007 Dentistry-Water based cements-Part 1: powder/liquid acid-base cements
ISO 11609:2010 Dentistry -- Dentifrices -- Requirements, test methods and marking
Claxton NS, Fellers TJ, Davidson MW (2006) Laser scanning confocal microscopy, Department of Optical Microscopy and Digital Imaging, National High Magnetic Field Laboratory, Florida State University, p 37 Unpublished (http://www.olympusfluoview.com/theory/LSCMIntro.pdf)
Jiaa X, Lingb R (2007) Two-body free-abrasive wear of polyethylene, nylon 10, epoxy and polyurethane coatings. Tribol Int 40:1276–1283
Jankauskas V, Skirkus R (2013) Steel abrasive wear forecasting by wearing surfaces microgeometric parameters. Mechanika 19:486–490
Eneren ES, Imazato S, Kaneshiro AV, Iwami Y, Ebusi S, Gurgan S (2010) Resistance of surface coating resins against tooth brushing abrasion. Am J Dent 23:70–74
Yap AU, Teoh SH, Hasting GW, Lu CS (1997) Comparative wear ranking of dental restorative materials utilizing different wear simulation models. J Oral Rehabil 24:574–580
Gando I, Ariyoshi M, Ikeda M, Sadr A, Nikaido T, Tagami J (2013) Resistance of dentin coating materials against abrasion by toothbrush. Dent Mater 32:68–74
Belli R, Pelka M, Petschelt A, Lohbauer U (2009) In vitro gap formation of self-adhesive resin cements: a CLSM evaluation. J Dent 37:984–993
Yamamoto T, Otuski H, Nishimoto C, Iwasaki S, Nikaido T, Tagami J (2008) Influence of adhesion on wear-resistance of resin-coating materials against toothbrush-abrasion. AADR Abstr. No. 1047
Fatima N, Ali Abidi SY, Qazi FU, Jat SA (2013) Effectiveness of commonly available surface protecting agents in maintaining microhardness of two cements. J Coll Physicians Surg Pak 23:315–318
Serra MC, Navarro MF, Freitas SF, Carvalho RM, Cury JA, Retief DH (1994) Glass ionomer surface protection. Am J Dent 7:203–206
Bonifacio CC, Werner A, Kleverlaan CJ (2012) Coating glass-ionomer cements with a nanofilled resin. Acta Odontol Scand 70:471–477
Diem VTK, Tyas MJ, Hien CN, Phuong LH, Khanh ND (2014) The effect of a nano-filled resin coating on the 3-year clinical performance of a conventional high-viscosity glass-ionomer cement. Cl Oral Invest 18:753–759
Acknowledgments
The authors would like to thank the GC Europe Corporation and SDI Limited for material and technical support to this study. Furthermore, special thanks are extended to the staff of Dental Clinic 1, School of Dentistry, University of Erlangen-Nuremberg, for technical assistance.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Funding
The Department of Research Projects of Ege University in Izmir, Turkey, supported the work.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
For this type of study, formal consent is not required.
Rights and permissions
About this article
Cite this article
Kanik, Ö., Turkun, L.S. & Dasch, W. In vitro abrasion of resin-coated highly viscous glass ionomer cements: a confocal laser scanning microscopy study. Clin Oral Invest 21, 821–829 (2017). https://doi.org/10.1007/s00784-016-1820-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-016-1820-5