Abstract
Introduction
To investigate the factors associated with changes in vertebral bone mineral density during teriparatide treatment.
Materials and methods
Single centre, longitudinal study involving 145 osteoporotic postmenopausal women treated with teriparatide. Clinical evaluation, bone mineral density (BMD) measurements assessment and laboratory analyses were performed at baseline then after 12 and 18 months of treatment. Bone non-response to treatment was defined as no significant increase in BMD at 18 months as compared to baseline.
Results
Of the 145 women initially included, 109 completed the 18-month course of the treatment. 75% of them had a history of prior osteoporotic treatment. Baseline mean age was 60 ± 8 years. Mean baseline vertebral T-score was − 3.7 ± 0.7 and 83 (76%) women had suffered at least one vertebral fracture. At the end of treatment, 18 women (17%) were classified as non-responders. In the responder group (n = 91), vertebral BMD increased by 0.091 ± 0.04 g/cm2 (12.2 ± 5.3%). Clinical characteristics, baseline BMDs and the percentage of women previously treated with bisphosphonates as well as the duration of prior treatment did not significantly differ between the two groups of responders and non-responders. At baseline, non-responders had significant mean lower C-terminal fragment of type 1 collagen (CTX) values than responders (p < 0.01). Only baseline CTX values (r = 0.30 p < 0.01) were independently correlated to vertebral BMD changes during teriparatide treatment.
Conclusion
A minority of treated women had no vertebral densitometric gain after 18 months of teriparatide therapy. Low levels of baseline bone remodeling were the main factor associated with poor response to treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoporosis is a major health problem characterized by low bone mineral density (BMD) and micro-architectural deterioration of bone tissue with consequently an increased risk of fracture. Recombinant human parathyroid hormone (PTH) (1–34) fragment, teriparatide (TPT) is the only anabolic bone agent currently available in France for the treatment of postmenopausal women and men with osteoporosis and those at high risk of fracture for a total of 24 months [1]. In the Phase III pivotal study [2], subcutaneous administration of TPT at a dose of 20 µg/day for 21 months reduced the risk of new vertebral fractures by 65% and the risk of non-vertebral fractures by 53% [2]. The increase in BMD averaged 9% and 3% at the lumbar spine (LS) and femoral neck (FN), respectively [2]. BMD changes were significantly associated with micro-architectural bone changes and the anti-fracture efficacy [3, 4]. Changes in biochemical markers of bone remodeling throughout treatment reflect the cellular effects of TPT with an anabolic window that is characterised by early stimulation of bone formation [5,6,7] followed by increased bone resorption [7, 8]. In several studies, the initial increase in bone formation markers, especially the N-terminal propeptide not only of type 1 procollagen (P1NP) [9,10,11] or osteocalcin (OC) [12] but also of bone resorption markers such as the C-terminal fragment of type 1 collagen (CTX) [8, 13], is correlated with the end-of-treatment densitometric response.
There is large individual variability in the densitometric response to TPT with non-response rates ranging from 6 to 13% in clinical trials [14] but up to 35% in current practice [15]. The underlying reasons are still under discussion and there are probably numerous explanatory factors [16]. Several determinants such as age [17, 18], the initial level of BMD [17] or bone remodeling [19, 20] as well as a prior bisphosphonate (BPN) treatment [15, 17, 21, 22] were reported to influence the bone response to TPT.
We thus conducted a longitudinal study in 145 osteoporotic postmenopausal women who were treated with TPT in a routine clinical setting to quantify the bone response rate. We then sought to investigate whether there were clinical, densitometric and biological factors associated with the bone response to TPT.
Materials and methods
Population
All osteoporotic postmenopausal women who received a full 18-month course of TPT (Forsteo®) treatment between July 2012 and March 2020 in the Menopause and Bone Metabolic Disease Censer of the Toulouse University hospital were included in this study. Osteoporosis was diagnosed on the basis of at least one vertebral fracture and/or a lumbar T-score < -3 after extensive clinical, densitometric and biological assessment (see below).
Treatment associated one daily TPT self-injection with vitamin D3 supplementation, depending on baseline 25-hydroxy vitamin D levels (25OH-vitD) in order to maintain 25OH-vitD levels above 30 ng/ml throughout treatment. All women received prior instructions from a nurse on how to use the injection pen and store the product. Correct use of the pen was checked at each visit. To be selected, patients had to have had a full 18-month course of treatment and lumbar BMD assessed at the beginning and end of the study (see below).
Methods
Clinical assessment
At baseline, all women were interviewed and underwent extensive clinical examination to record their personal and family medical and gynaecological history as well as prior use of menopause hormone therapy (MHT) according to a previously published procedure [23]. Personal history of non-vertebral and vertebral fractures (circumstances of onset) was recorded and confirmed by radiographs whenever necessary. Main causes of secondary osteoporosis including endocrine disorders (hypogonadism, hyperthyroidism, glucocorticoid excess, type 1 or type 2 diabetes mellitus, primary hyperparathyroidism or prolactinoma, anorexia nervosa, bulimia), celiac disease or other gastrointestinal malabsorption syndromes, inflammatory or autoimmune diseases (rheumatoid arthritis, connective tissue diseases), renal dysfunction, hypercalciuria, inflammatory neurological disorders and malignancy together with use of medication (glucocorticoids therapy, aromatase inhibitors, etc.) were investigated and recorded. Prior treatments of osteoporosis (BPN, raloxifene) were carefully evaluated and recorded (type, duration of treatment, date of withdrawal). For the analysis of the results, such prior treatment was considered significant only if it had been taken for more than 6 months. Also, toxic habits (tobacco, alcohol) and vitamin D intake were documented.
Ethical approval was obtained from our hospital’s institutional review board.
BMD measurements
Vertebral and hip (including femoral neck and total hip) BMD were measured using an iDXA (Lunar GE) device according to standard procedures at baseline and after 12 and 18 months of treatment in all women. The lumbar spine (LS) measurement was the average of L2 to L4 BMD or at least two contiguous lumbar vertebrae. The precision of measurements in healthy and osteoporotic subjects in our centre was previously published [24]. Vertebral fracture assessment (VFA) analyses of the lumbar spine from T4 to L5 was also carried out with the same device following BMD acquisition at baseline and at the end of the 18-month TPT treatment.
Biological measurements
Morning fasting blood samples were collected in all women at baseline, at 3, 6, 12 and 18 months of treatment. Baseline assessment included standard laboratory tests (electrolytes, blood creatinine, liver function test, full and differential blood count, proteins), calcium metabolism parameters [blood calcium levels corrected for albumin, phosphorus, PTH and 25-hydroxy (OH) vitamin D] and bone turnover markers (CTX and osteocalcin (OC)). All assays were performed in the Biology Department of the Toulouse CHU (University Hospital Centre) using the automated system (Roche Cobas 8000 Chemistry and ISYS-IDS chemiluminescence). The main causes of secondary osteoporosis were sought through additional investigations (hormonology, inflammatory and immunity tests). Fasting blood samples were repeated at 3, 6, 12 and 18 months of TPT treatment for measurements of calcium metabolism and bone turnover parameters. CTX levels were measured at each point in all women throughout the entire 18-month course of the TPT treatment while OC levels were only available in about 50% of the women (n = 57) due to changes in the laboratory procedures during the study period of time.
Statistical analyses
Consistent with previously published data [14], bone non-response to TPT was defined as a variation which was less than the smallest significantly change in lumbar BMD at 18 months, and calculated from the reproducibility of measurements, i.e. a minimum variation of 0.034 g/cm2 for our centre [23].
Data are presented in the form of mean values, standard deviation and percentages. Inter-group comparisons were performed by Student's t test for continuous variables and Chi 2 test for qualitative variables. Longitudinal intra- and inter-group variations were assessed by paired Student t tests and analysis of variance. Potential predictors of changes in lumbar BMD at 18 months (expressed in percentage and g/cm2) were analysed by simple linear regression and multiple regression analyses for significant variables. The minimum level of significance was set at p < 0.05. The analyses were carried out using Medcalc software (version 18.11.3).
Results
Of the 145 postmenopausal osteoporotic women who initially started TPT treatment during the inclusion period, 13 were excluded due to premature treatment discontinuation (4 lost to follow-up and 9 stopped treatment due to lack of motivation or personal reasons within the first 3 months) and 13 for missing data (because their home was too far from our center to attend the scheduled follow-up visits). At baseline, these women were slightly older than the rest of the cohort (65 ± 8 years) but did not differ in terms of number of fractures and T-score levels. In addition, 10 women were excluded for unusable lumbar BMD (osteoarthritis, fracture, percutaneous vertebroplasty), which thus led to 109 women who were included in the final analysis.
The main clinical characteristics of the population are shown in Table 1. Mean age of the population was 60 ± 8 years.
14 women had a secondary cause of osteoporosis (3 diabetes mellitus, 2 anorexia nervosa, 3 early menopause, 2 inflammatory bowel disease, 1 pregnancy-associated osteoporosis, 1 corticosteroid-induced osteoporosis, 1 hypercalciuria, 1 thyroid cancer).
83 patients (76%) had a history of vertebral fractures (with an average of 2 fractures) and 49 (45%) had a history of non-vertebral fractures, half of which involved the upper arm, ribs, pelvis, wrist or femur (Table 1).
Of the total population, 29 women (27%) had been previously treated with BPN (13 with alendronate, 6 with residronate, 2 with zoledronic acid and 8 with multiple therapeutic sequences) for a mean treatment duration of 65 months (± 51) and a mean free treatment period of 32 months (± 30) prior to TPT treatment. In addition, 29 women (27%) had been taking MHT with an average duration of treatment of 68 months (± 61). Of the 29 women, 18 (12%) were still currently treated during the study and 11 had stopped on average 80 months (± 73) prior to TPT treatment. Finally, 24 patients had previously received raloxifene (22%) for a mean duration of treatment of 65 months (± 36) and a mean period of discontinuation of 9 months (± 8) prior to TPT treatment (Table 1).
At baseline, mean T-scores were − 3.4 ± 0.7, − 2.1 ± 0.6 and − 2.3 ± 0.7 at the lumbar spine, femoral neck and for total hip, respectively. One hundred women (92%) had a T-score ≤ − 2.5 at least at one bone site measurement (Table 2).
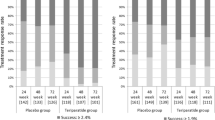
According to changes in lumbar BMD at 18 months, 91 women (83%) were categorized as responders and 18 (17%) as non-responders. Changes in vertebral and femoral BMD (expressed as absolute values) during 18 months of TPT treatment in both responder and non-responder groups are presented in Fig. 1.
In responders, there was a significant mean increase in LS BMD from baseline of 0.070 ± 0.04 g/cm2 (9.5 ± 5%) and 0.091 ± 0.04 g/cm2 (12.2 ± 5.3%) at 12 and 18 months, respectively (p < 0.0001). Compared to baseline, femoral neck and total hip BMD were also significantly higher at 12 and 18 months (FN: 0.008 ± 0.03 g/cm2 (1.1 ± 4%) and 0.022 ± 0.03 g/cm2 (3.1 ± 4.3%) (p < 0.001); TH: 0.013 ± 0.03 g/cm2 (1.9 ± 4.2%) and + 0.027 ± 0.03 g/cm2 (3.9 ± 5%) (p < 0.001)).
As expected, in non-responders there was no significant variation in LS (0.01 ± 0.02 g/cm2) or femur (FN: -0.009 ± 0.02 g/cm2, TH: − 0.006 ± 0.02 g/cm2) BMD at 18 months. The vertebral and femoral BMD changes expressed in absolute values (g/cm2) between baseline and both 12 and 18 months of TPT treatment were significantly different (p < 0.001) between the 2 groups.
The subgroup of women with secondary osteoporosis was significantly younger (56 ± 7 yrs vs 61 ± 7 yrs, p = 0.05), although there was no significant difference in baseline LS BMD values and BMD changes over the 18-month period of TPT treatment (0.096 ± 0.06 g/cm2 vs 0.075 ± 0.04 g/cm2, p = 0.12) between the two groups. The proportion of non-responders was similar between the two groups (21% vs 17%).
There was no significant difference in the increase in lumbar spine bone density in the 29 women previously treated with BPN compared to BPN-naive women (6.9 ± 5.5% and 9.2 ± 6.8% vs 8.7 ± 5.7% and 10.8 ± 6.2% after 12 and 18 months of teriparatide treatment, respectively). Also, there was the same number of women previously treated with BPN, MHT, or raloxifene in the two groups of non-responders and responders. Duration of prior osteoporotic treatment was also similar between the two groups (Table 1).
Over the course of the TPT treatment, two women experienced one incident fragility fracture (one femoral neck, one vertebrae) in the non-responder group versus none in the responder group.
Baseline clinical, densitometric and biological characteristics of both groups of responders and non-responders are shown in Tables 1 and 2. All clinical characteristics (age, weight, height, age and duration of menopause), smoking and number of prevalent fractures did not differ between the two groups. At baseline, non-responders had significantly lower CTX levels than responders: 324 ± 178 pg/ml vs 469 ± 226 pg/ml (p < 0.01) (Table 2). Serum CTX and OC concentrations increased significantly from the 3rd month of treatment onwards, reaching a peak at 6 months for CTX (+ 159 ± 217%) and for osteocalcin (+ 171 ± 112%) before declining at 18 months (Fig. 2). There was no significant difference in the CTX kinetic profile between responders and non-responders even though there was a trend toward a somewhat delayed increase in CTX levels in non-responders than in responders (data not shown).
In univariate regression analysis, baseline BMI (r = − 0.25 p < 0.01), baseline CTX levels (r = 0.30 p < 0.001), weight changes over 18 months (r = 0.21 p < 0.05) and changes in OC levels after 3 months of TPT treatment (r = 0.28 p < 0.05) (n = 57) were significantly associated with changes in LS BMD expressed in g/cm2. The association for baseline LS BMD was only significant (r = 0.21 p < 0.05) when LS BMD changes were expressed in percentage but not for absolute variation in g/cm2.
In multiple regression analyses, only baseline CTX levels (r = 0.30 p < 0.01) remained significantly and independently associated with the BMD changes at the lumbar spine. The results were not affected by the exclusion of the 18 patients who were treated with MHT over the course of the TPT treatment.
Discussion
In this longitudinal real-life study conducted in a cohort of quite young osteoporotic postmenopausal women, we found that only a minority of patients had no significant vertebral gain after 18 months of TPT treatment. The 17% non-responders in this study are in good concordance with published data [14, 16]. Also, the mean lumbar spine (LS) BMD changes (12% at the spine and 3–4% at the femur) at the end of the 18-month course of treatment were comparable to those reported in RCTs [1, 2]. As already reported, higher baseline BMI as well as greater BMD values were negatively associated with changes in LS BMD values at the end of treatment [17, 20, 21]. On the other hand, there was a positive correlation between baseline CTX mean values as well as changes in OC levels from baseline and LS BMD changes over the course of the study. Only baseline plasma CTX levels remained significantly and independently associated with changes in LS BMD in multivariate analyses.
The impact of age on the bone response to TPT is still under discussion. Several studies have shown that the gain in BMD is not age dependent [14, 15, 19], or that is greater in older patients [17]. In our study, age was not associated with changes in LS BMD. This certainly reflects selection biases linked to the heterogeneity of the study populations (patients’ age, type of osteoporosis, role of osteoarthritis). The mean age of our population was about 10 years younger than that of osteoporotic cohorts usually treated with TPT (60 vs 70 years) [2, 9, 17, 19, 20, 24]. Women with secondary osteoporosis were significantly younger by an average of 5 years than the rest of our cohort. Nevertheless, there was no difference in baseline mean LS BMD values or in the magnitude of vertebral densitometric gain at 18 months according to the type of osteoporosis (secondary vs postmenopausal osteoporosis) just as the rate of non-response (21%) was the same in these two groups. Most studies found no influence of weight on bone response to teriparatide [15, 17, 21]. In our study, baseline BMI and weight gain during treatment were associated with changes in LS BMD in univariate analyses, which was no longer the case in multivariate analyses.
Previous BPN intake is the most common factor associated with non-response to TPT treatment [17, 19, 25, 26]. In prospective trials [17, 19, 22, 24, 26], vertebral gain was reported 3 to 7% lower in patients previously treated with anti-osteoclastic agents than in treatment-naive patients, particularly for molecules that bind strongly to bone mineral. This effect is more marked with the BPNs which have the greatest retention time in bone (greater for alendronate compared to risedronate [19, 24, 26]). It is practically non-existent for raloxifene, which has a weaker anti-osteoclastic effect than BPN [24]. Similarly, prior use of MHT did not modify the bone response to TPT [27]. In our study, mean baseline CTX values were significantly lower in women previously treated with BPN than in treatment-naive women or women previously treated with raloxifene or MHT (data not shown). However, the number of women previously treated with BPN did not differ between the two non-responder and responder groups, although there was a trend toward a longer duration of prior BPN treatment and a shorter wash-out period before starting TPT in non-responders than in responders.
Teriparatide triggers an overall increase in bone formation and resorption activities, and early changes (3–6 months) in bone biomarkers are positively correlated (r = 0.2 to 0.5) with BMD gain after 12–24 months of TPT [8,9,10, 13]. Although P1NP was reported the best predictive performance marker [5, 8, 11], similar results were obtained with OC [12] but also bone resorption markers such as CTX [8, 13]. We found a positive correlation between the increase in OC levels at 3 months and the gain in BMD after 18 months of TPT. Strictly parallel kinetics of CTX changes were observed in both responders and non-responders throughout the 18-month period of treatment, which suggests that the difference in LS BMD changes between the two groups was not explained by differences in bone resorption activity throughout the course of treatment. We did not have sufficient data to determine whether or not there was a difference in the kinetic of OC changes between the two groups. A smaller increase in P1NP levels was reported during the first 6 months of TPT in non-responder women (similar to that observed in women previously treated with BPN [9]), although the difference with responders decreased over time and was no longer significant after 8 months of TPT treatment [19, 22, 26]. It could be assumed that a low level of bone remodelling either spontaneous or related to BPN treatment is likely to limit the exposure of bone cells to PTH, although P1NP levels were shown to increase in the majority of TPT non-responders [5, 14, 16].
Our study has a number of limitations. Given the relatively small number of non-responders, it cannot be excluded that our study was not powered enough to evidence significant differences in clinical characteristics or prior osteoporotic treatments (notably BPN) between the two groups of responders and non-responders. It is also the case for the correlations between biomarkers changes and the BMD gain. We used OC to assess bone formation activity while P1NP is the currently recommended biomarker, which may have limited the early identification of non-responders. Also, our study did not allow to draw conclusions regarding the impact of densitometric non-response on fracture risk. Only two women in the non-responder group sustained a major fracture over the course of the study and none in the responder group. Despite a positive correlation between vertebral BMD changes and the anti-fracture efficacy of TPT [3], it was not shown that non-responders to TPT had a higher fracture rate than responders at least over the duration of treatment. Also, none of the parameters which were associated with the bone non-response such as age, baseline BMD, biochemical markers of bone remodelling or prior BPN treatment were found to impact the anti-fracture efficacy of TPT in clinical trials [23, 28, 29]. Finally, it should be underlined that the reality of the "non-response" concept to well-conducted TPT treatment over 18 to 24 months has been challenged and partly linked to the reproducibility issue of BMD measurements [16]. We do not believe that this was the case in our study since BMD monitoring was conducted under optimal conditions (same experienced technician, same device and software used for the analyses, daily quality controls and centralised analysis by the same investigator). Furthermore, the vertebral BMD threshold value, which defined the non-response in our study, was calculated from the reproducibility performances assessed in our centre in routine setting and not based on theoretical values. The fact that the two bone response groups also differ in femoral BMD changes probably confirms the relevance of a posteriori approach.
Finally, despite these limitations, our study has the advantage, unlike clinical trials, of being representative of real-life use of TPT therapy in a cohort of relatively young, clinically well-characterized postmenopausal osteoporotic women.
In conclusion, this study confirms in a real-life setting, the good tolerance and bone efficacy of TPT in a population of relatively young women with postmenopausal or secondary osteoporosis. A minority of patients were categorized as “non-responders” after 18 months of treatment. A low baseline level of bone remodelling (especially in women previously treated with bisphosphonates) were the only factors associated with the bone non-response. Some data suggest that this does not preclude the anti-fracture efficacy of teriparatide. Further studies are therefore needed to better assess the possibility of a delayed response in some patients as well as the subsequent risk of fracture.
References
Thomas T (2006) Intermittent parathyroid hormone therapy to increase bone formation. Jt Bone Spine 73:262–269
Neer RM, Arnaud CD, Zanchetta JR, Prince R, Gaich GA et al (2001) Effect of parathyroid hormone (1–34) on fractures and bone mineral density in postmenopausal women with osteoporosis. N Engl J Med 344:1434–1441
Chen P, Miller PD, Delmas PD, Misurski DA, Krege JH et al (2006) Change in lumbar spine BMD and vertebral fracture risk reduction in teriparatide-treated postmenopausal women with osteoporosis. J Bone Miner Res 21:1785–1790
Chen P, Miller PD, Recker R, Resch H, Rana A et al (2007) Increases in BMD correlate with improvements in bone microarchitecture with teriparatide treatment in postmenopausal women with osteoporosis. J Bone Miner Res 22:1173–1180
Krege JH, Lane NE, Harris JM, Miller PD (2014) PINP as a biological response marker during teriparatide treatment for osteoporosis. Osteoporos Int 25:2159–2171
Eastell R, Krege JH, Chen P, Glass EV, Reginster J-Y et al (2006) Development of an algorithm for using PINP to monitor treatment of patients with teriparatide. Curr Med Res Opin 22:61–66
Glover SJ, Eastell R, McCloskey EV, Rogers A, Garnero P et al (2009) Rapid and robust response of biochemical markers of bone formation to teriparatide therapy. Bone 45:1053–1058
Eastell R, Mitlak BH, Wang Y, Hu M, Fitzpatrick LA et al (2019) Bone turnover markers to explain changes in lumbar spine BMD with abaloparatide and teriparatide: results from ACTIVE. Osteoporos Int 30:667–673
Blumsohn A, Marin F, Nickelsen T, Brixen K, Sigurdsson G et al (2011) Early changes in biochemical markers of bone turnover and their relationship with bone mineral density changes after 24 months of treatment with teriparatide. Osteoporos Int 22:1935–1946
Chen P, Satterwhite JH, Licata AA, Lewiecki EM, Sipos AA et al (2005) Early changes in biochemical markers of bone formation predict BMD response to teriparatide in postmenopausal women with osteoporosis. J Bone Miner Res 20:962–970
Niimi R, Kono T, Nishihara A, Hasegawa M, Matsumine A et al (2014) An algorithm using the early changes in PINP to predict the future BMD response for patients treated with daily teriparatide. Osteoporos Int 25:377–384
Lu C, Chen Y, Zhang B, Chen Y, Bai F et al (2017) Response to teriparatide in Chinese patients with established osteoporosis: osteocalcin and lumbar spine bone-mineral density changes from teriparatide phase III study. Clin Interv Aging 12:1717–1723
Tsujimoto M, Chen P, Miyauchi A, Sowa H, Krege JH et al (2011) PINP as an aid for monitoring patients treated with teriparatide. Bone 48:798–803
Gallagher JC, Rosen CJ, Chen P, Misurski DA, Marcus R et al (2006) Response rate of bone mineral density to teriparatide in postmenopausal women with osteoporosis. Bone 39:1268–1275
Elraiyah T, Ahmed AH, Wang Z, Farr JN, Murad MH et al (2016) Predictors of teriparatide treatment failure in patients with low bone mass. Bone Rep 4:17–22
Heaney RP, Watson P (2011) Variability in the measured response of bone to teriparatide. Osteoporos Int 22:1703–1708
Obermayer-Pietsch BM, Marin F, McCloskey EV, Hadji P, Farrerons J et al (2008) Effects of two years of daily teriparatide treatment on BMD in postmenopausal women with severe osteoporosis with and without prior antiresorptive treatment. J Bone Miner Res 23:1591–1600
Schwarz P, Jorgensen NR, Mosekilde L, Vestergaard P (2012) Effects of increasing age, dosage, and duration of PTH treatment on BMD increase–a meta-analysis. Calcif Tissue Int 90:165–173
Boonen S, Marin F, Obermayer-Pietsch B, Simões ME, Barker C et al (2008) Effects of previous antiresorptive therapy on the bone mineral density response to two years of teriparatide treatment in postmenopausal women with osteoporosis. J Clin Endocrinol Metab 93:852–860
Niimi R, Kono T, Nishihara A, Hasegawa M, Matsumine A et al (2014) Determinants associated with bone mineral density increase in response to daily teriparatide treatment in patients with osteoporosis. Bone 66:26–30
Niimi R, Kono T, Nishihara A, Hasegawa M, Kono T et al (2016) A retrospective analysis of nonresponse to daily teriparatide treatment. Osteoporos Int 27:2845–2853
Middleton ET, Steel SA, Doherty SM (2007) The effect of prior bisphosphonate exposure on the treatment response to teriparatide in clinical practice. Calcif Tissue Int 81:335–340
Geusens P, Marin F, Kendler DL, Russo LA, Zerbini CAF et al (2018) Effects of teriparatide compared with risedronate on the risk of fractures in subgroups of postmenopausal women with severe osteoporosis: the VERO trial. J Bone Miner Res 33:783–794
Ettinger B, San Martin J, Crans G, Pavo I (2004) Differential effects of teriparatide on BMD after treatment with raloxifene or alendronate. J Bone Miner Res 19:745–751
Pouilles JM, Tremollieres F, Todorovsky N, Ribot C (1991) Precision and sensitivity of dual-energy x-ray absorptiometry in spinal osteoporosis. J Bone Miner Res 6:997–1002
Miller PD, Delmas PD, Lindsay R, Watts NB, Luckey M et al (2008) Early responsiveness of women with osteoporosis to teriparatide after therapy with alendronate or risedronate. J Clin Endocrinol Metab 93:3785–3793
Ste-Marie LG, Schwartz SL, Hossain A, Desaiah D, Gaich GA et al (2006) Effect of teriparatide [rhPTH(1–34)] on BMD when given to postmenopausal women receiving hormone replacement therapy. J Bone Miner Res 21:283–291
Delmas PD, Licata AA, Reginster JY, Crans GG, Chen P et al (2006) Fracture risk reduction during treatment with teriparatide is independent of pretreatment bone turnover. Bone 39:237–243
Marcus R, Wang O, Satterwhite J, Mitlak B (2003) The skeletal response to teriparatide is largely independent of age, initial bone mineral density, and prevalent vertebral fractures in postmenopausal women with osteoporosis. J Bone Miner Res 18:18–23
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors have no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Anna, G., Anne-Lise, F., Clémence, D. et al. Factors associated with bone response to teriparatide in young postmenopausal women with osteoporosis. J Bone Miner Metab 41, 278–285 (2023). https://doi.org/10.1007/s00774-023-01412-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00774-023-01412-3