Abstract
Objectives
The aim of this study is to observe the durability of Class II nanohybrid resin composite restorations, placed with two different adhesive systems, in an 8-year follow-up.
Methods
Seventy-eight participants received at random at least two Class II restorations of the ormocer-based nanohybrid resin composite (Ceram X) bonded with either a one-step self-etch adhesive (Xeno III) or a control two-step etch-and-rinse adhesive (Excite). The 165 restorations were evaluated using slightly modified United States Public Health Services (USPHS) criteria at baseline and then yearly during 8 years.
Results
One hundred and fifty-eight restorations were evaluated after 8 years. Three participants with five restorations (three Xeno III, two Excite) were registered as dropouts. Twenty-one failed restorations (13.3 %) were observed during the follow-up. Twelve in the one-step self-etch adhesive group (13.5 %) and nine in the two-step etch-and-rinse group (13.0 %). This resulted in nonsignificant different annual failure rates of 1.69 and 1.63 %, respectively. Fracture of restoration was the main reason for failure.
Conclusion
Good clinical performance was shown during the 8-year evaluation and no significant difference in overall clinical performance between the two adhesives. Fracture was the main reason for failure.
Clinical relevance
The one-step self-etch adhesive showed a good long-term clinical effectiveness in combination with the nanohybrid resin composite in Class II restorations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Over the years, composite resins with different formulations have been introduced. To improve properties of resin composites, the size of the filler particles has been decreased. Many resin composites today belong to the nanocomposites, nanofiller or nanohybrid compositions, which contain filler particles in the range of 0.1–100 nm. The small particles are favourable to obtain a good wear resistance, high fracture toughness, optimum polishability and good aesthetics. They are difficult to wet with resin and are therefore often agglomerated [1, 2]. In a recently developed nanohybrid resin composite (Ceram X; DENTSPLY DeTrey, Konstanz, Germany), organically modified ceramic nanoparticles (2–3 nm) and nanofillers (10 nm) are used combined with conventional glass fillers of Ca 1 μm. The modified ceramic nanoparticles are achieved via controlled hydrolysis and condensation reactions and comprise a polysiloxane backbone. Methacrylic groups are attached to the backbone via silicon-carbon bonds. Nanotechnology is combined with ormocer (organically modified ceramics) technology, by replacing most of the conventional resin matrix by a matrix full of highly dispersed methacrylate-modified polysiloxane particles [2]. In contrast to conventional composites, the ormocer matrix is not only organic but also inorganic. The monomers are better embedded in the matrix what reduces the release of monomers [3, 4]. The inorganic siloxane part provides strength, while the organic methacrylic part makes the particles polymerizable with the resin matrix. In vitro, excellent marginal adaptation to both enamel and dentin has been observed combining the resin composite with a butanol-based etch-and-rinse adhesive [5]. The nanohybrid resin composite is characterized by an intermediate hardness and good flexural and diametral tensile strength but low flexural modulus [6, 7]. Clinically, acceptable short-time survival rates have been observed in a few studies for the ormocer-based nanohybrid [8–10].
Self-etch adhesive systems (SEA) are supposed to make the bonding procedure more user-friendly, eliminating the risk of over-etching and over-drying. The resulting hybrid layer is much thinner compared to that of traditional etch-and-rinse systems; the thickness however depends on its acidity [11, 12]. Due to the high content of hydrolytical components and increased permeability of the SEA hybrid layers, the bonds appear more vulnerable to degradation in the mouth than etch-and-rinse adhesives [13, 14]. Three-step etch-and-rinse adhesives have been considered as the most favourable bonding system, based on predictions by laboratory tests such as tensile or shear bond strength and clinical non-carious cervical lesion (NCCL) studies [15]. However, recent improved clinical results have been reported for several self-etching adhesives in NCCL and posterior restoration studies, mostly over short-time observation periods [9, 10, 16–21]. There is still a lack of long-term evidence. In a recently published randomized prospective short-term study, Class II ormocer-based nanohybrid resin composite restorations placed with a two-component one-step SEA showed a similar durability as restorations performed with a two-step etch-and-rinse system [10]. The aim of this study was to investigate the clinical longevity of the Class II nanohybrid resin composite restorations after 8 years. The hypothesis tested was that restorations performed with a two-component one-step SEA showed similar durability as restorations performed with a two-step etch-and-rinse system.
Material and methods
Experimental design
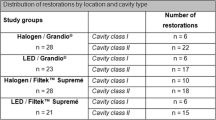
The study design adopted the guidelines and recommendations of CONSORT with regard to the conduction of a randomized clinical trial as far as possible. During November 2004–May 2005, adult patients attending the Dental School Public Dental Health Service clinic in Umeå and a private dental clinic in Copenhagen, who needed two similar Class II restorations, were asked to participate in the follow-up. Female patients who were pregnant or nursing were excluded. No patients were excluded because of caries activity, periodontal condition or parafunctional habits. All patients were informed on the background of the study, which was approved by the ethics committee of the University of Umeå (Dnr 07-152M). Reasons for placement of the resin composite restorations were primary or secondary carious lesions, fracture of old amalgam fillings or replacement because of aesthetic or other reasons. Seventy-eight patients participated, 34 men and 44 women, with a mean age of 52.7 years (range 28–86). One hundred and sixty-five restorations were placed in 61 premolar (24 in male, 37 in female) and 104 molar (38 in male, 66 in female) teeth. All teeth had opposing and adjacent tooth contacts. The distribution and the size of the restorations are given in Table 1.
Operative procedures were performed under local anaesthesia if necessary. Existing restorations and/or caries were removed under constant water cooling. No calcium hydroxide-base material was placed, and no bevels were prepared. The operative field was carefully isolated with cotton rolls and suction device. For all Class II cavities, a thin metallic matrix was used and carefully wedging was performed with wooden wedges (Kerr/Hawe Neos, Switzerland). The cavities were cleaned by a thorough rinsing with water. In order to make an intra-individual comparison possible, all except five patients received at least two restorations. Immediately, after the decision to include an individual pair of teeth in need of restorations in the study, randomization for the two treatments was performed by a coin toss, before preparation of the cavities. The cavities were randomly distributed to be restored with either the experimental combination Xeno III/Ceram X (DENTSPLY DeTrey) or the control restoration with the commercial two-step etch-and-rinse adhesive Excite (Ivoclar Vivadent AG, Schaan, Liechtenstein) followed by the resin composite Ceram X (Table 2). In participants with only one cavity, a Xeno III/Ceram X was placed.
Application of the two adhesive systems was done according to manufacturer’s instructions. The resin composite was then applied in layers of maximal 2 mm with, if possible, an oblique layering technique using selected composite instruments (Hu-Friedy Mfg. Co., Chicago, Ill, USA). Every increment was light cured with a well-controlled LED light unit (SmartLite, DENTSPLY DeTrey) for at least 20 s. The restorations were placed by two experienced operators. After checking the occlusion/articulation and contouring with finishing diamond burs, the final polishing was performed with the Shofu polishing system (Brownie; Shofu Dental Cooperation, Kyoto, Japan) and finishing strips (GC finishing strips; Tokyo, Japan).
Evaluation
Each restoration was evaluated according to slightly modified United States Public Health Services (USPHS) criteria for the following characteristics: anatomical form, marginal adaptation, colour match, marginal discoloration, surface roughness, caries (Table 3) [22]. The restorations were evaluated at baseline and then blindly every year during 8 years by the operators and at regular intervals, 2–4 days/month, by other calibrated evaluators. Radiographs were taken in most cases at the yearly recalls. The caries risk for each patient at baseline was estimated by the treating clinician by means of clinical and socio-demographic information routinely available at the annual clinical examinations, e.g. incipient caries lesions and former caries history [23, 24]. Bruxing activity was estimated as low or high by the treating clinician by means of clinical signs and history at the annual examinations [20]. Any failures during the study were counted as failures during all subsequent recalls. The failure percentage at each recall was the total number of failures to date in the following equation: failure percentage = (previous failures + new failures)/(previous failures + currently recalled restorations) × 100.
Statistical evaluation
The evaluated characteristics of the restorations, including the number of nonacceptable restorations (failures) are described by descriptive statistics by using frequency distributions of the scores. The overall performance of the experimental restorations was tested after intra-individual comparison and ranking using Friedman’s two-way analysis of variance test [25]. Patients with restorations, not belonging to a pair, as decided at the baseline randomization, were included in the descriptive statistics of the scores for the resin composite, but not in the analysis of the intra-individual comparison of the two adhesives. The hypothesis was rejected at the 5 % level.
Results
Postoperative sensitivity, self reported and/or reported after questioning by the authors, was reported for six teeth in six participants between 1 and 3 weeks after baseline, three Xeno III/Ceram X restorations during biting forces and three Excite/Ceram X restorations during biting forces or cold stimuli. At 8 years, 158 restorations, 89 Xeno III/Ceram X and 69 Excite/Ceram X were evaluated. These included 20 restorations which did not belong to a pair. Three patients with five restorations (1 year: one molar, Xeno III; 3 years: one premolar, Xeno III and one molar, Excite; 5 years: one molar, Xeno III and one molar, Excite) could not be evaluated, due to moving (1) and death (2), while another two molar teeth (one Xeno III and one Excite) were extracted at 7 years because of periodontal reasons. These were not included in the final statistical analysis.
Twenty one failed restorations (13.3 %) were observed during the follow-up, 12 Xeno III/Ceram X (13.5 %, four premolar and eight molar teeth) and nine Excite/Ceram X (13.0 %, three premolar and six molar teeth). This resulted in annual failure rates of 1.69 % for the Xeno III/Ceram X group and 1.63 % for the Excite/Ceram X group (ns). The failure rate at 8 years for restorations in premolar teeth was 11.5 % and in molar teeth 14.4 %. A lower failure rate was found in two surface restorations (10.2 %) compared to three or more surface restorations (18.6 %). Male participants showed a higher failure rate (16.1 %) than female (10.7 %).
Reasons and year of failure for the nonacceptable restorations are shown in Table 4. The main reason for failure was resin composite fracture. Small chip fractures were observed in five restorations, which were treated by polishing or left. Male participants showed a higher frequency secondary caries (8.1 %) than female (1.0 %).
A prediction of the caries risk showed that 19 of the patients were considered as risk patients. All except of one of the caries lesions were observed in participants with moderate to high caries risk. Twenty-five of the patients were estimated to have high bruxing activity. Ten of the 16 observed resin composite- and tooth fractures were observed in these participants.
Relative frequencies of the scores (%) for the evaluated variables are given in Table 5. A significant decrease in colour match was observed between baseline and 4 years, which continued slightly during the second half of the follow-up. The colour changes observed were within the acceptable score range, and no significant differences were seen between the bonding groups. Marginal discoloration increased significantly during the follow-up, but within the acceptable scores, no significant difference was observed between the adhesives. The surface characteristics of the nanohybrid resin composite showed no clinical change from the smooth characteristics at baseline to the end of the follow-up.
In the overall intra-individual comparisons between the etch-and-rinse and the self-etching technique, no significant differences were observed at the recalls (p > 0.05).
Discussion
During the years, many new types of promising resin composites have been introduced to overcome disadvantages of traditional materials. The ormocer resin composite materials were developed in the late 1990s showing lower shrinkage, improved wear resistance and high biocompatibility [26, 27]. Ceram X is based on a combination of ormocer and nanofiller technology. It contains methacrylate-modified silicon dioxide-containing nanofiller, while the resin matrix is largely replaced by a matrix of highly dispersed methacrylate-modified polysiloxane particles. Although the material has been on the market for many years, no evidence of its long-time effectiveness has been shown. Also, there is no evidence of which adhesive system is suitable to be used with the material in the long run. The resin composite was therefore tested with two simplified adhesives, a two-step etch-and-rinse and a one-step self-etch system. Like for resin composites, also dental adhesives have shown a continued development and introduction of new materials. Laboratory studies exhibited for a long time favourable results for etch-and-rinse systems compared to self-etch adhesives [28, 29], but newer studies and a review of the recent clinical results of self-etching adhesives showed the effectiveness of certain of these systems [10, 16, 20, 21]. Recently, Van Meerbeek et al. [16] suggested a moderate association between aged bond strength data from the laboratory and clinical retention data from NCCL studies. Bayne [30] on the other hand stated that in vitro laboratory research, although important, had not correlated highly with clinical performance. Therefore, clinical evaluations, especially prospective evaluations, are still the ultimate test of new biomaterials. The clinical effectiveness of adhesives has been assessed clinically mostly in NCCLs [16–20]. The dentin of these lesions, however, does not reflect the substrate in Class II cavities, which most often is influenced by caries and/or amalgam. Adhesive systems need therefore to be tested in load-bearing posterior cavities [20, 31]. A problem of clinical evaluations is that after several years of evaluation plus the time necessary to publish the study in a dental journal, many evaluated materials are withdrawn from the market or modified versions have been marketed. This is probably one of the reasons that most clinical evaluations are short-time studies. In this 8-year follow-up, the studied resin composite is one of the materials which have been on the market for a longer period without large modifications.
In the present 8-year follow-up, seven restorations could not be followed during the study giving a cumulative dropout frequency of 4.2 %. The yearly dropout of 0.5 % is rather low compared to those reported in many clinical follow-ups, including many short-time studies. Despite the fact that nanohybrid composite resins have been used for posterior restorations for several years, its evidence in the literature is still limited [8, 9, 32, 33]. For the investigated Ceram X, a few short-time evaluations between 2 and 4 years have been published. All were showing acceptable short-time effectiveness [8–10, 34]. One of these studies was the 4-year report of the present study observing annual failure rates (AFR) of 1.4 and 1.9 % [10]. Schirrmeister et al. [9] observed two failed restorations of 23 Class II restorations evaluated after 4 years (AFR 2.2 %), with a patient dropout of 37 %. Mahmoud et al. [34] evaluating several resin composite types reported no failures for Ceram X after 3 years, but they only evaluated ten Class II restorations. Monteiro et al. [8] reported one failure of 30 restorations (dropout 12 %) after 2 years resulting in an AFR of 1.7 %. Except for the present study, all other studies used etch-and-rinse adhesives only. The success rate of the Ceram X restorations presented in the above-mentioned studies needs to be considered with regard to the relatively short periods between 2 and 4 years of clinical service.
The AFR observed in the present study is clinically highly acceptable taking into account that no patient selection was performed, only Class II and rather large cavities were included with the majority in molar teeth. Frankenberger et al. [29] reported in a recent 8-year follow-up the effectiveness of 32 Class II Tetric Ceram and 36 Class II Grandio restorations. They used a selected group of young participants with high level of oral hygiene where application of rubber dam had to be possible. All participants attended the 8-year recall. Three Grandio and one Tetric Ceram failures resulted in an AFR of 1.2 and 0.4 %. In a similar design as the present study with a nonselected older patient group, van Dijken and Pallesen [35] found an AFR of 2 % for the same Tetric Ceram. This resin composite has been indicated during many years to be the golden standard between resin composite materials, without direct clinical evidence. Low AFRs, between 0.5 and 0.7 %, were reported by Lindberg et al. [36] in a 9-year follow-up of Class II resin composite restorations placed in mostly enamel-bordered cavities. These failure rates can be compared with the 1.7 % AFR in the present study for all restorations.
Considering the good durability of Class I resin composite restorations observed in long-term clinical evaluations, their inclusion has become questionable in posterior resin composite evaluations [37]. Low numbers of Class II restorations included, combined with high dropout figures, rises therefore problems for the interpretation of the results of many recent randomized studies of nanohybrid and nanofiller resin composites [9, 32, 38–43]. A recent review of these evaluations showed that the mean value of evaluated Class II restorations of ten prospective studies was 18.4 restorations (range 0–36) [10]. The mean number of both Class I and Class II restorations per resin composite evaluated was 32.5 (range 20–45). The low numbers that evaluated Class II restorations in many recent studies are probably too low to give significant clinical information. A number of at least 50 teeth/restorations have been suggested per test group, according to power analysis performed in earlier clinical studies and experience [10]. This number has been confirmed by recently performed sample size estimations in randomized intra-individual comparisons of resin composites and recommendations given by the FDI science committee [44, 45]. Another factor which also influences strongly the outcome of the clinical results is the type of participants selected. This should represent the whole spectrum of patients, who in the future are expected to receive restorations of the materials which have to be evaluated. In contrast to some of the evaluations [42, 43, 46], no patients were excluded in the present study, because of high caries activity, nonacceptable oral hygiene or parafunctional habits. In this way, the sample represents a normal clinical patient population. A high frequency of the failed restorations observed in the present study was observed in high-risk participants concerning both caries and bruxing activity.
The question to be answered in this evaluation concerned the use of adhesive system in combination with the ormocer-based nanohybrid resin composite. Etch-and-rinse or a self-etch adhesive? No significant and clinical difference was found in the 8-year follow-up. An AFR of 1.69 and 1.63 % was observed indicating clearly that adhesives in the self-etching group have been improved and are suitable also in loaded restorations. The hypothesis tested was therefore accepted.
In a review of clinical evaluations of posterior resin composites, Brunthaler et al. [47] stated in 2003 that in Class II cavities, the influence of adhesive system seemed not to influence the long-term results to a significant extent. Manhart et al. observed after 4 years a nonsignificant different 7.5 % failure rate for restorations bonded with Xeno III compared to 2.2 % for the control classic etch-and-rinse adhesive Syntac [41]. Swift et al. [48] compared Xeno III with another etch-and-rinse adhesive (OptiBond Solo Plus) during 3 years in Class I restorations. They observed a 3.3 % failure rate for the SEA not significantly different to the control adhesive. This seemed to be confirmed in a limited number of recently published short-time RCTs which compared the effectiveness of self-etch adhesives versus etch-and-rinse adhesives in posterior cavities [10, 20, 49–51]. Ermis et al. [50] compared during 2 years bonded posterior restorations with the SEA Clearfil SE (n = 43) and the etch-and-rinse Single Bond (n = 44). With a dropout of 24 %, they reported a nonsignificant failure rate for Single Bond of 6 % and for Clearfil SE of 0 %. Boeckel et al. [49] reported a nonsignificant difference after 4 years for restorations bonded with the etch-and-rinse adhesive Excite (0 % failures) and the SEA AdheSE (AFR 0.8 %). The study included 30 Class I and Class II per group while participants with poor oral hygiene and bruxism were excluded. A dropout of 40 % was reported. Higher failure rates were reported by Bottenberg et al. [51] in a 5-year follow-up of Class II restorations bonded with the etch-and-rinse adhesives Admira Bond (n = 22) and Syntac Sprint (n = 26) compared to the SEA Etch&Prime 3.0 (n = 29). Nonsignificant AFRs of 9.1, 5.4 and 4.1 %, respectively, and a dropout of 40 % were reported. van Dijken [20] published a 6-year comparison of Class II restorations, placed in nonselected participants, bonded with a one-step HEMA-free SEA (G-bond, n = 60) and a giomer SEA (FL Bond, n = 55). AFRs at 6 years were 1.4 % for G-Bond and 3.0 % for FL Bond (n. s.; dropout 3.5 %). The shorter follow-up studies comparing SEA with etch-and-rinse systems did not find significant differences between the adhesive systems, which is in accordance with our findings at 8 years.
No significant differences in any of the clinical criteria listed in Table 5 were found between the two adhesive systems tested. The clinical surface characteristics of the resin composite showed a texture similar to enamel, findings also reported in two earlier 4-year follow-ups [9, 10]. In vitro studies showed nonsignificant small differences in roughness values (Ra) for Ceram X compared to other nanohybrid and nanofiller resin composites [7, 52]. After 8 years, the clinical surface texture of the resin composite restoration will probably be determined by the degradation of the surface and participants’ toothbrush-dentifrice properties and their frequency of oral hygiene habits, irrespective of the finishing method used at baseline. The nanohybrid resin composite exhibited a significant colour change during the follow-up which may be related to the water absorption of the material or the structure and characteristics of the filler particles [53]. However, it must be mentioned that the effects were changes within scores 0–2, meaning that they are clinically acceptable. Marginal discoloration increased slightly during the follow-up to less than 20 % of the restorations after 4 years and 30 % after 8 years in most cases of score 1 type.
It can be concluded that the nanohybrid resin composite study showed good clinical effectiveness during the 8-year trial up with a 1.6 % annual failure rate for the Class II restorations. No significant differences were observed in durability between the SEA and the etch-and-rinse adhesive. Fracture of restoration was the main reason of failure. Most failures were observed in risk participants.
References
Saunders SA (2009) Current practicality of nanotechnology in dentistry. Part 1: focus on nanocomposite restoratives and biomimetics. Clin Cosmet Investig Dent 1:47–61
Chen MH (2010) Update on dental nanocomposites. J Dent Res 89:549–560
Polydorou O, König A, Hellwig E, Kümmerer K (2009) Long-term release of monomers from modern dental composite materials. Eur J Oral Sci 117:68–75
Zimmerli B, Strub M, Jeger F, Stadler O, Lussi A (2010) Composite materials: composition, properties and clinical applications. Schweiz Monatsschr Zahnmed 120:972–979
Manhart J, Trumm C (2007) Microleakage of XP Bond in Class II cavities after artificial aging. J Adhes Dent 9:261–264
Ilie N, Hickel R (2009) Investigations on mechanical behaviour of dental composites. Clin Oral Investig 13:427–438
Hahnel S, Henrich A, Bürgers R, Handel G, Rosentritt M (2010) Investigation of mechanical properties of modern dental composites after artificial aging for one year. Oper Dent 35:412–419
Monteiro PM, Manso MC, Gavinha S, Melo P (2010) Two-year clinical evaluation of packable and nanostructured resin-based composites placed with two techniques. JADA 141:319–329
Schirrmeister JF, Huber K, Hellwig E, Hahn P (2009) Four-year evaluation of a resin composite including nanofillers in posterior cavities. J Adhes Dent 11:399–404
van Dijken JWV, Pallesen U (2011) Four-year clinical evaluation of Class II nano-hybrid resin composite restorations bonded with a one-step self-etch and a two-step etch-and-rinse adhesive. J Dent 39:16–25
Van Meerbeek B, Van Landuyt K, De Munck J, Hashimoto M, Peumans M, Lambrechts P, Yoshida Y, Inoue S, Suzuki K (2005) Technique-sensitivity of contemporary adhesives. Dent Mater J 24:1–13
Skupien JA, Susin AH, Angst PDM, Anes R, Machado P, Bortolotto T, Krejci I (2010) Micromorphological effects and the thickness of the hybrid layer—a comparison of current adhesive systems. J Adhes Dent 12:435–442
De Munck J, Van Landuyt K, Peumans M, Poitivin A, Lambrechts P, Braem M, Van Meerbeek B (2005) A critical review of the durability of adhesion to tooth tissue: methods and results. J Dent Res 84:118–132
Tay FR, King NM, Chan KM, Pashley DH (2002) How can nanoleakage occur in self-etching adhesive systems that demineralize and infiltrate simultaneously? J Adhes Dent 4:255–269
Peumans M, Kanumilli P, De Munck J, Van Landuyt K, Lambrechts P, Van Meerbeek B (2005) Clinical effectiveness of contemporary adhesives: a systematic review of current clinical trials. Dent Mater 21:864–881
Van Meerbeek B, Peumans M, Poitivin E, Mine A, Van Ende A, De Munck J (2010) Relationship between bond strength tests and clinical outcomes. Dent Mater 26:e100–e121
van Dijken JWV, Sunnegårdh-Grönberg K, Lindberg A (2007) Clinical long term retention of etch-and-rinse and self-etch adhesive systems in non-carious cervical lesions. A 13 years evaluation. Dent Mater 23:1101–1107
van Dijken JWV, Pallesen U (2008) Long term dentin retention of etch-and-rinse and self-etch adhesives and a resin modified glass ionomer cement in non-carious cervical lesions. Dent Mater 24:915–922
van Dijken JWV (2010) A prospective 8-year evaluation of a mild two-step self-etching adhesive and a heavily filled two-step etch-and-rinse system in non-carious cervical lesions. Dent Mater 26:940–946
van Dijken JWV (2013) A 6-year prospective evaluation of a one-step HEMA-free self etching adhesive in Class II restorations. Dent Mater 29:1116–1122
van Dijken JWV (2013) A randomized controlled 5-year prospective study of two HEMAfree adhesives, a 1-step self etching and a 3-step etch-and-rinse, in non-carious cervical lesions. Dent Mater 29:e271–e280
van Dijken JWV (1986) A clinical evaluation of anterior conventional, microfiller and hybrid composite resin fillings. A six year follow up study. Acta Odontol Scand 44:357–367
Isokangas P, Alanen P, Tiekso J (1993) The clinician’s ability to identify caries risk subjects without saliva tests—a pilot study. Community Dent Oral Epidemiol 21:8–10
Seppä L, Hausen H, Pöllänen L, Helasharju K, Karkkainen S (1989) Past caries recording made in Public Dental Clinics as predictors of caries prevalence in early adolescence. Community Dent Oral Epidemiol 17:277–281
Siegel S (1956) Nonparametric statistics. McGraw-Hill Book Company, Inc, New York, pp 166–172
Fleming GJP, Hall DP, Shortall ACC, Burke FJT (2005) Cuspal movement and microleakage in premolar teeth restored with posterior filling materials of varying reported volumetric shrinkage values. J Dent 33:139–146
Wataha JC, Rueggenberg FA, Lapp CA, Lewis JB, Lockwood PE, Ergie JW, Bettenburg DJ (1999) In vitro cytotoxicity of resin-containing restorative materials after aging in artificial saliva. Clin Oral Investig 3:144–149
De Munck J, Van Meerbeek B, Yoshida Y, Inou S, Suzuki K, Lambrechts P (2003) Four-year water degradation of total etch adhesives bonded to dentin. J Dent Res 82:136–140
Frankenberger R, Tay FR (2005) Self-etch vs etch-and-rinse adhesives: effect of thermo-mechanical fatigue loading on marginal quality of bonded resin composite restorations. Dent Mater 21:397–412
Bayne SC (2007) Dental restorations for oral rehabilitation—testing of laboratory properties versus clinical performance for clinical decision making. J Oral Rehabil 34:921–932
Stangel I, Ellis TH, Sacher E (2007) Adhesion to tooth structure mediated by contemporary bonding systems. Dent Clin N Am 51:677–694
Ernst CP, Brandenbusch M, Meyer G, Canbek K, Gottschalk B, Willerhausen B (2006) Two-year clinical performance of a nanofiller vs a fine-particle hybrid resin composite. Clin Oral Investig 10:119–125
Stefanski S, van Dijken JWV (2012) Clinical performance of a nanofilled resin composite with and without a flowable composite liner. A 2-year evaluation. Clin Oral Investig 16:147–153
Mahmoud SH, El-Embaby AE, AbdAllah AM, Hamama HH (2008) Two-year clinical evaluation of ormocer, nanohybrid and nanofill composite restorations in posterior teeth. J Adhes Dent 10:315–322
van Dijken JWV, Pallesen U (2011) Clinical performance of a hybrid resin composite with and without an intermediate layer of flowable resin composite: a 7-year evaluation. Dent Mater 27:150–156
Lindberg A, van Dijken JWV, Lindberg M (2006) Nine-year evaluation of a poly-acid-modified resin composite open sandwich technique in Class II cavities. J Dent 35:124–129
van Dijken JWV (2010) Durability of resin composite restorations in high C-factor cavities. A 12-year follow-up. J Dent 38:469–474
Bekes K, Boeckler L, Gernhardt CR, H-G S (2007) Clinical performance of a self-etching and a total-etch adhesive system—2-year results. J Oral Rehabil 34:855–861
Gordan VV, Mondragan E, Watson RE, Garvan C, Mjör I (2007) A clinical evaluation of a self-etching primer and giomer restorative material. Results at eight years. JADA 138:621–627
Perdigão J, Geraldeli S, Hodges JS (2003) Total-etch versus self-etch adhesive. Effect on postoperative sensitivity. JADA 134:1621–1629
Manhart J, Chen H-Y, Hickel R (2009) Clinical evaluation of the posterior composite Quixfil in class I and II cavities: 4-year follow-up of a randomized controlled trial. J Adhes Dent 12:1–7
Palanappian S, Elsen L, Lijnen I, Peumans M, van Meerbeek B, Lamberchts P (2012) Nanohybrid and microfilled hybrid versus conventional hybrid composite restorations: 5-year clinical wear performance. Clin Oral Investig 16:181–190
Mahmoud SH, El-Embaby AE, AbdAllah AM (2014) Clinical performance of ormocer, nanofilled, and nanoceramic resin composites in Class I and Class II restorations. A three-year evaluation. Oper Dent 39:32–42
Hickel R, Roulet J-F, Bayne S, Heintze SD, Mjör IA, Peters M, Rousson V, Randall R, Schmalz G, Tyas M, Vanherle G (2007) Recommendations for conducting controlled clinical studies of dental restorative materials. Clin Oral Investig 11:5–33
Shi L, Wang X, Zhao Q, Zhang Y, Ren Y, Chen Z (2010) Evaluation of packable and conventional hybrid resin composites in class I restorations: three-year results of a randomized, double-blind and controlled clinical trial. Oper Dent 35:11–19
Dresch W, Volpato S, Gomes JC, Ribeiro NR, Reis A, Loguercio AD (2006) Clinical evaluation of a nanofilled composite in posterior teeth: 12-month evaluation. Oper Dent 31:409–417
Brunthaler A, König F, Lucas T, Sperr W, Schedle A (2003) Longevity of direct resin composite restorations in posterior teeth. Clin Oral Investig 7:63–70
Swift EJ Jr, Ritter AV, Heymann HO, Sturdevant JR, Wilder AD Jr (2008) 36-months clinical evaluation of two adhesives and microhybrid resin composites in Class I restorations. Am J Dent 21:148–152
Boeckel A, Boeckel L, Eppendorf K, Schaller H-G, Gernhardt CR (2012) A prospective, randomized clinical trial of a two-step self-etching vs two-step etch-and-rinse adhesive and SEM margin analysis: four-year results. J Adhes Dent 14:585–592
Ermis RB, Kam O, Celik EU, Temel UB (2009) Clinical evaluation of a two-step etch&rinse and a two-step self-etch adhesive system in class II restorations: two-year results. Oper Dent 34:656–663
Bottenberg P, Jaquet W, Alaerts M, Keulemans F (2009) A prospective randomized clinical trial of one bis-GMA-based and two ormocer-based composite restorative systems in class II cavities: five-year results. J Dent 37:198–203
Jung M, Sehr K, Klimek J (2007) Surface texture of four nanofilled and one hybrid composite after finishing. Oper Dent 32:45–52
Ergücü Z, Türkün LS (2007) Clinical performance of novel resin composites in posterior teeth: 18 month results. J Adhes Dent 9:209–216
Acknowledgments
This study was partly supported by the County Council of Västerbotten and DENTSPLY DeTrey.
Conflict of interest
The authors declare that they have no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
van Dijken, J.W.V., Pallesen, U. Eight-year randomized clinical evaluation of Class II nanohybrid resin composite restorations bonded with a one-step self-etch or a two-step etch-and-rinse adhesive. Clin Oral Invest 19, 1371–1379 (2015). https://doi.org/10.1007/s00784-014-1345-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-014-1345-8